Abstract
Aims: It is well documented that maternal morbidity and neonatal morbidity and mortality increase alike in high‐order multiple (HOM) births. There have, however, been few reports concerning the costs of maternal and neonatal medical care associated with HOM births. This is the first such report on the situation in Japan.
Materials and methods: All triplet and quadruplet pregnancies managed at this institution from before 16 weeks’ gestation, and delivered at no earlier than 22 weeks’ gestation, between 1997 and 2002 were included. Prophylactic cervical ligature, hospitalization to prevent premature labor from 23 weeks’ gestation until delivery, and delivery by cesarean section, were all routine for HOM pregnancies. All women with singleton and twin pregnancies, who underwent in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) and also delivered their babies at no earlier than 22 weeks’ gestation at this institution, between 1997 and 2002, were also examined as controls. Prophylactic cervical ligature, preventive hospitalization, and cesarean section were not routine in the control group.
Results: The average gestational ages at delivery in singleton (n = 58), twin (n = 21), triplet (n = 14) and quadruplet (n = 1) pregnancies, were 39.4, 35.6, 31.9 and 25.1 weeks, respectively (P < 0.001 by anova). Birthweights were 2886 ± 425 g, 2117 ± 623 g, 1430 ± 373 g, and 633 ± 77 g (mean ± SD), respectively (P < 0.001). The average inpatient medical care cost for mother and child(ren), from maternal admissions after 12 weeks’ gestation to the discharge of all family members from hospital, was ¥703 279 yen (∼US$5861), ¥4 903 270 (∼US$40 861), ¥11 810 327 (∼US$98 419), and ¥44 961 000 (∼US$374 675), respectively (P < 0.001).
Conclusion: The present study outlined the high costs of medical care for HOM pregnancies. Not only from a medical viewpoint, but also from the viewpoint of medical costs, it is important to avoid HOM pregnancies as a result of infertility treatment. (Reprod Med Biol 2004; 3: 159–164)
Keywords: maternal, medical care costs, neonatal, quadruplet, triplet
INTRODUCTION
HIGH‐ORDER MULTIPLE (HOM) births (triplets or more), have increased in frequency during the last 10–20 years, with advances in infertility treatment using human menopausal gonadotropins (hMG) and in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI). In Japan, the proportion of HOM births has increased from 100 per 1 million live births in 1985 to 260–280 per 1 million live births in the late 1990s. 1
It is well known that maternal morbidity and neonatal mortality and morbidity increase alike in HOM births. For triplet pregnancies, reported maternal complications include premature labor (76–92%); preterm premature rupture of membranes (15–20%); pre‐eclampsia (24–39%); hemolysis, elevated liver enzymes, and low platelets syndrome (HELLP) (8–10%); and post‐partum hemorrhage (8–12%). 2 , 3 , 4 For neonates, perinatal mortality is approximately 100–110/1000, three‐quarters of which are neonatal deaths. 5 , 6
The high costs of medical care associated with HOM are also a problem. Although medical complications associated with HOM have been well documented, there have so far been few reports concerning the medico‐economical issues. Callahan et al. reported the average inpatient costs per family in 1986–1991 for singleton, twin, and triplet deliveries were US$9845, US$37 947, and US$109 765, respectively. 7 Chelmow et al. reported that the average perinatal cost per family in 1992–1993 for triplets was US$64 347. 8 Our search of the literature revealed no reports on this subject emanating from Japan. In the present study, we investigated the costs of medical care for triplet and quadruplet pregnancies.
MATERIALS AND METHODS
Subjects
ALL TRIPLET AND quadruplet pregnancies (HOM group) managed between 1997 and 2002 were included. Patients referred to this institution at or after 16 weeks’ gestation, or delivered before 22 weeks’ gestation, were excluded. There were 14 triplet and one quadruplet pregnancies. Of the 14 triplet pregnancies, one was a spontaneous pregnancy, four followed hMG treatment, and nine were after IVF/ICSI. The quadruplet pregnancy followed hMG treatment.
