Abstract
Background
Optimal methods of mortality risk stratification in patients in the cardiac intensive care unit (CICU) remain uncertain. We evaluated the ability of the Sequential Organ Failure Assessment (SOFA) score to predict mortality in a large cohort of unselected patients in the CICU.
Methods and Results
Adult patients admitted to the CICU from January 1, 2007, to December 31, 2015, at a single tertiary care hospital were retrospectively reviewed. SOFA scores were calculated daily, and Acute Physiology and Chronic Health Evaluation (APACHE)‐III and APACHE‐IV scores were calculated on CICU day 1. Discrimination of hospital mortality was assessed using area under the receiver‐operator characteristic curve values. We included 9961 patients, with a mean age of 67.5±15.2 years; all‐cause hospital mortality was 9.0%. Day 1 SOFA score predicted hospital mortality, with an area under the receiver‐operator characteristic curve value of 0.83; area under the receiver‐operator characteristic curve values were similar for the APACHE‐III score, and APACHE‐IV predicted mortality (P>0.05). Mean and maximum SOFA scores over multiple CICU days had greater discrimination for hospital mortality (P<0.01). Patients with an increasing SOFA score from day 1 and day 2 had higher mortality. Patients with day 1 SOFA score <2 were at low risk of mortality. Increasing tertiles of day 1 SOFA score predicted higher long‐term mortality (P<0.001 by log‐rank test).
Conclusions
The day 1 SOFA score has good discrimination for short‐term mortality in unselected patients in the CICU, which is comparable to APACHE‐III and APACHE‐IV. Advantages of the SOFA score over APACHE include simplicity, improved discrimination using serial scores, and prediction of long‐term mortality.
Keywords: Acute Physiology and Chronic Health Evaluation score, cardiac critical care, cardiac intensive care unit, critical care, intensive cardiac care unit, intensive care unit, mortality, risk prediction, Sequential Organ Failure Assessment score
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Mortality/Survival, Quality and Outcomes, Clinical Studies
Clinical Perspective
What Is New?
This is the first study to validate the Sequential Organ Failure Assessment (SOFA) score, a simple illness severity score used to predict mortality in general critically ill patients, for prediction of mortality in a large cohort of patients in the cardiac intensive care unit (CICU).
The SOFA score on the first CICU day had good discrimination for hospital mortality and could stratify postdischarge mortality risk among hospital survivors.
Discrimination of hospital mortality was improved by calculating day‐to‐day changes in the SOFA score or using mean or maximum values of multiple daily SOFA scores.
What Are the Clinical Implications?
Risk stratification of patients in the CICU using the SOFA score on the first and subsequent CICU days allows identification of both low‐ and high‐risk patients, which may facilitate triage decisions and improve outcome prognostication.
Quantifying changes in daily SOFA scores over time provides a useful method of linking the response to treatment to future clinical outcomes for critically ill patients in the CICU.
The SOFA score allows risk stratification of patients in the CICU independent of admission diagnosis, allowing illness severity to be quantified in patients with undifferentiated or multisystemic acute illnesses.
Introduction
Risk prediction models have been important in acute cardiac care since Killip and Kimball reported the first risk‐stratification paradigm for patients with acute myocardial infarction 50 years ago.1 Since then, the cardiac intensive care unit (CICU) population has evolved to include an increasingly heterogeneous and complex mix of acute and chronic multiorgan dysfunction with superimposed cardiac pathological features.2, 3, 4, 5 Similarities between CICU and other ICU populations are growing, with an increasing prevalence of multisystem critical illnesses in patients in the CICU.2, 5, 6 Appropriate risk stratification models are, therefore, needed to optimize patient selection for CICU admission and to predict adverse outcomes to allow for effective care planning and therapeutic intervention.3, 4, 7 Disease‐specific risk prediction models have been derived, but many patients in the CICU have undifferentiated clinical syndromes with multiple acute and chronic cardiovascular disease processes.2, 6, 7, 8
ICU severity of illness scoring models identify high‐risk patients independent of their underlying disease process or clinical presentation.9, 10 The Sequential Organ Failure Assessment (SOFA) score was introduced to describe organ failure severity in patients with sepsis, including a 4‐point assessment of dysfunction in each of 6 organ systems (central nervous system, cardiovascular, respiratory, renal, liver, and coagulation; Table S1).10, 11, 12 In patients with sepsis, a SOFA score ≥2 reflects clinically relevant organ dysfunction and an increased risk of adverse outcomes.13 The SOFA score has been validated in critically ill patients with diseases other than sepsis, including a small CICU population.12, 14 Advantages of the SOFA score compared with other ICU risk scores include its simplicity and ease of use, allowing it to be calculated daily at bedside without complex algorithms to demonstrate clinical improvement or deterioration over time. Daily trends in the SOFA score can predict adverse outcomes, because an increase in SOFA score over time reflects progressive organ failure and higher risk of death.10, 13, 15
The purpose of this study was to evaluate the ability of the SOFA score to predict short‐ and long‐term mortality in a large cohort of unselected patients in the CICU and to determine if the SOFA score could differentiate high‐ and low‐risk patient populations, with the goal of improving future CICU triage protocols.
Methods
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure. This study was approved by the Mayo Clinic Institutional Review Board under an exception from informed consent as posing minimal risk to patients. This was a historical cohort analysis using an institutional database of patients admitted to the CICU at the Mayo Clinic Hospital, St Mary's Campus, a tertiary‐care hospital in Rochester, MN. The CICU at this facility is a single, 16‐bed, closed CICU in which all admissions are triaged, accepted, and cared for by a board‐certified cardiologist (J.C.J.), with comanagement by an intensivist for patients with respiratory failure. Unique adult patients ≥18 years old admitted to the CICU between January 1, 2007, and December 31, 2015, were identified by searching the archived electronic health records; data from the first CICU admission were used for patients subsequently readmitted during the same hospitalization.16 Patients still hospitalized on December 31, 2015, were excluded. According to Minnesota state law statute 144.295, patients must give consent before being included in observational research studies; patients who did not provide Minnesota Research Authorization were excluded from the study.
