Abstract
Background
The purpose of this study was to examine associations between several types of police‐recorded crime (violent, nonviolent, and homicide) and cardiometabolic health (obesity and elevated blood pressure [BP]), and to determine if associations were modified by age and sex.
Methods and Results
We analyzed cross‐sectional data (N=14 799 patients) from 3 primary care clinics at an academic medical center in Chicago, IL. Patient‐level health data were obtained from the electronic health record (June 1, 2014–May 31, 2015), including body mass index and BP, and linked to the City of Chicago Police Data Portal. Geocoded crime counts were aggregated to census tract and calculated as the annual crime rate per 1000 population. Generalized linear mixed models were used to assess obesity and BP status as a function of crime rate quartile, controlling for patient, clinic, and neighborhood characteristics. Median violent crime rates in each quartile ranged from 15 to 84 per 1000 population. Median age was 56 years (interquartile range, 38–72 years); 42% of patients were obese and 33% had elevated BP. Compared with patients living in the lowest quartile, patients living in the highest quartile for violent crime had 53% higher adjusted odds of obesity (95% confidence interval, 1.15–2.03) and 25% higher adjusted odds of elevated BP (95% confidence interval, 1.01–1.56). In subanalyses examining homicide, a relatively rare event, exposure was not associated with obesity and was inconsistently associated with elevated BP.
Conclusions
In a densely populated, high‐poverty region in Chicago, recurrent exposure to high rates of violent crime was consistently associated with obesity and elevated BP, but rare exposure to homicide was not.
Keywords: epidemiology, high blood pressure, obesity, risk factors, women
Subject Categories: Obesity, High Blood Pressure, Epidemiology, Risk Factors, Women
Clinical Perspective
What Is New?
Small area analysis using objective measures revealed a consistent relationship between exposure to violent crime and cardiometabolic health (body mass index and blood pressure).
Associations between violent crime and cardiometabolic health were more pronounced among women.
Recurrent exposure to “everyday violent crime” may be more strongly associated with cardiometabolic health than a single exposure to severe violent crime.
What Are the Clinical Implications?
Exposure to violent crime may be an important social determinant of health in vulnerable populations.
In an era of population health, healthcare organizations located in high‐crime regions may have incentive to participate in violence prevention and intervention efforts.
Violent crime has increased in 13 major US cities since 2014, including Los Angeles, CA; Houston, TX; Baltimore, MD; and Chicago, IL.1 Affected communities have been disproportionately urban, with high levels of concentrated poverty and residential segregation by race.1, 2 These same communities have a high burden of chronic health conditions, especially obesity and hypertension, raising concern about the potential relationship between exposure to violent crime and risk of preventable and costly cardiometabolic diseases.3, 4
Prior studies have hypothesized that people living in neighborhoods with high rates of violent crime may experience high levels of psychological distress that result in adverse health behaviors and outcomes.5, 6 For instance, studies of US children have documented lower rates of physical activity and higher rates of obesity in unsafe neighborhoods.7, 8, 9 Sandy et al examined 36 936 US children and found that higher violent crime rates were associated with higher body mass index (BMI).8 However, studies of adult populations and BMI have been more mixed.7, 10 Lovasi et al examined a sample of 13 102 adult New York City residents and found no relationship between homicide rates and BMI.11 Other adult studies have documented mixed findings for physical activity and other metabolic health outcomes.12, 13
One possible explanation for these mixed findings is that many prior studies have assessed neighborhood crime using subjective self‐reported measures of neighborhood safety.7 However, self‐reported measures may be systematically biased by individual characteristics, including how people perceive crime or hear about crime in their neighborhood. Allostatic load theory explains how cumulative prolonged exposure to stressors (eg, frequently hearing gunshots at night) may activate physiologic response pathways that result in metabolic or autonomic dysfunction.14, 15 For instance, excess cortisol secretion, resulting from fear of violent crime, can impair glucose metabolism, promote abdominal fat deposition, and increase vascular reactivity.14, 15 These physiologic processes can occur unconsciously and may be difficult for individuals to quantify by self‐report.16, 17 Prior studies have also used self‐reported measures of health,7, 10 which may lead to significant underestimation of health effects in communities with lower education (eg, poor health literacy)18 and unreliable access to health care.19
Other studies have used objective measures of crime, but they have not examined the different types of crime encountered (eg, violent crime and homicide) or demographic groups targeted (eg, elderly people and women), limiting comparative inference.10 Stress responses may fundamentally differ by exposure type, and scholars have theorized that violent crimes may be more closely linked to fear‐based physiological processes than nonviolent crimes.10, 20 Similarly, responses may vary on the basis of a person's perceived risk for being targeted. Prior literature has suggested that women and elderly adults may be more vulnerable to fear of victimization and, often, victimization itself.7 Weinstein et al examined 12 767 adults and found that perceived safety was more strongly associated with physical activity in women than in men.21 These differences may be of special importance for identifying and reducing disparities in women's cardiovascular health, particularly among vulnerable populations.22
More important, linkages between neighborhood crime and hypertension have been understudied. Although several prior studies have used objective crime rates to examine associations with physical activity and obesity,10 fewer studies have used objective crime rates to examine associations with hypertension. In the most compelling study to date, Kaiser and colleagues used data from the Multi‐Ethnic Study of Atherosclerosis and found no relationship between self‐reported safety and incident hypertension, after adjusting for race/ethnicity.23 Although this study used objective blood pressure (BP) measurements to assess incident hypertension, it used a survey‐based method to assess neighborhood safety.23 Few studies, if any, have used objective measures of both crime and BP to examine this relationship.
Building on this prior work, this study uses objective measures to examine associations between several types of police‐recorded crime (violent, nonviolent, and homicide) and cardiometabolic health (obesity and elevated BP) in a large clinical sample of adults in Chicago. As a secondary objective, this study also examines if associations are modified by age and sex. We hypothesized that use of objective measures would reveal positive associations between neighborhood violent crime rates and obesity and BP status. On the basis of prior studies,7, 21 we also hypothesized stronger associations among women and elderly adults.
