Abstract
Aim : This study was carried out to establish criteria for the elective transfer of two good‐quality embryos to reduce high‐order multiple pregnancy rates. The pregnancy and multiple pregnancy rates per transfer were retrospectively analyzed in 128 in vitro fertilization and embryo transfer (IVF‐ET) cycles.
Results : The analysis revealed that the pregnancy and multiple pregnancy rates were 26.6% (34 of 128) and 23.5% (eight of 34), respectively. Five twin and three triplet pregnancies were included. The pregnancy rates in women 29 years old and younger, 30–34 years, 35–39 years, and 40 years and older were 21.2 (seven of 33), 37.0 (17 of 46), 25.8 (eight of 31), and 11.1% (two of 18), respectively. There was a significant difference of the pregnancy rates between 30 and 34‐year‐old and 40‐year‐old and older women (P < 0.05). The multiple‐pregnancy rate in women 40 years and older was 0%. Three triplet pregnancies were established only in the first attempt of IVF‐ET. The pregnancy rates in women, to whom good‐quality embryos (0–4) were transferred, were 0% (none of 12) for 0, 17.2% (five of 29) for one, 41.2% (seven of 17) for two, 30.8% (12 of 39) for three, and 32.3% (10 of 31) for four and more embryos, respectively. The multiple pregnancy rates in women who had good‐quality embryos of one, two, three, and four and more transferred were 0% (none of five), 23.5% (four of seven), 16.7% (two of 12), and 20.0% (two of 10), respectively.
Conclusion : The criteria for the elective transfer of two good‐quality embryos were established as follows: age < 40 years, a first treatment cycle, and more than three good‐quality embryos available for transfer. After the application of the established criteria, the overall pregnancy and multiple pregnancy rates were 30.4% (14 of 46) and 14.3% (two of 14), respectively, which was satisfactory as compared with those in the 128 IVF‐ET cycles before application of the criteria. An elective transfer of two good‐quality embryos can be highly recommended to avoid high‐order multiple pregnancies in subjects with the established criteria. (Reprod Med Biol 2002; 1: 23–29)
Keywords: elective transfer of two embryos, embryo quality, in vitro fertilization–embryo transfer, multiple pregnancies
Introduction
IT IS ESTIMATED that approximately 1% of babies born per year in Japan result from in vitro fertilization and embryo transfer (IVF‐ET), and other assisted reproductive technologies (ART). In the studies conducted in 1998, the multiple pregnancy rate after IVF‐ET was 20.3%, including 2.3% of triplet or higher‐order multiple pregnancies in Japan. 1 These figures may be lower than that in some other countries because the policy of transferring a maximum three embryos in all IVF‐ET cycles has been accepted in this country. In the World Collaborative Report on In Vitro Fertilization, 2 figures for 1995 show that 24.7% of the pregnancies are twins, 4.1% are triplets and 0.2% are quadruplets. Multiple pregnancies have resulted in a considerable increase in demands for neonatal intensive care facilities and hospital costs. The major risks in a multiple pregnancy include preterm delivery, low birthweight and intrauterine growth restriction. The solution with selective fetal reduction will no doubt raise some medical, ethical and psychosocial dilemmas. 3 , 4 Thus, it is a challenge to avoid multiple pregnancies without compromising pregnancy rates in IVF‐ET.
The pregnancy rate after IVF‐ET is clearly correlated with the number of embryos transferred. It rises steadily with the number of transferred embryos, and reaches a plateau at three replaced embryos. 5 , 6 The need to regulate the number of embryos transferred has been debated; 7 , 8 however, elective transfer of two good‐quality embryos could solve the problem of triplet or higher‐order pregnancies. 9 , 10 , 11
In this study, criteria for the elective transfer of two good‐quality embryos were established. The clinical efficacy was also evaluated by comparing the pregnancy and multiple pregnancy rates before and after application of the criteria.
Materials and methods
Subjects
A TOTAL OF 174 cycles treated with conventional IVF‐ET between May 1995 and September 2000 at the Department of Obstetrics and Gynecology, Jichi Medical School, Japan, was entered into the present study. Severe male‐factor infertile patients treated with the use of intracytoplasmic sperm injection (ICSI) were not included. To establish criteria for the elective transfer of two embryos, pregnancy and multiple pregnancy rates per transfer were retrospectively analyzed in 128 conventional IVF‐ET cycles performed between May 1995 and July 1999. The rates of pregnancy and multiple pregnancy in 12 elective transfer cycles of two good‐quality embryos and 34 transfer cycles of three (at maximum) embryos were compared between August 1999 and September 2000.