Demographic and laboratory data and use of invasive and noninvasive ventilation and continuous renal replacement therapy were collected. Daily SOFA scores and individual organ subscores were automatically generated for all patients in the CICU from data in the electronic medical record system, following imputation of missing variables to normal as the default.17 Acute Physiology and Chronic Health Evaluation (APACHE)‐III scores and APACHE‐IV predicted mortality were automatically generated for all patients in the CICU from data in the electronic medical record system from the first 24 hours of CICU admission.18, 19 Charlson Comorbidity Index was calculated electronically.20 Hospital disposition, length of stay, and all‐cause mortality were determined using electronic review of medical records for notification of patient death and last follow‐up date. Mortality data were extracted from Mayo Clinic electronic databases, the state of Minnesota electronic death certificates, and the Rochester Epidemiology Project database, as previously described.21
The primary end point of the study was all‐cause hospital mortality; secondary end points included CICU mortality, 30‐day mortality, and postdischarge mortality. Categorical variables are reported as number (percentage), and the χ2 test was used to compare groups. Continuous variables are reported as mean±SD, and Student t test was used to compare groups. ANOVA and χ2 tests were used to compare >2 groups for continuous and categorical variables, respectively. Trends in categorical variables were assessed using the Cochran‐Armitage trend test. Univariate analysis was performed using continuous variables as predictors of mortality, and the area under the receiver‐operator characteristic curve (AUROC) values were determined from this analysis; the optimal cutoff for predicting mortality was defined as that with the highest value of Youden's J index (sensitivity+specificity−1). P<0.05 was considered statistically significant, receiver‐operating curves were calculated via 2000 bootstrap samples, and all AUROC comparisons were performed using DeLong's method. A logistic regression model was created to determine calibration of the SOFA score using the Hosmer‐Lemeshow statistic. Long‐term survival in patients discharged alive from the hospital as a function of day 1 SOFA score tertile was assessed using Kaplan‐Meier survival analysis, with groups compared using the log‐rank test. Statistical analyses were performed using JMP, version 10.0 (SAS Institute, Cary, NC), and R, version 3.2.0 (https://www.r-project.org).
Results
We screened 12 904 adult admissions to the CICU during the study period; 2900 patients were excluded (1877 readmissions, 755 patients with no Minnesota Research Authorization, and 268 patients admitted outside of the study period). The primary admission diagnoses included acute coronary syndrome (n=3101 [31%]), arrhythmia (n=2001 [20%]), heart failure (n=1801 [18%]), respiratory failure (n=1551 [16%]), acute renal failure (n=568 [5%]), cardiac arrest (n=250 [3%]), and sepsis (n=710 [7%]).
Day 1 SOFA scores were available in 9961 patients (99.6%), who composed the final study population. Baseline characteristics are shown in Table 1. The mean±SD day 1 SOFA score was 3.45±3.15, with a median of 2 (25th/75th percentile, 1.5) (Figure 1). CICU mortality occurred in 557 patients (5.6%), and hospital mortality occurred in 893 patients (9.0%); and 1127 patients (11.3%) died within 30 days after CICU admission (Figure 2). Hospital nonsurvivors were older, had more comorbidities, and had more frequent use of mechanical ventilation and continuous renal replacement therapy (Table 1).
Table 1.
Baseline Characteristics of Included Patients With Available Day 1 SOFA Score, Including Hospital Survivors and Inpatient Deaths
| Variable | No. With Available Data | Overall (n=9961) | Hospital Survivors (n=9404) | Nonsurvivors (n=893) | P Value (Survivors vs Deaths) |
|---|---|---|---|---|---|
| Age, y | 9961 | 67.5±15.2 | 67.0±15.3 | 72.1±13.8 | <0.001 |
| Female sex | 9961 | 3732 (37.5) | 3373 (37.2) | 359 (40.2) | 0.0767 |
| White race | 9961 | 9201 (92.4) | 8390 (92.5) | 811 (90.8) | 0.0670 |
| Admission source | 9961 | <0.001 | |||
| Procedural laboratory | 3967 (39.8) | 3760 (41.5) | 207 (23.2) | ||
| Transfer | 2713 (27.2) | 2429 (26.8) | 284 (31.8) | ||
| Emergency department | 1393 (14.0) | 1219 (13.4) | 174 (19.5) | ||
| Floor | 1599 (16.1) | 1415 (15.6) | 184 (20.6) | ||
| Other | 289 (2.9) | 245 (2.7) | 44 (4.9) | ||
| Prior myocardial infarction | 9935 | 1972 (19.8) | 1778 (19.7) | 194 (21.7) | 0.1408 |
| Prior heart failure | 9935 | 1949 (19.6) | 1706 (18.9) | 243 (27.2) | <0.001 |
| Prior diabetes mellitus | 9935 | 2823 (28.4) | 2525 (27.9) | 298 (33.4) | <0.001 |
| Prior lung disease | 9935 | 1935 (19.5) | 1714 (19.0) | 221 (24.8) | <0.001 |
| Prior cancer | 9935 | 2121 (21.4) | 1873 (20.7) | 248 (27.8) | <0.001 |
