Abstract
Background and Aims:
Identification of subarachnoid space in pregnant patients can pose a great challenge to anaesthesiologists. This study was designed to compare conventional landmark technique with pre-procedural ultrasonography-assisted midline approach for identification of the subarachnoid space in elective caesarean section.
Methods:
After institute ethics committee approval and written informed consent, 100 parturients scheduled for elective caesarean section under spinal anaesthesia were included in this prospective randomised control trial and divided into Group L (n = 50) (landmark technique) and Group U (n = 50) (ultrasound-guided technique). Parameters such as time taken for the identification of the interspace, distance between skin and dura mater, number of insertion attempts (the primary outcome), number of passes and time taken were recorded in both the groups. Statistical analysis was done using SPSS software 16.
Results:
Demographic profiles of both groups were comparable. The number of attempts for needle insertion (1.04 ± 0.19 vs. 1.97 ± 0.77), number of passes in the same interspinous space (1.26 ± 0.44 vs. 1.90 ± 0.51) and the total time for successful lumbar puncture (31.90 ± 6.30 vs. 51.80 ± 12.28 s) were significantly less in Group U as compared to Group L, but the time of identification of interspinous space was significantly more in Group U (56.70 ± 13.08 s) as compared to Group L (47.10 ± 10.45 s).
Conclusion:
Pre-procedural ultrasound is a useful tool for successful lumbar puncture in parturients as it reduces the number of attempts with fewer side effects as compared to conventional landmark technique.
Key words: Caesarean section, subarachnoid space, ultrasonography
INTRODUCTION
Spinal anaesthesia is one of the common techniques employed in obstetric anaesthesia, and its success relies on the proper identification of anatomical landmarks. However, the normal anatomical changes of pregnancy and labour pain pose a great challenge to anaesthesiologists for a successful subarachnoid block.[1,2] Use of ultrasound for the central neuraxial block is still underappreciated mainly because of difficulty in perceiving the image through the narrow acoustic windows produced by the bony framework of the spine.[3,4]
We hypothesised that the routine use of pre-procedural ultrasound-guided midline approach of spinal technique at L3–L4 interspinous space would result in fewer attempts to enter the subarachnoid space when compared to the conventional landmark-based midline approach for elective caesarean section. The primary objective was to study the number of insertion attempts and the secondary objectives were to study the number of passes, space identification time and time for successful lumbar puncture.
METHODS
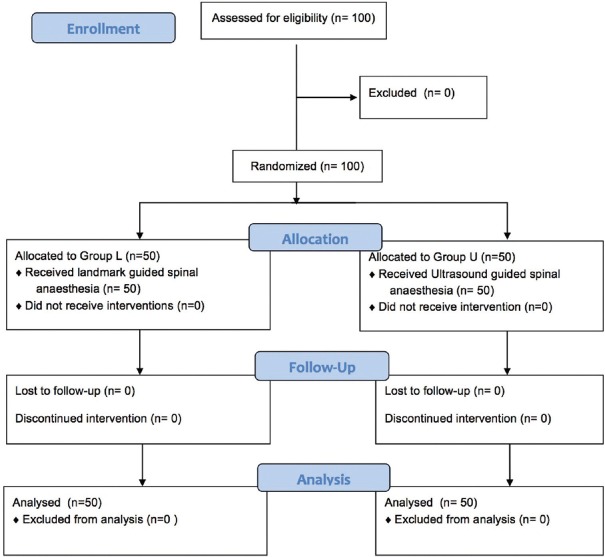
After getting institute ethics committee approval and written informed consent, the current study was done between September 2016 and June 2017. One hundred parturients scheduled to undergo elective caesarean section under spinal anaesthesia were included in this prospective randomised control trial. Selection of participant was done by simple random sampling technique. Parturients with spinal deformities, history of past spinal surgery, coagulopathy and those who refuse spinal anaesthesia were excluded from this study. All patients were randomised into two groups: Group L – landmark-guided technique (n = 50) and Group U – Ultrasound-guided technique (n = 50) by a computer-generated random number sequence using simple randomisation technique [Figure 1]. Group allocation and concealement was done by a closed envelope technique. Spinal anaesthesia was performed by anaesthesiologists who had the experience of more than 50 cases of ultrasound-guided identification of the subarachnoid space. All patients were given pre-medication as per departmental protocol and shifted in the left lateral position. In the operation theatre, after attaching all standard monitors (non-invasive blood pressure, pulse oximetry and electrocardiogram) and recording baseline parameters, intravenous access was established and the patients were positioned in sitting posture. In Group L, L3–L4 interspace