Abstract
Background and Aims:
Supraglottic airway devices (SGADs) are increasingly being used for airway management in paediatric patients undergoing general anaesthesia. This survey was designed to assess the nationwide practice patterns of SGAD usage in paediatric patients.
Methods:
A questionnaire of 28 questions was circulated amongst 16,532 members of the Indian Society of Anaesthesiologists through online survey engine Google Forms® and served manually to 500 delegates attending the Asian Society of Paediatric Anaesthesiologists conference 2017. Percentage, mean and standard deviation were calculated using Microsoft Excel 2016 (Redmond, WA, USA).
Results:
Four hundred and five (2.3%) valid responses were obtained. The most commonly used device was i-gel© (60.74%). Three hundred and four (75.06%) respondents had access to second-generation SGADs. Second-generation devices (60.74%) were more commonly used than first-generation devices (39.26%). Anaesthesiologists utilised SGADs in various challenging scenarios such as in the difficult airway (53.33%), remote locations (55.47%), ophthalmologic (38.77%) and long-duration surgeries (17.53%). Sixty per cent respondents did not use SGADs in laparoscopic surgery. Disposable SGADs were reused by 77.28% respondents. Oropharyngeal seal and intracuff pressures were not measured by 86.91% and 56.92% respondents, respectively. Difficulty in size selection (84.19%), securing position (82.22%) and maintaining unobstructed ventilation (78.76%) were common problems encountered while using SGADs.
Conclusion:
Although there is a widespread use of second-generation SGADs in Indian paediatric anaesthesia, safe practices such as using capnography, measurement of oropharyngeal seal pressure, cuff pressure and appropriate disinfection are lacking.
Key words: Airway management, disinfection, laryngeal masks, paediatric anaesthesia, supraglottic airway device, survey
INTRODUCTION
Supraglottic airway devices (SGADs) are routinely used for airway management in paediatric patients undergoing general anaesthesia for various surgeries. SGADs have changed the practice of paediatric anaesthesia.[1,2,3] The newer SGADs have improved features such as the gastric drain tube, better ventilation and seal pressures, and an ability to perform an endotracheal intubation through them. SGADs with a gastric drain tube are classified as second-generation SGADs and are promoted for routine use by Royal College of Anaesthetists in the National Audit Project 4.[4]
Although newer SGADs are freely available for commercial use, there is a dearth of high-quality studies to establish their safety in children.[5] There are studies and case reports in literature describing SGAD use in uncommon and unconventional situations such as laparoscopy and prone position in paediatric patients.[6,7] It would be worthwhile to know if these practices are being applied in clinical use. In the absence of high-quality evidence, there could be a possibility of bias for or against newer devices. A good quality survey may shed some more light on the practices associated with SGADs, identify problems which may have not been reported and bridge the lacunae in the existing literature.
The aim of this survey was to get an overview of SGAD usage in paediatric patients in terms of knowledge, attitudes and practice patterns of anaesthesiologists in India. The objectives were to find out (1) the choice of SGAD in routine use and reasoning behind the choice; (2) anaesthesia practices associated with SGAD use; (3) use of SGAD in complicated and uncommon situations; (4) use of SGAD in difficult airway; (5) safety measures followed while using SGADs and (6) desirable newer design features involving SGADs in paediatric patients.
METHODS
The instrumentation type of survey methodology was used. A questionnaire was prepared by doing a thorough literature search on web-based electronic databases such as PubMed, Google Scholar and Embase. The keywords used were paediatric, practice patterns, SGADs, laryngeal mask airways and extraglottic airway devices. Forty questions were prepared. In addition, 20 questions were added by the investigators based on their experience and problems encountered in clinical practice. All the questions were thoroughly analysed and 49 questions were shortlisted. The first version of the questionnaire was then mailed to thirty expert paediatric anaesthesiologists. Ten experts responded. They were asked to rate the relevance of every question on a 4-point scale (1 = not relevant, 2 = somewhat relevant, 3 = relevant and 4 = highly relevant). Item content validity index (ICVI) for each question was calculated (ICVI = number of experts rating questions as 3–4 divided by a total number of experts). The questions with ICVI >0.78 were retained in the second version (n = 35).[8] Scale content validity index (SCVI) (SCVI = Total of ICVI scores divided by the total number of included questions) of second version of questionnaire was 0.97 which was within acceptable limits.[8] This second questionnaire with 35 questions was circulated amongst anaesthesiologists of our teaching institute for checking feasibility. In the final version, 28 questions were retained. Ethics Committee approval was obtained. The survey was registered with Clinical Trials Registry of India (CTRI REF/2018/02/017539).
The questionnaire [Appendix 1], prepared in English, included basic demographic data such as age, state of residence, qualification, current affiliation, position in institute, years of experience, type of practice and average number of paediatric cases in a month. Twenty-seven questions had multiple choice answers and participants could tick one or more answers depending on the question. The participants had to rate design features on a scale of 1–5 in the last question. The questionnaire had six parts. Question numbers 1–6 included overview and choice of SGAD, questions 7–9 covered current anaesthesia practices associated with SGAD use, questions 10–16 comprised the use of SGAD in uncommon and complicated situations, questions 17 and 18 enquired about the usage of SGADs in difficult airway, questions 19–27 included safety measures associated with their use and question 28 sought personal opinion on design of SGAD.
