Abstract
This study assessed the relationship between solitary confinement and post-traumatic stress disorder (PTSD) symptoms in a cohort of recently released former prisoners. The cross-sectional design utilized baseline data from the Transitions Clinic Network, a multi-site prospective longitudinal cohort study of post-incarceration medical care. Our main independent variable was self-reported solitary confinement during the participants’ most recent incarceration; the dependent variable was the presence of PTSD symptoms determined by primary care (PC)-PTSD screening when participants initiated primary care in the community. We used multivariable logistic regression to adjust for potential confounders, such as prior mental health conditions, age, and gender. Among 119 participants, 43% had a history of solitary confinement and 28% screened positive for PTSD symptoms. Those who reported a history of solitary confinement were more likely to report PTSD symptoms than those without solitary confinement (43 vs. 16%, p < 0.01). In multivariable logistic regression, a history of solitary confinement (OR = 3.93, 95% CI 1.57–9.83) and chronic mental health conditions (OR = 4.04, 95% CI 1.52–10.68) were significantly associated with a positive PTSD screen after adjustment for the potential confounders. Experiencing solitary confinement was significantly associated with PTSD symptoms among individuals accessing primary care following release from prison. Larger studies should confirm these findings.
Keywords: Solitary confinement, Incarceration, Post-traumatic stress disorder, Post-traumatic stress disorder screening
Introduction
The USA incarcerates more of its citizens than any country in the world [1]. Chronic medical and mental health conditions are overrepresented among incarcerated individuals [2]. Incarceration itself may also pose independent health risks, including exposure to violence [3], infectious diseases [2], and the harsh conditions of solitary confinement.
The term “solitary confinement” may be used to describe different environments (special housing units (SHU), administrative segregation, restrictive housing, or “supermax” correctional facilities), but in general refers to use of isolation cells where inmates remain for 22–24 hours daily and have little physical contact with other inmates. Additionally, solitary confinement may restrict access to correctional programming, personal belongings, or means for mental stimulation, and time outside of the cell for exercise or hygiene may be limited to only a few hours per week [4–7]. Solitary confinement is commonly a form of punishment, but correctional staff may also place inmates at safety risk (e.g., LGBT or elderly inmates) in protective custody or isolate inmates who pose a threat to others [5, 6]. In the USA, approximately 20% of prison and 18% of jail inmates experience solitary confinement annually [5]. To our knowledge, there are no studies documenting lifetime prevalence of exposure to solitary confinement among the formerly incarcerated, but the fraction is likely much higher.
While the conditions of solitary confinement may be similar among inmates segregated from the general population, including the restriction of movement, programming, and contact with other inmates and staff, there are varying degrees of the completeness of this isolation. Therefore, not all solitary confinement is interchangeable and specific environmental conditions may have differing likelihood of producing negative effects on those incarcerated within them [8, 9]. One study in Colorado noted that conditions in punitive segregation (shorter-term isolation in response to “rule violation”) and a dedicated administrative segregation facility varied with regards to access to services, with library services, educational and treatment programs available cell-side in administrative segregation [10]. A longitudinal examination of this administrative segregation facility found no association with exacerbation of mental health symptoms measured by the investigators compared with general population controls [10]. Thus, the type of solitary confinement may be important in studying the effects of this exposure.
Several studies suggest that solitary confinement may contribute to high levels of psychological distress and physical harm during incarceration. From 2011 to 2012, the National Inmate Survey screened a sample of 91,177 adult inmates nationwide for serious psychological distress and a number of other outcomes and exposures. Serious psychological distress was more common among prisoners who had experienced solitary confinement within the past year than those who had not (29 vs. 15%) [5]. In the New York City jail system, inmates exposed to solitary confinement were nearly seven times more likely to commit acts of self-harm than those who were unexposed [11]. These studies suggest acute harms; however, it is unknown whether the exposure to solitary confinement continues to affect health after release from incarceration.