Methods
This study was conducted in a 324 census tract region on Chicago's south and west sides, a densely populated urban region with ≈992,000 residents, 58% of whom identified as non‐Hispanic black and 30% of whom identified as Hispanic or Latino. Many residents in this region were unemployed (21%) and/or living below the federal poverty level (30%).24 This study region was within the catchment area of clinical sites included in the parent study, CommunityRx, and was selected because of high rates of poverty and preventable illness in the target population. Our study population included all patients (N=14 799) living in the study region and seen in at least 1 of 3 primary care clinics at an urban academic medical center between June 1, 2014 and May 31, 2015. The only patients excluded from the CommunityRx study population were those who had a home address outside the study region; few were excluded because of missing covariate data (2.5%). The median sample size was 100 patients per census tract (interquartile range, 48–250 patients).
This study was conducted with a waiver of informed consent and approval from the University of Chicago (Chicago, IL) Institutional Review Board.
Data Sources and Measures
Geocoded crime counts were obtained from the City of Chicago Police Data Portal, a record of every incident of crime reported to or known by the Chicago Police Department. Data were publicly available and extracted weekly from the Chicago Police Department's Citizen Law Enforcement Analysis and Reporting system (https://data.cityofchicago.org). These data were linked to contemporaneous patient‐level data obtained from the CommunityRx database.25 The CommunityRx database included clinical information from the electronic health record systems of 3 primary care sites included in this study (internal medicine, obstetrics and gynecology, and geriatrics), including BMI and BP measurements.
The dependent variables were obesity and BP status. Obesity status was defined as BMI ≥30 kg/m2, and elevated BP was defined as systolic BP >140 mm Hg or diastolic BP >90 mm Hg. We chose to analyze BMI and BP as a binary outcome for clinical interpretability. For instance, a higher BP is not necessarily a poorer outcome unless it crosses the previously specified diagnostic threshold. However, we have included sensitivity analyses using continuous values for BMI and systolic BP in Table S1. The CommunityRx intervention, described in previously published work,25 was implemented during this study period; we thus abstracted the first recorded BMI and BP measured before the intervention to avoid any contamination effects. Standard procedure for the clinics represented in this study included a single BP measurement at the time of clinical encounter. Thus, those classified as having elevated BP included patients with aforementioned criteria, regardless of diagnosis status, including those who were diagnosed but uncontrolled. Patients who were classified as not having elevated BP included those with well‐controlled hypertension.
The independent variable in our analysis included all types of violent crime (assault, battery, criminal sexual assault, robbery, or homicide). We also included nonviolent crime (theft or criminal property crime) as a comparator group, reasoning that nonviolent crime should have a weaker relationship with health than violent crime. Crimes were classified as violent or nonviolent on the basis of the Chicago Police Department Crime Type Categories, derived from the Federal Bureau of Investigation's National Incident‐Based Reporting System.26 Nonviolent crime was limited to theft or criminal property crimes designated as “nonindex,” which are defined by the National Incident‐Based Reporting System as a “less serious offense.”26 Crime counts were aggregated to the census tract level and calculated as an annual crime rate per 1000 population; this rate was used as a proxy for individual exposure to crime. Census tracts were classified into 4 crime rate quartiles (low, medium, high, and very high) for each independent variable of interest (violent crime and nonviolent crime); each quartile contained 81 census tracts (Figure).
Figure 1.
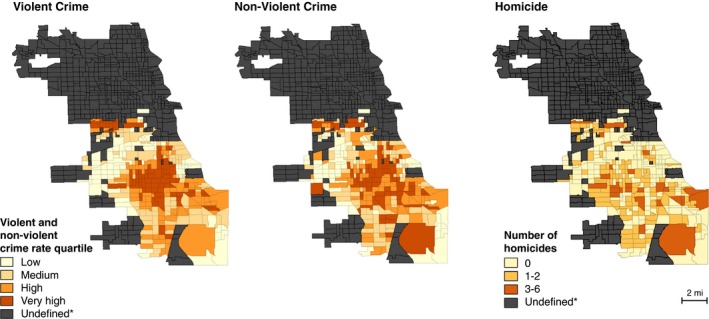
Distribution of crime types by census tract, South Side of Chicago, IL, from June 1, 2014 to May 31, 2015. *Undefined signifies census tracts outside the CommunityRx study area.
We additionally examined both the presence of and proximity to nearest homicide as independent variables, reasoning that homicide is an infrequent but potent violent crime (eg, high impact and media attention) and may be more likely to trigger psychological and physiological responses to violence (eg, stress and fear). Presence of homicide was defined as a dichotomous variable: no homicide or at least 1 homicide per census tract. Proximity to homicide was measured using euclidean distance from each patient's residential address to the nearest homicide. Even in census tracts with no homicide, proximity to each homicide in the data set (n=269) was considered, and distance to the nearest homicide was measured as a continuous value. Distances were subsequently categorized into 4 groups: >1, 0.5 to 1, 0.25 to 0.5, or <0.25 miles from the nearest homicide.
Covariates included patient demographic characteristics, including age (continuous), sex (male or female), self‐reported race/ethnicity (white non‐Hispanic, black non‐Hispanic, Hispanic or Latino, other race/ethnicity, and refused), and primary insurance status (private, Medicaid/Medicare, or none); clinic site (internal medicine, geriatrics, or gynecology); and neighborhood characteristics (2014 American Community Survey 5‐year estimates),24 including median household income (continuous), ≥25% less than high school graduation (dichotomous), ≥25% unemployed (dichotomous), ≥75% minority race/ethnicity (dichotomous), and ≥10% poor English fluency (dichotomous).
Statistical Analysis
Descriptive statistics were used to characterize the demographic and census tract characteristics of our sample. We fit generalized linear mixed models (logit link function) to assess obesity and BP status as a function of crime rate quartile for each crime category (violent crime and nonviolent theft or property crime). All analyses accounted for clustering at the census tract level with the inclusion of a random effect for census tract.