| Prior stroke | 9935 | 1227 (12.4) | 1074 (11.9) | 153 (17.1) | <0.001 |
| Prior moderate‐severe CKD | 9935 | 2021 (20.3) | 1767 (19.5) | 254 (28.4) | <0.001 |
| CCI (with age) | 9935 | 5.6±3.3 | 5.5±3.3 | 6.9±3.4 | <0.001 |
| CCI (excluding age) | 9935 | 2.4±2.6 | 2.3±2.6 | 3.2±3.0 | <0.001 |
| BMI, kg/m2 | 9845 | 29.5±7.1 | 29.5±7.0 | 29.7±8.0 | 0.3851 |
| CICU LOS, d | 9961 | 2.5±4.6 | 2.4±4.6 | 3.1±4.2 | <0.001 |
| Hospital LOS, d | 9961 | 7.9±13.2 | 7.8±1.24 | 9.0±19.3 | 0.0683 |
| Invasive ventilator use | 9961 | 1605 (16.1) | 1125 (12.4) | 480 (53.8) | <0.001 |
| Invasive ventilator use, d | 9961 | 0.35±1.47 | 0.27±1.28 | 1.21±2.58 | <0.001 |
| Noninvasive ventilator use | 9961 | 1489 (14.9) | 1286 (14.2) | 203 (22.7) | <0.001 |
| Noninvasive ventilator use, d | 9961 | 0.19±0.84 | 0.17±0.79 | 0.37±1.20 | <0.001 |
| Vasopressor/inotrope use CICU day 1 | 9957 | 1767 (17.8) | 1286 (14.2) | 481 (53.9) | <0.001 |
| CRRT use | 9961 | 167 (1.7) | 84 (0.9) | 83 (9.3) | <0.001 |
| APACHE‐III score | 9961 | 61.2±25.6 | 58.0±21.7 | 93.8±34.2 | <0.001 |
| APACHE‐IV predicted mortality | 9961 | 0.170±0.200 | 0.142±0.165 | 0.450±0.290 | <0.001 |
| Day 1 | |||||
| SOFA score | 9961 | 3.45±3.15 | 3.03±2.69 | 7.68±4.19 | <0.001 |
| Respiratory SOFA | 3119 | 2.53±1.05 | 2.43±0.97 | 2.91±1.05 | <0.001 |
| Coagulation SOFA | 9300 | 0.33±0.64 | 0.31±0.61 | 0.54±0.85 | <0.001 |
| Hepatic SOFA | 2651 | 0.36±0.74 | 0.60±0.97 | 0.32±0.68 | <0.001 |
| Cardiovascular SOFA | 9942 | 1.25±0.89 | 1.15±0.76 | 2.22±1.35 | <0.001 |
| Central nervous system SOFA | 9673 | 0.35±0.94 | 0.26±0.78 | 1.33±1.66 | <0.001 |
| Renal SOFA | 9429 | 0.83±1.12 | 0.74±1.05 | 1.76±1.36 | <0.001 |
| Day 2 SOFA score | 6792 | 2.94±2.77 | 2.62±2.42 | 6.56±3.72 | <0.001 |
| Maximum day 1–2 SOFA score | 9961 | 3.71±3.22 | 3.27±2.74 | 8.15±4.17 | <0.001 |
| Mean day 1–2 SOFA score | 9961 | 3.19±2.87 | 2.77±2.36 | 7.39±3.98 | <0.001 |
| Change in SOFA (day 1 to day 2) | 6792 | −0.76±2.21 | −0.74±2.09 | −0.94±3.28 | 0.1779 |
| Day 1 SOFA <2 | 9961 | 3579 (35.9) | 3525 (38.9) | 54 (6.0) | <0.001 |
| Increasing day 2 SOFA | 6792 | 1334 (19.6) | 1171 (18.8) | 163 (29.5) | <0.001 |
| Admission systolic blood pressure, mm Hg | 9911 | 123.1±26.2 | 124.1±25.9 | 112.9±28.2 | <0.001 |
| Admission diastolic blood pressure, mm Hg | 9606 | 69.4±17.0 | 69.9±16.7 | 64.2±19.1 | <0.001 |
| Admission mean blood pressure, mm Hg | 9606 | 83.5±18.1 | 84.1±17.6 | 77.8±21.1 | <0.001 |
| Admission heart rate, bpm | 9912 | 82.1±23.4 | 81.4±23.2 | 89.5±23.6 | <0.001 |
| Admission shock index, bpm/mm Hg | 9911 | 0.70±0.27 | 0.68±0.26 | 0.83±0.29 | <0.001 |
| Admission respiratory rate | 9574 | 18.4±5.7 | 18.2±5.6 | 20.8±6.4 | <0.001 |
| Admission oxygen saturation, % | 9908 | 95.7±6.0 | 96.1±5.1 | 92.1±11.3 | <0.001 |
Data are presented as mean±SD or number (percentage). APACHE indicates Acute Physiology and Chronic Health Evaluation; BMI, body mass index; bpm, beats per minute; CICU, cardiac intensive care unit; CCI, Charlson Comorbidity Index; CKD, chronic kidney disease; CRRT, continuous renal replacement therapy; LOS, length of stay; and SOFA, Sequential Organ Failure Assessment.
Figure 1.
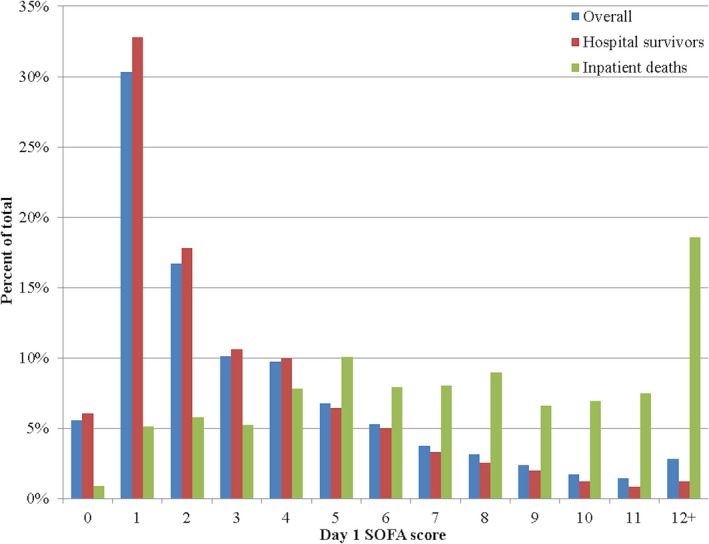
Distribution of day 1 Sequential Organ Failure Assessment (SOFA) scores, as a percentage of overall population, hospital survivors, and inpatient deaths. P<0.001 between groups.
Figure 2.
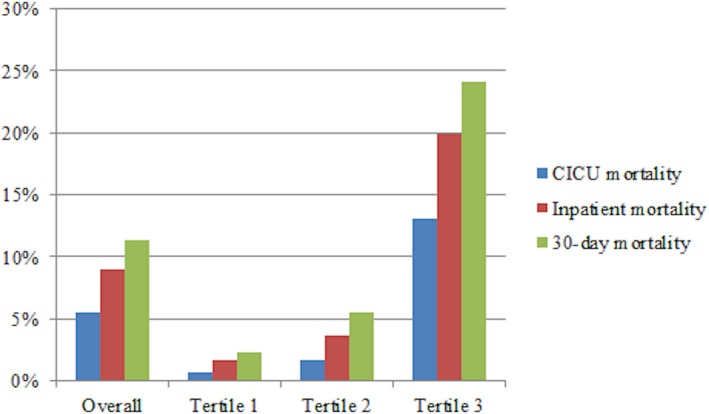
Short‐ and intermediate‐term mortality as a function of day 1 Sequential Organ Failure Assessment (SOFA) score tertile. Tertile 1 includes patients with day 1 SOFA score <2, tertile 2 includes patients with day 1 SOFA score of 2 to 3, and tertile 3 includes patients with day 1 SOFA score ≥4. P<0.001 between groups. CICU indicates cardiac intensive care unit.
The mean day 1 SOFA score was higher in patients who died in the hospital (7.67 versus 3.03; P<0.001), and these patients had a distribution of day 1 SOFA scores that was shifted towards higher values (Figure 1). Short‐term mortality increased significantly with increasing day 1 SOFA score tertile (day 1 SOFA score <2 versus 2 to 3 versus ≥4; P<0.001 for trend), as shown in Figure 2. Short‐term mortality rates increased progressively with an increasing day 1 SOFA score (Figure 3), and day 1 SOFA score was a significant univariate predictor of hospital mortality (Table 2). The 3579 patients (35.9%) without significant organ failure (day 1 SOFA score <2) had a low risk of hospital mortality (1.51%; odds ratio, 0.101; P<0.001). Day 1 SOFA score predicted hospital mortality, with an optimal cutoff of ≥5 by AUROC analysis, corresponding to the top quartile of day 1 SOFA score (Table 2). A day 1 SOFA score ≥5 predicted hospital mortality (24.5% versus 3.1%; odds ratio, 10.18; 95% confidence interval, 8.68–11.94; P<0.001). The 2736 patients (27.5%) with day 1 SOFA score ≥5 accounted for 80.8% of patients who died in the CICU and 75.0% of patients who died in the hospital.
