Abstract
Mowat-Wilson syndrome is a genetic disease caused by heterozygous mutations or deletions of the ZEB2 gene and characterized by typical clinical features. The congenital malformations typical of this syndrome call for early diagnostic and surgical procedures requiring general anesthesia, but few information about the anesthesiology management of such patients is available. We enrolled 11 families of patients with Mowat-Wilson syndrome who had undergone surgical or diagnostic procedures requiring general anesthesia, and sent them a retrospective questionnaire including 16 open questions about the procedures. They were further contacted by phone for a semistructured interview. A total of 37 procedures requiring general anesthesia was reported in 11 patients. Only two patients reported anesthesia-related complications during the procedure. No true additional anesthesiarelated risk was present for the patients with MW syndrome, besides difficult intubation, weaning and lower respiratory tract infection. Perception of risk, however, is derived by non-medical observation on the part of the parents.
Key words: Mowat Wilson syndrome, general anesthesia, anesthesia-related risk
Introduction
Mowat-Wilson syndrome (MWS; OMIM#235730) is a genetic disease caused by heterozygous mutations or deletions of the ZEB2 gene,1,2 and characterized by typical face, epilepsy, moderate-to-severe mental retardation, and variable congenital malformations, including Hirschsprung disease (HSCR), agenesis of the corpus callosum (ACC), congenital heart disease (CHD), genital anomalies (particularly hypospadias in males), and eye defects. Since the first delineation by Mowat et al. (1998), more then 200 patients with ZEB2 mutations, deletions or cytogenetic abnormalities have been reported primarily from Northern Europe, Australia, Italy and the United States, and over 100 mutations have been described.3-17
Congenital malformations typical of this syndrome call for early diagnostic investigations and surgical resolutions; general anesthesia is required for diagnostic and surgical procedures, both in election and in emergency, but few information about anesthesiologic management is available.9
The aim of our study was to collect retrospective data on general anesthesia interviewing a large numbered group of Italian patients with MWS, assess the anesthesiologic outcomes and identify the conditions that required general anesthesia; aware of the fact that few clinical data would be derived from this interview
Materials and Methods
A retrospective cohort study design was performed with questionnaire was sent to the parents using the mailing list of the Italian association of the Mowat-Wilson Syndrome. Thirty six questionnaires were sent out in total and each questionnaire included 16 open questions about age, type of surgery/diagnostic test requiring general anesthesia and outcome of the procedure. Some questions relating to the perception of the families about the knowledge of the disease by the anesthesiologist were also included. All of the families who initially replied to the questionnaire by mail were then contacted by phone for an additional semistructured interview.
Furthermore a further call was necessary to obtain clinical data such as the hospital stay from the clinical documentation in the possession of the families.
Results
We have collected questionnaires from 11 patients with MWS on thirty six.
A total of 37 anesthesiologic procedures was reported in 11 patients; in all cases, anesthesia was required in relation to various type of surgery and diagnostic procedures (Table 1).
Table 1.
Age of surgery and diagnostic procedures in 11 Italian patients with MWs.
| Patient | Age | Type of diagnostic/surgical procedure | Elective/urgent procedure | Patient’s trust in the anesthesiologist | Complications | Hospital stay |
|---|---|---|---|---|---|---|
| PT1 | 3 yr | megacolon resection | elective | excellent | no | 9 d |
| PT2 | 18 mo | brain MRI | elective | good | no | 2 d |
| 3 yr | brain MRI | elective | good | no | 2 d | |
| PT3 | 52 d | megacolon resection | urgent | very good | no | 11 d |
| 8 yr | undescended testicle | elective | good | no | 3 d | |
| PT4 | 21 d | diagnostic bronchoscopy | elective | satisfactory | no | 2 d |
| 27 d | cardiac catheterization | elective | satisfactory | no | 5 d | |
| 29 d | vascular ring correction + PDA closure | urgent | satisfactory | no | 7 d | |
| 80 d | transanal endorectal pull-through | elective | N/A | no | 11 d | |
| PT5 | 3 mo | cardiac catheterization + PDA closure | elective | very good | no | 6 d |
| 3 yr | adenotonsillectomy | elective | good | no | 3 d | |
| PT6 | 16 mo | cardiac catheterization | elective | very good | cardiac | 5 d |
| 19 mo | brain MRI | elective | very good | no | 2 d | |
| PT7 | 1 mo | colostomy confection | elective | satisfactory | no | 3 d |
| 6 mo | bowel resection | elective | satisfactory | no | 6 d | |
| 9 mo | colostomy reversal | elective | satisfactory | no | 7 d | |
| 30 mo | MRI | elective | satisfactory | no | 2 d | |
| 4 yr | hypospadias | elective | satisfactory | no | 4 d | |
| 5 yr | MRI | elective | satisfactory | no | 2 d | |
| 16 yr | undescended testicle removal | elective | satisfactory | no | 5 d | |
| PT8 | 1 mo | pulmonic valve stenosis surgery | elective | very poor | respiratory | 5 d |
| 3 mo | pyloric stenosis | urgent | very poor | no | 3 d | |
| 1 yr | IVD closure | elective | very poor | respiratory | 4 d | |
| 7 yr | vertebral column arthrodesis | elective | very good | no | 7 d | |
| PT9 | 1 mo | megacolon | urgent | good | no | 7 d |
| 6 mo | bowel resection | elective | good | no | 4 d | |
| 9 mo | colostomy reversal | elective | good | no | 7 d | |
| 4 yr | hypospadias | elective | good | no | 3 d | |
| 16 yr | undescended testicle removal | elective | good | no | 4 d | |
| 21 yr | brain MRI + urethrotomy | elective | good | no | 3 d | |
| PT10 | 6 mo | MRI | elective | satisfactory | no | 2 d |
| 3 yr | MRI | elective | satisfactory | no | 1 d | |
| 3 yr | facial and hand warts excision | elective | good | no | 2 d | |
| PT11 | 11 mo | tear duct opening + orchidopexy | elective | satisfactory | no | 5 d |
| 1 yr | MRI | elective | satisfactory | no | 2 d | |
| 18 mo | muscle biopsy | elective | satisfactory | no | 1 d | |
| 4 yr | testicle removal | elective | satisfactory | no | 5 d |
The age of surgery and diagnostic procedures is reported in Figure 1.