All women with singleton and twin pregnancies (control group), who underwent IVF/ICSI and also delivered at no earlier than 22 weeks at this institution, from 1997 to 2002, were also investigated. There were 58 singleton and 21 twin pregnancies.
Chorionicity
In the examined multiples, two sets of triplets were 2‐chorionic‐3‐amnionic. The other multiples did not contain monochorionic fetuses. No cases of feto‐fetal transfusion syndrome were detected in the present study.
Antenatal management
All subjects in the HOM group underwent prophylactic cervical ligature at approximately 15 weeks’ gestation, and were hospitalized from approximately 23 weeks’ gestation until delivery. During this admission, all subjects were administered oral ritodrine. Subjects were not strictly confined to bed, and were allowed to move freely about the hospital, but in practice they spent most of the day in bed. Cervical length was determined by vaginal ultrasonography at intervals of 7–14 days. Subjects with a shortened cervical canal of 20 mm or less, and/or uterine contractions occurring at a rate of 10 per hour or more, were commenced on intravenous ritodrine. Where appropriate, and in addition to complete bed rest, intravenous magnesium sulfate, urinastatin suppositories 9 or indomethacin suppositories were prescribed. Informed consent was obtained before indomethacin was administered. Delivery was by cesarean section for all the HOM group, as an elective procedure at or after 32 weeks’ gestation. This policy is based on evidence that the optimal gestational age for triplets is 32–37 weeks. 5
Prophylactic cervical ligature and preventive hospitalization were not routine in the control group. Normal vaginal delivery route was the norm. The cesarean rates in singleton and twin pregnancies were 7/58 (12.1%) and 11/21 (52.4%), respectively. The management of subjects with a shortened cervix and/or preterm labor was the same as for the HOM group.
Medical care costs
The billing records of all mothers and neonates were examined. Data was collated for maternal admissions after 12 weeks gestation until discharge, and from birth (admission) until discharge for neonates. Costs of infertility treatment, outpatient antenatal management, food, and single‐room charges were excluded.
Calculations were made on the basis of an exchange rate in 2003 of US$1 equal to approximately ¥120.
Statistics
Data are given as mean ± SD. Inter‐group comparisons were made using anova, and P < 0.05 was regarded as significant. Correlations were examined using simple regression analysis and F > 4 was regarded as significant.
RESULTS
Gestational age at delivery, length of hospital stay, and costs of medical care for each group
FOR EACH GROUP, gestational ages at delivery, lengths of maternal hospital stay, costs of maternal medical care, birthweights, lengths of neonatal hospital stay, costs of neonatal medical care, and the total costs of medical care for the family are shown in Table 1. Both maternal and neonatal costs were highest for the quadruplet pregnancy, and lowest in the singleton pregnancies (P < 0.001).
Table 1.
Comparison of medical care costs between singleton, twin, triplet, and quadruplet pregnancies
| Control group | High‐order multiple group | Comparison using anova P‐value | |||
|---|---|---|---|---|---|
| Singleton (n = 58) | Twin (n = 21) | Triplet (n = 14) | Quadruplet (n = 1) | ||
| Gestational age at delivery (weeks) | 39.4 ± 1.7 | 35.6 ± 4.1 | 31.9 ± 2.6 | 25.1 | <0.001 |
| Length of maternal hospital stay (days) | 18.3 ± 21.5 | 46.1 ± 33.8 | 102.2 ± 33.2 | 108 | <0.001 |
| Maternal costs (× 1000 yen) | 530 ± 467 | 1124 ± 709 | 2070 ± 525 | 3522 | <0.001 |
| Birthweight (g) | 2886 ± 425 | 2117 ± 623 | 1430 ± 373 | 633 ± 77 | <0.001 |
| Length of neonatal hospital stay (days) | 9.0 ± 4.6 | 30.9 ± 38.1 | 52.9 ± 29.9 | 133 | <0.001 |
| Cost per neonate (× 1000 yen) | 173 ± 410 | 1889 ± 3061 | 3247 ± 2350 | 10 360 ± 85 | <0.001 |
| Total family cost (× 1000 yen) | 703 ± 680 | 4903 ± 6199 | 11810 ± 4869 | 44 961 | <0.001 |
In the HOM group, the ratio of the cost of neonatal medical care to the total family cost medical care was on average 80.1%, indicating that neonatal care accounts for the great majority of the cost of medical care in HOM births.