Figure 3.
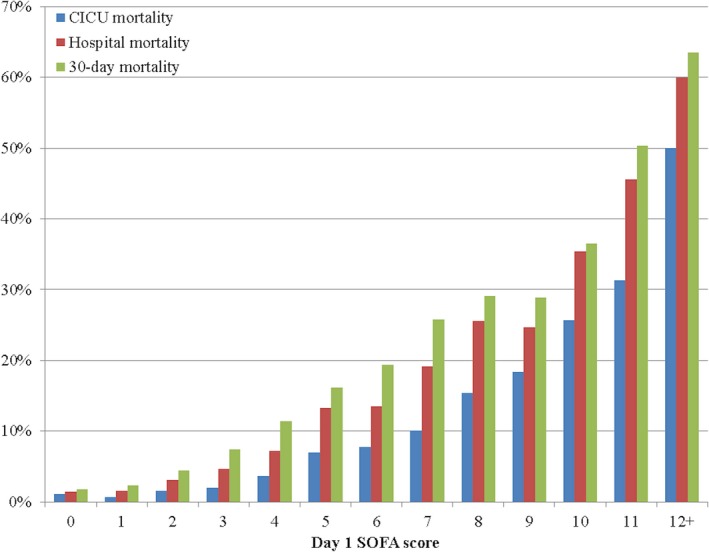
Short‐term mortality stratified by day 1 Sequential Organ Failure Assessment (SOFA) score. CICU indicates cardiac intensive care unit.
Table 2.
Univariate Analysis of SOFA and APACHE Scores for Prediction of Short‐Term Mortality
| Variable | CICU Mortality | Hospital Mortality | ||||||
|---|---|---|---|---|---|---|---|---|
| Unit OR | 95% CI | AUROC | 95% CI | Unit OR | 95% CI | AUROC | 95% CI | |
| Day 1 SOFA | 1.441 | 1.408–1.476 | 0.852 | 0.835–0.870 | 1.417 | 1.389–1.446 | 0.828 | 0.813 to 0.843 |
| Day 2 SOFA | 1.498 | 1.448–1.551 | 0.857 | 0.835–0.878 | 1.455 | 1.415–1.498 | 0.821 | 0.803 to 0.840 |
| Maximum day 1–2 SOFA | 1.472 | 1.437–1.509 | 0.867 | 0.850–0.883 | 1.435 | 1.406–1.465 | 0.837 | 0.822 to 0.851 |
| Mean day 1–2 SOFA | 1.545 | 1.504–1.589 | 0.876 | 0.860–0.892 | 1.517 | 1.482–1.553 | 0.847 | 0.833 to 0.861 |
| Maximum day 1–3 SOFA score | 1.489 | 1.453–1.527 | 0.875 | 0.859–0.891 | 1.444 | 1.415–1.475 | 0.842 | 0.828 to 0.857 |
| Mean day 1–3 SOFA score | 1.596 | 1.552–1.644 | 0.886 | 0.870–0.901 | 1.569 | 1.531–1.610 | 0.856 | 0.842 to 0.869 |
| Maximum day 1–7 SOFA score | 1.498 | 1.462–1.537 | 0.881 | 0.865–0.897 | 1.452 | 1.422–1.483 | 0.849 | 0.835 to 0.863 |
| APACHE‐III | 1.049 | 1.046–1.052 | 0.847 | 0.829–0.865 | 1.047 | 1.044–1.050 | 0.823 | 0.808 to 0.838 |
| APACHE‐IV | 179.1 | 130.3–247.5 | 0.859 | 0.843–0.876 | 141.5 | 107.0–188.0 | 0.834 | 0.820 to 0.849 |
Daily SOFA scores were only available for patients remaining in the CICU for at least part of a given day. APACHE indicates Acute Physiology and Chronic Health Evaluation; AUROC, area under the receiver‐operator characteristic curve; CI, confidence interval; CICU, cardiac intensive care unit; OR, odds ratio; and SOFA, Sequential Organ Failure Assessment.
Mean APACHE‐III score and APACHE‐IV predicted mortality were higher in patients who died in the hospital (P<0.001) (Table 1), and APACHE‐III and APACHE‐IV were significant univariate predictors of hospital mortality (Table 2). AUROC values for day 1 SOFA score did not differ from either APACHE‐III or APACHE‐IV for predicting ICU mortality or hospital mortality (all P>0.05). On the basis of the Hosmer‐Lemeshow statistic, calibration for probabilities produced by a logistically transformed day 1 SOFA score was acceptable (P=0.11) for CICU mortality and suboptimal (P<0.05) for hospital mortality (Figure S1).
A total of 3169 patients (31.8%) left the CICU on day 1, including 239 (7.5%) who died; 6792 patients (68.2%) remained in the CICU on day 2, and 3829 patients (38.4%) remained in the CICU on day 3. Maximum and mean SOFA scores for day 1 and day 2 (substituting the day 1 SOFA score if no day 2 SOFA score was available) had significantly higher AUROC values for hospital mortality than day 1 SOFA score (Table 2). The maximum and mean daily SOFA scores during the first 3 CICU days (substituting day 1 or day 2 SOFA scores in patients who left the CICU before day 3) and the maximum daily SOFA score over the first 7 CICU days had significantly higher AUROC values for hospital mortality than mean or maximum day 1 to 2 SOFA scores (Table 2). Mean SOFA score over days 1 to 3 had the highest AUROC value for hospital mortality, followed by maximum SOFA score over the first 7 CICU days (Table 2). All significant comparisons yielded P<0.01 by the DeLong test.
The mean±SD change in SOFA scores between day 1 and day 2 was −0.76±2.21. Characteristics of patients with increasing (n=1334 [19.6%]), decreasing (n=3157 [46.5%]), or unchanged (n=2301 [33.9%]) SOFA score from day 1 to day 2 are shown in Table 3. Hospital mortality was significantly higher in patients with an increasing day 2 SOFA score than in patients with a declining day 2 SOFA score (P<0.001; Figure 4), despite similar mean day 1+day 2 SOFA score and maximum week 1 SOFA score and lower APACHE‐III score and APACHE‐IV predicted mortality (Table 3). Patients with unchanged SOFA score from day 1 to day 2 were at the lowest risk.
Table 3.