The questionnaire was manually distributed to the 500 delegates of the Asian Society of Paediatric Anaesthesiologists Conference 2017, at Mumbai. E-mails were also sent to 16,532 members of the Indian Society of Anaesthesiologists from 15/7/17 to 15/9/17. E-mails were not sent to those who had manually filled the forms. Two E-mail reminders were sent to those who did not respond. Participants were requested to fill the questionnaire only once. Completion and submission of questionnaire by the respondents implied consent. Responses received till 30/09/17 were analysed.
All analyses were performed using Microsoft Excel 2016 (Redmond, WA, USA). Sample size was calculated using online calculator from 'The survey system 2016, Creative research systems, Sebastopol, California'. For an estimated population of 17,000, the sample size was calculated to be 376 for a margin of error of 5% and 95% confidence interval.
RESULTS
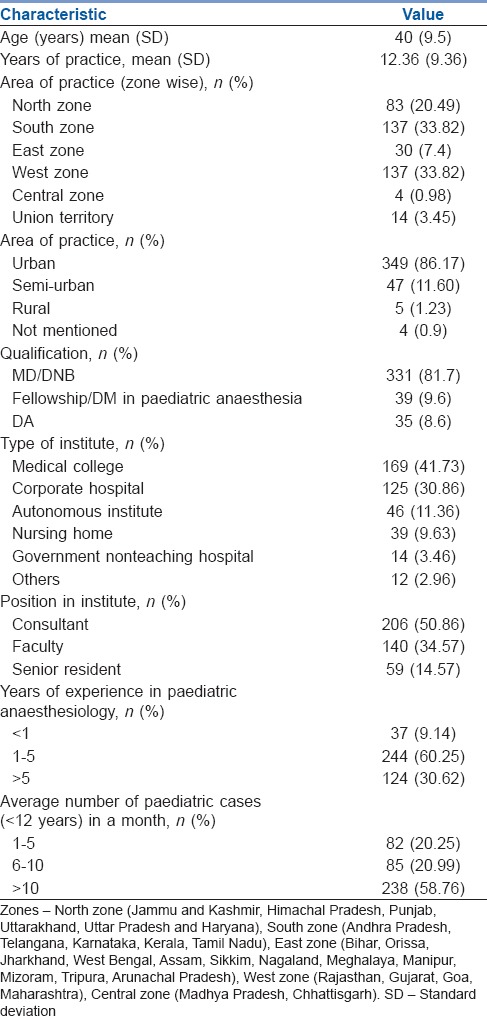
Five hundred and seven anaesthesiologists responded to the survey. We excluded the responses of postgraduate students (59), of those who practiced outside India (15) and of those who did not use SGADs in paediatric patients (34). Six responses fit two or more above-mentioned exclusion criteria, so they were excluded only once. Four hundred and five valid responses (370 online and 35 manual) were analysed. The demographic details of the respondents are presented in Table 1. In question numbers 3, 6, 8 and 18, multiple responses were allowed and the sum of responses does not add up to 405 and the percentages do not add up to 100.
Table 1.
Demographic profile of survey respondents
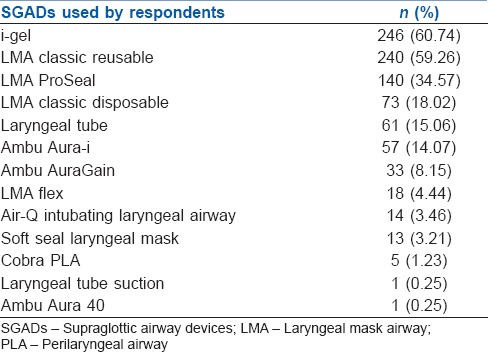
The various SGADs used by respondents are summarised in Table 2. The most commonly used device was i-gel© (n = 246, 60.74%) followed by LMA classic© (cLMA) reusable (n = 240, 59.26%). Three hundred and four (75.06%) respondents had access to second-generation SGADs. Second-generation devices (n = 246, 60.74%) were more commonly used than first-generation devices (n = 159, 39.26%). The order of preference of first-generation devices (n = 159) was: cLMA© reusable – 111 (69.8%), cLMA© disposable – 30 (18.87%), Ambu Aura i© – 12 (7.54%), Soft Seal Laryngeal Mask© – 3 (1.89%), LMA Flex© – 2 (1.26%) and Ambu Aura 40© – 1 (0.63%). The order of preference of second-generation devices (n = 246) was i-gel© – 149 (60.57%), LMA ProSeal© – 60 (24.39%), LMA Supreme© – 24 (9.76%), Ambu AuraGain© – 12 (4.88%) and Laryngeal Tube Suction© (LTS) – 1 (0.40%). Past experience – 277 (68.4%), evidence from research – 133 (32.8%), cost – 120 (29.6%), hospital or department recommendation – 80 (19.75%) and reusability – 64 (15.80%), whatever is given to them – 48 (11.85%), availability – 9 (2.22%) and others – 4 (0.98%) were the factors which influenced the choice of respondents while using any SGAD.