was identified by traditional landmark technique (intersection between the midline and Tuffier's line) and time taken for the identification of the interspace (time from which the anaesthesiologist started palpating to identify the landmark to completion of palpation) was noted. In Group U, curvilinear probe (3–6 MHz) of portable ultrasound machine (Sonosite M Turbo™) was used for pre-procedural marking. A sagittal oblique view of the spine was obtained, and the L3–L4 interspinous space with best image of the anterior complex (anterior dura mater, posterior longitudinal ligament and body of corresponding vertebra) and posterior complex (ligamentum flavum and posterior dura mater) was obtained. At this selected interspace, the probe was positioned in transverse view and a skin marker was used to mark the midpoint of the long and short borders of the probe. The point of intersection of both lines was identified as the needle entry point.[5] Time taken for identification of the interspace (the time from which ultrasound probe is placed on the patient to completion of marking), the distance between skin and posterior complex and the angulation of the probe were noted in transverse view. Ultrasound depth (UD), i.e., the distance between skin and the ventral border of posterior complex was measured in Group U only.
Figure 1.
Consolidated Standards of Reporting Trials flow diagram showing patient progress through the study phases. Group L: Landmark group, Group U: Ultrasound group
Strict asepsis was maintained throughout the procedure in both the groups. Spinal anaesthesia was given with 25-G Quincke 90-mm needle. Needle depth (ND), that is the distance from tip to the skin level was measured after removing the spinal needle. During the procedure, parameters such as insertion attempts (defined as the number of times the spinal needle was withdrawn from the skin and reinserted), passes (defined as the number of advancements, that is withdrawal and redirection of the spinal needle without exiting the skin) and time taken for performing the procedure (time from insertion of the needle to getting free cerebrospinal fluid [CSF] flow) were recorded in both the groups.
Sample size was calculated based on the previous study by Kim et al.[6] which showed that the average number of attempts per spinal anaesthetic for an experienced anaesthesiologist would be 3.3 ± 3.1 (mean ± standard deviation). We hypothesised that using a pre-procedural ultrasound, the number of attempts could be reduced to 1.3. It was found that a total of 44 patients in each group will be needed to achieve a power of 90% and type 1 error of <0.05. We included 50 participants in each group to compensate for attrition. Statistical analysis was done using SPSS software version 16 (SPSS Inc., Chicago, Illinosis, USA). All data were analysed for normal distribution using the Shapiro–Wilk test. Categorical data were analysed using the Chi-square test or Fisher exact test as appropriate. Normally distributed parametric data were analysed using Student t-test. All tests were two-tailed. P < 0.05 was considered as statistically significant.
RESULTS
Demographic profile such as age, weight, height and body mass index was comparable between the groups [Table 1]. Time taken for identification of interspinous space was significantly more in Group U (56.70 ± 13.08 s) as compared to Group L (47.10 ± 10.45 s.) (P < 0.001). However, other parameters such as number of attempts for needle insertion, number of passes in the same interspinous space and the total time for successful lumbar puncture were significantly less in Group U as compared to Group L [Table 2]. Successful lumbar puncture in the first attempt [Figure 2] and in one pass [Figure 3] was significantly high in Group U that is 96% and 74%, respectively, whereas in Group L, it was 30% and 18%, respectively (P < 0.001). In Group U, only 2% patients had paraesthesia, whereas in Group L, 28% patients had paraesthesia during the procedure (P = 0.0001). None of the patients in Group U had blood mixed CSF as compared to 14% of patients in Group L (P = 0.0001).
Table 1.
Demographic profile of the study groups
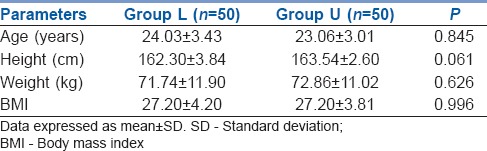
Table 2.
