ABSTRACT
Background: Sepsis is a significant cause of mechanical ventilation in hospitalized patients.
Objective: The aim of our study was to recognize the demographic and clinical characteristics associated with an increased need for invasive mechanical ventilation in hospitalized sepsis patients.
Methods: We used National Inpatient Sample database from the years 2009–2011 to identify sepsis patients requiring invasive mechanical ventilation. We compared demographic and clinical characteristics of sepsis patients requiring and not requiring ventilator support and conducted univariate and multivariate analyses to determine odds ratio (OR) of association.
Results: A total of 4,827,769 sepsis patients were identified among which 21.38% required invasive ventilation. Multivariate logistic regression [OR (95% CI), p<0.001] determined the following to be associated with increased odds of ventilator use: morbid obesity [1.37 (1.31–1.42)] and age group 35-64 years [1.18 (1.14–1.22)] compared to 18–34 years, whereas females [0.90 (0.88–0.91)] and age >85 years [0.49 (0.47–0.52)] had reduced odds of invasive ventilation. Hyperkalemia [1.12 (1.09–1.16)] and hypernatremia [2.26 (2.16–2.36)] were associated with increased odds while hypokalemia [0.94 (0.91–0.97)] had reduced odds of invasive ventilation. Septic patients requiring IMV had higher length of stay by 9.72 ± 0.17 days, hospitalization cost by US $ 43010.31 ± 988.24 and in-hospital mortality (41.33% vs 8.91%). Conclusion: Sepsis is a major cause of intensive care unit admission and initiation of invasive ventilation. Baseline demographic and clinical features affect the need for invasive ventilation. A clear understanding of these risk factors is integral for an appropriate and timely management.
KEYWORDS: Sepsis, severe sepsis, invasive mechanical ventilation
1. Introduction
Sepsis is defined as ‘life-threatening organ dysfunction caused by a dysregulated host response to infection’ [1] and is a major cause of increased healthcare cost and in-hospital mortality. The overall incidence is above 240 per 100,000 person-years for sepsis and 51–95 per 100,000 person-years for severe sepsis, in the USA [2]. An observational cohort study showed that over 750,000 cases of sepsis occur each year in the US, with an initiation of mechanical ventilation in over 130,000 cases [3,4].
Recognition of risk factors for increased need of IMV is integral for timely intervention, better patient counselling, and overall patient safety. Factors like male gender, advanced age and morbid obesity have been identified as independent predictors of increased incidence and duration of IMV in patients of various aetiologies, including chronic obstructive pulmonary disease (COPD) and in patients undergoing bariatric surgery [5,6]. The aim of our study is to determine if those previously identified predictors for increased need of IMV would also apply to sepsis.
2. Method
National Inpatient Sample (NIS) database, which is the largest publicly available all-payer inpatient care database in the USA, was used to identify adults (≥18 years) with sepsis and septic shock (ICD-9-CM codes 995.91, 995.92, 038.x, 999.39, 790.7, 785.52) and the use of IMV, including endotracheal tube and tracheostomy (ICD 9-CM Procedure Codes 96.7x, 96.04, 31.1, 31.2x) from 2009 to 2011 (Figure 1). NIS is sponsored by the Agency for Healthcare Research and Quality and contains data on approximately 20% sample of US hospitalizations, the weighted estimate of which represent >95% of the hospitalized US population. Univariate and multivariate analyses was done to determine OR of association of various factors with the utilization of IMV. Two-tailed p ≤ 0.05 was considered statistically significant. STATA version 13.0 (College Station, TX) was used for all analyses.
Figure 1.