Figure 1.
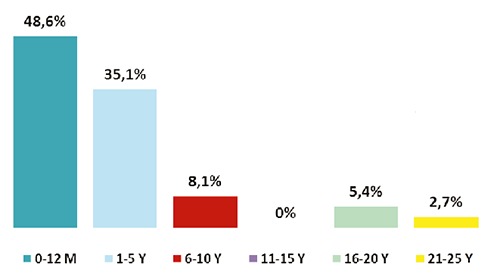
The age of patients as a percentage. At the time of general anesthesia, the age of patients ranged from month to 21 years.
The more common operations were the following: gastrointestinal surgeries (27%); diagnostic investigation, mainly MRI (24,3%); cardiac surgeries (16,2%); orchiopexy/orchiectomy of a cryptorchid testicle (13,5%); hypospadias correction (5,4%) (Figure 2). Unfortunately it was not possible to derive from the interviews the duration of the single surgical and instrumental procedures.
Figure 2.
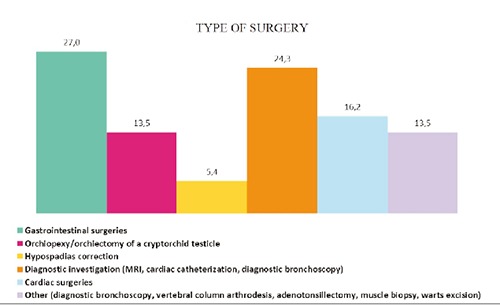
Type of surgery and diagnostic procedures in 11 Italian patients with MWs.
75.7% of families reported that the anesthesiologists were not aware of the syndrome; nevertheless, 43.2% of parents declared that they have been sufficiently reassured by the competence of the physician to trust him/her, even if we do not have data that attest to the clinical experience of anesthetists with pediatric patients.
In 78.4% of cases no complications of anesthesia emerged during the procedures (data collected from patients’ perception of patients and not from clinical data). Two patients reported anesthesia-related problems: a patient had cardiac complication during one procedure and another patient had respiratory complications during two different procedures.
Anesthesia was required for 33 elective procedures and for 4 urgent procedures. No one of the parents received a report after the procedure.
Discussion
The involvement of patients’ organizations in collecting clinical data has been a strong instrument for natural history of rare diseases. The anesthetic risk is present at each procedure but particular syndromes may provide an additional risk.18 However, very little is known about the anesthetic risk of MWS. The survey through social media has advantages and disadvantages, as well summarized in a recent article by William Davies:19 fast turnaround, low costs, a large number of patients recruited (often seen individually in different hospitals) but the evaluation of the point of view of the individuals or the caregivers, the compilation of retrospective questionnaire was on a voluntary basis and this may introduce an additional bias.
However, a similar investigation made for the MWS was done in the same manner for the Cri du Chat syndrome.20
Analysis of the type of surgery allows to note that most of these are made in election, except for those made in urgency (i.e. digestive canal at birth), when the diagnosis of MW has not yet been made.
No true additional anesthesia-related risk was present for the patients with MW syndrome, both parents and professionals can take comfort in knowing the real anesthesiologic risk linked to issues involving the Mowat-Wilson syndrome. It is recommended to carry out an examination of patient’s cardiac function before any procedure; in case of cardiac malformation, antibiotic prophylaxis for bacterial endocarditis is required. Furthermore, in according to Deshmukt et al.,21 the main anesthetic challenges in MW syndrome are a risk of difficult intubation and possibility of difficulty in weaning, lower respiratory tract infection and anemia.
The recollections of the patient’s parents may be biased, even if it was their choice whether or not to participate in the study, hence we can assume that their responses correspond to reality, but not as a real clinical evaluation.