Table 2.
Types of various supraglottic airway devices used by respondents
The maximum duration of surgery for which respondents would use SGAD was < 30 min – 37 (9.14%), 30–60 min – 175 (43.21), >60–90 min – 122 (30.12%) and >90 min – 71 (17.53%). Spontaneous ventilation was used by 274 (67.65%) respondents. Manual ventilation using the Jackson Rees circuit or Bain's circuit was the next most common practice (n = 183, 45.19%). Pressure control (n = 127, 31.36%), volume control (n = 107, 26.42%) and pressure support ventilation (n = 87, 21.48%) were the other modes of ventilation used. Similar number of respondents preferred removing the SGAD in deep plane of anaesthesia (n = 202) and awake state (n = 203).
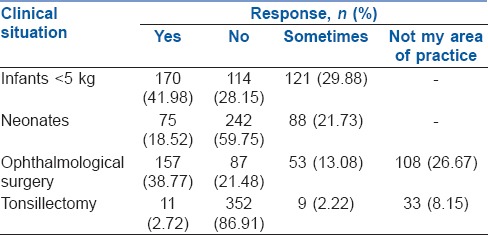
The responses about the use of SGAD in uncommon and complicated clinical situations are summarised in Table 3. Of the 400 respondents who do paediatric laparoscopic surgical cases, 243 (60.75%) never used, whereas 66 (16.5%) used sometimes, 62 (15.5%) rarely, 26 (6.5%) almost always and 3 (0.75%) always used SGAD for laparoscopic surgeries. Amongst those who do cases in remote locations (n = 323), 179 (55.42%) used SGADs. All respondents were comfortable while using SGAD in supine position but fewer used it in lithotomy (n = 209, 51.60%), lateral (n = 198, 48.89%) and prone position (n = 9, 2.22%).
Table 3.
Supraglottic airway device use in different situations
Two hundred and sixteen (53.33%) respondents had used a SGAD in a known difficult airway. The devices used by respondents in a known difficult airway were i-gel© – 83 (38.43%), cLMA© – 66 (30.56%), LMA ProSeal© – 32 (14.81%), Ambu AuraGain© – 11 (5.09%), LMA Supreme© – 10 (4.63%), Ambu Aura-i© – 16 (7.41%), LMA Flex© – 6 (2.78%), air-Q© – 4 (1.85%), Intubating LMA© – 3 (1.39%), LTS© – 2 (0.93%) and Ambu Aura 40© – 1 (0.46%). Eighty-six respondents (21.23%) had intubated through a SGAD at least once. SGAD was used as an intubation conduit by 33 (8.15%) in normal airways, 67 (16.54%) in a known difficult airway and 24 (5.92%) in unanticipated difficult airway. Fibre-optic bronchoscope (FOB), bougie/introducer-guided and blind technique were used by 33 (8.14%), 39 (9.62%) and 28 (6.91%), respectively.
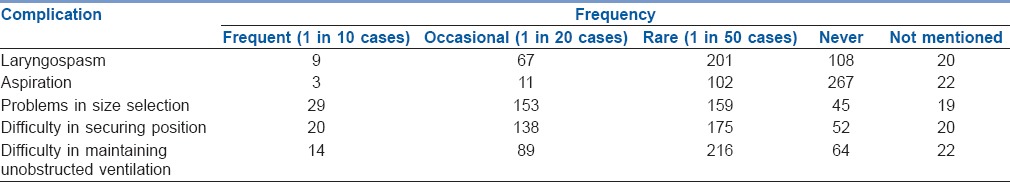
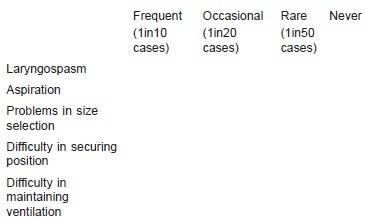
The complications faced by respondents are mentioned in Table 4. Capnometer was used always by 316 (78.02%) respondents, while it was used sometimes or never by 70 (17.28%) and 12 (2.96%), respectively. The rest (7 [1.73%]) did not have access to capnometer.
Table 4.
Frequency of complications faced by respondents
When a cuffed SGAD was used (n = 390), 43 (11.03%) measured the intracuff pressure always, 125 (32.05%) measured it sometimes and 116 (29.74%) did not measure it at all. Equipment needed to measure intracuff pressures was not available to 106 (27.18%). Gradual inflation of the cuff till there is no leak, but up to the maximum recommended volume, was practiced by 234 (60%) respondents, while 97 (24.87%) inflated with the maximum and 24 (6.15%) with half the recommended volume. Cuff pressure monitor to guide the inflation of the cuff was used by 35 (8.98%) respondents. The vast majority of the respondents (n = 352, 86.91%) did not measure seal pressures. Seal pressure was measured for every case by 53 (13.09%) of respondents only. Only 33 (8.15%) respondents measured it again after change in position of patients.