We included all theoretically relevant confounders in final adjusted models, including aforementioned sociodemographic characteristics, clinic site, and neighborhood characteristics. Notably, we adjusted for neighborhood unemployment, which has been shown in prior literature to be independently linked to both high rates of crime and poor health outcomes.27, 28 Similarly, we adjusted for English fluency as a proxy for immigration status, paying special attention to the Mexican immigrant communities on Chicago's South Side. Recent attention on immigration in the United States has led to growing awareness that immigrants are more likely to be victims of violent crime, related to underreporting because of fear of law or immigration enforcement.29 These same communities are often less likely to be insured,30 less likely to access health care,31 and more likely to have undiagnosed health conditions.32 We tested for multicollinearity between neighborhood‐level covariates using variance inflation factor; mean variance inflation factor was 1.50, with no values exceeding the standard threshold of 10.33 We additionally applied spline representations in a sensitivity analysis to adjust for age and median household income more flexibly; this analysis revealed no significant differences in the observed effect of violent crime for either obesity or elevated BP.
To further characterize the relationship between census tract‐level exposure to crime and obesity or BP status, we conducted exploratory interaction tests and subgroup analyses by sex (male or female) and age group (<65 or ≥65 years). The interaction effects were formally tested in the full model, with the reported sex‐specific findings based on subgroup‐restricted models. Statistical significance was defined as P<0.05.
We fit generalized linear mixed models to assess obesity and BP status as a function of census tract homicide (no homicide or at least 1 homicide) and proximity to homicide (>1, 0.5–1, 0.25–0.5, and <0.25 miles). Model implementation was identical to that previously described, controlling for patient demographic characteristics, clinic site, and neighborhood characteristics.
Using empirical Bayes means estimation, we generated histogram and Q‐Q plots to verify the assumption that the random effects were normally distributed. We also used bootstrap methods (500 replications) to examine robustness of the crime effect. Nonparametric bootstrap estimation was performed by resampling observations with replacement from the sample data in both a simple model and the fully specified model (mixed‐effects model with adjustment for all confounders). These analyses validated our primary findings. Data were analyzed using Stata/SE, version 15.0 (StataCorp LP, College Station, TX) and GeoDa, version 1.10.0.12.
Results
In a 324 census tract region of Chicago, median total crime rates in each quartile ranged from 54 to 240 crimes per 1000 population (Table 1). The quartile containing the lowest crime exposure had a median violent crime rate of 15 per 1000 population, similar to the national average rate of 19 per 1000 population.34 The quartile containing the highest crime exposure had a median violent crime rate of 84 per 1000 population (Figure), >4 times higher than the national average. Almost two thirds of census tracts (65%) had ≥25% residents living below the federal poverty level; more than a third (37%) had an unemployment rate of ≥25%; and more than a third (38%) had a high school graduation rate of <75%. More than half of census tracts (58.8%) were composed of a black non‐Hispanic majority population (≥75% of the population) (Table 1).
Table 1.
Characteristics of Census Tracts, South Side of Chicago, IL
| Demographic Composition(N=324 Census Tracts)a | Census Tracts, % |
|---|---|
| Below federal poverty level | |
| <25% | 34.7 |
| 25%–49% | 56.7 |
| ≥50% | 8.7 |
| High school graduation or higher | |
| <50% | 5.0 |
| 50%–74% | 32.5 |
| 75%–100% | 61.6 |
| Unemployment rate | |
| <25% | 62.8 |
| 25%–49% | 36.2 |
| ≥50% | 1.0 |
| Uninsurance rate | |
| <25% | 74.3 |
| 25%–49% | 25.7 |
| ≥50% | 0 |
| Black non‐Hispanic | |
| <25% | 28.2 |
| 25%–74% | 13.0 |
| 75%–100% | 58.8 |
| Hispanic or Latino | |
| <25% | 69.3 |
| 25%–74% | 15.4 |
| 75%–100% | 15.2 |
| Census Tract Quartiles | Median Census Tract Crime per 1000 Population (IQR) |
|---|---|
| Total crime | |
| Low | 54.0 (43.3–62.2) |
| Medium | 109.9 (93.6–121.9) |
| High | 162.1 (152.5–176.7) |
| Very high | 240.3 (216.9–271.0) |
| Nonviolent theft or property crime | |
| Low | 19.2 (15.7–21.7) |
| Medium | 37.8 (33.1–40.6) |
| High | 48.3 (45.2–52.1) |
| Very high | 64.4 (58.3–76.5) |
| Violent crime | |
| Low | 14.5 (11.7–17.1) |
| Medium | 32.7 (26.5–37.8) |
| High | 56.4 (48.8–60.0) |
| Very high | 84.1 (78.5–99.3) |
IQR indicates interquartile range.
Census tract data were abstracted from the 2014 American Community Survey (5‐year estimates) and reflect a densely populated study region of 992,000 residents.
Of the 14 799 patients included in this study, 42% were obese and 33% had elevated BP (Table 2). Most patients were aged ≥45 years (67.5%), women (76.8%), and black non‐Hispanic (72.4%); half had Medicaid and/or Medicare (Table 2).
Table 2.
Patient Characteristics From Primary Care Clinics
| Patient Characteristics (N=14 799)a | % of Patients |
|---|---|
| Age, y | |
| 18–24 | 6.9 |
| 25–34 | 12.9 |
| 35–44 | 12.8 |
| 45–54 | 13.7 |
| 55–64 | 16.0 |
| 65–74 | 16.3 |
| ≥75 | 21.5 |
| Sex | |
| Female | 76.8 |
| Male | 23.2 |
| Race | |
| White non‐Hispanic | 17.6 |
| Black non‐Hispanic | 72.4 |
| Hispanic or Latino | 4.1 |
| Other | 5.0 |
| Refused | 0.9 |
| Insurance status | |
| Private | 44.1 |
| Medicaid and/or Medicare | 51.0 |
| None or unknown | 5.0 |
| Weight status (BMI) | |
| Underweight (<18.5 kg/m2) | 2.1 |
| Normal weight (18.5–24.9 kg/m2) | 27.6 |
| Overweight (25–29.9 kg/m2) | 28.4 |
| Obese (≥30 kg/m2) | 41.9 |
| BP status, mm Hg | |
| Systolic BP <140 and diastolic BP <90 | 66.8 |
| Systolic BP ≥140 or diastolic BP ≥90 | 33.2 |
BMI indicates body mass index; and BP, blood pressure.