Ovarian stimulation and in vitro fertilization protocol and morphological assessment of embryos
The patients were stimulated by using a combination of a gonadotrophin releasing hormone (GnRH) agonist started in the luteal phase (suppression protocol) followed by gonadotrophins as we reported previously. 12 , 13 , 14 On the second day after oocyte retrieval, the morphological assessment of embryos was performed under the inverted microscope using the Veeck’s classification before transfer. 15 Grade 1 embryos with regular blastomeres and no cytoplasmic fragments, and grade 2 embryos with regular blastomeres and minor cytoplasmic fragments were considered good‐quality embryos. Grade 3, 4 and 5 embryos were considered poor‐quality embryos. Clinical pregnancy was diagnosed when the gestational sac was detected under a transvaginal ultrasonography.
Statistical analysis
Statistical analysis of the data was performed by using a chi‐squared analysis and a Student’s t‐test using statview 4.5 (Abacus Concepts, Berkeley, CA, USA) for Macintosh, and P < 0.05 was defined as representing a significant difference.
Results
Pregnancy and multiple pregnancy rates according to a woman’s age
AS SHOWN IN Table 1, 34 clinical pregnancies were established in 128 conventional IVF‐ET cycles performed between May 1995 and July 1999, giving a pregnancy rate of 26.6%. Out of the 34 pregnancies, the multiple pregnancy rate was 23.5% (eight of 34), including five sets of twins and three sets of triplets. The pregnancy rates in women 29 years old and younger, 30–34 years, 35–39 years, and 40 years and older were 21.2% (seven of 33), 37.0% (17 of 46), 25.8% (eight of 31), and 11.1% (two of 18), respectively. There was a significant difference in the pregnancy rate between 30 and 34 years, and 40 years and older (P < 0.05). Multiple pregnancy rates in women 29 years and younger, 30–34 years, 35–39 years, and 40 years and older were 28.% (two of seven), 17.6% (three of 17), 37.5% (three of eight), and 0% (none of two), respectively. There were no significant differences in the multiple pregnancy rates between these four groups.
Table 1.
Pregnancy and multiple pregnancy rates according to the age of women patients
| Patient age (years) | No. ET cycles | No. clinical pregnancies (Pregnancy rate %) | No. multiple pregnancies (Multiple pregnancy rate %) | No. twins | No. triplets |
|---|---|---|---|---|---|
| < 29 | 33 | 7 (21.2) | 2 (28.6) | 2 | 0 |
| 30–34 | 46 | 17 (37.0)* | 3 (17.6) | 0 | 3 |
| 35–39 | 31 | 8 (25.8) | 3 (37.5) | 3 | 0 |
| > 40 | 18 | 2 (11.1)* | 0 (0) | 0 | 0 |
| Total | 128 | 34 (26.6) | 8 (23.5) | 5 | 3 |
P < 0.05.
Pregnancy and multiple pregnancy rates according to the number of attempts
The rates of pregnancy and multiple pregnancy according to the number of attempts were investigated (Table 2). The pregnancy rates in women who attempted IVF‐ET at the first, second, third, and fourth or more times were 26.1% (24 of 92), 25.9% (seven of 27), 42.9% (three of seven), and 0% (none of two), respectively. There were no significant differences between these groups. Multiple pregnancy rates in the first, second, and third attempt were 25.0% (six of 24), 14.3% (one of seven), and 33.3% (one of three), respectively. There were no significant differences in the multiple pregnancy rates between these groups. However, three triplet pregnancies were established only in the first attempt of IVF‐ET.
Table 2.
