Abstract
Since transvaginal hydrolaparoscopy (THL) was introduced as the first‐line procedure in the early stage of the exploration of the tubo‐ovarian structures in infertile women, it has been shown that THL is a less traumatic and a more suitable outpatient procedure than diagnostic laparoscopy. In the present study, a minimally invasive surgery was carried out in infertile women with polycystic ovary syndrome (PCOS) by THL. Ovarian drilling using Nd:YAG laser vaporization by THL was performed in two clomiphen citrate‐resistant infertile women with PCOS. After ovarian drilling with THL, a patient recovered an ovulatory cycle. These findings suggest that ovarian drilling by THL seems to be a safe procedure in infertile women with PCOS. However, further investigations are required to evaluate the effectiveness and risks of this minimally invasive operation. (Reprod Med Biol 2003; 2: 37–40)
Keywords: anovulation, laser vaporization, ovarian drilling, polycystic ovary syndrome, transvaginal hydrolaparoscopy
INTRODUCTION
SINCE TRANSVAGINAL HYDROLAPAROSCOPY (THL) was introduced as the first‐line procedure in the early stage of the exploration of the adnexal structures in infertile women, it has been shown that THL is a less traumatic and a more suitable outpatient procedure than diagnostic laparoscopy. 1 , 2 , 3 , 4 , 5 , 6 Transvaginal access and the systematic use of hydro flotation are potential advantages of THL for the exploration of tubo‐ovarian structures in infertility. The advantages of THL include accurate and atraumatic inspection of adnexal structures without complex manipulation, with the opportunity to perform dye hydrotubation and salpingoscopy. Moreover, inspection under fluid in THL improves the visualization of the distal tubal disease. The risks of a general anesthetic are avoided, and there is less chance of trauma to major vessels.
We have been performing THL as a diagnostic laparoscopy on infertile women based on any of the following four indications: (i) tubal obstruction and/or peritubal adhesion are suggested by the hysterosalpingography (HSG); (ii) serum antibody against Chlamydia trachomatis is positive; (iii) diagnosis of early stage endometriosis; and (iv) unexplained infertility. 3 , 4 , 5 , 6
As the advantages of THL include accurate inspection of adnexal structures without manipulation, THL was not developed as an operative procedure. However, Fernandez et al. 7 have recently reported the feasibility of ovarian drilling by THL.
In the present study, a minimally invasive surgery was carried out in infertile women with polycystic ovary syndrome (PCOS) by THL. Ovarian drilling by THL was performed in two clomiphen citrate‐resistant infertile women with PCOS. Nd:YAG laser vaporization was used to ablate the portions of the ovarian cortex.
PROCEDURE FOR OVARIAN DRILLING BY TRANSVAGINAL HYDROLAPAROSCOPY
THE PROCEDURE OF THL was followed as we previously described. 3 Women with a retroverted uterus were excluded from THL because Darai et al. 8 suggested it should be considered as a relative contra‐indication to THL. Briefly, THL was performed under general anesthesia with Sevofrane (Sevoflurane; Maruishi, Japan) in the lithotomy position. After disinfection, a Hys‐cath (Sumitomo Bakelite Co. Ltd, Tokyo, Japan) was inserted into the uterine cavity for the use of chromotubation. The uterine cervix was lifted with a tenaculum placed on the posterior lip.
Tubo‐ovarian structures and tubal passage were investigated using THL (Circon ACMI, Stamford, CT, USA). The Veress needle was introduced 1.5 cm below the cervix and inserted in the pelvic cavity. Approximately 100 mL saline was instilled in the pouch of Douglas. A 5.5‐mm blunt trocar for operative THL was inserted by a stab incision in the posterior fornix, then a 2.7‐mm diameter semirigid endoscope was used with an optical angle of 30° and a flow channel attached to a 3 CCD digital video camera. The saline irrigation was continued throughout the procedure to keep the bowel and tubo‐ovarian structures afloat. The posterior of the uterus and the tubo‐ovarian structures were carefully observed, and tubal passage using indigocarmin was confirmed.
Ovarian drilling was performed using Nd:YAG laser (Stage MY‐100, Laser Peripherals LLC, MN, USA) to ablate the portions of the ovarian cortex. A sterile quartz glass fiber of 1 mm in core diameter was passed through the operating channel of the laparoscope with a special laser fiber steering device having a deflectable tip. The power used ranged 10 W. The focused laser beam was used from a distance of 1.5–3.0 mm to create approximately 40 holes on the surface of each ovary (Fig. 1).
Figure 1.