Patient data were abstracted from clinical visits recorded in the electronic health record between June 1, 2014 and May 31, 2015.
Compared with patients living in the lowest quartile, patients living in the highest quartile for violent crime rate had 53% higher adjusted odds of obesity (95% confidence interval [CI], 1.15–2.03) and 25% higher adjusted odds of elevated BP (95% CI, 1.01–1.56; Table 3). Patients living in the highest quartile for nonviolent theft or property crime had 41% higher adjusted odds of obesity (95% CI, 1.13–1.76); higher exposure to nonviolent theft or property crime was not significantly associated with BP status in adjusted models (Table 3).
Table 3.
Census Tract Crime and BMI or BP Status
| Crime Type | Obesity (BMI ≥30 kg/m2)(n=12 358)a | Elevated BP (SBP ≥140 or DBP ≥90 mm Hg)(n=14 331)b | ||||
|---|---|---|---|---|---|---|
| % | OR (95% CI) | AOR (95% CI)c | % | OR (95% CI) | AOR (95% CI)c | |
| Nonviolent crime rate quartile | ||||||
| Low | 24.8 | Reference | Reference | 24.1 | Reference | Reference |
| Medium | 44.2 | 1.89 (1.49–2.40)d | 1.57 (1.27–1.93)d | 32.8 | 1.33 (1.10–1.61)e | 1.09 (0.94–1.27) |
| High | 44.9 | 1.79 (1.42–2.25)d | 1.36 (1.10–1.68)e | 36.1 | 1.44 (1.20–1.73)d | 1.14 (0.97–1.33) |
| Very high | 48.7 | 1.82 (1.44–2.28)d | 1.41 (1.13–1.76)e | 36.6 | 1.44 (1.20–1.73)d | 1.15 (0.98–1.36) |
| Violent crime rate quartile | ||||||
| Low | 24.8 | Reference | Reference | 24.1 | Reference | Reference |
| Medium | 41.2 | 1.69 (1.35–2.10)d | 1.36 (1.07–1.73)f | 33.1 | 1.41 (1.19–1.69)d | 1.14 (0.95–1.37) |
| High | 50.0 | 2.07 (1.66–2.58)d | 1.52 (1.17–1.96)e | 38.6 | 1.71 (1.44–2.04)d | 1.24 (1.02–1.51)f |
| Very high | 50.3 | 2.10 (1.68–2.62)d | 1.53 (1.15–2.03)e | 36.2 | 1.51 (1.26–1.80)d | 1.25 (1.01–1.56)f |
| Presence of homicideg | ||||||
| No homicide | 36.7 | Reference | Reference | 30.0 | Reference | Reference |
| At least 1 homicide | 49.1 | 1.37 (1.17–1.60)d | 1.07 (0.95–1.21) | 37.7 | 1.28 (1.14–1.45)d | 1.16 (1.06–1.27)e |
| Proximity to nearest homicide, mile | ||||||
| >1 | 33.8 | Reference | Reference | 28.9 | Reference | Reference |
| >0.5–1 | 34.4 | 1.32 (1.01–1.71)f | 0.93 (0.72–1.20) | 29.4 | 1.16 (0.92–1.48) | 0.98 (0.78–1.24) |
| >0.25–0.5 | 44.7 | 1.46 (1.11–1.91)e | 0.96 (0.73–1.25) | 34.8 | 1.20 (0.94–1.53) | 1.01 (0.80–1.29) |
| ≤0.25 | 48.4 | 1.58 (1.19–2.08)e | 1.00 (0.76–1.32) | 36.3 | 1.24 (0.96–1.59) | 1.08 (0.84–1.38) |
AOR indicates adjusted OR; BMI, body mass index; BP, blood pressure; CI, confidence interval; DBP, diastolic BP; OR, odds ratio; and SBP, systolic BP.
Derived from height and weight measurements recorded in the electronic health record; standard definitions obtained from the Centers for Disease Control and Prevention.
Derived from systolic and diastolic BP measurements recorded in the electronic health record; standard definitions obtained from the Seventh Report of the Joint National Committee.
Estimates obtained from generalized linear mixed models. Adjusted for patient demographics, including age (continuous), sex, race, and insurance status; clinic site; and census tract characteristics, including median household income (continuous), ≥25% less than high school graduation, ≥25% unemployment, ≥75% minority racial/ethnic composition, and ≥10% poor English fluency.
P<0.001.
P<0.01.
P<0.05.
Presence of homicide on the basis of census tract of residence.
In adjusted models examining continuous values for BMI and systolic BP, patients living in the highest quartile for violent crime had, on average, 1.6 kg/m2 higher BMI (95% CI, 0.59–2.57 kg/m2; P=0.002) and 2.2 mm Hg higher systolic BP (95% CI, 0.32–4.02 mm Hg; P=0.02) compared with those living in the lowest quartile (Table S1).
In interaction tests by sex, living in a neighborhood with higher rates of violent crime had a larger effect on obesity rates among women than among their male counterparts (Χ2[3 df]=31.2; P<0.001); interaction tests were not statistically significant for elevated BP (Χ2[3 df]=7.4; P=0.06). In subgroup analyses, women living in the highest quartile for violent crime had 71% higher adjusted odds of obesity (95% CI, 1.25–2.35) than those living in the lowest quartile (Table 4). In interaction tests by age group, the associations between violent crime and obesity (Χ2[3 df]=28.0; P<0.001) or elevated BP (Χ2[3 df]=16.2; P=0.001) were weaker among elderly adults (aged ≥65 years) than among their nonelderly counterparts; however, effect sizes in adjusted models were similar between age groups in subgroup analyses (Table S2).
Table 4.
