Abstract
Background and Aims:
Both transversus abdominis plane (TAP) block and combined ilioinguinal-iliohypogastric (IIN/IHN) blocks are used routinely under ultrasound (USG) guidance for postoperative pain relief in patients undergoing inguinal hernia surgery. This study compares USG guided TAP Vs IIN/IHN block for post-operative analgesic efficacy in adults undergoing inguinal hernia surgery.
Methods:
Sixty adults aged 18 to 60 with American Society of Anesthesiologsts' grade I or II were included. After general anaesthesia, patients in Group I received USG guided unilateral TAP block using 0.75% ropivacaine 3 mg/kg (maximum 25 mL) and those in Group II received IIN/IHN block using 10 mL 0.75% ropivacaine. Postoperative rescue analgesia was with tramadol (intravenous) IV ± diclofenac IV in the first 4 h followed by oral diclofenac subsequently. Total analgesic consumption in the first 24 h was the primary objective, intraoperative haemodynamics, number of attempts and time required for performing the block as well as the postoperative pain scores were also evaluated.
Results:
Time to first analgesic request was 319.8 ± 115.2 min in Group I and 408 ± 116.4 min in Group II (P = 0.005). Seven patients (23.33%) in Group I and two (6.67%) in Group II required tramadol in first four hours. No patient in either groups received diclofenac IV. The average dose of tablet diclofenac was 200 ± 35.96 mg in Group I and 172.5 ± 34.96 mg in Group II (P = 0. 004).
Conclusion:
USG guided IIN/IHN block reduces the postoperative analgesic requirement compared to USG guided TAP block.
Key words: Iliohypogastric nerve block, ilioinguinal nerve block, inguinal hernia, ultrasound guided
INTRODUCTION
Inguinal hernia repair is one of the most common surgical procedures performed, and post-operative pain may be moderate-to-severe. It is associated with delayed return to normal daily activities and may also be related to persistent post-surgical pain (affecting between 0% and 43% of patients).[1]
The major goal in the management of post-operative pain is minimising the dose of medications to lessen side effects while still providing adequate analgesia. Various modalities available to control pain after hernia surgery include pharmacological methods, topical analgesics, peripheral local anaesthetics, epidural analgesia and non-pharmacological approaches; however, optimal evidence-based pain therapy remains unknown.[2]
Regional nerve block techniques offer a great degree of post-operative pain relief thus facilitating early ambulation and discharge. Ilioinguinal and iliohypogastric (IIN/IHN) nerve blocks are among the most frequently used regional blocks performed for analgesia following inguinal surgery and have been shown to significantly reduce pain associated with herniorrhaphy.[3,4,5] The failure rate with blind technique is 20%–30% even in experienced hands. In addition, blind technique may cause complications. The use of ultrasound may potentially reduce the incidence of these complications.[6,7]
The transversus abdominis plane (TAP) block is a novel, rapidly expanding regional anaesthesia technique that provides analgesia to the parietal peritoneum as well as the skin and muscles of the anterior abdominal wall following abdominal surgery. It has become increasingly popular worldwide because of its relative simplicity and efficacy. The use of ultrasound improves the success rate and accuracy of nerve blocks and prevents potential complications.[8,9]
The efficacy of TAP and IIN/IHN blocks for post-operative pain following inguinal hernia surgeries has previously been compared by a few authors, but the results are conflicting.[10,11] Since there are no conclusive studies favouring either of the two aforementioned techniques, the present study was conducted to compare ultrasound-guided TAP and IIN/IHN block for their post-operative analgesic efficacy in adult patients undergoing hernia surgeries.
METHODS
This was a prospective, randomised single-blind study. After Local Institutional Research and Ethical Committee approval and written informed consent from the participating patients, a total of 60 adults between 18 and 60 years age with the American Society of Anesthesiologsts' status I or II scheduled for elective primary inguinal hernia repair were included in the study. Patients with refusal to participate in the study, obesity with body mass index above 35 kg/m2, relevant drug allergy, pregnancy, alcohol or drug abuse, infection at the site of injection, consumption of pain medications within 24 h before surgery, chronic hepatic or renal failure and deranged coagulation profile were not included in the study.
Patients were familiarised with the use of visual analogue scale (VAS) (0–10 cm) for the assessment of pain where 0 meant no pain and 10 was worst pain imaginable during preanaesthetic visit in the evening prior to surgery. They were premedicated with tablet alprazolam 0.25 mg and tablet ranitidine 150 mg at bed time and 2 h before surgery.