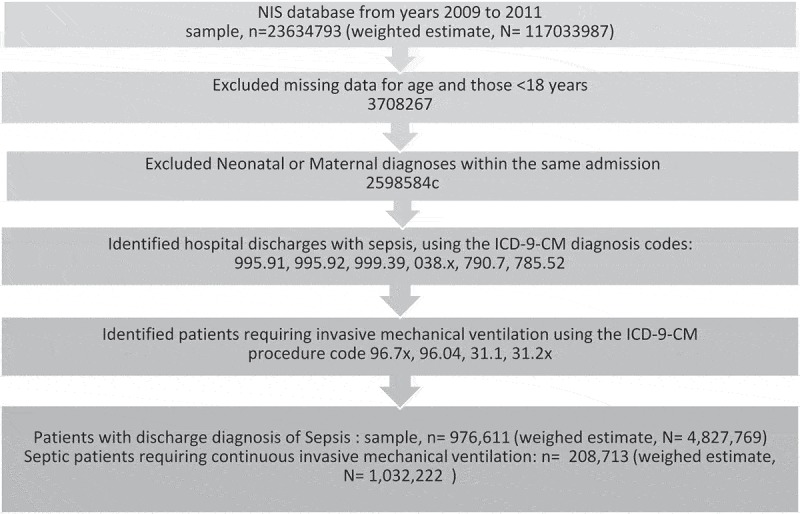
Selection process for discharges included in the analyses.
3. Results
A sample of n = 976,611 [weighted estimate, N = 4,827,769] sepsis patients was identified for 2009–2011. Among them, n = 208,713 [weighted estimate, N = 1,032,222] i.e. 21.38% of sepsis patients were on IMV at some point during their hospital course, compared to 2.65% without sepsis. The mean age of patients requiring MV was 64.66 ± 0.15 years, and more males than females were noted to utilize ventilator support. Septic patients requiring IMV had prolonged length of stay by 9.72 ± 0.17 days, hospitalization cost by US $ 43,010.31 ± 988.24 and in-hospital mortality (41.33 vs. 8.91%). The baseline characteristics and hospitalization outcome of septic patients, as well as the disposition status, in relation to the need for IMV are listed in Table 1.
Table 1.
Comparison of hospitalized sepsis patients requiring or not requiring invasive mechanical ventilation.
| Invasive Mechanical Ventilation (N = 1,032,222 = 21.38%) | No invasive Mechanical Ventilation (N = 3,795,547 = 78.62%) | p value | |
|---|---|---|---|
| Mean age ±SE (years) | 64.66 ± 0.15 | 66.90 ± 0.16 | <0.001 |
| Male (%) | 53.59 | 48.68 | <0.001 |
| Age categories (%) | |||
| 18–34 years | 4.97 | 5.90 | |
| 35–64 years | 42.33 | 35.75 | |
| 65–84 years | 44.60 | 43.27 | |
| >85 years | 8.10 | 15.08 | |
| Mean Charlson comorbidity index ±SE (%) | 2.57 ± 0.02 | 2.33 ± 0.15 | <0.001 |
| Hospitalization Outcomes: | |||
| Mean Length of stay ±SE (days) | 18.73 ± 0.22 | 9.01 ± 0.89 | <0.001 |
| Mean Cost ±SE (US $) | 63,146.57 ± 1268.869 | 20,136.26 ± 344.879 | <0.001 |
| Mortality (%) | 41.33 | 8.91 | <0.001 |
Multivariate logistic regression [OR (95% CI), p < 0.001] determined the following to be independent predictors of increased IMV: Charlson comorbidity index [1.08 (1.06–1.09)], hyperkalaemia [1.12 (1.09–1.16)], hypernatremia [2.26 (2.13–2.16)]. Moreover, compared to 18–34 cohort, the 35–64 cohort was noted to have an increased IMV utilization [1.18 (1.14–1.22)]. Conversely, reduced odds of IMV was noted among females [0.90 (0.88–0.91)] and age group>85 years [0.49 (0.47–0.52)] (Table 2).
Table 2.
Factors associated with use of invasive mechanical ventilation in hospitalized sepsis patients.