Subgroup Analysis by Sex: Census Tract Violent Crime and BMI or BP Status
| Violent Crime by Sex Crime Rate Quartile | Obesity (BMI ≥30 kg/m2) (n=12 358)a | Elevated BP (SBP ≥140 or DBP ≥90 mm Hg) (n=14 331)b | ||||
|---|---|---|---|---|---|---|
| % | OR (95% CI) | AOR (95% CI)c | % | OR (95% CI) | AOR (95% CI)c | |
| Men and women | ||||||
| Low | 24.8 | Reference | Reference | 24.1 | Reference | Reference |
| Medium | 41.2 | 1.69 (1.35–2.10)d | 1.36 (1.07–1.73)e | 33.1 | 1.41 (1.19–1.69)d | 1.14 (0.95–1.37) |
| High | 50.0 | 2.07 (1.66–2.58)d | 1.52 (1.17–1.96)f | 38.6 | 1.71 (1.44–2.04)d | 1.24 (1.02–1.51)e |
| Very high | 50.3 | 2.10 (1.68–2.62)d | 1.53 (1.15–2.03)f | 36.2 | 1.51 (1.26–1.80)d | 1.25 (1.01–1.56)e |
| Women only | ||||||
| Low | 24.8 | Reference | Reference | 21.5 | Reference | Reference |
| Medium | 43.4 | 1.92 (1.49–2.46)d | 1.55 (1.19–2.02)f | 31.6 | 1.55 (1.26–1.90)d | 1.18 (0.95–1.46) |
| High | 52.7 | 2.45 (1.91–3.14)d | 1.75 (1.32–2.34)d | 37.5 | 1.90 (1.55–2.33)d | 1.28 (1.01–1.62)e |
| Very high | 52.6 | 2.37 (1.85–3.04)d | 1.71 (1.25–2.35)f | 34.0 | 1.60 (1.30–1.97)d | 1.23 (0.95–1.59) |
| Men only | ||||||
| Low | 24.8 | Reference | Reference | 30.8 | Reference | Reference |
| Medium | 32.7 | 1.39 (1.05–1.85)e | 1.01 (0.71–1.45) | 38.2 | 1.35 (1.06–1.72)e | 1.07 (0.79–1.44) |
| High | 39.5 | 1.76 (1.31–2.36)d | 1.19 (0.80–1.77) | 42.5 | 1.59 (1.25–2.02)d | 1.13 (0.81–1.58) |
| Very high | 40.4 | 1.85 (1.36–2.50)d | 1.27 (0.82–1.95) | 45.0 | 1.75 (1.36–2.27)d | 1.32 (0.91–1.90) |
AOR indicates adjusted OR; BMI, body mass index; BP, blood pressure; CI, confidence interval; DBP, diastolic BP; OR, odds ratio; and SBP, systolic BP.
Derived from height and weight measurements recorded in the electronic health record; standard definitions obtained from the Centers for Disease Control and Prevention.
Derived from systolic and diastolic BP measurements recorded in the electronic health record; standard definitions obtained from the Seventh Report of the Joint National Committee.
Estimates obtained from generalized linear mixed models. Adjusted for patient demographics, including age (continuous), sex, race, and insurance status; clinic site; and census tract characteristics, including median household income (continuous), ≥25% less than high school graduation, ≥25% unemployment, ≥75% minority racial/ethnic composition, and ≥10% poor English fluency.
P<0.001.
P<0.05.
P<0.01.
Homicides were rare events, ranging from 0 to 6 homicides per census tract. There were 13 “double homicides” (single events with 2 homicides), but there were no events with ≥3 homicides recorded during the study period. We were unable to determine if homicides occurring on the same date in different locations were related events. Similarly, there were homicides occurring in identical locations over a short period of time (eg, 5–10 days); we were unable to determine if these were related events (eg, retaliation). Most census tracts (52%) had no homicides during the study period; few census tracts (8%) had ≥3 homicides. Approximately a quarter of patients (25.7%) lived one‐quarter mile or less from the nearest homicide. Compared with patients living in a census tract with no homicides, patients living in a census tract with at least 1 homicide had 16% higher adjusted odds of elevated BP (95% CI, 1.06–1.27; Table 3); in analyses examining obesity status, findings were not statistically significant in adjusted models (adjusted odds ratio=1.07; 95% CI, 0.95–1.21). Proximity to nearest homicide was not significantly associated with obesity or BP status in adjusted models (Table 3).
Discussion
We found that exposure to a higher police‐recorded violent crime rate was consistently associated with measured obesity and elevated BP in this sample of urban‐dwelling adults. This study, using objective measures of both violence and health (BMI and BP), corroborates prior work suggesting a relationship between neighborhood safety and health.35, 36, 37 Higher exposure to nonviolent theft or property crime was also associated with obesity, but these effects were somewhat attenuated compared with analyses examining exposure to violent crime. In the most similar study published to date, Miranda and colleagues examined 1785 school‐aged children and found a stronger relationship between violent crime rates and measured BMI, compared with property crime rates.38 However, similar studies using objective measures in adult populations have typically examined homicide rates only, resulting in null findings.11, 39, 40 Our study distinguishes between 3 types of crime (violent crime, nonviolent property crime, and homicide), revealing notable differences in their associations with obesity and elevated BP. Findings in our study were also more pronounced among women, supporting prior evidence that women who feel unsafe may be less likely to engage in physical activity relative to men.7 This finding, along with the high prevalence of female‐headed households in neighborhoods with the most crime,41 aligns with growing concern about disparities in cardiovascular outcomes among women residing in disadvantaged communities.22
Consistent with prior literature,11, 39, 40 we additionally found that exposure to homicide alone was not associated with obesity status and was inconsistently associated with BP status. The presence of at least 1 homicide in a community was associated with elevated BP; however, the relative effect was smaller compared with analyses examining overall violent crime rates. Moreover, proximity to nearest homicide was not associated with obesity or BP status in adjusted models. Our findings possibly suggest that recurrent exposure to violent crime may be more strongly associated with physical health than a single exposure to severe violent crime (ie, homicide). Interestingly, prior research has identified that most adults confronted with a serious life event (eg, death of a loved one) do not experience long‐term deleterious health effects.42, 43, 44 However, other research has revealed that exposure to an extreme event of violence (eg, a terrorist attack) can trigger poor physical health.45, 46 Our study offers preliminary evidence to support the hypothesis that secondary exposure to recurrent violence may confer unique health risks compared with isolated events of lethal violence. However, it is also possible that homicide has rippling effects that are more diffuse, both spatially and socially, which may not be captured in studies of neighborhood effects. For instance, robbery concerns may be neighborhood specific, whereas homicide may affect more diffuse social networks and settings.