Baseline Characteristics and Outcomes of Patients Based on Change in SOFA Score From Day 1 to Day 2
| Variable | No Change in SOFA (n=2301) | Decreasing SOFA (n=3157) | Increasing SOFA (n=1334) | Left CICU on Day 1 (n=3169) | P Value |
|---|---|---|---|---|---|
| Age, y | 66.7±15.1 | 68.0±15.1 | 68.2±14.9 | 67.2±15.5 | 0.0040 |
| Female sex | 888 (38.6) | 1166 (36.9) | 489 (36.7) | 1189 (37.5) | 0.5717 |
| White race | 2144 (93.2) | 2937 (93.0) | 1221 (91.5) | 2899 (91.5) | 0.0295 |
| Admission source | <0.001 | ||||
| Procedural laboratory | 925 (40.2) | 1077 (34.1) | 571 (42.8) | 1394 (44.0) | |
| Transfer | 653 (28.4) | 977 (31.0) | 380 (28.5) | 703 (22.2) | |
| Emergency department | 340 (14.8) | 492 (15.6) | 169 (12.7) | 392 (12.4) | |
| Floor | 332 (14.4) | 509 (16.1) | 175 (13.1) | 583 (18.4) | |
| Other | 51 (2.2) | 102 (3.2) | 39 (2.9) | 97 (3.1) | |
| Prior myocardial infarction | 467 (20.3) | 643 (20.4) | 289 (21.8) | 573 (18.2) | 0.0216 |
| Prior heart failure | 400 (17.4) | 747 (23.7) | 254 (19.1) | 548 (17.5) | <0.001 |
| Prior diabetes mellitus | 671 (26.8) | 989 (31.4) | 384 (28.9) | 833 (26.4) | <0.001 |
| Prior lung disease | 415 (18.1) | 632 (20.1) | 259 (19.5) | 629 (19.9) | 0.2589 |
| Prior cancer | 469 (20.4) | 719 (22.8) | 282 (21.2) | 651 (20.6) | 0.0992 |
| Prior stroke | 263 (11.4) | 422 (13.4) | 159 (12.0) | 383 (12.1) | 0.1560 |
| Prior moderate‐severe CKD | 415 (18.1) | 781 (24.8) | 254 (19.1) | 571 (18.1) | <0.001 |
| CCI | 5.4±3.2 | 6.0±3.4 | 5.7±3.2 | 5.5±3.4 | <0.001 |
| BMI, kg/m2 | 29.4±7.1 | 29.7±7.1 | 29.4±6.7 | 29.4±7.2 | 0.2639 |
| CICU LOS, d | 3.1±5.5 | 3.3±4.8 | 3.8±6.2 | 0.7±0.3 | <0.001 |
| Hospital LOS, d | 7.7±10.7 | 9.5±16.9 | 9.6±14.7 | 5.7±8.9 | <0.001 |
| Invasive ventilator use | 180 (7.8) | 840 (26.6) | 251 (18.8) | 334 (10.5) | <0.001 |
| Invasive ventilator use, d | 0.26±1.51 | 0.62±1.83 | 0.62±1.94 | 0.03±0.13 | <0.001 |
| Noninvasive ventilator use | 304 (13.2) | 712 (22.6) | 246 (18.4) | 227 (7.2) | <0.001 |
| Noninvasive ventilator use, d | 0.21±0.92 | 0.28±0.97 | 0.33±1.22 | 0.02±0.09 | <0.001 |
| Vasopressor/inotrope use on CICU day 1 | 930 (29.5) | 192 (14.4) | 439 (13.9) | 209 (9.0) | <0.001 |
| CRRT use | 31 (1.4) | 68 (2.2) | 59 (4.4) | 9 (0.3) | <0.001 |
| APACHE‐III score | 55.4±19.3 | 69.4±26.4 | 60.5±22.6 | 57.5±26.8 | <0.001 |
| APACHE‐IV predicted mortality | 0.124±0.145 | 0.233±0.228 | 0.164±0.182 | 0.141±0.197 | <0.001 |
| Day 1 SOFA score | 2.32±2.17 | 5.07±3.34 | 2.82±2.68 | 2.91±3.10 | <0.001 |
| Day 2 SOFA score | 2.32±2.17 | 2.60±2.68 | 4.80±3.08 | NA | <0.001 |
| Maximum day 1+day 2 SOFA score | 2.32±2.17 | 5.07±3.34 | 4.79±3.08 | 2.91±3.10 | <0.001 |
| Mean day 1+day 2 SOFA score | 2.32±2.17 | 3.84±2.89 | 3.81±2.80 | 2.91±3.10 | <0.001 |
| Change in SOFA score (day 1 to day 2) | 0.00±0.00 | −2.47±1.80 | 1.97±1.38 | NA | <0.001 |
| Maximum week 1 SOFA score | 2.65±2.52 | 5.19±3.42 | 5.13±3.34 | 2.91±3.10 | <0.001 |
| Day 1 SOFA score <2 | 1162 (50.5) | 428 (13.6) | 567 (42.5) | 1422 (44.9) | <0.001 |
| Admission systolic blood pressure, mm Hg | 123.7±24.8 | 120.8±27.2 | 125.6±26.5 | 123.9±26.2 | <0.001 |
| Admission heart rate, bpm | 80.6±22.3 | 83.6±23.8 | 83.3±24.7 | 81.0±23.0 | <0.001 |
| Admission shock index, bpm/mm Hg | 0.68±0.26 | 0.73±0.27 | 0.69±0.27 | 0.68±0.27 | <0.001 |
| Admission oxygen saturation, % | 96.2±4.8 | 95.3±6.2 | 95.8±5.7 | 95.7±6.7 | <0.001 |
Patients without a day 2 SOFA score are classified as “left CICU on day 1.” P values are for the χ2 test (categorical variables) or ANOVA (continuous variables). APACHE indicates Acute Physiology and Chronic Health Evaluation; BMI, body mass index; bpm, beats per minute; CCI, Charlson Comorbidity Index; CICU, cardiac intensive care unit; CKD, chronic kidney disease; CRRT, continuous renal replacement therapy; LOS, length of stay; NA, not applicable; and SOFA, Sequential Organ Failure Assessment.
Figure 4.
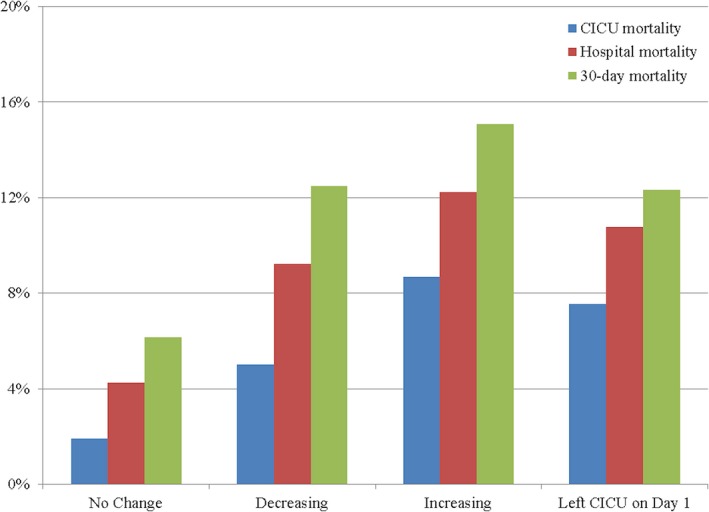
Short‐term mortality as a function of change in Sequential Organ Failure Assessment (SOFA) score from day 1 to day 2. Patients without a day 2 SOFA score are classified as “left cardiac intensive care unit (CICU) on day 1.” P<0.001 between groups.