| Variable | Univariate analysis (OR, 95% CI) | p value | Multivariate analysis (OR, 95% CI) | p valuea |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age categories (reference: 18–34 years) | ||||
| 35–64 years | 1.40 (1.36–1.45) | <0.001 | 1.18 (1.14–1.22) | <0.001 |
| 65–84 years | 1.22 (1.18–1.27) | <0.001 | 0.95 (0.93–1.02) | 0.403 |
| >85 years | 0.64 (0.61–0.67) | <0.001 | 0.49 (0.47–0.52) | <0.001 |
| Female (ref: Male) | 0.82 (0.81–0.83) | <0.001 | 0.90 (0.88–0.91) | <0.001 |
| Race: (reference: whites) | ||||
| Black | 1.23 (1.17–1.28) | <0.001 | 1.06 (1.01–1.10) | 0.009 |
| Hispanic | 1.15 (1.09–1.22) | <0.001 | 1.08 (1.03–1.15) | 0.004 |
| Others | 1.30 (1.24–1.38) | <0.001 | 1.25 (1.18–1.31) | <0.001 |
| Morbid obesity | 1.28 (1.24–1.31) | <0.001 | 1.37 (1.31–1.42) | <0.001 |
| Charlson comorbidity index | 1.16 (1.14–1.18) | <0.001 | 1.08 (1.06–1.09) | <0.001 |
| Hospital location and teaching status (reference: Rural hospital) | ||||
| Urban non-teaching | 1.78 (1.62–1.95) | <0.001 | 1.56 (1.42–1.71) | <0.001 |
| Urban teaching | 2.34 (2.12–2.57) | <0.001 | 1.86 (1.69–2.04) | <0.001 |
| Electrolyte imbalances: | ||||
| Hyponatremia | 1.23 (1.20–1.26) | <0.001 | 0.98 (0.96–1.004) | 0.10 |
| Hypernatremia | 3.05 (2.94–3.17) | <0.001 | 2.26 (2.16–2.36) | <0.001 |
| Hypokalaemia | 0.94 (0.91–0.97) | <0.001 | 0.94 (0.91–0.97) | <0.001 |
| Hyperkalaemia | 1.72 (1.67–1.77) | <0.001 | 1.12 (1.09–1.16) | <0.001 |
aBold implies significant p values in multivariate analyses.
4. Discussion
Sepsis is known to be an important cause of increased (ICU) admission and in-hospital mortality [3,4], accounting for about 31.28% of IMV requirement [7]. The mean age of sepsis patients in our study was 66.77 ± 0.14 years, similar to that reported in a prior study [8]. Men accounted for more than half of patients receiving mechanical ventilation, as reported previously [9].
Predictors of increased need of IMV in hospitalized patients of various pathologies have been studied. Factors such as morbid obesity (BMI >40 kg/m2), advanced age, and males were associated with prolonged IMV in post cardiac surgery patients [10–12]. Other factors associated with increased incidence of acute lung injury in sepsis include elevated lactate, delayed antibiotics, alcohol abuse, and diabetes mellitus [13,14]. The finding from our study of hospitalized sepsis patients shows similar predictors of IMV, and also helps stratify the risk based on different age groups. A higher Charlson comorbidity index, a widely used index for measuring disease burden, which has been validated by NIS database analyses as a reliable measure of disease burden [15,16], positively correlated with an increased odds of invasive ventilation.
Our data show that 4 intervals of age (35≤, 35–64, 65–84, ≥85 years) have different implications with regards to invasive ventilation in sepsis, even after adjusting for multiple factors. Compared to the age group 18–34 years, patients aged 35–64 years were shown to have higher ventilator utilization, whereas patients ≥85 years had lower odds of being placed on ventilator support. Prior studies suggest that physicians do not readily refer and admit older individuals >80 years to ICU despite a clear indication of the need to do so, and those admitted to the ICU often receive lesser intensive treatment (IMV and renal support), compared to patients <80 years, even after adjusting for illness severity [17,18]. Also, old age being a significant factor influencing the issue of ‘Do not resuscitate or intubate’ order, may result in decreased intensive management, partly explaining for the reduced use of IMV in critically ill elderly patients [19,20].
The strengths of our study include: the availability of baseline demographic characteristics and the utilization of a large database. However, due to its retrospective observational nature, it is not possible to establish causality. Information about the timing of initiation of IMV after admission for sepsis is not known. Plasma levels of electrolytes (Na, K) cannot be determined. This database also does not provide the benefit of follow-up data.
5. Conclusion
In conclusion, hospitalized adults with sepsis have a higher requirement for IMV, which negatively impacts outcome. Furthermore, the probable course of a patient’s stay may be predicted based on certain demographic and clinical features. Identification of such patients can facilitate appropriate and timely intervention.
Funding Statement
None.