Pregnancy and multiple pregnancy rates according to the number of attempts
| No. attempts | No. ET cycles | No. clinical pregnancies (Pregnancy rate %) | No. multiple pregnancies (Multiple pregnancy rate %) | No. twins | No. triplets |
|---|---|---|---|---|---|
| 1 | 92 | 24 (26.1) | 6 (25.0) | 3 | 3 |
| 2 | 27 | 7 (25.9) | 1 (14.3) | 1 | 0 |
| 3 | 7 | 3 (42.9) | 1 (33.3) | 1 | 0 |
| ≥ 4 | 2 | 0 (0.0) | 0 (–) | 0 | 0 |
| Total | 128 | 34 (26.6) | 8 (23.5) | 5 | 3 |
Pregnancy and multiple pregnancy rates per transfer according to the number of good‐quality embryos transferred
The rates of pregnancy and multiple pregnancy were calculated according to the number of good‐quality embryos. As shown in Table 3, the pregnancy rates in women, to whom good‐quality embryos (0–4) were transferred, were 0% (none of 12) for none, 17.2% (five of 29) for one, 41.2% (seven of 17) for two, 30.8% (12 of 39) for three, and 32.3% (10 of 31) for four and more, respectively. The pregnancy rate in women who were transferred with no good‐quality embryos was significantly lower than those transferred two, three, and four and more good‐quality embryos (P < 0.05). Multiple pregnancy rates in women who were transferred with one, two, three, and four or more good‐quality embryos were 0% (none of five), 23.5% (four of seven), 16.7% (two of 12), and 20.0% (two of 10), respectively. There were no significant differences in the multiple pregnancy rates between these groups.
Table 3.
Pregnancy and multiple pregnancy rates per transfer according to the number of good‐quality embryos transferred
| No. good‐quality embryos transferred | No. ET cycles | No. clinical pregnancies (Pregnancy rate %) | No. multiple pregnancies (Multiple pregnancy rate %) | No. twins | No. triplets |
|---|---|---|---|---|---|
| 0 | 12 | 0 (0.0)*,†,‡ | 0 (–) | 0 | 0 |
| 1 | 29 | 5 (17.2) | 0 (0.0) | 0 | 0 |
| 2 | 17 | 7 (41.2)* | 4 (23.5) | 2 | 2 |
| 3 | 39 | 12 (30.8)† | 2 (16.7) | 2 | 0 |
| ≥ 4 | 31 | 10 (32.3)‡ | 2 (20.0) | 1 | 1 |
| Total | 128 | 34 (26.6) | 8 (23.5) | 5 | 3 |
P < 0.05.
Establishment of criteria for the elective transfer of two good‐quality embryos
Taken together, criteria for the elective transfer of two embryos were established as follows: age < 40 years old, a first treatment cycle, and more than three embryos available for transfer. By using these criteria, the elective transfer of two good‐quality embryos was performed in 12 cycles, while a three (at maximum) embryo transfer was carried out in 34 cycles between August 1999 and September 2000. As shown in Table 4, there were no differences in women’s ages and the number of eggs collected between these two groups. The number of embryos transferred in three (at maximum) transfer cycles was 2.6 ± 0.7, which was significantly higher than that in the elective transfer of two good‐quality embryos (2.0 ± 0.0; P < 0.05). However, there was a significant difference in the pregnancy rate between the elective two good‐quality embryo transfer cycles (58.3%) and three (at maximum) embryo transfer cycles (20.6%; P < 0.05). Out of 14 clinical pregnancies established in 46 conventional IVF‐ET cycles, a pregnancy rate of 30.4% was found. Out of the 14 pregnancies, the multiple‐pregnancy rate was 14.3% (two of 14). One twin pregnancy was established in an elective two embryo transfer cycle, and one twin pregnancy was established in a three (at maximum) embryo transfer cycle.
Table 4.
Comparison of the data between elective transfer of two good‐quality embryos and three (at maximum) embryo transfers
| Elective transfer of two good quality embryos | Three (at maximum) embryo transfers | Total | |
|---|---|---|---|
| No. cycles | 12 | 34 | 46 |
| Women’s ages | 33.0 ± 4.0 | 36.7 ± 4.9 | 35.7 ± 4.8 |
| No. eggs collected | 9.9 ± 5.0 | 6.5 ± 4.4 | 7.4 ± 4.8 |
| No. embryos transferred | 2.0 ± 0.0* | 2.6 ± 0.7* | 2.4 ± 0.7 |
| No. pregnancy cycles | 7 | 7 | 14 |
| Pregnancy rate/ET (%) | 58.3** | 20.6** | 30.4 |
| No. single pregnancies | 6 | 6 | 12 |
| No. multiple pregnancies | 1 | 1 | 2 |
| Multiple pregnancy rate (%) | 14.3 | 14.3 | 14.3 |
| No. good‐quality embryos frozen | 4.7 ± 4.8*** | 1.3 ± 2.3*** | 2.2 ± 3.4 |
ET, embryo transfer. *,**,***P < 0.05.