The long-term mental and physical health sequelae of isolation are not well understood. In 1983, a psychiatrist performed a series of interviews with inmates in solitary confinement in a Massachusetts correctional facility and documented a distinct set of shared disturbances among them, including perceptual distortions, paranoid ideation without overt delusions, ego-dystonic aggressive fantasies, difficulties with memory and attention, and derealization experiences [8]. It was noted that these effects of solitary confinement varied with the rigidity of the enforced sensory and social isolation [8]. Likewise, in a random sampling of “supermax” prisoners at Pelican Bay (CA) State Prison’s SHU in 2003, there were elevated rates of eight mental health symptoms (ranging from heightened anxiety to hallucinations) with 34% of the sample experiencing all eight of the symptoms and more than half (56%) experiencing at least five of them [9]. The author of this study noted that many of the deleterious effects of solitary confinement “are analogous to the acute reactions suffered by torture and trauma victims, including post-traumatic stress disorder or PTSD” [9].
The mechanisms by which solitary confinement may produce short- and long-term harms are not fully elucidated. One theory is that isolation and lack of stimulation produce severe distress because human beings require social contact to perform “social reality testing,” which helps them to distinguish whether their perceptions of the environment are real [4]. Potentially, following periods of distress, individuals could develop post-traumatic stress disorder (PTSD).
By definition, PTSD develops when an initial traumatic event is persistently re-experienced without intention to do so by the individual, leading to avoidance, negative alterations in cognition and mood, and derangements in arousal and reactivity to otherwise benign stimuli [12]. A large meta-analysis found that risk factors most closely associated with development of PTSD were lack of social support, life stress, and trauma severity [13]. When these risk factors coincided with or closely followed the traumatic episode temporally, PTSD symptoms were most likely [13]. Because solitary confinement removes opportunities for social support and likely increases distress, it may put individuals exposed to solitary at risk for developing PTSD.
The current literature has not addressed solitary confinement and PTSD. Formerly incarcerated individuals have significantly more lifetime traumatic episodes and a two times higher rate of PTSD symptoms than those with similar demographics who have never experienced incarceration [14]. Having a PTSD diagnosis was associated with arrest and prior incarceration in a civilian cohort recruited from medical (non-psychiatric) waiting rooms in an urban hospital system [3]. However, there are no studies assessing solitary confinement as a harmful exposure.
In this study, we investigated the link between solitary confinement and PTSD symptoms in a cohort of primary care patients who had recently been released from prison. We hypothesized that prior solitary confinement would be associated with PTSD symptoms after adjustment for potential confounding factors. We also explored whether time in solitary confinement and the type of solitary confinement (punitive vs. administrative) were associated with PTSD symptoms.
Methods
This cross-sectional study utilizes baseline data from the Transitions Clinic Network (TCN, www.transitionsclinic.org), a multi-site prospective longitudinal cohort study of post-incarceration medical care. Because the parent study included a PTSD screening questionnaire which can be administered in a primary care setting, two TCN sites (Bronx, NY and New Haven, CT) chose to implement a secondary questionnaire assessing for exposure to solitary confinement.
Setting
The TCN includes 15 community-based healthcare programs in seven states and Puerto Rico. Multi-disciplinary health care teams at each site include community health workers (CHWs) who have a history of incarceration and have been trained in health education, health system navigation, and motivational enhancement. CHWs link individuals released from prison or jail to primary care at the TCN sites. Other features of the TCN sites include provider training in best practices in caring for individuals with a history of incarceration, an ability to provide or refer for mental health and substance use services, and linkages to social service providers, including housing, employment, and legal aid. Individual TCN sites have been described in more detail [15, 16].
Participants
All new patients at the two TCN sites seen between May 2013 and February 2015 were screened for inclusion. Inclusion criteria were (1) recent release from prison (within 6 months), (2) presence of at least one chronic health condition (including substance use and mental health conditions) warranting primary medical care or age equal to or greater than 50 years old, (3) ability to provide consent in English or Spanish, and (4) plan to live in the area near the TCN program site for the duration of the study. Patients who planned to return to a previous primary care provider were excluded.