In the operating room, intravenous access was secured and standard monitors were attached including electrocardiogram (ECG), non-invasive blood pressure (NIBP) and pulse oximeter SpO2. A standard anaesthesia protocol was followed. Prior to preoxygenation, the patients received glycopyrrolate 0.2 mg intravenous (IV) and fentanyl 2 μg/kg IV. Anaesthesia was induced with propofol 2 mg/kg IV, and neuromuscular blockade achieved with atracurium 0.5 mg/kg IV. After ventilation for 3 min using isoflurane in oxygen, appropriate-sized supraglottic device was used to secure the airway. Anaesthesia was maintained using isoflurane 1 minimum alveolar concentration with a mixture of 67% nitrous oxide in oxygen. The patient was administered TAP or IIN/IHN block on the side of surgery, according to the group to which the patient was allocated using a computer-generated sequence of random numbers. In Group I (n = 30), patients were administered TAP block using 0.75% ropivacaine (3 mg/kg) to a maximum 25 mL and in Group II (n = 30), patients were administered IIN/IHN block using 10 mL 0.75% ropivacaine. SonoSite M-Turbo ultrasound machine with high frequency 38 × 13-6 MHz 40 mm broadband linear array probe was used. For TAP block, ultrasound probe was placed on the lateral abdominal wall cephalad to the iliac crest and caudal to the costal margin. The probe was tilted as necessary in cephalad or caudal direction until a clear optimized image of the three lateral abdominal muscles and TAP was obtained. The needle tip was then targeted in TAP plane between internal oblique and transversus abdominis muscles using in plane technique, and the drug was administered. For IIN/IHN block, the probe was placed obliquely on a line joining anterior superior iliac spine and the umbilicus immediately superior to anterior superior iliac spine. After identifying the plane between internal oblique and transversus abdominis muscle, needle tip was targeted in the plane and the drug was administered. Surgery was commenced after administration of block. After the surgery, residual neuromuscular blockade was antagonised with neostigmine IV and glycopyrrolate IV at appropriate doses. The supraglottic airway device was removed when the patient was fully awake and breathing spontaneously.
A standard post-operative analgesia regimen was used in the 24 h immediate post-operative period. The patients received tramadol 2 mg/kg IV if VAS ≥4 in the first 4 h after the surgery. For persistent VAS ≥4 in this period, diclofenac 75 mg IV was administered. After 4 h, patients were administered oral diclofenac 75 mg if VAS ≥4. Injection ondansetron (4 mg) IV was given for post-operative nausea and vomiting. Total analgesic consumption in the 24 h postoperative period was the primary objective of the study.
Demographic data consisting of age, sex, weight, height and body mass index were recorded. Haemodynamic parameters such as non-invasive blood pressure and heart rate were monitored and recorded before induction, before administering the block, before the incision and after the incision. They were recorded intra-operatively at an interval of 10 min up to first 30 min and at 15 min thereafter. Number of attempts taken to administer the block, time taken to administer the block, any complications such as vessel puncture, bowel perforation, and femoral anaesthesia, if present were recorded in addition to duration of the surgery.
The patients were interviewed at 0, 0.5, 1, 1.5, 2, 4, 6, 8, 10, 19, and 24 h after surgery. VAS scores at rest and at knee flexion, duration after which first analgesic was demanded by the patient, incidence of nausea, vomiting and number of patients receiving ondansetron as well as the overall patient satisfaction was also observed.
The data were analysed using Statistical Package for Social Sciences (SPSS) version 20.0 (IBM Corp. Released 2011. IBM SPSS Statistics for windows, Version 20.0. Armonk, NY: IBM Corp.). For continuous variables, paired or unpaired student t-test was done and for categorical data, Chi-square test or Fisher test (whichever applicable) was done. VAS pain score was analysed using Mann–Whitney U-test. A probability of P < 0.05 was considered statistically significant.
We conducted the study on a convenience sample of 60 patients.
RESULTS
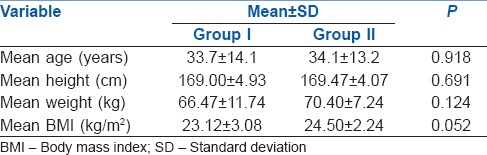
Mean age, mean height, mean weight and mean body mass index were comparable in both the groups. No statistical difference was found in the two groups [Table 1].
Table 1.