Factors influencing the cost for the HOM neonates
We examined the factors influencing the cost of neonatal medical care in the HOM group. First we examined these factors in all triplet neonates (n = 42) and the quadruplet neonates (n = 4). The cost of neonatal care was greatest when the gestational age at delivery was smallest (F = 42.6, Fig. 1a). Similarly, the cost of neonatal care was greatest when the birthweight was smallest (F = 48.6, Fig. 1b).
Figure 1.
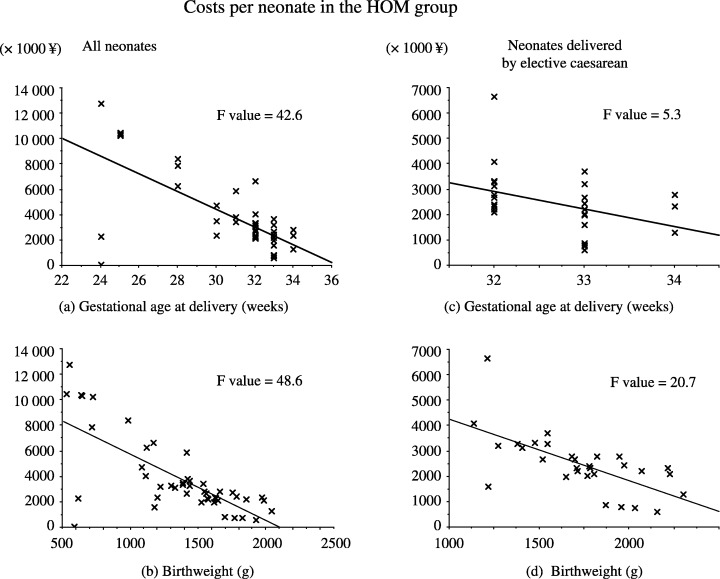
The relationship between gestational age at delivery or birthweight and the costs of neonatal medical care. For all high‐order multiple (HOM) neonates, both (a) gestational age at delivery and (b) birthweight correlated negatively with the neonatal medical care costs were calculated. A similar relationship was also seen in triplet neonates delivered by elective cesarean section between 32 and 34 weeks (c, d).
We then examined the factors influencing the costs of neonatal medical care in the 30 triplets who were delivered by elective cesarean section between 32 and 34 weeks’ gestation. The cost of neonatal care was greatest when the gestational age at delivery was smallest (F = 5.3, Fig. 1c). Similarly, the cost of neonatal care was greatest when the birthweight was smallest (F = 20.7, Fig. 1d). The cost of care for neonates delivered at 34 weeks was less than for those delivered at 32 weeks.
DISCUSSION
IN THE CURRENT report, we present for the first time in Japan the costs of medical care for HOM births. In Table 2, we compare our results with reports from the USA. 7 , 8 The average length of maternal hospital stay was 14.1 and 16.8 days in the USA studies, and 102.6 days in the present study. The average cost of maternal care was $15 379 and $20 067 in the USA studies, and $18 057 (converted from yen, as below) in the present study. The length of maternal hospital stay was considerably longer in the current study than in the USA studies, while the costs of maternal care were similar for the two countries. This is probably because the inpatient cost per day is much higher in the USA than in Japan. We will discuss the significance of preventive maternal admission later. The average length of neonatal hospital stay was 10.0 and 13.5 days in the USA studies, and 60.0 days in the present study. The average cost of neonatal care was $13 650 and $31 462 in the USA studies, and $32 211 in the present study. In the USA, neonates who do not require intensive care are transferred to local hospitals, whereas at this institution neonates are not discharged unless they exceed 2300 g in weight. Lengths of neonatal hospital stay and costs of neonatal care cannot therefore be directly compared. In our estimation, the total costs of neonatal, for both intensive care and non‐intensive care, are similar between the USA and Japan.