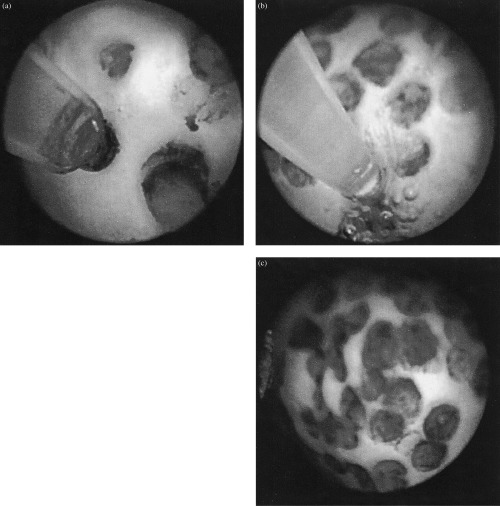
Procedure for ovarian drilling using Nd:YAG laser by transvaginal hydrolaparoscopy (THL). (a, b) Ovarian drilling was performed using Nd:YAG laser to ablate the portions of the ovarian cortex. (c) Final phase of ovarian drilling. The focused laser beam was used to create approximately 40 holes on the surface of each ovary.
CASE REPORTS
Case 1
A 26‐YEAR‐OLD woman, having a normal body mass index (BMI = 18.2 kg/m2), with a half‐year history of primary infertility, visited our hospital for treatment in April 2001. She had been treated with several cycles of unsuccessful ovarian stimulation with clomiphen citrate (up to 150 mg/day for 5 days) by a local gynecologist. Her menarche had been at the age of 14 years and her menstrual cycle was infrequent and irregular. She was not hirsute and an abdomino‐pelvic examination found her to be normal. A laboratory analysis at the early follicular phase yielded the following data: follicle stimulating hormone (FSH) 10.7 mIU/mL (normal, 3.1–23.7 mIU/mL), luteinizing hormone (LH) 14.4 mIU/mL (normal, 0.9–15.5 mIU/mL), prolactin 25.5 ng/mL (normal, 3.2–26.2 ng/mL), testosterone 23.5 ng/dL (normal, 10–60 ng/dL). A transvaginal ultrasound showed ovaries with ‘pearl necklace’ appearance and a normal‐looking endometrium. Thus, the diagnosis of PCOS was confirmed. After a treatment of C. trachomatis for the couple with antibiotics, a successful ovulation was induced with clomiphen citrate (150 mg/day) following withdrawal bleeding by a progesterone treatment. Pregnancy was established in the first treatment cycle. However, a left salpingectomy was performed at 6 weeks of gestation because it was diagnosed as left tubal pregnancy.
After a confirmation of right tubal passage by a HSG, ovulation was induced with clomiphen citrate. However, it was unsuccessful. As she was diagnosed as clomiphen citrate‐resistant, ovarian drilling by THL was proposed.
In April 2002, ovarian drilling using Nd:YAG laser by THL was performed after informed consent was obtained. In this case, the surgical procedure was carried out only for the right ovary because the left tube had been removed. The procedure was completed within 45 mins. A dye test was performed and the right tubal passage was reconfirmed. The Nd:YAG laser was used to ablate the portions of the right ovarian cortex. No complications occurred during or after the operation.
After ovarian drilling by THL, she recovered an ovulatory cycle, followed by anovulatory cycles. Ovulation is now induced with clomiphen citrate.
Case 2
A 30‐year‐old woman, having a body mass index (BMI) of 34.7 kg/m2, with a 3.5‐year history of primary infertility, visited our hospital for treatment in October 2001. Her menarche had been at the age of 13 years and her menstrual cycle was infrequent and irregular. When she was a single 18‐year‐old, with a BMI of 22.0 kg/m2, a diagnosis of PCOS was confirmed in our hospital, based on oligoanovulatory cycles associated with amenorrhea, a ratio of LH to FSH > 1.0, and characteristic appearance of ovaries on ultrasonography.
She was not hirsute and an abdomino‐pelvic examination found her to be normal. Ovulation was induced with clomiphen citrate following withdrawal bleeding by a progesterone treatment. However, she was considered to be a clomiphen citrate‐resistant infertile woman with PCOS.
In April 2002, ovarian drilling by THL was performed after informed consent was obtained. The procedure was completed for bilateral ovaries within 75 mins. A dye test was performed and the tubal passage was bilaterally reconfirmed. The Nd:YAG laser was used to ablate the portions of each ovarian cortex. No complication occurred during or after the operation.
After ovarian drilling with THL, she did not recover an ovulatory cycle. Ovulation is now induced with clomiphen citrate.