Nevertheless, related research may point to some possible explanations for the observed differences between these types of violent crime. Studies of racial discrimination find that “everyday discrimination” is more strongly associated with physical health than rare events of severe discrimination, even for the most toxic experiences.47, 48 Prior studies have attributed these differences to the biological impacts of chronic stressors, or allostatic load, on autonomic regulation, immune and endocrine system function, and inflammatory processes.15, 44 Despite overwhelming public attention on homicides, it is possible that incremental and cumulative stress because of “everyday” crime (eg, robbery) plays a larger role in physical health. Another possibility is that persistent occurrences of nonlethal violence trigger behavioral responses that affect daily activities, such as reduced physical activity, whereas isolated events of homicide do not. Indeed, homicides may be perceived as being personal and targeted events, because only a minority of homicides are committed by strangers,49 whereas robberies may be perceived as more impersonal and “random” events that can occur to anyone who appears vulnerable (eg, frail, obese, and disabled people). It is also possible that a single homicide may have few practical impacts on neighborhood businesses, whereas persistent robbery concerns may prompt businesses to avoid locating to high‐crime neighborhoods.
Overall, our study of a predominantly black primary care population points to a relationship between exposure to violent crime and chronic disease status, with possible implications for clinical population health management. Although prior literature has described the importance of addressing community violence as a public health issue, healthcare systems may have financial incentive to address community violence as a population health issue. Indeed, policies that favor per‐capita and performance‐based payments may inadvertently tie reimbursement to population‐level social conditions that determine health. Thus, healthcare organizations located in regions of particular social vulnerability, similar to the region examined in this study, must think critically about broader approaches to optimize health. For instance, healthcare organizations located in high‐crime regions may opt to invest in violence prevention and intervention strategies.50 We speculate that these strategies may have potential health benefits for not only those directly affected by violence (eg, trauma victims), but also for those with downstream health consequences (eg, obesity, hypertension, and mental health). As such, recognizing and addressing the impacts of violence may be an important consideration for managing the health risks of low‐income urban communities of color.
This study has several limitations. First, this is a cross‐sectional study, which limits causal inference. Second, this study uses data from 3 primary care clinics at an academic medical center, limiting generalizability. For instance, half of the patients in our sample were insured by Medicaid and/or Medicare; our findings should be interpreted in light of these characteristics. For related reasons, we did not use diagnostic codes or prescription medications recorded in the electronic health record for classification purposes. Estimates for the completeness of diagnostic codes have been highly variable in prior studies,51 and although prescription medications may have been used to delineate treated and untreated individuals, medication underuse has been reported to be high this population.52 We were concerned that these additional electronic health record data may have conferred imprecise subclassifications. By classifying BP on the basis of clinical measurement data alone, individuals without hypertension and individuals with controlled hypertension were analyzed as a single group. However, prior literature has documented that medication adherence is itself a function of safety.53 Thus, classifications are consistent with hypotheses about both the physiological and behavioral health benefits of living in a low‐crime neighborhood.
In addition, 16.5% of patients had missing BMI information; fewer (3.2%) had missing BP information. It is possible that those with missing BMI information declined or were unable to use the weight scale (eg, because of disability, wheelchair confinement, or related issues). In sensitivity analyses, however, patients with missing BMI information did not differ appreciably from those without missing BMI information (Table S3); also, sensitivity testing using multiple imputation methods did not alter the study findings (Table S4). Although we did not have data on individual socioeconomic characteristics, we partially mitigated this concern by analyzing a sample of individuals with access to health care, adjusting for person‐level insurance type, and using multilevel models to adjust for neighborhood‐level socioeconomic status indicators, similar to prior studies.37 However, point estimates may be overestimated. In addition, the CommunityRx study protocol abstracted health records during the study period only, and did not abstract health records before this period. Thus, longitudinal associations were not explored, and future studies should consider temporal trends.
We assigned exposure to crime using geographic methods, thus subjecting our findings to ecological fallacy: patients’ level of exposure to violence, even within the same census tract, may vary depending on individual factors. Although census tract remains the enduring choice for neighborhood effects research because of relatively homogeneous population characteristics, economic status, and living conditions,54 it is possible that patients were also affected by surrounding or more distant contexts, such as work environments or activity spaces. Furthermore, the objective secondary data used in this analysis do not enable assessments of individual trauma from violent events; therefore, we are limited in our ability to interpret findings within the broader literature on the psychological and behavioral effects of trauma. Finally, it is possible that the completeness of police crime records may vary geographically and by the severity of the crime, because of recording practices, reporting practices, or both. However, there is no compelling evidence for systematic discrepancies between census tracts. Similarly, violent crimes, such as homicide and assault, are likely to be known and recorded by police and, therefore, are likely to reflect accurate estimates of exposure.
Conclusion
In a densely populated, high‐poverty region in Chicago, exposure to a higher rate of violent crime was consistently associated with obesity and elevated BP among adult primary care patients. Moreover, a high rate of recurrent exposure to all types of violent crime was more strongly associated with health than a rare exposure to severe violent crime (homicide). Interventions to mitigate the harmful health effects of everyday violent crime, particularly in high‐crime communities, may be a critical consideration for sustainably improving the cardiovascular health of vulnerable populations.
Author Contributions
Study concept and design: Tung, Makelarski, Peek, and Lindau. Acquisition of data: Tung, Makelarski, and Lindau. Analysis and interpretation of data: Tung, Wroblewski, and Boyd. Drafting of the article: Tung, Makelarski, Peek, and Lindau. Critical revision of the article for important intellectual content: All authors. Statistical Analysis: Tung, Wroblewski, and Boyd. Administrative, technical, or material support: Peek and Lindau. Final approval of the version to be published: All authors. Tung had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Sources of Funding
This project was supported in part by the National Institutes of Health (NIH)/National Institute on Aging 1R01AG047869 (Lindau, principal investigator) to the University of Chicago. Tung was supported by the Agency for Healthcare Research and Quality K12 grant in patient‐centered outcomes research 5K12HS023007 and the Chicago Center for Diabetes Translation Research NIDDK P30DK092949. The content of this article is solely the responsibility of the authors and does not necessarily represent the views of any NIH institutes.