Table 2.
Comparison of our data with other reports
| Callahan et al. | Chelmow et al. | Present study† | |
|---|---|---|---|
| Subjects | |||
| Number of fetuses | ≥3 | 3 | ≥3 |
| Gestational age at delivery | ≥20 weeks | ≥20 weeks | >22 weeks |
| Study period | 1986–1991 | 1992–1993 | 1997–2002 |
| Calculated costs | Inpatient costs | Perinatal costs (outpatient costs included) | Inpatient costs |
| Mothers | n = 85 | n = 20 | n = 15 |
| Number of stillbirths | Not stated | n = 2 (10%) | n = 0 |
| Number of transfers | Not stated | n = 4 (20%) | n = 0 |
| Caesarean delivery | 86% | 80% | 100% |
| Mean length of hospital stay | 14.1 days | 16.8 days | 102.6 days |
| Mean cost | $15 379 | $20 067 | $18 057 |
| Neonates | n = 218 | n = 54 | n = 46 |
| Mean gestational age at delivery | Not stated | 30.7 weeks | 31.4 weeks |
| Mean length of hospital stay | 10.0 days | 13.5 days | 60.0 days |
| Mean cost per neonate | $31 462 | $13 650 | $32 211 |
| Mean total family cost (US$) | |||
| Triplets and quadruplets | $109 765 | No data | $116 836 |
| Triplets only | Not stated | $64 347 | $98 419 |
120 yen is converted to $US1.00.
In the current study, we demonstrated that the costs of both maternal and neonatal medical care were much higher in the HOM group than in the control group. The average total family costs in singleton, twin, triplet and quadruplet pregnancies were ¥703 279, ¥4 903 270, ¥11 810 327, and ¥44 961 000, respectively. When these are divided by the number of children, they are ¥703 279, ¥2 451 635, ¥3 936 776, and ¥11 240 250, respectively. The perinatal and neonatal costs of medical care for one baby is 3.5 times, 5.6 times, and 16 times in twin, triplet, and quadruplet pregnancies, respectively, than that for a singleton pregnancy. The majority of HOM pregnancies are now the result of modern infertility treatments. The risks to mother and baby are higher in HOM pregnancies, and the costs of medical care are also high. From both a medical viewpoint and from the viewpoint of medical costs, the importance of avoiding HOM as a result of infertility treatments is evident.
Is it possible to reduce the costs of medical care for HOM pregnancies without adversely affecting maternal and neonatal outcomes? In this context, we will discuss the following three issues: (i) prophylactic cervical ligature; (ii) preventive hospitalization; and (iii) the timing of elective cesarean section.
First, is it possible to eliminate the maternal cost associated with prophylactic cervical ligature? There are no reports of randomized controlled trials with large subject numbers, although several reports have demonstrated that prophylactic cervical ligature does not affect the gestational age at delivery of triplets. 10 , 11 The average cost for prophylactic cervical ligature, with a hospital stay of 2 weeks, was approximately ¥350 000 at this institution. If in the future it is definitively shown that prophylactic cervical ligature is not effective in preventing premature delivery in triplets, this cost can be eliminated without affecting medical outcomes.
Second, can the maternal costs of routine hospitalization be reduced? According to the review by Newman and Luke, most obstetricians recommend that women pregnant with triplets stop work and have bed rest at home after 20 weeks’ gestation, but the effectiveness of routine hospitalization remains controversial. 5 Several authors report that routine hospitalization does not have a significant effect on the gestational age at delivery, 3 , 12 , 13 while others report that it is helpful to prolong the pregnancy. 14 , 15 Another question is: at what stage of gestation should women be hospitalized? In the reports indicating that preventive hospitalization is helpful in prolonging the pregnancy, 14 , 15 hospitalization is from approximately 28 weeks’ gestation, whereas at this institution preventive hospitalization begins at 23 weeks. In the present study, the average inpatient cost for subjects administered oral ritodrine only was approximately ¥100 000 per week. If hospitalization after 28 weeks’ gestation is effective in preventing premature delivery, it should commence at 28 weeks, not at 23 weeks, resulting in a saving of approximately ¥500 000.