Data Collection
We used data from baseline surveys from the two TCN sites. Surveys were administered by trained research staff either in person at the TCN site or via telephone. Data were stored in an online HIPAA-approved portal, and relevant clinical information was provided to primary care providers to facilitate medical care. Data included sociodemographics; self-reported incarceration history; past medical, mental health, and substance use history; and treatment.
Measures
The main independent variable was any self-reported solitary confinement during the participants’ most recent incarceration; the dependent variable was the presence of PTSD symptoms determined by primary care (PC)-PTSD screening at the time of the baseline survey.
Solitary Confinement
Participants reported whether or not they were placed in solitary confinement during their last prison term. We used self-report of any solitary confinement (dichotomous, yes/no) for the main analysis. We also performed additional analyses based on the type of restricted status (disciplinary action, protective custody, short- or long-term administrative segregation, chronic discipline, special risk group, or special needs), the total time spent in solitary confinement in the last prison term (continuous, number of weeks), and whether or not the participant was released from prison directly from restricted status.
Post-Traumatic Stress Disorder Symptoms
All participants were screened for PTSD symptoms using a validated 4-item screen for PTSD in primary care, or PC-PTSD. Participants were first asked about presence of a prior traumatic event, and then asked four questions to assess for symptoms of PTSD in the past 30 days. Participants reporting a prior traumatic event and three or four PTSD symptoms were considered to screen positive (categorical, yes/no) for symptoms. Prior literature supports a cut point of three items (sensitivity 69–85%; specificity 82–92%) [17–20]. The PC-PTSD has been validated in primary care and prison settings and has similar or better positive and negative predictive value compared to longer screening tools [17, 18, 21].
Covariates
Other potential confounders used for the analyses included age (continuous, years), race/ethnicity (categorical: non-Hispanic black, Hispanic, non-Hispanic white, other), marital status (dichotomous: single/divorced or married), education (categorical: less than high school grad, GED, high school grad, at least some college, college graduate), unstable housing (dichotomous, yes/no: determined by current homelessness or immediate concern for future homelessness within 1 month of interview due to temporary living arrangement), prior PTSD diagnosis (dichotomous, yes/no: self-reported), any chronic mental health condition (dichotomous, yes/no: defined as any self-reported major depressive disorder, bipolar disorder, schizophrenia, or PTSD), current substance use (dichotomous, yes/no: defined as self-reported use of any illicit substance after release from prison, including cocaine, methamphetamine, heroin or other opiates, hallucinogens, ecstasy, or prescription drugs that had not been prescribed to participants), lifetime substance use (dichotomous, yes/no: defined as any self-reported use of illicit substances listed above), any substance use disorder (dichotomous, yes/no: self-reported), length of most recent incarceration (continuous, months), parole status (dichotomous, yes/no: self-reported), and time from prison release to primary care engagement (continuous, days).
Analysis
First, we compared sociodemographic and clinical variables between participants with and without exposure to solitary confinement using chi-square, Mann–Whitney, or T tests as appropriate. Next, we constructed a multivariable logistic regression model with solitary confinement as the main independent variable and PTSD symptoms as the dependent variable. In our preliminary model, we adjusted for age, gender, and history of mental health conditions, which are known risk factors for PTSD [13]. We then added the other covariates, one at a time in a forward stepwise fashion, which were either unbalanced between those with and without exposure to solitary confinement or independently associated with PTSD symptoms (p < 0.15 in bivariate testing). We only retained variables that remained significantly associated with the dependent variable, because of the small sample size.
We then performed two sensitivity analyses. We excluded individuals with a prior PTSD diagnosis, and repeated the multivariable logistic regression model described above to determine whether solitary confinement was associated with new symptoms of PTSD. We also stratified the sample by history of chronic mental health conditions and tested the association of solitary confinement and PTSD symptoms using chi-square analysis.
Finally, we performed several exploratory analyses. We compared PTSD symptoms among participants with short periods of solitary confinement (≤1 week) to those with longer periods (>1 week) using chi-square. We also compared PTSD symptoms among participants reporting solitary confinement for disciplinary reasons to those reporting solitary confinement for other reasons using chi-square.