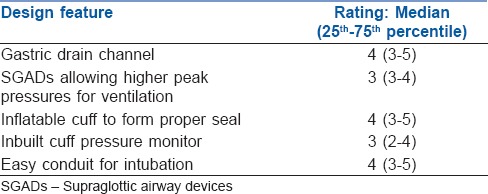
Disposable and reusable devices were preferred by 46 (11.36%) and 132 (32.59%), respectively, while 227 (56.05%) respondents have no such preference. Disposable SGADs were reused by 313 (77.28%) respondents. Amongst these, 157 (50.16%) reused the SGAD till it is no longer usable while rest reused it up to 10 times. Various techniques of disinfection used are mentioned in Table 5. The ratings given for various desirable design features in SGADs are highlighted in Table 6.
Table 5.
Various methods of disinfection of disposable supraglottic airway devices
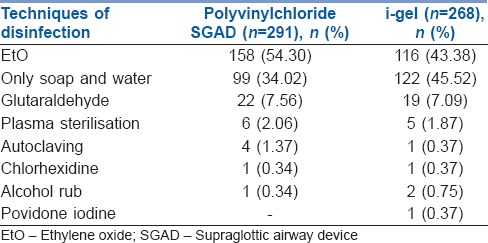
Table 6.
Rating given to various design features in supraglottic airway devices
DISCUSSION
This survey provides an insight into the practice patterns of anaesthesiologists working in India, while using SGADs in paediatric patients. Surveys have been conducted by the Society of Pediatric Anesthesia (SPA) and Association of Paediatric Anaesthetists of Great Britain and Ireland (AAGBI).[5,9] However, there is a dearth of comprehensive large-scale pan-Indian data.[10] AAGBI survey focussed mainly on the choice of SGADs and their use in difficult airway. SPA survey concentrated mainly on practice patterns pertaining to LMA family. Unlike SPA survey, we asked 'have you used' instead of 'would you use' to elicit practice patterns and eliminate theoretical responses. The only survey conducted in India focussed on few practice patterns.[10] We aimed to develop a comprehensive validated questionnaire covering choice, practice patterns in a variety of situations, safety measures employed and desirable newer design features involving SGADs in paediatric patients.
A wide variety of second-generation SGADs are now available in paediatric sizes[1,11] making their use quite common in India. This is significantly different from the findings of older surveys where first-generation devices were used more often.[5,10] The extensive use of i-gel© and cLMA© is perhaps due to ease of use and low rate of serious complications.[3,11] A single point survey involving delegates of national paediatric conference in 2016 found cLMA© to be most popular.[10] Our nationwide survey conducted 1½ years later has shown i-gel© as the most commonly used device. This may represent a shift in the preference of Indian anaesthesiologists. Past experience, rather than evidence from research, guides the choice while selecting a particular SGAD, which is similar to survey conducted by AAGBI.5
Controlled ventilation and pressure support ventilation have been shown to be superior to spontaneous ventilation with ProSeal LMA©.[12,13,14] Spontaneous ventilation or controlled ventilation using Bain's or Jackson Rees circuit was the most commonly used method of ventilation while using SGAD amongst our respondents. This is in contrast to the SPA survey where pressure support ventilation was used by a large number of respondents.[9] Lack of sophisticated anaesthesia ventilators, knowledge and experience in using advanced modes could explain this difference. Advanced modes improve ventilation parameters, thereby enabling anaesthesiologists to use SGADs for prolonged duration.[10] This also explains the reluctance that our respondents had in using SGADs in surgeries lasting for >90 min, unlike the SPA survey.
A greater percentage (28.15%) of our respondents and those from previous Indian survey (38%) do not use SGADs in infants which is in contrast to SPA survey where 9% respondents would not use at all.[9,10] This could be attributed to the late introduction of very small SGADs in the Indian market. Majority of our respondents also did not use SGADs in neonates or used them only sometimes. This reluctance to use SGADs in younger patients could be due to the differences in airway anatomy of such patients causing suboptimal placement, thereby requiring frequent repositioning.[15]
The use of SGAD in ophthalmological surgery is high like previous survey.[9] Although the efficacy of second-generation SGADs in paediatric laparoscopic surgeries is reported,[6,16] majority of our respondents were uncomfortable with their use. However, SGADs have made an inroad into practice with around 7.25% respondents using it almost always or always during laparoscopy like the respondents of SPA survey.[9] SGADs do not appear to be a choice of airway management for tonsillectomies for most respondents. Small studies have shown SGADs to be a suitable alternative to endotracheal intubation,[17,18] but a larger study reveals higher incidence of complications, mainly airway obstruction.[19] Appropriate patient selection, careful insertion, spontaneous ventilation and experience may decrease the incidence of complications. Very few respondents are comfortable with the use of SGAD in prone position like in the SPA survey.[9] Prone positioning limits access to the airway and can pose a dangerous situation if SGAD is malpositioned. The demand for anaesthetising paediatric patients in remote locations such as radiology suites is rising, and it is encouraging to know that SGADs are commonly used by our respondents and this is also being reported in literature.[20,21]
SGADs are now an integral part of paediatric difficult airway algorithms and guidelines[22,23] and more than half of the respondents have used SGADs in a child with a known difficult airway. i-gel© and cLMA© were the most commonly used devices. Use of introducers and FOB through a SGAD serve as facilitators for intubation.[24] SPA and AAGBI surveys have only assessed fibre-optic intubation through SGAD, whereas we incorporated the blind/introducer-guided technique in our questionnaire.[5,9] More than 50% respondents in AAGBI survey had performed FOB-assisted intubation through SGAD in contrast to India where only 9% had done the same. A significant number of our respondents used the blind technique indicating lack of availability of paediatric size FOB.