Of interest to this discussion, Adams et al. compared inpatient and outpatient management strategies, demonstrating that pre‐eclampsia and neonatal intraventricular hemorrhage were significantly lower in the hospitalization group (8.8 vs 31%, 0.9 vs 10.4%, respectively). 16 In the present study, no cases of pre‐eclampsia and HELLP were detected, although the reported frequencies are 24–39% and 8–10%, respectively. 2 , 3 , 4 In addition, we detected no cases of neonatal intraventricular hemorrhage. These results are in accordance with the observation of Adams et al. that hospital admission reduces pre‐eclampsia. Even if preventive hospitalization does not have a significant effect on gestational age at delivery, if it reduces pre‐eclampsia we should not discontinue preventive hospitalization. Further investigation of this topic, with data from more subjects, is needed to determine the impact of preventive hospitalization.
Third, can the costs of neonatal care be reduced? Our policy has been to perform elective cesarean section after 32 weeks gestation, based on a report that the optimal gestational age for triplets is 32–37 weeks 5 and in practice this procedure is performed at 32–34 weeks. A more recent report, however, indicates the best timing is at 34–35 weeks’ gestation. 17 Analysis of our data of elective cesarean deliveries between 32 and 34 weeks also showed that earlier gestational ages result in higher costs of neonatal care. Although a quantitative estimation is difficult, our best guess is that the decrease in costs for three neonates would overcome the increase in the maternal cost caused by elongation of the length of maternal hospital stay by 2–3 weeks. If there are no problems on either the maternal or fetal side, delivery by elective cesarean section should be performed at 34–35 weeks, not at 32–34 weeks, from both the medical and economical viewpoints. At this institution, we will henceforth perform elective cesarean sections for triplets at 34–35 weeks.
In conclusion, the total costs of maternal and neonatal care for HOM births can be reduced to some extent by discontinuation of routine cervical ligatures, delaying preventive maternal hospitalization, and performing elective cesarean section at 34–35 weeks’ gestation. Major savings would appear difficult, however, as the average total family cost for triplets in the present study was ¥11 810 327.
In Japan, most of the costs of maternal and neonatal medical care are covered by public institutions, the health insurance unions and the regional governments, except in the case of normal vaginal delivery at term. Maternal costs are covered 70% by the health insurance union, and the remaining 30% are charged to the patient. When the charge to the patient exceeds a certain level (some ¥73 000 a month for a family with average earnings), the health insurance union covers the excess. Costs for premature babies are covered 80% by the health insurance union, and the remaining 20% by the regional government. No medical costs for premature babies are charged to the family. The high costs of medical care associated with HOM are therefore a considerable financial burden on health insurance unions and regional governments.
Advances in prenatal and neonatal care have improved maternal and neonatal outcomes in HOM births, but neonatal mortality and morbidity are still high. The high risks and high costs of HOM births underline the importance of avoiding HOM associated with infertility treatment.
ACKNOWLEDGMENTS
THE AUTHORS WOULD like to thank Dr Shinichi Watabe in the Department of Pediatrics, and Dr Masaki Ise and Mr Yasuharu Nishide in the Department of Rehabilitation of Kurashiki Central Hospital. Our thanks also go to Mrs Mariko Murakami for her assistance in the calculation of the costs of medical care.