The study was approved by the Yale University School of Medicine Human Investigation Committee, the Einstein institutional review board, and the Office for Human Research Protections in the US Department of Health and Human Services.
Results
Of 119 participants with data on solitary confinement, median age was 44 years (interquartile (IQ) range 35–52), and most were male (85%), non-Hispanic Black (51%) or Hispanic (34%), and unstably housed (85%). Prior mental health conditions (42%), a prior PTSD diagnosis (17%), and lifetime substance use (66%) were common. None of these sociodemographic or clinical variables differed between those with and without a history of solitary confinement (Table 1).
Table 1.
Characteristics of formerly incarcerated individuals by history of solitary confinement in recent incarceration
| Characteristic | No Hx solitary (N = 68) | Hx solitary (N = 51) | P value |
|---|---|---|---|
| Age (median, IQR) | 47 (38.5–52) | 43 (33–52) | 0.10 |
| Male | 59 (87%) | 42 (82%) | 0.19 |
| Race/ethnicitya | 0.78 | ||
| Non-Hispanic Black | 33 (50) | 27 (53) | |
| Hispanic | 22 (33) | 18 (36) | |
| Non-Hispanic White | 9 (14) | 6 (12) | |
| Other | 2 (3) | 0 (0) | |
| Married | 11 (16) | 4 (8) | 0.18 |
| Education | 0.80 | ||
| Did not complete high school | 19 (28) | 17 (33) | |
| High school graduate or completed GED | 32 (47) | 23 (45) | |
| At least some college | 17 (25) | 11 (22) | |
| Unstable housingb | 55 (85) | 42 (86) | 0.87 |
| Any chronic mental health conditionc | 27 (40) | 23 (45) | 0.56 |
| Prior PTSD diagnosis | 8 (12) | 12 (24) | 0.09 |
| Any substance use (current)d | 12 (18) | 11 (22) | 0.58 |
| Substance use disorder (lifetime)e | 37 (62) | 26 (58) | 0.69 |
| Alcohol use disorder (lifetime) | 23 (38) | 11 (24) | 0.12 |
| On parole | 53 (78) | 45 (88) | 0.15 |
| Incarceration length, median months (IQR) | 24.5 (11–43) | 45 (21–82) | <0.01 |
| Time to TCNf engagement, median days (IQR) | 16 (7–42) | 21 (13–50) | 0.25 |
a2 missing
b5 missing
cSelf-reported depression, schizophrenia, bipolar, or PTSD
dSelf-reported heroin, cocaine, or methamphetamine use since release from prison
eSelf-reported, any “drug dependence”
fTransitions Clinic Network, initial primary care visit
Overall, 43% of the participants had a history of solitary confinement. Of these, the most common reason for solitary confinement was disciplinary action (73%). Forty-two percent remained in solitary confinement for 1 month to 1 year, and 12% remained in solitary confinement for more than a year (Table 2).
Table 2.