Comparison of space identification time, number of attempts, number of passes and total time taken for successful lumbar puncture between Group L and Group U
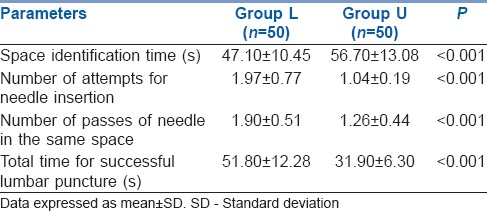
Figure 2.
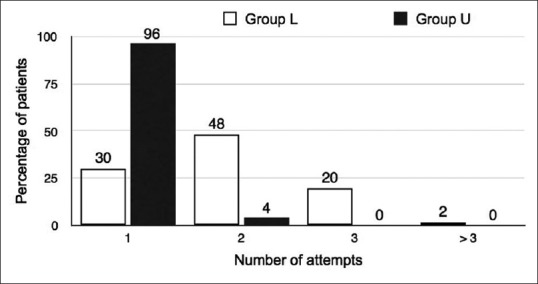
Comparison of number of attempts between Group L and Group U
Figure 3.
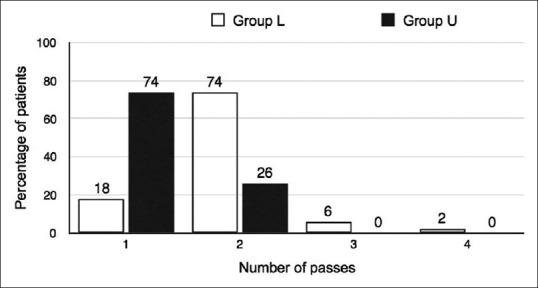
Comparison of number of passes between Group L and Group U
The Pearson correlation coefficient (r) between the UD and the ND was 0.97% (95% confidence interval [CI]: 0.91–1.0, r2 = 0.97). The concordance correlation coefficient was 0.79 (95% CI: 0.71–0.88). The graphical representation of the UD versus the ND demonstrating the line of best fit is shown in Figure 4. The mean ND was 4.79 ± 0.91 cm, whereas the UD was 4.87 ± 0.67 cm and the difference between the measurements was statistically insignificant (P = 0.59).
Figure 4.
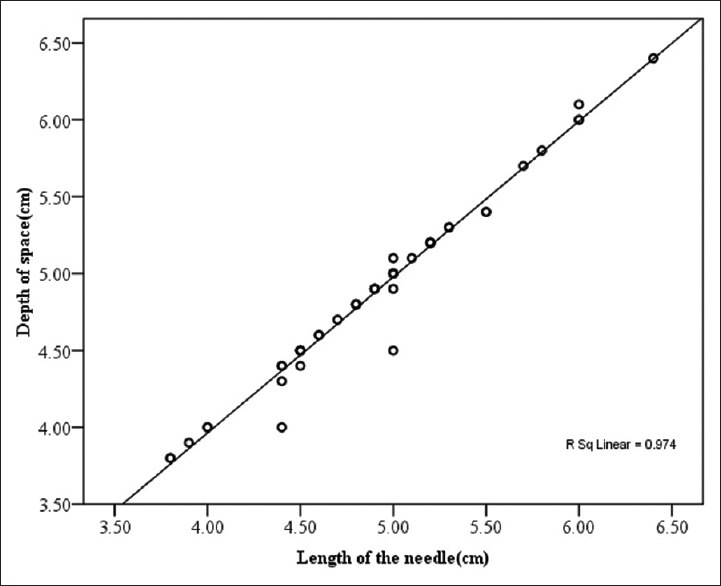
Scatter plot for correlation of ultrasound measured depth and actual needle length
DISCUSSION
Our study demonstrated that the use of a pre-procedural ultrasound-guided midline spinal technique resulted in a significant reduction in the number of attempts and passes required for successful spinal anaesthesia compared with a conventional landmark-based midline approach in patients undergoing caesarean section.