Demographic profile
The time taken for block was measured from the time that the ultrasound probe was placed on the abdomen till the time that the needle was withdrawn out of the abdomen. The average time taken for administering the block was 3.53 ± 1.06 min in Group I and 4.73 ± 0.69 min in Group II. The duration ranged from 3 to 7 min in Group I while it was 4–6 min in Group II. Using independent t-test, this difference was found to be very significant (P < 0.001).
A single insertion and withdrawal of needle were considered as a single attempt at block. If the needle was withdrawn and reinserted, this was counted as a second attempt. Out of thirty patients, 28 patients (93.33%) were administered the block in a single attempt and 2 (6.67%) in the second attempt in Group I. In Group II, four patients (13.33%) required 2 attempts while 26 patients (86.67%) were blocked in a single attempt. The average numbers of attempts taken were 1.07 ± 0.25 in Group I and 1.13 ± 0.35 in Group II. Using the t-test, this was not found statistically significant (P > 0.05).
The VAS score at rest and at knee flexion was assessed immediately post-operatively, followed by 30 min intervals till 2 h post-operatively and 2 h intervals till 10 h post-operatively. This was also assessed at 19 h and 24 h post-operatively.
The mean VAS score at rest was lower in Group II than in Group I at all time frames. This difference attained significant value at 2 h post-operatively and remained significantly lower till 8 h post-operatively. The difference was not statistically significant at other points of time (P > 0.05). The increase in VAS score from baseline value of the same group reached a statistically significant value at 2 h in Group I and 6 h in Group II [Table 2].
Table 2.
Variation of visual analogue scale at rest with time
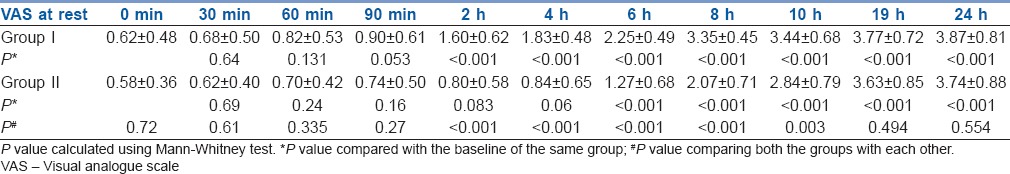
The mean VAS score at knee flexion was lower in Group II than in Group I at all time frames. This difference attained statistical significance at 2 h post-operatively and remained significantly lower till 10 h post-operatively. The increase in VAS score from baseline value of the same group reached a statistically significant difference at 2 h in Group I and 6 h in Group II [Table 2].
The average time after which rescue analgesia was required was 319.8 ± 115.2 min in Group I and 408 ± 116.4 min in Group II. The duration ranged from 2 to 8 h in Group I while it was 4–10 h in Group II. Using independent t-test, this difference was found to be statistically significant (P < 0.05) [Table 3].
Table 3.
Rescue analgesia
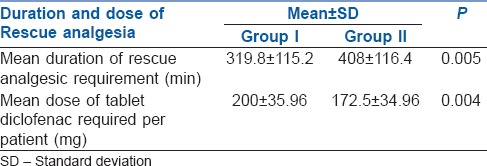
The number of patients who required injection tramadol in the first four post-operative hours was 7 (23.33%) in Group I and 2 (6.67%) in Group II. This difference was not statistically significant (P > 0.05). No patient in Group I or Group II needed IV diclofenac. The average dose of tablet diclofenac was 200 ± 35.96 mg in Group I and 172.5 ± 34.96 mg in Group II. This difference was found to be significant (P = 0.04). The power of the study to detect a difference in total consumption of oral diclofenac of 27.5 mg with the within group standard deviation was 0.85 (85%)., with an alpha error of 0.05. Two patients (6.67%) in Group I required ondansetron for nausea associated with tramadol injection. No patient in Group II required ondansetron. This difference was not statistically significant.
Two patients (6.67%) in Group II developed haematoma and two patients (6.67%) in Group I complained of nausea. No patients in either group suffered from any other complications.
Patient satisfaction was assessed using a 2-point scale, after enquiring from the patient about their willingness to have the same analgesia if ever operated again.
1= (Good): 'If ever operated again in the future, I want the same analgesia'
2= (Bad): 'If ever operated again in the future, I want a different analgesia.'
Twenty patients in Group I and 28 in Group II were satisfied with the block; however, the difference was not statistically significant (P > 0.05).