Current studies tell us more about efficacy rather than safety of SGADs.[25] Aspiration is the most common complication reported in the NAP4.[4] However, in this survey, we found that difficulty in size selection was the most common problem, followed by difficulty in securing position and maintaining unobstructed ventilation. This is similar to previous surveys.[5,10] Here lies the importance of survey where day-to-day difficulties encountered during routine practice get highlighted. However, surveys have limitations as the incidence of rare complications may not get reflected.
Capnography is essential at all times as per the American Society of Anesthesiologists' minimum monitoring standards.[26] General anaesthesia causes significant alterations in respiratory mechanics of paediatric patients. This causes a gradual rise in end-tidal carbon dioxide even though the child is breathing spontaneously. However, nearly a quarter of respondents did not always use a capnometer along with SGADs. This could probably be due to a reluctance to attach a heavy mainstream capnometer adapter to a small SGAD, unavailability, or ignorance of its benefit for short duration procedures. This safety issue has not been addressed in previous surveys.
Very few respondents used a cuff pressure manometer while inflating the cuff of SGADs. Lack of equipment or knowledge could be the probable cause. Using clinical end points to inflate LMA cuffs is associated with significant hyperinflation and may lead to loss of seal between larynx and oesophagus. When cuff pressure exceeds mucosal perfusion pressure, complications such as sore throat and nerve injuries occur.[1] Very young patients are not able to communicate these problems and they may become irritable in the post-operative period. Therefore, cuff manometers should routinely be used.[27]
Measurement of oropharyngeal seal pressure quantifies the efficacy of the seal and ensures optimum ventilation. It also reduces leaks into the oesophagus, thereby reducing the risk of regurgitation and aspiration.[1] Experts have recommended that oropharyngeal seal pressure should be assessed routinely and also rechecked with every change of patient position.[1] Yet, a majority of respondents did not measure the seal pressure at all. Lack of emphasis given during training could possibly be the reason why these important safety practices are seldom used. Moreover, these important issues have not been covered in the previous surveys.
The current survey found that there is widespread reuse of disposable SGADs. This is similar to a survey conducted on SGADs in adults in India.[28] This could be due to its initial easy availability at low cost. Rampant reusing indicates a compulsion of keeping costs low in a limited-resource country. The techniques used for disinfection also varied widely amongst respondents and were largely inadequate for semi-critical equipment such as SGADs which require high-level disinfection.[29] Such practices may predispose the patient to infection, and the oropharyngeal seal of the SGAD may also be lost due to damage caused by repeated reuse.
Novel design features such as in-built cuff pressure monitor and devices allowing higher ventilation pressures have found lower rating in this survey, mainly because of lack of importance given to cuff and oropharyngeal seal pressures in routine practice or an associated increase in cost. It is interesting that the sought-after feature is a design allowing use as an easy conduit for intubation, highlighting the importance of SGAD in a difficult airway.[23]
The poor response rate of the survey could be due to the highly selective field of study, i.e., supraglottic devices in paediatric patients. Furthermore, the responses of predominantly urban anaesthesiologists may not necessarily reflect the practice patterns across the country.
CONCLUSION
Second-generation SGADs are increasingly being used by anaesthesiologists across India in varied situations, representing a paradigm shift in the approach towards airway management in paediatric patients. However, techniques to improve safety, i.e., intracuff and seal pressure measurement, use of capnography and appropriate disinfection techniques are lacking which needs to be emphasised during training and continued medical education.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We sincerely thank all the experts for spending their valuable time and validating the survey questionnaire: Children's Anaesthesia Services, Mumbai, Dr. Ashwin Udupa, Dr. Chandrika Y. R., Dr. Diganta Saikia, Dr. Dilip Pawar, Dr. Jeson Doctor, Dr. Nandini Dave, Dr. Rakhee Goyal, Dr. Sandhya Yaddanapudi, Dr. S. Ramesh, Dr. Snehalata Dhaygude and Dr. Vibhavari Naik.
APPENDIX 1: SURVEY QUESTIONNAIRE
Dear Doctor,
We are anaesthesiologists working in LTMMC, Sion, Mumbai. We invite you to participate in this survey. We thank you in anticipation for your valuable time. Your feedback is important to us as this data is being collected as part of a comprehensive study on the prevalence of SGAD usage and associated practices in paediatric patients among anaesthesiologists. We understand that practice patterns may differ across states/ types of practice/ institute/ freelance, etc. Whatever is ideal may not be practical for innumerable reasons. We are making a sincere attempt to find the practice pattern across India. Please note that your participation in this survey is optional and the data collected will be used for medical publication. We assure that confidentiality will be maintained.