Conclusions
The study presents possible limits, such as potential bias due to the set nature of the design: a retrospective survey based on the memory of the patients’ parents. Moreover, the lack of some clinical data such as the duration of surgical and instrumental procedures, ASA score, the experience of the anesthetists inherent in pediatric patients, the anesthetic technique used, do not make the present study definitive. However our perception of risk, however, is derived by non-medical observation on the part of the parents, therefore further investigations − including the analysis of the medical files of all subject − are needed to confirm our findings; a prospective study would be desirable.
Acknowledgements
The authors would like to thank Italian Association of the Mowat-Wilson- Syndrome.
Funding Statement
Funding: none.
References
- 1.Adam MP, Bean LJH, Ranger Miller V. Mowat-Wilson sindrome. Genereviews www.genetests.org [Google Scholar]
- 2.Bissonnette B, Luginbruehl I, Marciniak B, et al. Syndromes: rapid recognition and perioperative implications. McGraw-Hill, 2006. [Google Scholar]
- 3.Cacheux V, Dastot-Le Moal F, Kääriäinen H, et al. Loss-of-function mutations in SIP1 Smad interacting protein 1 results in a syndromic Hirschsprung disease. Hum Mol Genet 2001;10:1503-10. [DOI] [PubMed] [Google Scholar]
- 4.Cerutti Mainardi P, Pastore G, Zweier C, et al. Mowat-Wilson sindrome and mutation in the zinc finger homeo box 1B gene: a well defined clinical entity J Med Genet 2004;41:e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dastot-Le Moal F, Wilson M, Mowat D, et al. ZFHX1B mutations in patients with Mowat-Wilson syndrome. Hum Mutat 2007:1-9. [DOI] [PubMed] [Google Scholar]
- 6.Garavelli L, Donadio A, Zanacca C, et al. Hirschsprung disease, mental retardation, characteristic facial features and mutation in the gene ZFHX1B (SIP1): confirmation of the Mowat- Wilson syndrome. Am J Med Genet 2003;116A 385-8. [DOI] [PubMed] [Google Scholar]
- 7.Garavelli L, Mainardi PC. Mowat- Wilson syndrome. Orphanet J Rare Dis 2007;2:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garavelli L, Zollino M, Mainardi PC, et al. Mowat-Wilson Syndrome: phenotype changing with age. Study of 19 Italian patients and review of the literature. Am J Med Genet Am 2009;149A:417-26. [DOI] [PubMed] [Google Scholar]
- 9.Kiernan F, Crowe S. Safe use of the classic laryngeal mask airway and endotracheal intubation in general anaesthesia for a patient with Mowat- Wilson syndrome. Paediatr Anaesth 2009;19:174-5. [DOI] [PubMed] [Google Scholar]
- 10.Mowat DR, Croaker GDH, Cass DT, et al. Hirschsprung disease, microcephaly, mental retardation, and characteristic facial features: delineation of a new syndrome and identification of a locus at chromosome 2q22-q23. J Med Genet 1998;35:617-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mowat DR, Wilson MJ, Goossens M. Mowat-Wilson syndrome J Med Genet 2003;40:305-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Electronic Database Information: Online Mendelian Inheritance in Man (OMIM), http://www.ncbi.nlm.nih.gov/Omim/ [Google Scholar]
- 13.Wakamatsu N, Yasukazu Y, Kenichiro Y, et al. Mutations in SIP1, encoding Smad interacting protein-1, cause a form of Hirschsprung disease. Nat Genet 2001;27:369-70. [DOI] [PubMed] [Google Scholar]
- 14.Wilson M, Mowat D, Dastot-LeMood F. Further delineation of the phenotype associated with heterozygous mutation in ZFHX1B. Am J Med Genet 2003;119A:257-65. [DOI] [PubMed] [Google Scholar]
- 15.Zweier C, Albrecht B, Mitulla B, et al. Mowat-Wilson Syndrome with and without Hirschsprung Disease is a distinct, recognizable Multiple Congenital Anomalies-Mental Retardation Syndrome caused by Mutations in the Zinc finger homeobox 1 B gene (ZFHX1B). Am J Med Genet 2002;108:177-81. [PubMed] [Google Scholar]
- 16.Zweier C, Temple IK, Beemer F, et al. Characterisation of deletions of the ZFHX1B region and genotypephenotype analysis in Mowat-Wilson syndrome. J Med Genet 2003;40:601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zweier C, Thiel CT, Dufke A, et al. Clinical and Mutational Spectrum of Mowat-Wilson Sindrome. Eur J Med Genet. 2005, 48: 97-111. [DOI] [PubMed] [Google Scholar]
- 18.Biro P, Vagts D, Emmig U, et al. Anasthesie bei seltenen Erkrankungen. Berlin: Springer-Verlag; 2011. [Google Scholar]
- 19.Davies W. Insights into rare diseases from social media surveys. Orphan J Rare Dis. 2016,11:151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guala A, Spunton M, Mainardi PC, et al. Anesthesia in Cri du Chat syndrome: information on 51 Italian patients. Am J Med Genet. 2015,167A:1168-70. [DOI] [PubMed] [Google Scholar]
- 21.Deshmukt AS, Kelkar KV, Khedkar SM, et al. Anaesthetic management of Mowat-Wilson syndrome. Ind J Anaesthesia. 2016,40:292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