Data were available to calculate the cardiovascular, coagulation, central nervous system, and renal SOFA subscores in >90% of patients, whereas data to calculate the respiratory and liver SOFA subscores were available in fewer than one third of patients (Table 1). Each of the individual SOFA organ subscores was higher in patients who died in the hospital (all P<0.001), and each SOFA organ subscore was a univariate predictor of hospital mortality (all P<0.001). The distribution of day 1 SOFA subscores for each organ system in the overall population is shown in Figure 5; the distribution of organ system subscores differed between hospital survivors and nonsurvivors (P<0.001 by χ2 test). The cardiovascular and renal SOFA subscores had the highest odds ratio and AUROC values for hospital mortality using the original data, and the respiratory and cardiovascular SOFA subscores had the highest odds ratio and AUROC values when missing subscore data were imputed as normal (Table 4).
Figure 5.
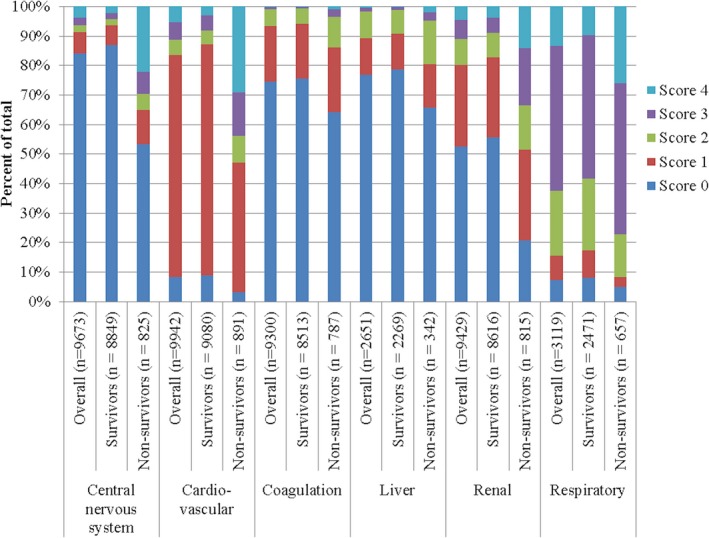
Distribution of day 1 Sequential Organ Failure Assessment organ system subscores in the overall population, hospital survivors, and hospital nonsurvivors (P<0.001 between hospital survivors and hospital nonsurvivors).
Table 4.
Univariate Analysis of Individual Day 1 SOFA Organ Subscores for Prediction of Short‐Term Mortality, as a Function of Whether Missing Data Were Imputed as Normal (Subscore Value of 0)
| SOFA Subscore | WITHOUT Missing Data Imputed as Normal | WITH Missing Data Imputed as Normal | ||||||
|---|---|---|---|---|---|---|---|---|
| CICU Mortality | Hospital Mortality | CICU Mortality | Hospital Mortality | |||||
| Unit OR | AUROC | Unit OR | AUROC | Unit OR | AUROC | Unit OR | AUROC | |
| Respiratory | 1.861 | 0.650 | 1.689 | 0.637 | 2.086 | 0.769 | 1.952 | 0.742 |
| Coagulation | 1.515 | 0.561 | 1.556 | 0.563 | 1.386 | 0.540 | 1.450 | 0.546 |
| Liver | 1.440 | 0.563 | 1.536 | 0.571 | 1.777 | 0.544 | 1.897 | 0.546 |
| Cardiovascular | 2.875 | 0.775 | 2.484 | 0.720 | 2.765 | 0.757 | 2.421 | 0.708 |
| Central nervous system | 2.137 | 0.712 | 1.981 | 0.680 | 2.029 | 0.683 | 1.906 | 0.659 |
| Renal | 1.888 | 0.730 | 1.845 | 0.721 | 1.729 | 0.683 | 1.722 | 0.685 |
AUROC indicates area under the receiver‐operator characteristic curve; CICU, cardiac intensive care unit; OR, odds ratio; and SOFA, Sequential Organ Failure Assessment.
Hospital discharge disposition was available for 6328 of hospital survivors (69.7%): home in 4643 (73.4%), long‐term care facility in 1375 (21.7%), rehabilitation facility in 150 (2.4%), and acute‐care hospital in 93 (1.5%). A total of 2934 (32.4%) of 9068 hospital survivors died during a median follow‐up of 1.64 years (25th–75th percentile, 0.25–4.17); 2326 hospital survivors (25.6%) had follow‐up of <1 year. Patients with a day 1 SOFA score <2 had higher long‐term postdischarge survival by Kaplan‐Meier analysis (P<0.001 by log‐rank test). Increasing tertile of day 1 SOFA score was associated with lower long‐term postdischarge survival by Kaplan‐Meier analysis (Figure 6; P<0.001 by log‐rank test).
Figure 6.
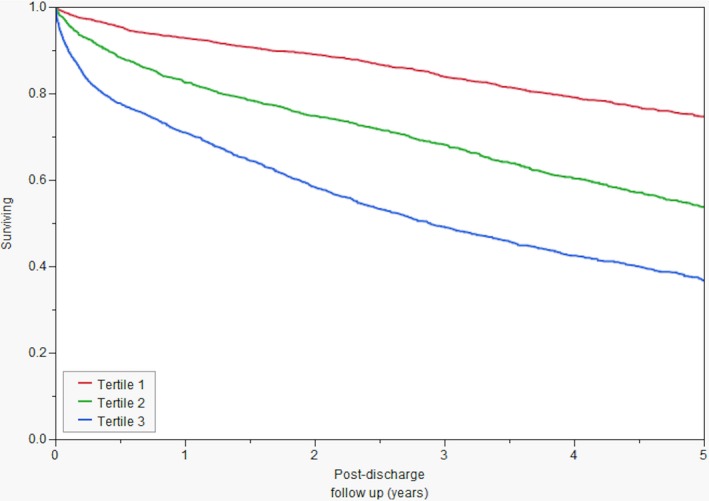
Kaplan‐Meier survival curves for hospital survivors, by day 1 Sequential Organ Failure Assessment (SOFA) score tertile. Tertile 1 includes patients with day 1 SOFA score <2, tertile 2 includes patients with day 1 SOFA score of 2 to 3, and tertile 3 includes patients with day 1 SOFA score ≥4. P<0.001 between groups by log‐rank test.