Age: ___________ State: ____________________ Area of practice: urban/ semi urban/ rural
Email :___________________________________
Qualification: DA / MD / DNB / Fellowship or DM in paediatric anaesthesia
Type of institute where you work:
□Medical College □ Corporate hospital □ Government non-teaching hospital □ Nursing home □ Autonomous institute □Others
Position in the institute: □ PG student □ Senior resident □ Faculty □ Consultant
Years of practice ___________
Average number of paediatric cases (<12 years) in a month: □1-5 □ 6-10 □>10
Years of experience in paediatric anaesthesiology: □<1years □1-5 years□> 5 years
Do you exclusively practice paediatric anaesthesia? □ Yes □ No
1. Do you use SGADs in paediatric patients?
□ Yes □ No
2. Out of all paediatric cases, in what percentage of cases are you putting SGAD?
□< 25% □ 25-50% □> 50%
3. Which SGADs do you use in paediatric patients? (Tick as many as appropriate)
□ LMA classic reusable
□ Cobra PLA
□ LMA classic disposable(unique)
□i-gel
□ LMA Flex
□Ambu Aura-i
□ LMA ProSeal
□Ambu AuraGain
□ LMA Supreme
□ Laryngeal Tube
□ Soft Seal Laryngeal mask
□ Laryngeal Tube Suction
□air-Q Intubating Laryngeal Airway
□ Others(specify)_________
4. Do you have 2nd generation SGAD for paediatric patients in your institute?
□ Yes □ No
5. Which SGAD do you commonly use in paediatric patients?(Tick one)
□ First Generation
□ Second Generation
If first generation, then which is your first choice
□ LMA classic reusable□ LMA classic disposable□ LMA Flex □ Soft Seal Laryngeal Mask □ air- Q Intubating Laryngeal Airway □Ambu Aura-i □ Cobra PLA□ Laryngeal Tube □ Others_________
If second generation, then which is your first choice
□ LMA ProSeal□ LMA Supreme □i-gel □Ambu AuraGain □ Laryngeal Tube Suction
□ Others_______
6. What guides your choice for choosing a particular SGAD?(tick as many as appropriate)
□ Past Experience
□ Whatever is given to me
□ Whatever my hospital or department recommends
□ Cost
□ Reusability
□ Evidence from research
□ Type of surgery
□ Any other
7. What is the maximum duration of surgery for which you have used a SGAD in a paediatric patient comfortably?
□<30 minutes □ 30minutes-1hour □>1- 1 ½ hours □> 1 ½ hours
8. What mode of ventilation do you use while using SGAD in paediatric patients?(tick as many as appropriate)
□ Spontaneous
□ Controlled ventilation with JR circuit/Bain's circuit
□ Manually controlled ventilation with circle absorber
□ Volume controlled
□ Pressure controlled
□ Pressure support ventilation
□ Any other (Specify) ________
9. Which is your preferred method for removal of paediatric SGAD?
□ Remove when patient is in deep plane of anaesthesia
□ Child bringing out SGAD on his own/awake state
10. Are you comfortable in using SGAD in infants< 5kg?
□ Yes □ No □ Sometimes
11. Do you use SGAD in a paediatric patient undergoing ophthalmological surgery?
□ Yes □ No □ Sometimes □ I don't do ophthalmic cases.
12. Do you use SGAD in a paediatric patient who is undergoing laparoscopy?
□ Always □ Almost always □ Sometimes □ Rarely □ Never
□ I don't do laparoscopy cases
13. Do you use SGAD in paediatric patients undergoing tonsillectomy?
□ Yes □ No □ Sometimes □ I don't do tonsillectomy
14. Do you use SGAD in neonates?
□ Yes □ No □ Sometimes
15. In which surgical positions are you comfortable in using SGAD in paediatric patients? (tick as many as appropriate)
□ Supine □ Lateral □ Lithotomy □ Prone
16. Have you used SGAD in a paediatric patient in a remote location like CT scan, MRI, interventional radiology, etc.?
□Yes □ No □ I don?t do cases in remote locations
17. Have you ever used SGAD in a child with known difficult airway? □Yes □ No
Which device/devices did you use? ______________________________
18. Have you ever intubated through paediatric SGAD?
□ Yes □ No
If Yes, then intubation was performed (tick as many as appropriate)
□ In a normal airway
□ In anticipated Difficult Airway
□ In unanticipated difficult airway
If Yes, then intubation through SGAD was (tick as many as appropriate)
□ Blind
□ Fibreoptic guided
□ Introducer/bougie guided
□ Other (specify)
19. How often have you faced problems while using SGADs in paediatric patients? (please tick in the appropriate boxes)
Please mention if any particular device/s has caused problems_________
Any other problem/complication(specify) ________
20. Do you use capnometer when SGAD is used?
□Always □ Never □ Sometimes□ Equipment not available
21. Do you monitor intra-cuff pressure when SGAD with inflatable cuff is used?
□Always □ Never □ Sometimes□ Equipment not available
22. After SGAD insertion, with how much volume do you inflate the cuff?
□ With maximum recommended volume
□ With half the maximum recommended volume
□ Gradually till there is no leak but upto the maximum recommended volume.