As for the number of good‐quality frozen embryos, 4.7 ± 4.8 embryos were frozen in an elective transfer of two good‐quality embryo cycles, while 1.3 ± 2.3 embryos were frozen in three (at maximum) embryo transfer cycles. There was also a significant difference between the two groups (P < 0.05).
Comparison of pregnancy and multiple pregnancy rates before and after application of the criteria for the elective transfer of two good‐quality embryos
Pregnancy and multiple pregnancy rates were compared before and after the application of criteria for the elective transfer of two good‐quality embryos (Fig. 1). Although the pregnancy rate after application of criteria was as high as that before application (30.4 vs 26.6%), the multiple pregnancy rate of the former was lower than the latter (14.3 vs 23.5%). However, there were no significant differences between pregnancy and multiple pregnancy rates between the groups. No high‐order multiple pregnancies were established after the application of criteria.
Figure 1.
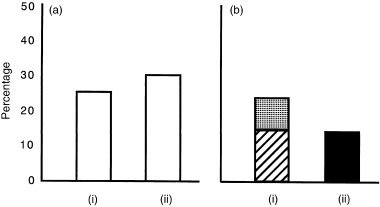
Comparison of (a) pregnancy and (b) multiple pregnancy rates (i) before and (ii) after the application of the criteria for elective transfer of two good‐quality embryos. Although the pregnancy rate after application of the criteria was as high as that before application (30.4 vs 26.6%), the multiple pregnancy rate of the former was lower than the latter (14.3 vs 23.5%). However, there were no significant differences in pregnancy and multiple pregnancy rates between the groups. No high‐order multiple pregnancies were established after the application of the criteria. (▪) Twin – 14.3%, (▨) twin – 14.7%, () triple – 8.8%.
Discussion
TRANSFERRING MORE THAN one embryo to increase the chance of implantation to achieve high pregnancy rates in IVF‐ET is common. The pregnancy rate rises steadily with the number of embryos transferred, and reaches a plateau at three replaced embryos. 5 , 6 However, multiple pregnancy rates are obviously higher when the number of embryos transferred exceeds three. To reduce multiple pregnancy rates, the number of embryos transferred should theoretically be limited to a maximum of two. In this case, however, a significant reduction of the pregnancy rate might occur because of the impaired factors for pregnancy, which includes poor embryo quality 16 and maternal age. 17 The present study demonstrated that the elective transfer of two good‐quality embryos could reduce the incidence of multiple pregnancies without impairing the pregnancy rates.
Since Waterstone and Parsons 18 first reported that there was no significant difference in the pregnancy rates between the elective transfer of two embryos and the transfer of three embryos, other investigators have also shown that the consequences of transferring two embryos prevented triplet pregnancies. 9 , 10 , 11 There are some factors that have been shown to influence multiple pregnancies in IVF‐ET. In the present study, no multiple pregnancy was established in women aged 40 years and older (Table 1). The pregnancy rate in women aged 40 years and older was also significantly lower than that in women aged between 30 and 34 years (P < 0.05; Table 1). These results might support the conclusion by Padilla and Garcia, who demonstrated a highly significant negative linear correlation between age and ongoing pregnancy rate. 17
As for the number of attempts of IVF‐ET, Templeton et al. observed that the live birth rate per ET cycle was highest in the first cycle. 19 In the present study, no significant differences between the pregnancy and multiple pregnancy rates and the number of attempts of IVF‐ET were observed (Table 2). However, three triplet pregnancies were established only in the first attempt of IVF‐ET (Table 2). These results may indicate that careful decision‐making for the number of embryos transferred should be considered, especially in the first attempt of IVF‐ET.
A multiple pregnancy rate is also significantly linked to embryo quality. 16 In the present study, the pregnancy and multiple pregnancy rates reached a plateau at two replaced good‐quality embryos (Table 3). Taken together, the criteria for the elective transfer of two embryos were established as follows: age < 40 years, a first treatment cycle, and more than three embryos available for transfer.
The number of embryos transferred in three (at maximum) transfer cycles was significantly higher than that in the elective transfer of two good‐quality embryos; however, the pregnancy rate in the latter was significantly higher than that in the former (Table 4). These results indicate that the patients who satisfied the criteria are highly related with establishing pregnancies. Moreover, the multiple pregnancy was established in only one case who was transferred with two elective good‐quality embryos. As for the number of good‐quality embryos frozen, significantly higher numbers of embryos were frozen in the elective transfer of two good‐quality embryo cycles than that in three (at maximum) embryo transfer cycles (Table 4). These results indicate that the elective transfer of two good‐quality embryos also increase the number of good‐quality frozen embryos, yielding the maximum chance of pregnancy from the original oocyte collection.