Discussion
This is the largest study examining the prognostic value of SOFA scores for short‐ and long‐term mortality in a contemporary CICU population, demonstrating a continuous increase in mortality as a function of increasing day 1 SOFA score. Day 1 SOFA score had good discrimination for short‐term mortality, and the discriminative ability was further improved by using the maximum and mean SOFA scores over the first 2 to 3 CICU days. The day 1 SOFA score had similar discrimination for short‐term mortality compared with the APACHE‐III and APACHE‐IV scoring models. Patients with increasing SOFA scores between day 1 and day 2 had an increased risk of short‐term mortality. The cardiovascular and renal SOFA subscores were the strongest predictors of mortality among the SOFA organ subscores. Patients without significant organ failure (ie, SOFA score <2) on CICU day 1 were at low risk for death during hospitalization and long‐term follow‐up after hospital discharge. Stratification of hospital survivors by tertiles of day 1 SOFA score demonstrated significant differences in long‐term survival.
These results demonstrate the utility of the SOFA score for mortality prediction in patients in the CICU, even without considering other potentially relevant prognostic variables, such as age and diagnosis.12 The SOFA score can adequately risk stratify complex or undifferentiated patients in the CICU, even if disease‐specific risk scores continue to be useful in patients with clearly defined disease processes.7, 8 Progressive organ failure (as reflected by an increase in SOFA scores between day 1 and day 2) predicted higher mortality. The maximum and mean SOFA score over the first 2 to 3 CICU days had greater discrimination when compared with the day 1 SOFA score alone; mean daily SOFA scores were superior to maximum daily SOFA scores in our population.12 Therefore, the day 1 SOFA score provides useful early risk prediction; subsequent SOFA scores can be assessed each day to provide improved risk stratification, with the mean daily SOFA score providing the best discrimination for patients remaining in the CICU for multiple days. In addition, the change in SOFA score over time provides useful data on the progression of organ failure and clinical response to therapy. The increased risk associated with an elevated SOFA score on CICU day 1 persisted throughout follow‐up, and even minimal organ failure (day 1 SOFA score ≥2) increased the risk of death at all time points.
Although it is tempting to suggest that the SOFA score can help in clinical decision making about the need for aggressive intervention or candidacy for advanced therapies by identifying patients at high risk of death, caution is warranted when applying population‐based risk scores to individual patients.9 If confirmed prospectively, the low short‐term mortality risk conferred by a low day 1 SOFA score (<2) may imply that a subset of these patients could be safely cared for outside of a CICU setting. Long‐term survival was lower for hospital survivors with higher tertiles of day 1 SOFA score, showing the relevance of organ dysfunction for determining long‐term outcomes.
The only other published study we identified examining the SOFA score in patients in the CICU was recently reported by Argyriou et al.14 This small study of 300 patients in the CICU from Greece during 2010 through 2012 showed excellent discrimination of the day 1 SOFA score for CICU mortality (AUROC, 0.88) and hospital mortality (AUROC, 0.90), compared with AUROC values in the present study of 0.85 and 0.83, respectively.14 Similar to our study, Argyriou et al demonstrated equivalent discrimination for day 1 SOFA score and the older APACHE‐II score.14 The population in the study by Argyriou et al had double the prevalence of acute coronary syndromes (two thirds versus one third in our population), and a markedly higher mortality rate both in the CICU (18.3% versus 5.6%) and hospital (23.7% versus 9.1%), despite a modestly higher mean SOFA score (4.1 versus 3.5).14 Unlike the study by Argyriou et al,14 we examined long‐term outcomes, allowing us to report a novel association between day 1 SOFA score and postdischarge survival.
A prior study by Janssens et al reported on the predictive value of the SOFA score in 303 medical patients in the ICU with predominantly cardiovascular disorders; although this was not a true CICU population, the reported AUROC value of 0.82 for day 1 SOFA as a predictor of hospital mortality is similar to the value observed in our study.22 The AUROC values for day 1 SOFA and maximum and mean day 1 to 3 SOFA scores in the present study are compatible with those reported in prior studies in other ICU populations, as reviewed by Minne et al.12 Minne et al found superior discrimination for APACHE scores compared with SOFA score, whereas we demonstrated equivalent discrimination for day 1 SOFA score compared with both APACHE‐III and APACHE‐IV.12 The good discrimination provided by the SOFA score in this CICU population likely reflects the ability of the SOFA score to differentiate the large majority of low‐risk patients with single‐organ dysfunction from the important minority of truly critically ill patients with multiorgan failure who account for most hospital deaths. In addition, the 2 major forms of organ failure in the CICU, cardiovascular and renal, are strongly associated with mortality and readily identified by the respective SOFA subscores.
The most important advantages of the SOFA score remain the simplicity and ease of use, allowing calculation at the bedside, with mortality discrimination similar to more complex scores.10, 12, 14 The SOFA score can be calculated daily, and changes over time have important prognostic relevance.12, 15 Although the SOFA score excludes age and diagnosis‐ and procedure‐related data, the admission diagnosis can contribute substantially to the accuracy of mortality prediction by other models.9 Nonetheless, AUROC values for hospital mortality in this unselected CICU population compare favorably with those previously reported for the acute coronary syndrome–specific Global Registry of Acute Coronary Events risk score.7 The organ failure variables included in the SOFA score are reflective of those commonly seen in sepsis and may be less relevant in other critical illnesses. Unlike the APACHE scoring system, the SOFA score was not designed to predict mortality and does not differentiate between acute and chronic organ dysfunction.9, 10 Lack of a specific mortality‐prediction algorithm for the SOFA score limits assessment of calibration, which was suboptimal for hospital mortality on the basis of our analysis.9 We chose not to perform multiple imputation for missing variables to demonstrate the real‐world performance of the SOFA score in our population, representing a lower estimate of model discriminative ability.
This single‐center, historical, cohort study has several limitations, including unmeasured confounding and potential bias attributable to local practice patterns and a patient population that may be distinct from other centers. CICU and hospital death rates in this study were lower than in prior CICU studies, with a lower rate of acute coronary syndromes than in most prior studies; these factors may influence mortality prediction by the SOFA score.2, 5, 6, 14 Holland and Moss describe a similar patient population with a significant burden of noncardiac illnesses and a lower proportion of acute coronary syndromes.6 Serial SOFA scores were only available for patients remaining in the CICU, limiting our assessment of SOFA score changes over time. The variables needed to calculate the SOFA score were not available for all patients, so we imputed the missing variables as normal; in particular, the respiratory SOFA subscore was calculated only for patients with arterial blood gas measurements.17 This is a significant limitation for interpreting the predictive value of the individual SOFA subscores for mortality, particularly considering the effects of imputing missing data as normal for these subscores. Prior studies have shown that missing variables in prognostic scores for critically ill patients can lead to underestimation of mortality risk.23 Patient‐level admission diagnoses were not available, preventing diagnosis‐specific analysis of the predictive performance of the SOFA score. Because of inconsistent documentation, we were unable to obtain Killip classification to calculate the Global Registry of Acute Coronary Events risk score for comparison.7 Resuscitation status was not available, although this may not substantially affect mortality prediction by APACHE models.19 The use of electronic health record review to determine patient death may underestimate postdischarge mortality by potentially failing to capture patients dying in other health systems.