Correct identification of the interspinous space is one of the important steps for successful spinal anaesthesia as it minimises the number of attempts, which in turn reduces the risk of spinal haematoma, post-dural puncture headache, trauma-to-neural structures and patient discomfort.[7,8,9] In our study, the success rate of correct identification of the subarachnoid space in parturients using ultrasound guidance on the first attempt was 96% which was similar to various other patient populations.[10,11] Furthermore, the mean total number of attempts was significantly less in ultrasound group as compared to conventional group. This is in contrary to study done by Ansari et al.[12] which showed no significant difference in the total number of attempts. This could be due to the difference in the study population as they included only easily palpable spine patients. Perlas also showed that ultrasound is more accurate than palpation for correct identification of lumbar interspaces and also decreases the number of attempts required to perform the block.[3]
In our study, one pass success rate was 74% in ultrasound group which was similar to study done by Lim et al.[13] Grau et al. have also shown that use of real-time ultrasound guidance for combined spinal–epidural insertion in a younger obstetric population significantly reduced the number of needle passes required when compared to a traditional landmark-based approach.[14] In our study, we found that the time taken for identification of the L3–L4 interspinous space was less in landmark-based technique as compared to ultrasound-guided identification of the interspinous space. This may be due to difficulty in identifying a satisfactory acoustic window in ultrasound technique. Although the identification time was long in ultrasound group, the procedural time was significantly less in ultrasound group. Sahin et al. also showed that the total duration of the spinal procedure was shorter in the ultrasound group.[15]
In our study, we also found that ultrasound imaging in the transverse plane in parturients provides a reasonable estimation of the depth of the subarachnoid space from the skin puncture site. Wallace et al.[16] and Grau et al.[17] also showed that ultrasonography estimation of depth to the epidural space was reliable in obese parturients; however, they measured the distance from the skin to the lamina in the longitudinal paramedian plane, rather than the distance from the skin to the ligamentum flavum in the transverse plane. We preferred transverse plane as the study conducted by Sahota et al.[18] showed that the estimates of the ultrasound determined the distance to the epidural space in the transverse median view were comparable to those in the parasagittal oblique view.
We measured the distance between skin puncture site and posterior complex in the transverse scan and correlated it with the depth of needle insertion after the procedure. We found that the ultrasound-estimated depth to the subarachnoid space correlated highly with the actual depth of needle in parturients. The regression analysis showed that the estimation of the depth by ultrasound differs minimally from the ND as the ND increases [Figure 4]. It was also found that the UD underestimates the ND by about 0.08 cm which may be attributed to the greater subcutaneous tissue compression by the ultrasound probe.
In our study, paresthesia during the procedure and bloody tap were also found to be significantly less in ultrasound group as compared to landmark group which can be attributed to the accurate identification of interspace by ultrasound technique. Limitations of our study include the difficulty of blinding of anaesthesiologists for the study group, as the patients belonging to ultrasound group will have skin markings. Further randomised, controlled trial with a big sample size is necessary to confirm the utility of ultrasound in this patient population.
CONCLUSION
Thus, we conclude that pre-procedural ultrasound is a useful tool for successful lumbar puncture in parturients as it reduces the number of attempts with fewer side effects as compared to conventional landmark technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lie J, Patel S. Ultrasound for obstetric neuraxial anesthetic procedures: Practical and useful? J Obstet Anaesth Crit Care. 2015;5:49–53. [Google Scholar]