In total, 14 clinical pregnancies were established in 46 conventional IVF‐ET cycles, giving a pregnancy rate of 30.4%. The multiple pregnancy rate was 14.3% (two of 14), including one twin pregnancy in the elective two‐embryo transfer cycle, and one twin pregnancy in a three (at maximum) embryo transfer cycle (Table 4). The pregnancy and multiple pregnancy rates were compared before and after the application of the criteria for the elective transfer of two good‐quality embryos (Fig. 1). In this study period, the pregnancy rate after application of the criteria was as high as that before application (30.4%vs 26.6%). Moreover, the multiple pregnancy rate of the former was remarkably lower than the latter (14.3 vs 23.5%), although there was no significant difference between these two groups. No high‐order multiple pregnancies were established after the application of the criteria.
There are some solutions, except for the elective transfer of two embryos, to avoid multiple pregnancies in IVF‐ET. Natural cycle IVF offers a simpler and less invasive form of IVF than the stimulated cycle IVF, and avoids multiple pregnancies. However, recent investigations of pregnancy rates after IVF in natural cycles are limited, and rates of 5–17.5% of ongoing pregnancy per natural cycles are reported. 20 , 21 , 22 , 23 The solution with selective fetal reduction will no doubt raise some medical, ethical and psychosocial dilemmas. Selective fetal reduction, when carried out by experienced clinicians, still carries a 10% risk of miscarriage. 24 These procedures are not without risks for the newborn. 25
Vilska et al. recently reported that the elective transfer of one good‐quality embryo resulted in an acceptable pregnancy rate, and it eliminated the risk of multiple births, at least in subjects who are younger than 35 years of age. 26 To avoid twin pregnancies after IVF‐ET, selective transfer of one good‐quality embryo might be necessary; however, our group showed that the adverse outcome in twins conceived after artificial reproductive techniques was lower when compared with spontaneously conceived twins. 27 Further studies would be useful to compare the outcome of elective one and two embryo transfers.
Acknowledgments
WE ARE GRATEFUL to Mr Hiromichi Tsunoda and Ms Chieko Yamaguchi (IVF Laboratory, Jichi Medical School, Japan) for their technical assistance.
References
- 1. Japan Society of Obstetrics and Gynecology. International working group for registers on assisted reproduction: 1998. Acta Obst Gynaec Jpn 2001; 1: 670–680. [Google Scholar]
- 2. World Collaborative Report on In vitro Fertilization. Preliminary data for 1995. J Assist Reprod Genet 1997; 14: S251–S265. [Google Scholar]
- 3. Donner C, McGinnis JA, Simon P, Rodesch F. Multifetal pregnancy reduction: a Belgian experience. Eur J Obstet Gynecol Reprod Biol 1991; 38: 183–187. [DOI] [PubMed] [Google Scholar]
- 4. Vauthier‐Brouzes D, Lefebvre P. Selective reduction in multifetal pregnancies: technical and psychological aspects. Fertil Steril 1992; 57: 1012–1016. [PubMed] [Google Scholar]
- 5. Wood C, McMaster R, Rennie G, Trounson A, Leeton J. Factors influencing pregnancy rates following in vitro fertilisation and embryo transfer. Fertil Steril 1985; 43: 245–250. [DOI] [PubMed] [Google Scholar]
- 6. Sharma V, Riddle A, Mason BA, Pampiglione J, Cambell S. An analysis of factors influencing the establishment of a clinical pregnancy in an ultrasound‐based ambulatory in vitro fertilization program. Fertil Steril 1988; 49: 468–478. [DOI] [PubMed] [Google Scholar]
- 7. Alikani M, Wiemer K. Embryo number of transfer should not be strictly regulated. Fertil Steril 1997; 68: 782–783. [DOI] [PubMed] [Google Scholar]
- 8. De Jonge CJ, Wolf DP. Embryo number for transfer should be regulated. Fertil Steril 1997; 68: 784–786. [DOI] [PubMed] [Google Scholar]