□ Guided by cuff pressure monitor
23. Do you measure seal pressure/ oropharyngeal leak pressure for every case whenever you use a SGAD?
□ Yes □ No
If yes, then do you remeasure if there is a change in position like head flexion, extension or supine to lateral position?
□ Yes □ No
24. What do you prefer?
□ Single use/disposable SGAD □Resusable SGAD □ Both
25. Do you reuse disposable SGAD? □ Yes □ No
If yes, how often? □Upto 10 uses □ Till it is no longer usable
26. If you are reusing polyvinyl chloride (disposable) SGAD, how do you disinfect it?
□ Only soap and water□ Glutaraldehyde □ ETO sterilisation□ Any other
□ Not applicable
27. If you are reusing i-gel, how do you disinfect it?
□ Only soap and water □ Glutaraldehyde □ ETO sterilisation □ Any other
□ Not applicable
28. What feature you feel is important in paediatric SGAD? (rate each on a scale of 1-5 where 1 = least important and 5= most important)
Gastric drain channel _________
SGADs allowing higher peak pressures for ventilation________
Inflatable cuff to form proper seal________
Non-inflatable cuff to form proper seal_________
Inbuilt cuff pressure monitor _________
Easy conduit for intubation________
REFERENCES
- 1.Goyal R. Small is the new big: An overview of newer supraglottic airways for children. J Anaesthesiol Clin Pharmacol. 2015;31:440–9. doi: 10.4103/0970-9185.169048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramesh S, Jayanthi R. Supraglottic airway devices in children. Indian J Anaesth. 2011;55:476–82. doi: 10.4103/0019-5049.89874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White MC, Cook TM, Stoddart PA. A critique of elective pediatric supraglottic airway devices. Paediatr Anaesth. 2009;19(Suppl 1):55–65. doi: 10.1111/j.1460-9592.2009.02997.x. [DOI] [PubMed] [Google Scholar]
- 4.Cook T, Woodall N, Frerk C. Major Complications of Airway Management in the United Kingdom. 4th National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society; Reports and Findings;; 2011. pp. 86–95. [DOI] [PubMed] [Google Scholar]
- 5.Bradley AE, White MC, Engelhardt T, Bayley G, Beringer RM. Current UK practice of pediatric supraglottic airway devices – A survey of members of the Association of Paediatric Anaesthetists of Great Britain and Ireland. Paediatr Anaesth. 2013;23:1006–9. doi: 10.1111/pan.12230. [DOI] [PubMed] [Google Scholar]
- 6.Sinha A, Sharma B, Sood J. ProSeal as an alternative to endotracheal intubation in pediatric laparoscopy. Paediatr Anaesth. 2007;17:327–32. doi: 10.1111/j.1460-9592.2006.02127.x. [DOI] [PubMed] [Google Scholar]
- 7.Taxak S, Gopinath A. Insertion of the i-gel airway in prone position. Minerva Anestesiol. 2010;76:381. [PubMed] [Google Scholar]
- 8.Polit DF, Beck CT. The content validity index: Are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–97. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 9.Patel A, Clark SR, Schiffmiller M, Schoenberg C, Tewfik G. A survey of practice patterns in the use of laryngeal mask by pediatric anesthesiologists. Paediatr Anaesth. 2015;25:1127–31. doi: 10.1111/pan.12727. [DOI] [PubMed] [Google Scholar]
- 10.Kaniyil S, Smithamol PB, Joseph E, Krishnadas A, Ramadas KT. A survey of current practice of supraglottic airway devices in pediatric anesthesia from India. Anesth Essays Res. 2017;11:578–82. doi: 10.4103/0259-1162.206870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jagannathan N, Ramsey MA, White MC, Sohn L. An update on newer pediatric supraglottic airways with recommendations for clinical use. Paediatr Anaesth. 2015;25:334–45. doi: 10.1111/pan.12614. [DOI] [PubMed] [Google Scholar]
- 12.Templeton TW, Hoke LK, Templeton LB, Ririe DG, Rose DM, Bryan YF, et al. Acomparison of 3 ventilation strategies in children younger than 1 year using a Proseal laryngeal mask airway: A randomized controlled trial. J Clin Anesth. 2016;35:502–8. doi: 10.1016/j.jclinane.2016.07.042. [DOI] [PubMed] [Google Scholar]