DISCUSSION
Post-operative pain remains grossly undertreated with up to 70% of patients reporting moderate-to-severe pain following surgery.[12] Pain control is essential for improvement of the quality of patient care. Regional nerve block techniques offer a great degree of post-operative pain relief, thus facilitating early ambulation and discharge. Greater success can be achieved using ultrasound by more accurate placement of reduced volumes of local anaesthetic agents closer to the targeted nerves.[13,14]
The mean dose of oral diclofenac required was 200 ± 35.96 mg in Group I and 172.5 ± 34.96 mg in Group II. This difference was found to be statistically significant. Although we used a convenience sample of 60 patients, our study had sufficient power to detect the observed difference in the consumption of oral diclofenac. These findings are contrasting to those of Petersen et al., who studied the post-operative analgesic effect of TAP block and ilioinguinal block in ninety patients undergoing inguinal hernia repair. The TAP block was evaluated versus placebo and versus ilioinguinal block and wound infiltration. They found no significant differences in morphine or ketobemidone consumption in the first 24 h between the groups that received TAP block and ilioinguinal block for post-operative analgesia.[11] These observations are also contrasting to those of Aveline et al., who conducted a study in 273 patients undergoing inguinal hernia repair surgery who were randomly allocated to receive either ultrasound-guided TAP block or blind IHN block with levobupivacaine 0.5% before surgery. They found that post-operative morphine requirements were lower in the TAP group in the first 24 h.[10] TAP block in both the studies was performed under ultrasound guidance. However, neither of them used ultrasound guidance for IHN block which could be a cause of reduced efficacy of block.
In the immediate post-operative period and up to 90 min after surgery, the VAS at rest was comparable in both the groups. However, at 2 h and up to 8 h thereafter, the group which received IIN/IHN block had a significantly lower VAS score at rest than the group which received TAP block (P < 0.05). Thereafter, though the VAS score remained lower in IIN/IHN group, the difference was not found to be statistically significant. A similar trend was seen in VAS at knee flexion, where the VAS score was comparable in the two groups till 90 min after surgery. This difference was significant at 2 h and up to 10 h post-operatively. Thereafter, the VAS score at knee flexion was comparable in both the groups till 24 h. Hence, the patients who received IIN/IHN block were found to be more comfortable than those who received TAP block in the first 24 h. The VAS both at rest and at knee flexion increased with time in the two groups. In the TAP group, the VAS at rest was significantly higher than the baseline value of VAS after 2 h and remained so till 24 h. In the IIN/IHN group, the VAS at rest was significantly higher than the baseline value after 6 h and remained so till 24 h. The VAS at knee flexion was also found to be significantly higher than the baseline at 2 h up to 24 h in TAP group and at 6 h up to 24 h in IIN/IHN group.
These findings correlate with those of Petersen et al., who found that pain scores for the first area under curve 6 h (AUC6 h) were significantly lower in group IIN than in group TAP both at rest and on coughing. However, they found that VAS pain scores calculated for the first 24 h as AUC24 h both while coughing and at rest demonstrated no significant differences among the three groups – group TAP, group infiltration (wound infiltration with ilioinguinal block) and group placebo.[11] This could be attributed to the performance of blind ilioinguinal block and absence of ultrasound to confirm the placement of needle in their study.
These observations are in contrast to those of Aveline et al., who found that patients who received TAP block expressed significantly less pain at rest for VAS scores at 4, 12, and 24 h.[10] However, in their study also, the IHN block was performed blindly and it is likely that in some patients, local anaesthetic solution could have been distributed into the subcutaneous layer or within muscle planes causing lesser efficacy of block.
There were two incidents of haematoma formation in Group II, and none of the other known complications were observed in either group. Petersen et al. also found no complications in the patients in group TAP, but three patients in the group which received blind ilioinguinal block had partial paralysis of thigh musculature.[11]
All the patients except two were satisfied with the pain relief achieved in Group II. However, ten patients in Group I were not satisfied with the analgesia achieved post-operatively. The number of patients who were satisfied with the anaesthetic technique in the two groups were comparable.
One of the limitations of present study was the absence of assessment points from 10 h to 19 h post-operatively and we, therefore, have limited information on any differences between the groups during this period. Long-term follow-up of patients was not done, and differences between the two groups regarding incidence and severity of chronic post-surgical pain could not be compared.