- 9. Nijs M, Geerts L, Van Roosendaal E, Segal‐Bertin G, Vanderzwalmen P, Schoysman R. Prevention of multiple pregnancies in an in vitro fertilization program. Fertil Steril 1993; 59: 1245–1250. [DOI] [PubMed] [Google Scholar]
- 10. Matson PL, Browne J, Deakin R, Bellinge B. The transfer of two embryos instead of three to reduce the risk of multiple pregnancy: a retrospective analysis. J Assist Reprod Genet 1999; 16: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Devreker F, Emiliani S, Revelard P, Van den Bergh M, Govaerts I, Englert Y. Comparison of two elective transfer policies of two embryos to reduce multiple pregnancies without impairing pregnancy rates. Hum Reprod 1999; 14: 83–89. [DOI] [PubMed] [Google Scholar]
- 12. Shibahara H, Mitsuo M, Ikeda Y, Shigeta M, Koyama K. Effects of sperm immobilizing antibodies on pregnancy outcome in infertile women treated with IVF‐ET. Am J Reprod Immunol 1996; 36: 96–100. [DOI] [PubMed] [Google Scholar]
- 13. Shibahara H, Funabiki M, Shiotani T, Ikeda Y, Koyama K. A case of primary ovarian pregnancy after in‐vitro fertilization and embryo transfer. J Assist Reprod Genet 1997a; 14: 63–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shibahara H, Naito S, Hasegawa A, Mitsuo M, Shigeta M, Koyama K. Evaluation of sperm fertilizing ability using the Sperm Quality Analyzer. Int J Androl 1997b; 20: 112–117. [DOI] [PubMed] [Google Scholar]
- 15. Veeck LL. Oocyte assessment and biological performance. Ann NY Acad Sci, 1998; 541: 259–274 . [DOI] [PubMed] [Google Scholar]
- 16. Staessen C, Camus M. The relationship between embryo quality and the occurrence of multiple pregnancy. Fertil Steril 1992; 57: 626–630. [PubMed] [Google Scholar]
- 17. Padilla S, Garcia J. Effect of maternal age and number of in vitro fertilization procedures on pregnancy outcome. Fertil Steril 1989; 52: 270–273. [DOI] [PubMed] [Google Scholar]
- 18. Waterstone J, Parsons J. Elective transfer of two embryos. Lancet 1991; 337: 975–976. [DOI] [PubMed] [Google Scholar]
- 19. Templeton A, Morris J, Parslow W. Factors that affect outcome of in vitro fertilization treatment. Lancet 1996; 348: 1402–1406. [DOI] [PubMed] [Google Scholar]
- 20. Foulot H, Ranoux C, Dubuisson JB, Rambaud D, Aubriot FX, Poirot C. In vitro fertilization without ovarian stimulation; a simplified protocol applied in 80 cycles. Fertil Steril 1989; 52: 617–621. [DOI] [PubMed] [Google Scholar]
- 21. Lenton E. Natural cycle versus stimulated cycle IVF. J Assist Reprod Genet 1993; 10: 406–408. [DOI] [PubMed] [Google Scholar]
- 22. Claman P, Domingo M, Garner P, Leader A, Spence JE. Natural cycle in vitro fertilization‐embryo transfer at the University of Ottawa: an inefficient therapy for tubal infertility. Fertil Steril 1993; 60: 298–302. [DOI] [PubMed] [Google Scholar]
- 23. Fahy M, Cahill D, Wardle PG, Hull MG. In vitro fertilization in completely natural cycles. Hum Reprod 1995; 10: 572–575. [DOI] [PubMed] [Google Scholar]
- 24. Evans MI, Kramer RL, Yaron Y, Drugan A, Johnson MP. What are the ethical and technical problems associated with multifetal pregnancy reduction? Clin Obstet Gynecol 1998; 41: 46–54. [DOI] [PubMed] [Google Scholar]
- 25. Geva E, Lerner‐Geva L, Stavorovsky Z et al. Multifetal pregnancy reduction: a possible risk factor for periventricular leukomalacia in premature newborns. Fertil Steril 1998; 69: 845–850. [DOI] [PubMed] [Google Scholar]
- 26. Vilska S, Tiitinen A, Hyden‐Granskog C, Hovatta O. Elective transfer of one embryo results in an acceptable pregnancy rate and eliminates the risk of multiple birth. Hum Reprod 1999; 14: 2392–2395. [DOI] [PubMed] [Google Scholar]
- 27. Minakami H, Sayama M, Honma Y et al. Lower risks of adverse outcome in twins conceived by artificial reproductive techniques compared with spontaneously conceived twins. Hum Reprod 1998; 13: 2005–2008. [DOI] [PubMed] [Google Scholar]