Characteristics of solitary confinement (N = 51)
| Characteristic | Number (%) |
|---|---|
| Time in solitary confinementa | |
| ≤1 week | 10 (20) |
| 1–4 weeks | 13 (26) |
| 1–12 months | 21 (42) |
| >1 year | 6 (12) |
| Type of restricted statusb | |
| Disciplinary action | 37 (73) |
| Protective custody | 6 (12) |
| Administrative segregation (short-term) | 17 (33) |
| Administrative segregation (long-term) | 3 (6) |
| Chronic discipline | 3 (6) |
| Special risk group | 6 (12) |
| Special needs | 2 (4) |
| Directly released from solitary confinement | 4 (8) |
a1 missing
bMay have experienced more than one
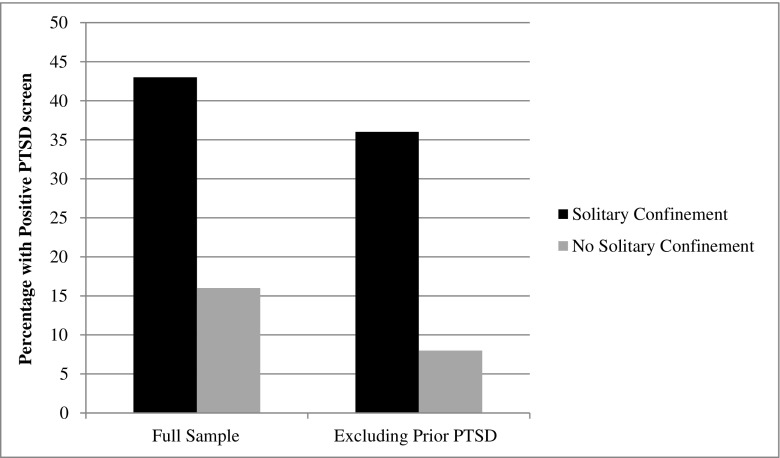
Thirty-three participants (28%) screened positive for PTSD symptoms. In bivariate testing, those with a history of solitary confinement were more likely to report PTSD symptoms than those without solitary confinement (43 vs. 16%, p < 0.01) (Fig. 1).
Fig. 1.
Prevalence of post-traumatic stress disorder (PTSD) symptoms by solitary confinement history among former prisoners seeking primary care (N = 119)
In multivariable logistic regression, a history of solitary confinement (adjusted odds ratio (AOR) = 3.93, 95% CI 1.57–9.83) and chronic mental health conditions (AOR = 4.04, 95% CI 1.52–10.68) were significantly associated with a positive PTSD screen. The final model also included male gender and age, but these variables were not significantly associated with PTSD symptoms. Current substance use, time from release to primary care engagement, length of incarceration, parole status, and history of alcohol use disorder were introduced but not retained in the final model.
In the sensitivity analyses, excluding those with prior PTSD diagnoses decreased the number of participants who screened positive for PTSD symptoms, but PTSD symptoms remained significantly more common among those with than those without solitary confinement (36 vs. 8%, p < 0.01) (Fig. 1). In our adjusted regression model, solitary confinement remained significantly associated with PTSD symptoms. After stratifying by a history of prior mental health conditions, solitary confinement remained significantly associated with PTSD symptoms in those without (32 vs. 5%, p < 0.01) but not among those with a history of a chronic mental health conditions (57 vs. 33%, p = 0.10).
In exploratory analyses, there was no difference in PTSD symptoms between those with longer (>1 week) and shorter (≤1 week) periods of solitary confinement (38 vs. 33%). The reason for solitary confinement was not associated with presence of PTSD symptoms.
Discussion
Among formerly incarcerated individuals with chronic health conditions who were linked to primary care, more than 40% reported a history of solitary confinement during their most recent incarceration. PTSD symptoms were also common with 28% screening positive using a validated screening instrument. Consistent with our hypothesis, we found a significant association between prior solitary confinement and PTSD symptoms, with those reporting solitary confinement having a three times greater odds of reporting PTSD symptoms after adjustment for potential confounders. Based on our methods, we cannot be certain that solitary confinement played a causative role in the exacerbation or development of PTSD symptoms, but our findings highlight the specific mental health needs of individuals recently released from prison.
To our knowledge, our study is the first to demonstrate an association between prior solitary confinement and PTSD symptoms among former prisoners. In one other study, Danish prisoners in solitary confinement had more psychiatric illness than the general population, but PTSD rates were not reported [22]. In the USA, the Department of Justice has documented high rates of serious psychological distress among inmates held in solitary confinement, but it is unknown whether these individuals went on to develop PTSD [5]. Our findings should be confirmed by larger studies, but they raise concern that solitary confinement may have health effects following release from prison.