REFERENCES
- 1. Aono T. Seishoku iryou no shinpo to tatai (Advances in reproductive medicine and multiple pregnancy). Sanka Fujinka 2003; 70: 143–149 (in Japanese). [Google Scholar]
- 2. Seoud MAF, Toner JP, Kruithoff C, Muasher SJ. Outcome of twin, triplet, and quadruplet in vitro fertilization pregnancies: the Norfolk experience. Fertil Steril 1992; 57: 825–834. [PubMed] [Google Scholar]
- 3. Albrecht JL, Tomich PG. The maternal and neonatal outcome of triplet gestations. Am J Obstet Gynecol 1996; 174: 1551–1556. [DOI] [PubMed] [Google Scholar]
- 4. Malone FD, Kaufman GE, Chelmow D, Athanassoiu A, Nores JA, D’Alton ME. Maternal morbidity associated with triplet pregnancy. Am J Perinatol 1998; 15: 73–77. [DOI] [PubMed] [Google Scholar]
- 5. Newman RB, Luke B. Management of triplet and other high order multiples In: Newman RB, Luke B. (eds). Multifetal Pregnancy. Philadelphia: Lippincott, Williams & Wilkins, 2000; 192–219. [Google Scholar]
- 6. Blickstein I, Keith LG. Outcome of triplets and high‐order multiple pregnancies. Curr Opin Obstet Gynecol 2003; 15: 113–117. [DOI] [PubMed] [Google Scholar]
- 7. Callahan TL, Hall JE, Ettner SL, Christiansen CL, Greene MF, Crowley WF. The economic impact of multiple‐gestation pregnancies and the contribution of assisted‐reproduction techniques to their incidence. N Engl J Med 1994; 331: 244–249. [DOI] [PubMed] [Google Scholar]
- 8. Chelmow D, Penzias AS, Kaufmann G, Cetrulo C. Costs of triplet pregnancy. Am J Obstet Gynecol 1995; 172: 677–682. [DOI] [PubMed] [Google Scholar]
- 9. Kanayama N, El Maradny E, Halim A et al. Urinary trypsin inhibitor prevents uterine muscle contraction by inhibition of Ca++ influx. Am J Obstet Gynecol 1995; 173: 192–199. [DOI] [PubMed] [Google Scholar]
- 10. Mordel N, Zajicek G, Benshushan A, Schenker JG, Laufer N, Sadovsky E. Elective suture of the uterine cervix in triplets. Am J Perinatol 1993; 10: 14–16. [DOI] [PubMed] [Google Scholar]
- 11. Strauss A, Heer IM, Janssen U, Dannecker C, Hillemanns P, Muller‐Egloff S. Routine cervical cervical ligature in higher order multiple gestation – does it prolong the pregnancy? Twin Res 2002; 5: 67–70. [DOI] [PubMed] [Google Scholar]
- 12. Newman RB, Hamer C, Miller MC. Outpatient triplet management: a contemporary review. Am J Obstet Gynecol 1989; 161: 547–555. [DOI] [PubMed] [Google Scholar]
- 13. Peaceman AM, Dooley SL, Tamura RK, Socol ML. Antepartum management of triplet gestations. Am J Obstet Gynecol 1992; 167: 1117–1120. [DOI] [PubMed] [Google Scholar]
- 14. Holcberg G, Biale Y, Lewenthal H, Insler V. Outcome of pregnancy in 31 triplet gestations. Obstet Gynecol 1982; 59: 472–476. [PubMed] [Google Scholar]
- 15. Skrablin S, Kuvacic I, Jukic P, Kalafatic D, Peter B. Hospitalization vs. outpatient care in the management of triplet gestations. Int J Gynaecol Obstet 2002; 77: 223–229. [DOI] [PubMed] [Google Scholar]
- 16. Adams DM, Sholl JS, Haney EI, Russell TL, Silver RK. Perinatal outcome associated with outpatient management of triplet pregnancy. Am J Obstet Gynecol 1998; 178: 843–847. [PubMed] [Google Scholar]
- 17. Kahn B, Lumey LH, Zybert PA et al. Prospective risk of fetal death in singleton, twin, and triplet gestations: implications for practice. Obstet Gynecol 2003; 102: 685–692. [DOI] [PubMed] [Google Scholar]