- 13.Templeton TW, Hoke LK, Yaung J, Aschenbrenner CA, Rose DM, Templeton LB, et al. Comparing 3 ventilation modalities by measuring several respiratory parameters using the ProSeal laryngeal mask airway in children. J Clin Anesth. 2016;34:272–8. doi: 10.1016/j.jclinane.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Lim B, Pawar D, Ng O. Pressure support ventilation vs. spontaneous ventilation via ProSeal™ laryngeal mask airway in pediatric patients undergoing ambulatory surgery: A randomized controlled trial. Paediatr Anaesth. 2012;22:360–4. doi: 10.1111/j.1460-9592.2012.03819.x. [DOI] [PubMed] [Google Scholar]
- 15.Von Ungern-Sternberg BS, Wallace CJ, Sticks S, Erb TO, Chambers NA. Fibreoptic assessment of paediatric sized laryngeal mask airways. Anaesth Intensive Care. 2010;38:50–4. doi: 10.1177/0310057X1003800110. [DOI] [PubMed] [Google Scholar]
- 16.Tulgar S, Boga I, Cakiroglu B, Thomas DT. Short-lasting pediatric laparoscopic surgery: Are muscle relaxants necessary? Endotracheal intubation vs. laryngeal mask airway. J Pediatr Surg. 2017;52:1705–10. doi: 10.1016/j.jpedsurg.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Sierpina DI, Chaudhary H, Walner DL, Villines D, Schneider K, Lowenthal M, et al. Laryngeal mask airway versus endotracheal tube in pediatric adenotonsillectomy. Laryngoscope. 2012;122:429–35. doi: 10.1002/lary.22458. [DOI] [PubMed] [Google Scholar]
- 18.Peng A, Dodson KM, Thacker LR, Kierce J, Shapiro J, Baldassari CM, et al. Use of laryngeal mask airway in pediatric adenotonsillectomy. Arch Otolaryngol Head Neck Surg. 2011;137:42–6. doi: 10.1001/archoto.2010.230. [DOI] [PubMed] [Google Scholar]
- 19.Lalwani K, Richins S, Aliason I, Milczuk H, Fu R. The laryngeal mask airway for pediatric adenotonsillectomy: Predictors of failure and complications. Int J Pediatr Otorhinolaryngol. 2013;77:25–8. doi: 10.1016/j.ijporl.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 20.Ucisik-Keser FE, Chi TL, Hamid Y, Dinh A, Chang E, Ferson DZ, et al. Impact of airway management strategies on magnetic resonance image quality. Br J Anaesth. 2016;117(Suppl 1):i97–i102. doi: 10.1093/bja/aew210. [DOI] [PubMed] [Google Scholar]
- 21.Zaballos M, Bastida E, del Castillo T, de Villoria JG, Jiménez C. In vitro study of magnetic resonance imaging artefacts of six supraglottic airway devices. Anaesthesia. 2010;65:569–72. doi: 10.1111/j.1365-2044.2010.06299.x. [DOI] [PubMed] [Google Scholar]
- 22.Weiss M, Engelhardt T. Proposal for the management of the unexpected difficult pediatric airway. Paediatr Anaesth. 2010;20:454–64. doi: 10.1111/j.1460-9592.2010.03284.x. [DOI] [PubMed] [Google Scholar]
- 23.Pawar DK, Doctor JR, Raveendra US, Ramesh S, Shetty SR, Divatia JV, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in paediatrics. Indian J Anaesth. 2016;60:906–14. doi: 10.4103/0019-5049.195483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong DT, Yang JJ, Mak HY, Jagannathan N. Use of intubation introducers through a supraglottic airway to facilitate tracheal intubation: A brief review. Can J Anaesth. 2012;59:704–15. doi: 10.1007/s12630-012-9714-8. [DOI] [PubMed] [Google Scholar]
- 25.Cook TM, Kelly FE. Time to abandon the 'vintage' laryngeal mask airway and adopt second-generation supraglottic airway devices as first choice. Br J Anaesth. 2015;115:497–9. doi: 10.1093/bja/aev156. [DOI] [PubMed] [Google Scholar]
- 26.Standards for Basic Anesthetic Monitoring – American Society of Anesthesiologists. American Society of Anesthesiologists. 2015. [Last accessed on 2017 Nov 22]. Available from: http://www.asahq.org/quality-and-practice-management/practice-guidance-resource-documents/standards-for-basic-anesthetic-monitoring .
- 27.Licina A, Chambers NA, Hullett B, Erb TO, von Ungern-Sternberg BS. Lower cuff pressures improve the seal of pediatric laryngeal mask airways. Paediatr Anaesth. 2008;18:952–6. doi: 10.1111/j.1460-9592.2008.02706.x. [DOI] [PubMed] [Google Scholar]
- 28.Kadar SM, Koshy R. Survey of supraglottic airway devices usage in anaesthetic practice in South Indian state. Indian J Anaesth. 2015;59:190–3. doi: 10.4103/0019-5049.153044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rutala WA, Weber DJ. Guideline for Disinfection and Sterilization in Healthcare Facilities. Atlanta: Centers for Disease Control and Prevention; 2008; 2008. [Last accessed on 2018 Jan 22]. Infection Control Practices Advisory Committee (HICPAC) Available from: http://www.cdc.gov/hicpac/pdf/guidelines/disinfection_nov_2008.pdf . [Google Scholar]


