Report of a Case
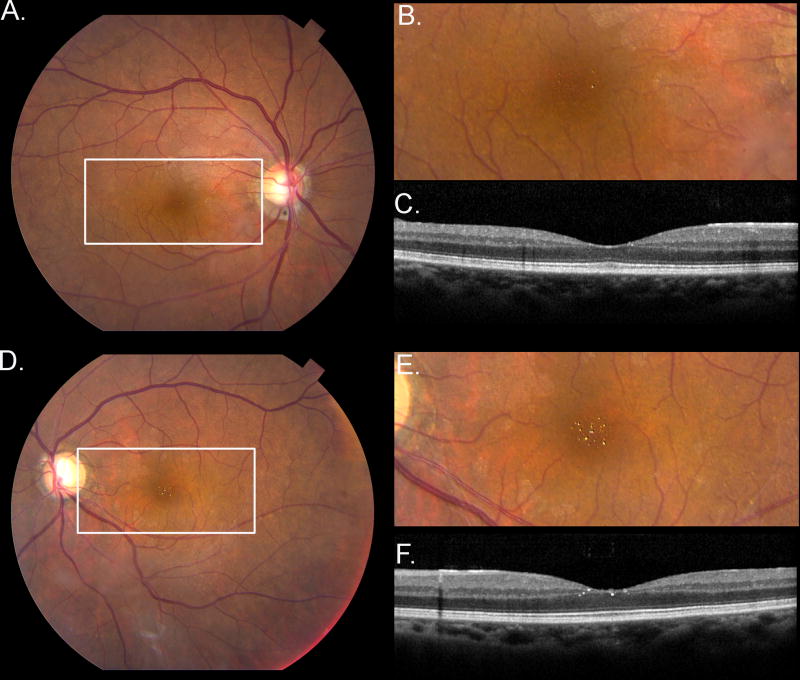
A Filipina woman in her sixties with glaucoma but no macular degeneration was referred to the retina clinic for bilateral “foveal sparkles”. Her ocular, medical, family, and medication histories were non-contributory. She had no visual complaints, and her visual acuity was 20/20 OD and OS with no afferent pupillary defect. Extraocular movements and visual fields by confrontation were full OU. Slit lamp examination of the anterior segment was unremarkable OU. Dilated fundus examination showed bilateral intraretinal round, yellow, glistening deposits in the fovea, and optical coherence tomography (OCT) indicated that these crystals were in the inner layers of the foveal region (Figure 1).
Figure 1. Foveal sparkles related to high dietary lutein and supplement consumption.
Fundus photographs of the right (A) and left (D) eyes showing crystal deposits. Magnified views of the boxed regions (B&E). OCT showing crystals in the inner layers of the right (C) and left (F) foveal regions.
It was noted that for the past 8 years she took a daily 20 mg lutein supplement and 4 g of fish oil and had an unusually high dietary consumption of lutein, which included a broccoli, kale, spinach, and avocado smoothie every morning. We evaluated her carotenoid status through three objective methods. Her total macular pigment levels in both eyes within 9° of eccentricity by Heidelberg Spectralis dual-wavelength autofluorescence imaging1 (30,750 OD, 30,215 OS) were approximately 3.5 times higher than our unsupplemented clinic population (UCP) average (9662±3961). Her skin carotenoid level by resonance Raman spectroscopy2 (110,770 Raman counts) was 2.7 times greater than the UCP average (41,668±14,736). Lastly, her serum lutein level by HPLC (519 ng/mL) was 2.9 times greater than the mean for the UCP (182±196 ng/mL). She agreed to discontinue her lutein supplement but made no other dietary changes.
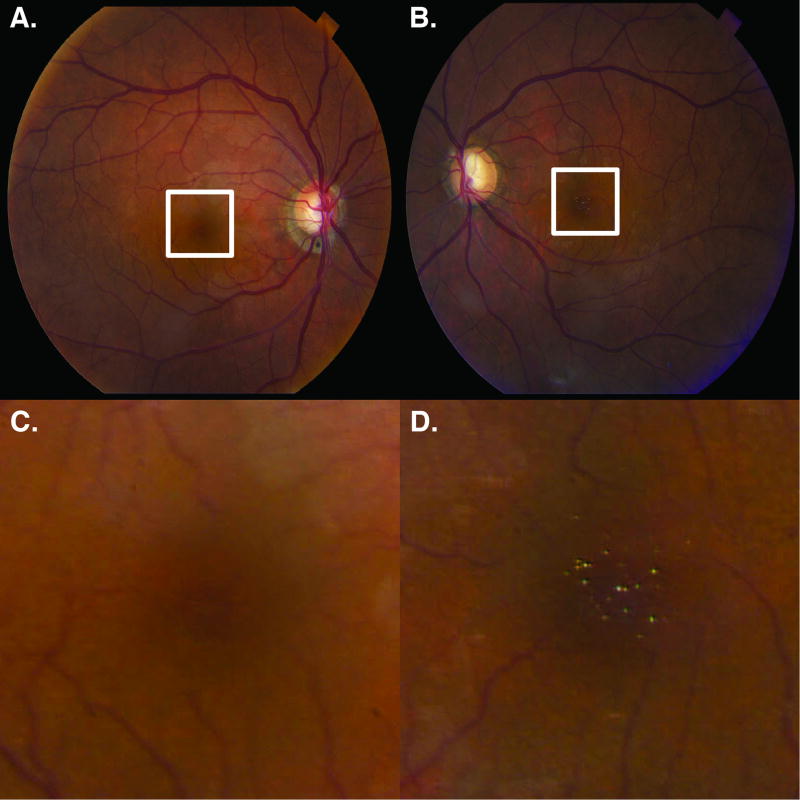
At her 7-month return visit, the crystals in her right eye were resolving; however, crystals were still apparent in the left eye (Figure 2). Her skin carotenoid level dropped substantially (72,798 Raman counts), as well as her macular pigment levels (24,828 OD, 25,245 OS). Serum lutein (191 ng/mL) also decreased to near the population mean.