Disclosures
None.
Supporting information
Table S1. Sensitivity Analysis of Continuous Outcomes: Census Tract Violent Crime and Body Mass Index or Systolic Blood Pressure
Table S2. Subgroup Analysis by Age Group: Census Tract Violent Crime and Body Mass Index or Blood Pressure Status
Table S3. Patient Characteristics by Missing or Non‐Missing BMI Information
Table S4. Sensitivity Analysis: Imputed for Missing Body Mass Index
(J Am Heart Assoc. 2018;7:e008030 DOI: 10.1161/JAHA.117.008030.)
This article was presented in part at the Society of General Internal Medicine Annual Meeting, April 19 to 22, 2017, in Washington, DC.
References
- 1. Friedman M, Grawert A, Cullen J. Crime in 2016. New York, NY: Brennan Center for Justice; 2016:7. [Google Scholar]
- 2. Sampson RJ. Great American City: Chicago and the Enduring Neighborhood Effect. Chicago, IL: University of Chicago Press; 2012. [Google Scholar]
- 3. Fowler‐Brown AG, Bennett GG, Goodman MS, Wee CC, Corbie‐Smith GM, James SA. Psychosocial stress and 13‐year BMI change among blacks: the Pitt County Study. Obesity (Silver Spring). 2009;17:2106–2109. [DOI] [PubMed] [Google Scholar]
- 4. Sumner SA, Mercy JA, Dahlberg LL, Hillis SD, Klevens J, Houry D. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314:478–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burdette AM, Hill TD. An examination of processes linking perceived neighborhood disorder and obesity. Soc Sci Med. 2008;67:38–46. [DOI] [PubMed] [Google Scholar]
- 6. Astell‐Burt T, Feng X, Kolt GS, Jalaludin B. Does rising crime lead to increasing distress? Longitudinal analysis of a natural experiment with dynamic objective neighbourhood measures. Soc Sci Med. 2015;138:68–73. [DOI] [PubMed] [Google Scholar]
- 7. Foster S, Giles‐Corti B. The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Prev Med. 2008;47:241–251. [DOI] [PubMed] [Google Scholar]
- 8. Sandy R, Tchernis R, Wilson J, Liu G, Zhou X. Effects of the built environment on childhood obesity: the case of urban recreational trails and crime. Econ Hum Biol. 2013;11:18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shinew KJ, Stodolska M, Roman CG, Yahner J. Crime, physical activity and outdoor recreation among Latino adolescents in Chicago. Prev Med. 2013;57:541–544. [DOI] [PubMed] [Google Scholar]
- 10. Yu E, Lippert AM. Neighborhood crime rate, weight‐related behaviors, and obesity: a systematic review of the literature. Sociol Compass. 2016;10:187–207. [Google Scholar]
- 11. Lovasi GS, Bader MD, Quinn J, Neckerman K, Weiss C, Rundle A. Body mass index, safety hazards, and neighborhood attractiveness. Am J Prev Med. 2012;43:378–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood‐based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93:1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sanchez BN, Moore K, Adar SD, Horwich TB, Watson KE, Diez Roux AV. Longitudinal associations between neighborhood physical and social environments and incident type 2 diabetes mellitus: the Multi‐Ethnic Study of Atherosclerosis (MESA). JAMA Intern Med. 2015;175:1311–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. [DOI] [PubMed] [Google Scholar]
- 15. McEwen B, Lasley EN. Allostatic load: when protection gives way to damage. Adv Mind Body Med. 2003;19:28–33. [PubMed] [Google Scholar]
- 16. Leininger S, Skeel R. Cortisol and self‐report measures of anxiety as predictors of neuropsychological performance. Arch Clin Neuropsychol. 2012;27:318–328. [DOI] [PubMed] [Google Scholar]
- 17. Gidlow CJ, Randall J, Gillman J, Silk S, Jones MV. Hair cortisol and self‐reported stress in healthy, working adults. Psychoneuroendocrinology. 2016;63:163–169. [DOI] [PubMed] [Google Scholar]
- 18. Mackenbach JP, Looman CW, van der Meer JB. Differences in the misreporting of chronic conditions, by level of education: the effect on inequalities in prevalence rates. Am J Public Health. 1996;86:706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stewart AW, Jackson RT, Ford MA, Beaglehole R. Underestimation of relative weight by use of self‐reported height and weight. Am J Epidemiol. 1987;125:122–126. [DOI] [PubMed] [Google Scholar]
- 20. Lorenc T, Clayton S, Neary D, Whitehead M, Petticrew M, Thomson H, Cummins S, Sowden A, Renton A. Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health Place. 2012;18:757–765. [DOI] [PubMed] [Google Scholar]
- 21. Weinstein A, Feigley P, Pullen P, Mann L, Redman L. Neighborhood safety and the prevalence of physical inactivity: selected states, 1996. MMWR Morb Mortal Wkly Rep. 1999;48:143–146. [PubMed] [Google Scholar]
- 22. Wenger NK, Speroff L, Packard B. Cardiovascular health and disease in women. N Engl J Med. 1993;329:247–256. [DOI] [PubMed] [Google Scholar]
- 23. Kaiser P, Diez Roux AV, Mujahid M, Carnethon M, Bertoni A, Adar SD, Shea S, McClelland R, Lisabeth L. Neighborhood environments and incident hypertension in the Multi‐Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016;183:988–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. US Census Bureau . American Community Survey 5‐Year Estimates. 2014. http://factfinder.census.gov. Accessed July 4, 2016.
- 25. Lindau ST, Makelarski J, Abramsohn E, Beiser DG, Escamilla V, Jerome J, Johnson D, Kho AN, Lee KK, Long T, Miller DC. CommunityRx: a population health improvement innovation that connects clinics to communities. Health Aff (Millwood). 2016;35:2020–2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chicago Police Department . Crime type categories: definition & description. 2017. http://gis.chicagopolice.org/clearmap_crime_sums/crime_types.html. Accessed April 6, 2017.