DISCUSSION
TREATMENT OF PCOS widely accepted includes induction of ovulation with clomiphen citrate, FSH, and gonadotropin‐releasing hormone analogs; and ovarian drilling by laparoscopy. Infertile women with PCOS have been initially treated with oral antiestrogen medications such as clomiphen citrate. However, approximately 15% of patients with PCOS remain anovulatory despite treatment with it, and half of them with PCOS ovulating on antiestrogen treatment fail to conceive. 9 Gonadotropin stimulation is the next step in the treatment of clomiphen citrate‐resistant infertile women with PCOS. Ovarian surgery has been indicated in women who hyperrespond to gonadotropin therapy to avoid such complications as the ovarian hyperstimulation syndrome (OHSS) or multiple gestations, but postoperative adhesions are another cause of infertility. Postoperative adhesions are more common after laparotomy than after laparoscopy; nonetheless, the cumulative pregnancy rate after ovarian surgery for PCOS is approximately 55%, which is similar to that obtained by medical induction of ovulation. 10 , 11 , 12
Transvaginal hydrolaparoscopy is a less traumatic technique than standard laparoscopy, which can minimize the risks including major vascular injuries 13 and gastrointestinal injuries 14 that occurred even in diagnostic laparoscopy. Our aim was to apply THL for an operative procedure and investigate the feasibility of ovarian drilling by THL. So far, there is only one study that has reported the usefulness of operative THL for the treatment of PCOS by ovarian drilling. 7 In that study, ovarian drilling was performed using bipolar electrosurgery by THL in 13 clomiphen citrate‐resistant anovulatory women with PCOS. Six (46.2%) patients recovered to have regular ovulatory cycles. The cumulative pregnancy rate was 33% at 3 months after THL and 71% at 6 months after THL. No immediate or late operative complications occurred. Based on these experiences, they concluded that THL with ovarian drilling using bipolar electrosurgery appears to be an alternative minimally invasive procedure in patients with PCOS who are resistant to clomiphen therapy.
Although we experienced only two cases in the present study, ovarian drilling using laser vaporization by THL seems to be a safe procedure in infertile women with PCOS. However, further investigations are required to evaluate the effectiveness and risks of this minimally invasive operation.
REFERENCES
- 1. Gordts S, Campo R, Rombauts L, Brosens I. Transvaginal hydrolaparoscopy as an outpatient procedure for infertility investigation. Hum Reprod 1998; 13: 99–103. [DOI] [PubMed] [Google Scholar]
- 2. Campo R, Gordts S, Rombauts L, Brosens I. Diagnostic accuracy of transvaginal hydrolaparoscopy in infertility. Fertil Steril 1999; 6: 1157–1160. [DOI] [PubMed] [Google Scholar]
- 3. Shibahara H, Fujiwara H, Hirano Y et al. Usefulness of transvaginal hydrolaparoscopy in investigating infertile women with Chlamydia trachomatis infection. Hum Reprod 2001; 16: 1690–1693. [DOI] [PubMed] [Google Scholar]
- 4. Shibahara H, Hirano Y, Ayustawati, et al. Chemokine bioactivity of RANTES is elevated in the sera of infertile women with past Chlamydia trachomatis infection. Am J Reprod Immunol, in press. [DOI] [PubMed]
- 5. Shibahara H, Takamizawa S, Hirano Y et al. Relationships between Chlamydia trachomatis antibody titers and tubal pathology assessed using transvaginal hydrolaparoscopy in infertile women. Am J Reprod Immunol, in press. [DOI] [PubMed]
- 6. Fujiwara H, Shibahara H, Hirano Y, Suzuki T, Takamizawa S, Sato I. Usefulness and prognostic value of transvaginal hydrolaparoscopy (THL) in infertile women. Fertil Steril, in press. [DOI] [PubMed]
- 7. Fernandez H, Alby J‐D, Gervaise A, De Tayrac R, Frydman R. Operative transvaginal hydrolaparoscopy for treatment of polycystic ovary syndrome: a new minimally invasive surgery. Fertil Steril 2001; 75: 607–611. [DOI] [PubMed] [Google Scholar]
- 8. Darai E, Dessolle L, Lecuru F, Soriano D. Transvaginal hydrolaparoscopy compared with laparoscopy for the evaluation of infertile women: a prospective comparative blind study. Hum Reprod 2000; 15: 2379–2382. [DOI] [PubMed] [Google Scholar]
- 9. Nugent D, Vandekerckhove P, Hughes E, Arnot M, Lilford R. Gonadotrophin therapy for ovulation induction in subfertility associated with polycystic ovary syndrome. Cochrane Database Syst Rev 2000; 4: CD000410. [DOI] [PubMed] [Google Scholar]
- 10. Donesky BW, Adashi EY. Surgically induced ovulation in the polycystic ovary syndrome: wedge resection revisited in the age of laparoscopy. Fertil Steril 1995; 63: 439–463. [DOI] [PubMed] [Google Scholar]
- 11. Campo S. Ovulatory cycles, pregnancy outcome and complications after surgical treatment of polycystic ovary syndrome. Obstet Gynecol Surv 1998; 53: 297–308. [DOI] [PubMed] [Google Scholar]
- 12. Felemban A, Lin Tan S, Tulandi T. Laparoscopic treatment of polycystic ovaries with insulated needle cautery: a reappraisal. Fertil Steril 2000; 73: 266–269. [DOI] [PubMed] [Google Scholar]
- 13. Chapron C, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg 1997; 185: 461–465. [PubMed] [Google Scholar]
- 14. Chapron C, Pierre F, Harchaoui Y et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod 1999; 14: 333–337. [DOI] [PubMed] [Google Scholar]