- 2.Borges BC, Wieczorek P, Balki M, Carvalho JC. Sonoanatomy of the lumbar spine of pregnant women at term. Reg Anesth Pain Med. 2009;34:581–5. doi: 10.1097/AAP.0b013e3181bfbe99. [DOI] [PubMed] [Google Scholar]
- 3.Perlas A. Evidence for the use of ultrasound in neuraxial blocks. Reg Anesth Pain Med. 2010;35:S43–6. doi: 10.1097/AAP.0b013e3181d2462e. [DOI] [PubMed] [Google Scholar]
- 4.Jain PN, Ranganathan P. Ultrasound in anaesthesia. Indian J Anaesth. 2007;51:176–83. [Google Scholar]
- 5.Kallidaikurichi Srinivasan K, Iohom G, Loughnane F, Lee PJ. Conventional landmark-guided midline versus preprocedure ultrasound-guided paramedian techniques in spinal anesthesia. Anesth Analg. 2015;121:1089–96. doi: 10.1213/ANE.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 6.Kim JH, Song SY, Kim BJ. Predicting the difficulty in performing a neuraxial blockade. Korean J Anesthesiol. 2011;61:377–81. doi: 10.4097/kjae.2011.61.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amin WA, Abou Seada MO, Bedair E, Elkersh MM, Karunakaran E. Comparative study between ultrasound determination and clinical assessment of the lumbar interspinous level for spinal anesthesia. Middle East J Anaesthesiol. 2014;22:407–12. [PubMed] [Google Scholar]
- 8.Reynolds F. Damage to the conus medullaris following spinal anaesthesia. Anaesthesia. 2001;56:238–47. doi: 10.1046/j.1365-2044.2001.01422-2.x. [DOI] [PubMed] [Google Scholar]
- 9.Davies JM, Posner KL, Lee LA, Cheney FW, Domino KB. Liability associated with obstetric anesthesia: A closed claims analysis. Anesthesiology. 2009;110:131–9. doi: 10.1097/ALN.0b013e318190e16a. [DOI] [PubMed] [Google Scholar]
- 10.Weed J, Finkel K, Beach ML, Granger CB, Gallagher JD, Sites BD, et al. Spinal anesthesia for orthopedic surgery: A detailed video assessment of quality. Reg Anesth Pain Med. 2011;36:51–5. doi: 10.1097/AAP.0b013e3182030863. [DOI] [PubMed] [Google Scholar]
- 11.Puolakka R, Haasio J, Pitkänen MT, Kallio M, Rosenberg PH. Technical aspects and postoperative sequelae of spinal and epidural anesthesia: A prospective study of 3,230 orthopedic patients. Reg Anesth Pain Med. 2000;25:488–97. doi: 10.1053/rapm.2000.7607. [DOI] [PubMed] [Google Scholar]
- 12.Ansari T, Yousef A, El Gamassy A, Fayez M. Ultrasound-guided spinal anaesthesia in obstetrics: Is there an advantage over the landmark technique in patients with easily palpable spines? Int J Obstet Anesth. 2014;23:213–6. doi: 10.1016/j.ijoa.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Lim YC, Choo CY, Tan KT. A randomised controlled trial of ultrasound-assisted spinal anaesthesia. Anaesth Intensive Care. 2014;42:191–8. doi: 10.1177/0310057X1404200205. [DOI] [PubMed] [Google Scholar]
- 14.Grau T, Leipold RW, Fatehi S, Martin E, Motsch J. Real-time ultrasonic observation of combined spinal-epidural anaesthesia. Eur J Anaesthesiol. 2004;21:25–31. doi: 10.1017/s026502150400105x. [DOI] [PubMed] [Google Scholar]
- 15.Sahin T, Balaban O, Sahin L, Solak M, Toker K. A randomized controlled trial of preinsertion ultrasound guidance for spinal anaesthesia in pregnancy: Outcomes among obese and lean parturients: Ultrasound for spinal anesthesia in pregnancy. J Anesth. 2014;28:413–9. doi: 10.1007/s00540-013-1726-1. [DOI] [PubMed] [Google Scholar]
- 16.Wallace DH, Currie JM, Gilstrap LC, Santos R. Indirect sonographic guidance for epidural anesthesia in obese pregnant patients. Reg Anesth. 1992;17:233–6. [PubMed] [Google Scholar]
- 17.Grau T, Leipold RW, Horter J, Conradi R, Martin EO, Motsch J, et al. Paramedian access to the epidural space: The optimum window for ultrasound imaging. J Clin Anesth. 2001;13:213–7. doi: 10.1016/s0952-8180(01)00245-8. [DOI] [PubMed] [Google Scholar]
- 18.Sahota JS, Carvalho JC, Balki M, Fanning N, Arzola C. Ultrasound estimates for midline epidural punctures in the obese parturient: Paramedian sagittal oblique is comparable to transverse median plane. Anesth Analg. 2013;116:829–35. doi: 10.1213/ANE.0b013e31827f55f0. [DOI] [PubMed] [Google Scholar]