CONCLUSION
Ultrasound guided ilioinguinal and iliohypogastric nerve block reduces the postoperative analgesic consumption compared to ultrasound guided transversus abdominis plane block in patients undergoing elective primary inguinal herniorrhaphy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the help of Dr. Hemant Kamal, Department of Urology, University of Health Sciences, Rohtak, Haryana, and Dr. Saloni Kapoor, Department of Ophthalmology, All India Institute of Medical Sciences, New Delhi, India.
REFERENCES
- 1.Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, et al. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia. 2011;15:239–49. doi: 10.1007/s10029-011-0798-9. [DOI] [PubMed] [Google Scholar]
- 2.PROSPECT collaboration. Joshi GP, Rawal N, Kehlet H, Bonnet F, Camu F, Fischer HB, et al. Evidence-based management of postoperative pain in adults undergoing open inguinal hernia surgery. Br J Surg. 2012;99:168–85. doi: 10.1002/bjs.7660. [DOI] [PubMed] [Google Scholar]
- 3.Ding Y, White PF. Post-herniorrhaphy pain in outpatients after preincision ilioinguinal-iliohypogastric nerve block during monitored anaesthesia care. Can J Anesth. 1995;42:12–5. doi: 10.1007/BF03010564. [DOI] [PubMed] [Google Scholar]
- 4.Bugedo GJ, Cárcamo CR, Mertens RA, Dagnino JA, Muñoz HR. Preoperative percutaneous ilioinguinal and iliohypogastric nerve block with 0.5% bupivacaine for post-herniorrhaphy pain management in adults. Reg Anesth. 1990;15:130–3. [PubMed] [Google Scholar]
- 5.Toivonen J, Permi J, Rosenberg PH. Effect of preincisional ilioinguinal and iliohypogastric nerve block on postoperative analgesic requirement in day-surgery patients undergoing herniorrhaphy under spinal anaesthesia. Acta Anaesthesiol Scand. 2001;45:603–7. doi: 10.1034/j.1399-6576.2001.045005603.x. [DOI] [PubMed] [Google Scholar]
- 6.Demirci A, Efe EM, Türker G, Gurbet A, Kaya FN, Anil A, et al. Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: Comparison of the anatomical landmark and ultrasound guided techniques. Rev Bras Anestesiol. 2014;64:350–6. doi: 10.1016/j.bjan.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Bærentzen F, Maschmann C, Jensen K, Belhage B, Hensler M, Børglum J, et al. Ultrasound-guided nerve block for inguinal hernia repair: A randomized, controlled, double-blind study. Reg Anesth Pain Med. 2012;37:502–7. doi: 10.1097/AAP.0b013e31825a3c8a. [DOI] [PubMed] [Google Scholar]
- 8.Venkatraman R, Abhinaya RJ, Sakthivel A, Sivarajan G. Efficacy of ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing inguinal hernia repair. Local Reg Anesth. 2016;9:7–12. doi: 10.2147/LRA.S93673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frassanito L, Pitoni S, Gonnella G, Alfieri S, Del Vicario M, Catarci S, et al. Utility of ultrasound-guided transversus abdominis plane block for day-case inguinal hernia repair. Korean J Anesthesiol. 2017;70:46–51. doi: 10.4097/kjae.2017.70.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aveline C, Le Hetet H, Le Roux A, Vautier P, Cognet F, Vinet E, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–6. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 11.Petersen PL, Mathiesen O, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, et al. The effect of transversus abdominis plane block or local anaesthetic infiltration in inguinal hernia repair: A randomised clinical trial. Eur J Anaesthesiol. 2013;30:415–21. doi: 10.1097/EJA.0b013e32835fc86f. [DOI] [PubMed] [Google Scholar]
- 12.Pyati S, Gan TJ. Perioperative pain management. CNS Drugs. 2007;21:185–211. doi: 10.2165/00023210-200721030-00002. [DOI] [PubMed] [Google Scholar]
- 13.Willschke H, Marhofer P, Bösenberg A, Johnston S, Wanzel O, Cox SG, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30. doi: 10.1093/bja/aei157. [DOI] [PubMed] [Google Scholar]
- 14.Willschke H, Bösenberg A, Marhofer P, Johnston S, Kettner S, Eichenberger U, et al. Ultrasonographic-guided ilioinguinal/iliohypogastric nerve block in pediatric anesthesia: What is the optimal volume? Anesth Analg. 2006;102:1680–4. doi: 10.1213/01.ane.0000217196.34354.5a. [DOI] [PubMed] [Google Scholar]