In conclusion, the SOFA score can be easily applied to modern patients in the CICU using an electronic algorithm. The discrimination of the day 1 SOFA score for short‐term mortality was comparable to the APACHE scoring system in this large contemporary cohort of unselected patients in the CICU. Patients with a SOFA score <2 on the first CICU day had a low risk of death during follow‐up. Maximum and mean SOFA scores over the first 3 CICU days strongly predicted mortality, and patients with an increasing SOFA score between CICU day 1 and day 2 were at increased risk of death. Further research is needed to determine the optimal ways to use the prognostic information provided by this established ICU risk score in CICU populations.
Disclosures
None.
Supporting information
Table S1. Calculating the SOFA Score and Individual Organ Sub‐Scores
Figure S1. Observed vs predicted hospital mortality based on probabilities produced by a logistically transformed Day 1 SOFA score.
Acknowledgments
We acknowledge the dedicated physicians and nurses who care for our patients in the cardiac intensive care unit every day.
(J Am Heart Assoc. 2018;7:e008169 DOI: 10.1161/JAHA.117.008169.)29525785
This work was presented in abstract form at the American College of Cardiology Scientific Sessions, March 17 to 19, 2017, in Washington, DC.
References
- 1. Killip T III, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol. 1967;20:457–464. [DOI] [PubMed] [Google Scholar]
- 2. Katz JN, Shah BR, Volz EM, Horton JR, Shaw LK, Newby LK, Granger CB, Mark DB, Califf RM, Becker RC. Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. 2010;38:375–381. [DOI] [PubMed] [Google Scholar]
- 3. Katz JN, Minder M, Olenchock B, Price S, Goldfarb M, Washam JB, Barnett CF, Newby LK, van Diepen S. The genesis, maturation, and future of critical care cardiology. J Am Coll Cardiol. 2016;68:67–79. [DOI] [PubMed] [Google Scholar]
- 4. Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, Kuvin JT, Lopez‐Sendon J, McAreavey D, Nallamothu B, Page RL II, Parrillo JE, Peterson PN, Winkelman C; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Council on Quality of Care and Outcomes Research . Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126:1408–1428. [DOI] [PubMed] [Google Scholar]
- 5. Casella G, Cassin M, Chiarella F, Chinaglia A, Conte MR, Fradella G, Lucci D, Maggioni AP, Pirelli S, Scorcu G, Visconti LO; BLITZ‐3 Investigators . Epidemiology and patterns of care of patients admitted to Italian Intensive Cardiac Care units: the BLITZ‐3 registry. J Cardiovasc Med (Hagerstown). 2010;11:450–461. [DOI] [PubMed] [Google Scholar]
- 6. Holland EM, Moss TJ. Acute noncardiovascular illness in the cardiac intensive care unit. J Am Coll Cardiol. 2017;69:1999–2007. [DOI] [PubMed] [Google Scholar]
- 7. Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, De Van, Werf F, Avezum A, Goodman SG, Flather MD, Fox KA; Global Registry of Acute Coronary Events Investigators . Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. [DOI] [PubMed] [Google Scholar]
- 8. Fonarow GC. Clinical risk prediction tools in patients hospitalized with heart failure. Rev Cardiovasc Med. 2012;13:e14–e23. [DOI] [PubMed] [Google Scholar]
- 9. Keegan MT, Gajic O, Afessa B. Severity of illness scoring systems in the intensive care unit. Crit Care Med. 2011;39:163–169. [DOI] [PubMed] [Google Scholar]
- 10. Vincent JL, Moreno R. Clinical review: scoring systems in the critically ill. Crit Care. 2010;14:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG;on behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis‐related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–710. [DOI] [PubMed] [Google Scholar]
- 12. Minne L, Abu‐Hanna A, de Jonge E. Evaluation of SOFA‐based models for predicting mortality in the ICU: a systematic review. Crit Care. 2008;12:R161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, Pilcher DV; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE) . Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in‐hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317:290–300. [DOI] [PubMed] [Google Scholar]
- 14. Argyriou G, Vrettou CS, Filippatos G, Sainis G, Nanas S, Routsi C. Comparative evaluation of Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment scoring systems in patients admitted to the cardiac intensive care unit. J Crit Care. 2015;30:752–757. [DOI] [PubMed] [Google Scholar]
- 15. Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. [DOI] [PubMed] [Google Scholar]
- 16. Herasevich V, Pickering BW, Dong Y, Peters SG, Gajic O. Informatics infrastructure for syndrome surveillance, decision support, reporting, and modeling of critical illness. Mayo Clin Proc. 2010;85:247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aakre C, Franco PM, Ferreyra M, Kitson J, Li M, Herasevich V. Prospective validation of a near real‐time EHR‐integrated automated SOFA score calculator. Int J Med Inform. 2017;103:1–6. [DOI] [PubMed] [Google Scholar]
- 18. Chandra S, Kashyap R, Trillo‐Alvarez CA, Tsapenko M, Yilmaz M, Hanson AC, Pickering BW, Gajic O, Herasevich V. Mapping physicians' admission diagnoses to structured concepts towards fully automatic calculation of acute physiology and chronic health evaluation score. BMJ Open. 2011;1:e000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Keegan MT, Gajic O, Afessa B. Comparison of APACHE III, APACHE IV, SAPS 3, and MPM0III and influence of resuscitation status on model performance. Chest. 2012;142:851–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Singh B, Singh A, Ahmed A, Wilson GA, Pickering BW, Herasevich V, Gajic O, Li G. Derivation and validation of automated electronic search strategies to extract Charlson comorbidities from electronic medical records. Mayo Clin Proc. 2012;87:817–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ III. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Janssens U, Graf C, Graf J, Radke PW, Konigs B, Koch KC, Lepper W, Vom Dahl J, Hanrath P. Evaluation of the SOFA score: a single‐center experience of a medical intensive care unit in 303 consecutive patients with predominantly cardiovascular disorders: Sequential Organ Failure Assessment. Intensive Care Med. 2000;26:1037–1045. [DOI] [PubMed] [Google Scholar]
- 23. Afessa B, Keegan MT, Gajic O, Hubmayr RD, Peters SG. The influence of missing components of the Acute Physiology Score of APACHE III on the measurement of ICU performance. Intensive Care Med. 2005;31:1537–1543. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Calculating the SOFA Score and Individual Organ Sub‐Scores
Figure S1. Observed vs predicted hospital mortality based on probabilities produced by a logistically transformed Day 1 SOFA score.