Acknowledgements
None.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Danai P, Martin GS.. Epidemiology of sepsis: recent advances. Curr Infect Dis Rep. 2005;7(5):329–334. [DOI] [PubMed] [Google Scholar]
- [3].Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. [DOI] [PubMed] [Google Scholar]
- [4].Morrell MR, Micek ST, Kollef MH. The management of severe sepsis and septic shock. Infect Dis Clin North Am. 2009;23(3):485–501. [DOI] [PubMed] [Google Scholar]
- [5].Gursel G. Determinants of the length of mechanical ventilation in patients with COPD in the intensive care unit. Respiration. 2005;72(1):61–67. [DOI] [PubMed] [Google Scholar]
- [6].Helling TS, Willoughby TL, Maxfield DM, et al. Determinants of the need for intensive care and prolonged mechanical ventilation in patients undergoing bariatric surgery. Obes Surg. 2004;14(8):1036–1041. [DOI] [PubMed] [Google Scholar]
- [7].Chiwhane A, Diwan S. Characteristics, outcome of patients on invasive mechanical ventilation: A single center experience from central India. Egypt J Crit Care Med. 2016;4(3):113–118. [Google Scholar]
- [8].Novosad SA. Vital signs: epidemiology of sepsis: prevalence of health care factors and opportunities for prevention. MMWR Morb Mortal Wkly Rep. 2016;65 DOI: 10.15585/mmwr.mm6533e1 [DOI] [PubMed] [Google Scholar]
- [9].Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–355. [DOI] [PubMed] [Google Scholar]
- [10].Altaani H, Al-Adwan H, Moh’d AF, et al. Predictors of postoperative mechanical ventilation time, length of ICU stay and hospitalization period after cardiac surgery in adults. JRMS. 2015;22(4):31–39. DOI: 10.12816/0018548 [DOI] [Google Scholar]
- [11].Prapas SN, Panagiotopoulos IA, Hamed Abdelsalam A, et al. Predictors of prolonged mechanical ventilation following aorta no-touch off-pump coronary artery bypass surgery. Eur J Cardiothorac Surg. 2007;32(3):488–492. [DOI] [PubMed] [Google Scholar]
- [12].Mehmood A, Kabbani MS, Younus F, et al. Predictors for prolonged mechanical ventilation in children undergoing cardiac surgery. J Saudi Heart Assoc. 2015;27(4):311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Iscimen R, Cartin-Ceba R, Yilmaz M, et al. Risk factors for the development of acute lung injury in patients with septic shock: an observational cohort study*. Crit Care Med. 2008;36(5):1518. [DOI] [PubMed] [Google Scholar]
- [14].Mikkelsen ME, Shah CV, Meyer NJ, et al. The epidemiology of acute respiratory distress syndrome in patients presenting to the emergency department with severe sepsis. Shock Augusta Ga. 2013;40(5):375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mandawat A, Mandawat A, Mandawat MK, et al. Hospitalization rates and in-hospital mortality among centenarians. Arch Intern Med. 2012;172(15):1179–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lee CS, Chien CV, Bidwell JT, et al. Comorbidity profiles and inpatient outcomes during hospitalization for heart failure: an analysis of the U.S. Nationwide inpatient sample. BMC Cardiovasc Disord. 2014;14:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Garrouste-Orgeas M, Boumendil A, Pateron D, et al. Selection of intensive care unit admission criteria for patients aged 80 years and over and compliance of emergency and intensive care unit physicians with the selected criteria: an observational, multicenter, prospective study*. Crit Care Med. 2009;37(11):2919–2928. [DOI] [PubMed] [Google Scholar]
- [18].Boumendil A, Aegerter P, Guidet B, the CUB-Rea Network . Treatment intensity and outcome of patients aged 80 and older in intensive care units: a multicenter matched-Cohort study. J Am Geriatr Soc. 2005;53(1):88–93. DOI: 10.1111/j.1532-5415.2005.53016.x [DOI] [PubMed] [Google Scholar]
- [19].Chang Y, Huang C-F, Lin -C-C. Do-not-resuscitate orders for critically ill patients in intensive care. Nurs Ethics. 2010;17(4):445–455. [DOI] [PubMed] [Google Scholar]
- [20].Salottolo K, Offner PJ, Orlando A, et al. The epidemiology of do-not-resuscitate orders in patients with trauma: a community level one trauma center observational experience. Scand J Trauma Resusc Emerg Med. 2015;23 DOI: 10.1186/s13049-015-0094-2 [DOI] [PMC free article] [PubMed] [Google Scholar]