In interpreting our data, we cannot be sure of the direction of the association, but both directions have important implications. Solitary confinement may be a traumatic event that could lead to PTSD, especially if there is a lack of attention to inmates’ mental health during incarceration. Alternatively, inmates with unrecognized PTSD may have exacerbations of symptoms while incarcerated, which could lead to conflicts that result in punishment and solitary confinement. Therefore, better screening and provision of mental health care during incarceration and upon release is likely necessary to meet inmates’ needs. One correctional facility has proposed therapeutic alternatives to solitary confinement for individuals with serious mental illness [23]. A cohort recruited before exposure to solitary confinement could better establish causality, and qualitative research could better elucidate the precise role of solitary confinement in development of PTSD symptoms. Additional research, including longitudinal studies documenting mental health status before and after exposure to incarceration and solitary confinement, would be made more robust by including a structured clinical interview for DSM disorders (SCID) to definitively diagnose PTSD among participants who screened positive for PTSD symptoms.
Solitary confinement was common in the TCN cohort–primary care patients with chronic medical conditions returning home from prison. Most participants reporting solitary confinement were in isolation for at least a month and 12% for at least a year. While we did not find association between length of time in solitary confinement or reason for solitary confinement and PTSD symptoms, future studies should explore how the specific conditions of confinement may be associated with worse health outcomes, including PTSD.
The strengths of our study include a patient population that was recently released from prison, use of a validated screening instrument for PTSD, and a detailed measure of solitary confinement. However, there are several limitations. The TCN study recruited participants because of medical and psychiatric needs, so both solitary confinement and post-traumatic stress disorder symptoms may be overrepresented in this sample. It is possible that PTSD symptoms were present, but unrecognized, prior to the period of solitary confinement. The participants were not asked to identify the traumatic event that preceded PTSD symptoms, so we are unsure of the precise role that solitary confinement may have played. We had a small sample size and data (for both solitary confinement and past medical or mental health diagnoses) are all based on self-report. Finally, it is possible that unmeasured confounders could explain the associations that we detected.
Nearly all prisoners (93%) are eventually released, and if those experiencing solitary confinement are negatively affected by the exposure, it is society at large that bears the burden of “resocializing” them [24]. Others have more specifically called for the medical community to be involved in the debate regarding the use of solitary confinement in the USA [6]. Our study highlights a potentially important association between solitary confinement and PTSD symptomatology. Because rates of recidivism and re-incarceration are so high following release from incarceration, additional research is critical to understand whether exposures during incarceration, such as solitary confinement, contribute to challenges with successful community reentry and overall wellness among formerly incarcerated individuals. Understanding the health needs of prisoners is critical to both individual and community health.
Acknowledgments
We thank all of the community health workers, clinical staff, and research staff who contributed to the Transitions Clinic Network study. We also thank our patients for their participation.
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies.
The project described was supported by Grant Numbers 1CMS331071-01-00 and 1C1CMS331300-01-00 from the Department of Health and Human Services, Centers for Medicare and Medicaid Services
Contributor Information
Brian O. Hagan, Email: brian.hagan@med.einstein.yu.edu
Aaron D. Fox, Phone: 718-920-7173, Email: adfox@montefiore.org
References
- 1.Glaze E, Kaeble D. Correctional populations in the United States, 2013. US Department of Justice, Bureau of Justice Statistics; December 2014, NCJ 248479.https://www.bjs.gov/content/pub/pdf/cpus13.pdf.