- 27. Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62:2061–2071. [DOI] [PubMed] [Google Scholar]
- 28. Zagozdzon P, Parszuto J, Wrotkowska M, Dydjow‐Bendek D. Effect of unemployment on cardiovascular risk factors and mental health. Occup Med (Lond). 2014;64:436–441. [DOI] [PubMed] [Google Scholar]
- 29. Reina AS, Lohman BJ, Maldonado MM. “He said they'd deport me”: factors influencing domestic violence help‐seeking practices among Latina immigrants. J Interpers Violence. 2014;29:593–615. [DOI] [PubMed] [Google Scholar]
- 30. Martinez‐Donate AP, Ejebe I, Zhang X, Guendelman S, Le‐Scherban F, Rangel G, Gonzalez‐Fagoaga E, Hovell MF, Amuedo‐Dorantes C. Access to health care among Mexican migrants and immigrants: a comparison across migration phases. J Health Care Poor Underserved. 2017;28:1314–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nandi A, Galea S, Lopez G, Nandi V, Strongarone S, Ompad DC. Access to and use of health services among undocumented Mexican immigrants in a US urban area. Am J Public Health. 2008;98:2011–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Barcellos SH, Goldman DP, Smith JP. Undiagnosed disease, especially diabetes, casts doubt on some of reported health “advantage” of recent Mexican immigrants. Health Aff (Millwood). 2012;31:2727–2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kutner MH, Nachtsheim CJ, Neter J. Multicollinearity diagnostics: variance inflation factor Applied Linear Regression Models. 4th ed Chicago, IL: McGraw‐Hill Irwin; 2004:406–410. [Google Scholar]
- 34. Truman JL, Morgan RE. Criminal victimization, 2015. 2016. https://www.bjs.gov/content/pub/pdf/cv15.pdf. Accessed August 1, 2017.
- 35. Piro FN, Noss O, Claussen B. Physical activity among elderly people in a city population: the influence of neighbourhood level violence and self perceived safety. J Epidemiol Community Health. 2006;60:626–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med. 2007;65:2440–2457. [DOI] [PubMed] [Google Scholar]
- 37. Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS. Areas with high rates of police‐reported violent crime have higher rates of childhood asthma morbidity. J Pediatr. 2016;173:175–182.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Miranda ML, Edwards SE, Anthopolos R, Dolinsky DH, Kemper AR. The built environment and childhood obesity in Durham, North Carolina. Clin Pediatr. 2012;51:750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mendes LL, Nogueira H, Padez C, Ferrao M, Velasquez‐Melendez G. Individual and environmental factors associated for overweight in urban population of Brazil. BMC Public Health. 2013;13:988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Velasquez‐Melendez G, Mendes LL, Padez CM. Built environment and social environment: associations with overweight and obesity in a sample of Brazilian adults. Cad Saude Publica. 2013;29:1988–1996. [DOI] [PubMed] [Google Scholar]
- 41. Vespa J, Lewis JM, Kreider RM. America's families and living arrangements. Popul Charact. 2013. https://www.census.gov/prod/2013pubs/p20-570.pdf. Accessed September 9, 2017. [Google Scholar]
- 42. Baum A, Cohen L, Hall M. Control and intrusive memories as possible determinants of chronic stress. Psychosom Med. 1993;55:274–286. [DOI] [PubMed] [Google Scholar]
- 43. Cohen S, Kessler RC, Gordon LU. Strategies for Measuring Stress in Studies of Psychiatric and Physical Disorders. New York, NY: Oxford University Press; 1995. [Google Scholar]
- 44. Cohen S, Janicki‐Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. [DOI] [PubMed] [Google Scholar]
- 45. Lauderdale DS. Birth outcomes for Arabic‐named women in California before and after September 11. Demography. 2006;43:185–201. [DOI] [PubMed] [Google Scholar]
- 46. Bhattacharyya MR, Steptoe A. Emotional triggers of acute coronary syndromes: strength of evidence, biological processes, and clinical implications. Prog Cardiovasc Dis. 2007;49:353–365. [DOI] [PubMed] [Google Scholar]
- 47. Taylor TR, Williams CD, Makambi KH, Mouton C, Harrell JP, Cozier Y, Palmer JR, Rosenberg L, Adams‐Campbell LL. Racial discrimination and breast cancer incidence in US black women: the Black Women's Health Study. Am J Epidemiol. 2007;166:46–54. [DOI] [PubMed] [Google Scholar]
- 48. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harrell E. Violent victimization committed by strangers, 1993–2010. Washington, D.C.: U.S. Department of Justice, Bureau of Justice Statistics; 2012:18. [Google Scholar]
- 50. Purtle J, Dicker R, Cooper C, Corbin T, Greene MB, Marks A, Creaser D, Topp D, Moreland D. Hospital‐based violence intervention programs save lives and money. J Trauma Acute Care Surg. 2013;75:331–333. [DOI] [PubMed] [Google Scholar]
- 51. Chan KS, Fowles JB, Weiner JP. Review: electronic health records and the reliability and validity of quality measures: a review of the literature. Med Care Res Rev. 2010;67:503–527. [DOI] [PubMed] [Google Scholar]
- 52. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost‐related medication underuse, and unmet needs. Am J Med. 2014;127:303–310.e3. [DOI] [PubMed] [Google Scholar]
- 53. Billimek J, Sorkin DH. Self‐reported neighborhood safety and nonadherence to treatment regimens among patients with type 2 diabetes. J Gen Intern Med. 2012;27:292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. US Census Bureau . Census Bureau geography: census tracts and block numbering areas. 2013. https://www2.census.gov/geo/pdfs/reference/GARM/Ch10GARM.pdf. Accessed September 9, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Sensitivity Analysis of Continuous Outcomes: Census Tract Violent Crime and Body Mass Index or Systolic Blood Pressure
Table S2. Subgroup Analysis by Age Group: Census Tract Violent Crime and Body Mass Index or Blood Pressure Status
Table S3. Patient Characteristics by Missing or Non‐Missing BMI Information
Table S4. Sensitivity Analysis: Imputed for Missing Body Mass Index