Figure 2. Partial resolution of foveal sparkles 7 months after stopping lutein supplementation.
Fundus photograph of the right eye (A) of the patient showing resolving foveal crystals 7-months after stopping lutein supplementation. Fundus photograph of the left eye (B) showing persistent crystals. Magnified views of the boxed foveal regions (C&D).
Discussion
Large-scale clinical trials such as AREDS2 have brought attention to the ocular health and functional benefits of lutein, and therefore it is now widely recommended as dietary supplementation for the prevention of visual loss from age-related macular degeneration (AMD).3,4 For these reasons, it is common in ophthalmology practices to come across a large number of patients on lutein supplementation. Unfortunately, the general population often thinks that more is better and may end up consuming much more than the recommended 10 mg of lutein a day,3 at times even without a diagnosis of AMD. Lutein is considered a very safe compound, and there have been no previous reports of toxicity;4 however, we report a case of retinal crystals that were noted in a patient with an unusually high consumption level of supplemental and dietary lutein in which the crystals in one eye were less apparent upon cessation of lutein supplementation.
These findings may represent a crystalline maculopathy in a patient who had an exceedingly high daily ingestion of lutein for 8 years prior to presentation. The crystals, reminiscent of canthaxanthin retinopathy and West African crystalline maculopathy,5,6 were found in the inner layers of the fovea and did not affect her visual acuity or cause other visual symptoms. Upon cessation of her 20 mg lutein supplement, the foveal crystals began to resolve in the right eye, coincident with decreases in her skin carotenoids, serum lutein, and macular pigment levels. Foveal crystals remained in the left eye.
While dietary supplements containing lutein are considered for the prevention of visual loss from AMD, chronic consumption of lutein at levels far exceeding the AREDS2 dose of 10 mg per day is not always better.
Acknowledgments
Drs. Bernstein and Choi had full access to all of the data in the study and take full responsibility for the integrity of the data and the accuracy of the data analysis.
Drs. Bernstein and Choi wrote the manuscript. Dr. Chortkoff initially identified the patient. Dr. Gorusupudi performed the laboratory evaluations. All authors reviewed and approved the manuscript.
Dr. Bernstein and the University of Utah hold a patent on the measurement of carotenoids in retina, skin, and other tissues using resonance Raman spectroscopy.
Dr. Bernstein has received consulting fees and research supplies from Kemin Health, DSM, and Science Based Health in the past 36 months.
This work was supported by NIH grants EY11600 and EY14800, and an unrestricted departmental grant from Research to Prevent Blindness. None of the funders had any involvement in the design and conduct of the study, management, analysis, and interpretation of the data, and preparation, review, or approval of the manuscript.
Footnotes
Conflicts of Interest: Dr. Bernstein and the University of Utah hold a patent on the measurement of carotenoids in retina, skin, and other tissues using resonance Raman spectroscopy.
References
- 1.Akuffo KO, Nolan JM, Stack J, et al. The Impact of Cataract, and Its Surgical Removal, on Measures of Macular Pigment Using the Heidelberg Spectralis HRA+OCT MultiColor Device. Invest Ophthalmol Vis Sci. 2016;57(6):2552–2563. doi: 10.1167/iovs.16-19141. [DOI] [PubMed] [Google Scholar]
- 2.Mayne ST, Cartmel B, Scarmo S, et al. Noninvasive assessment of dermal carotenoids as a biomarker of fruit and vegetable intake. Am J Clin Nutr. 2010;92(4):794–800. doi: 10.3945/ajcn.2010.29707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Age-Related, Eye Disease Study 2 (AREDS2) Research Group. Chew EY, Clemons TE, et al. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: AREDS2 report No. 3. JAMA Ophthalmol. 2014;132(2):142–149. doi: 10.1001/jamaophthalmol.2013.7376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernstein PS, Li B, Vachali PP, et al. Lutein, zeaxanthin, and meso-zeaxanthin: The basic and clinical science underlying carotenoid-based nutritional interventions against ocular disease. Prog Retin Eye Res. 2016:5034–66. doi: 10.1016/j.preteyeres.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espaillat A, Aiello LP, Arrigg PG, Villalobos R, Silver PM, Cavicchi RW. Canthaxanthine retinopathy. Arch Ophthalmol. 1999;117(3):412–413. doi: 10.1001/archopht.117.3.412. [DOI] [PubMed] [Google Scholar]
- 6.Sarraf D, Ceron O, Rasheed K, Drenser KA, Casey R. West African crystalline maculopathy. Arch Ophthalmol. 2003;121(3):338–342. doi: 10.1001/archopht.121.3.338. [DOI] [PubMed] [Google Scholar]