- 2.Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–65. doi: 10.1016/S0140-6736(10)61053-7. [DOI] [PubMed] [Google Scholar]
- 3.Donley S, Habib L, Jovanovic T, et al. Civilian PTSD symptoms and risk for involvement in the criminal justice system. J Am Acad Psychiatry Law. 2012;40(4):522–529. [PMC free article] [PubMed] [Google Scholar]
- 4.Arrigo BA, Bullock JL. The psychological effect of solitary confinement on prisoners in supermax units—reviewing what we know and recommending what should change. Intl J Offender Ther Comp Criminol. 2008;52(6):622–640. doi: 10.1177/0306624X07309720. [DOI] [PubMed] [Google Scholar]
- 5.Beck AJ. Use of restrictive housing in US prisons and jails, 2011–12. Washington DC: Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2015. [Google Scholar]
- 6.Williams B, Ahalt C. Reforming solitary-confinement policy—heeding a presidential call to action. N Engl J Med. 2016;347(18):1704–1706. doi: 10.1056/NEJMp1601399. [DOI] [PubMed] [Google Scholar]
- 7.Frost NA, Monteiro CE. Administrative segregation in US prisons. Washington, DC: Department of Justice, Office of Justice Programs, National Institute of Justice; 2016. [Google Scholar]
- 8.Grassian S. Psychopathological effects of solitary confinement. Am J Psychiatry. 1983;140:1450–1454. doi: 10.1176/ajp.140.11.1450. [DOI] [PubMed] [Google Scholar]
- 9.Haney C. Mental health issues in long-term solitary and “supermax” confinement. Crime Delinq. 2003;49:124–156. doi: 10.1177/0011128702239239. [DOI] [Google Scholar]
- 10.O’Keefe K, et al. A longitudinal study of administrative segregation. J Am Acad Psychiatry Law. 2013;41(1):49–60. [PubMed] [Google Scholar]
- 11.Kaba F, Lewis A, Glowa-Kollisch S, et al. Solitary confinement and risk of self-harm among jail inmates. Am J Public Health. 2014;104(3):442–447. doi: 10.2105/AJPH.2013.301742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 13.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. doi: 10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- 14.Anderson RE, Geier TJ, Cahill SP. Epidemiological associations between posttraumatic stress disorder and incarceration in the National Survey of American Life. Crim Behav Ment Health. 2015, Wiley Online Library. 26(2): 110–123. [DOI] [PubMed]
- 15.Wang EA, Hong CS, Samuels L, et al. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010;125:171–177. doi: 10.1177/003335491012500205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox AD, Anderson MR, Bartlett G, et al. A description of an urban transitions clinic serving formerly incarcerated people. J Health Care Poor Underserved. 2014;25(1):376–382. doi: 10.1353/hpu.2014.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freedy JR, Steenkamp MM, Magruder KM, et al. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27:615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- 18.Spoont MR, Williams JW, Kehle-Forbes S, Nieuwsma JA, Mann-Wrobel MC, Gross R. Does this patient have posttraumatic stress disorder? Rational clinical examination systematic review. JAMA: Ration Clin Exam. 2015;314(5):501–510. doi: 10.1001/jama.2015.7877. [DOI] [PubMed] [Google Scholar]
- 19.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76(2):272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 20.Hanley J, de Roon-Cassini T, Brasel K. Efficiency of a four-item posttraumatic stress disorder screen in trauma patients. J Trauma Acute Care Surg. 2013;75(4):722–7. doi: 10.1097/TA.0b013e3182a53a5f. [DOI] [PubMed] [Google Scholar]
- 21.Goff A, Rose E, Rose S, Purves D. Does PTSD occur in sentenced prison populations? A systematic literature review. Crim Behav Ment Health. 2007;17:152–162. doi: 10.1002/cbm.653. [DOI] [PubMed] [Google Scholar]
- 22.Andersen HS, Sestoft D, Lillebaek T, Gabrielsen G, Hemmingsen R, Kramp P. A longitudinal study of prisoners on remand: psychiatric prevalence, incidence and psychopathology in solitary vs. non-solitary confinement. Acta Psychiatr Scand. 2000;102:19–25. doi: 10.1034/j.1600-0447.2000.102001019.x. [DOI] [PubMed] [Google Scholar]
- 23.Glowa-Kollisch S, Kaba F, Waters A, Leung YJ, Ford E, Venters H. From punishment to treatment: the “Clinical Alternative to Punitive Segregation” (CAPS) program in New York City jails. Int J Environ Res Public Health. 2016;2:13(2). doi: 10.3390/ijerph13020182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kupers TA. What to do with the survivors? Coping with the long-term effects of isolated confinement. Crim Just Behav. 2008;35:1005–1016. doi: 10.1177/0093854808318591. [DOI] [Google Scholar]