Abstract
The cell cycle is a highly regulated and fundamental cellular process that involves complex feedback regulation of many proteins, and any compromise to its integrity elicits dire consequences for the cell. For example, in neurodegenerative diseases such as Alzheimer disease (AD), evidence for abnormal cell cycle re-entry precedes other hallmarks of disease and as such, implicates cell cycle aberrations in the aetiology of AD. The mechanism(s) for cell cycle re-entry in AD, however, remain unclear. Current theory suggests it to be part of a combination of early events that together elicit the degenerative pathology and cognitive phenotype consistent with the disease. We propose a ‘Two-Hit Hypothesis’ that highlights the concerted interaction between cell cycle alterations and oxidative stress that combine to produce neurodegeneration. Here, we review the evidence implicating cell cycle mechanisms in AD and how such changes, especially in combination with oxidative stress, would lead to a cascade of events leading to disease. Based on this concept, we propose new opportunities for disease treatment.
Keywords: Alzheimer disease, cell cycle re-entry, mitotic insult, mitotic steady state, oxidative stress
Introduction
The cell cycle consists of elaborate feedback mechanisms and regulatory checkpoints that are typically divided into four phases: S-phase, during which DNA replication occurs, M-phase, where cell division, or mitosis, takes place, and the gap phases that separate the two; G1 and G2, respectively. Additionally, quiescent cells, such as many of the neurones in the adult hippocampus, exist in a non-dividing, silent phase known as G0. Once in this phase, cells are deemed terminally differentiated, meaning they are not capable of re-entering the cell cycle [1]. It is in this capacity that vulnerable neurones are affected. As increasing evidence indicates, cells that exist in G0, and thus are no longer mitotically active, become wrongly reactivated in Alzheimer disease (AD) and other neurodegenerative diseases, and are forced through a cell cycle that they are no longer capable of completing [2–5]. That is, re-entrant cells that proceed past late G1, some even entering and completing S-phase, cannot return to G0. Moreover, for reasons not completely understood, these already differentiated cells cannot undergo mitosis, and, because of limited options, induced their own deaths via apoptotic pathways [6,7]. As this phenotype precedes much of the other associated markers of neurodegeneration in AD [8], it is of increasing relevance to the field and merits further investigation.
Cell cycle protein regulation
Vital to the cycle, and thus to the proliferation of the cell, are the set of proteins generally associated with guiding the cell from one phase to the next. These proteins, the cyclins and the associated cyclin-dependant kinases (cdks), fluctuate in their expression and activity as the cell transitions from S-phase to M-phase [9,10]. In particular, the expression/activation of cyclin D/cdk4,6 complex, which is triggered by the presence of mitotic growth factors, control the re-entry of resting (G0) cells into the G1 phase of cell cycle [11]. The G1/S transition, then, is controlled by the activation of the cyclin E/cdk2 complex [11] such that the absence of cyclin E and/or the inhibition of the cyclin E/cdk2 complex by p21, p27 and p53 causes the cell cycle to be arrested at the G1 checkpoint. The subsequent fate of the G1-arrested cells depends on the presence or absence of cyclin A [9] such that, in the absence of cyclin A, the cells return to G0 and re-differentiate. However, if allowed to proceed, in the presence of cyclin A, the cells are committed to division, lack the ability to re-differentiate and, if unable to complete the cell cycle, die via an apoptotic pathway [6]. Therefore, once beyond late G1, when cyclin A is expressed, arrest will lead to cell death.
The regulation of the cyclin–cdk complexes is achieved through cyclic proteolysis [12]. In a functioning cell, the mitotic cycle progresses as the appropriate cyclins are expressed while all others are inhibited. Furthermore, to enable the completion of one phase and the corresponding transition to another, the controlled proteolysis of the former’s cyclins effectively down-regulates the events of the first phase such that the next phase can proceed (through the subsequent up-regulation of its cyclins). As we shall see, however, despite the pivotal role of proteolysis in cell cycle regulation, the re-entrant phenotype characteristic of neurodegenerative disorders like AD is not the result of its reduced activity. Rather, it is a triggered departure from G0 to G1 (via cyclin D/cdk4, 6) that initiates the tragic demise of the cell [13–15].
Alzheimer disease and the cell cycle: overlapping phenotypes
Alzheimer disease is characterized by neurodegeneration and cognitive impairment and is the leading cause of senile dementia in the USA, affecting 15% of people over 65 years and almost 50% of those over 85 years [16]. Although the precise molecular mechanisms behind its pathogenesis are not fully understood, several key elements to the disease are noteworthy. Specifically, the hallmark features of AD, neurofibrillary tangles and amyloid-β (Aβ) plaques, while not the sole proprietors of neurodegeneration, are crucial to its development.
Amyloid-β is the major component of senile plaques characteristic of AD and is derived from its precursor, amyloid-β protein precursor (AβPP), which is encoded on chromosome 21 [17]. Its importance in disease is attested to the fact that mutations in the AβPP gene are directly linked to the onset of familial AD [18]. While recent evidence indicates the initial role of Aβ to be one of oxidative protection [19], its accumulation in neuronal tissue is certainly detrimental to cell functioning and survival. Specifically, Aβ-senile plaques elicit responses from surrounding microglial and astrocytic cells [20,21] and may ultimately ensure neuronal cell death through increased oxidative damage and further self-aggregation [22]. Interestingly, studies report AβPP to be up-regulated by mitogenic stimulation and that AβPP metabolism is controlled by cell cycle-dependant changes [23–25]. Even more, Aβ itself has been identified as mitogenic in vitro [23,24]; events of the cell cycle and their malfunctions have therefore been implicated in AD neurodegeneration.
Similarly, the major protein component of neurofibrillary tangles, a hyperphosphorylated form of the microtubule-associated protein tau [26,27], produces neuronal dysfunction in AD through microtubule destabilization. Notably, this hyperphosphorylated tau pathology is present in normal, mitotically active cells and has been linked to the activity of cdks [28,29]; once again, cell cycle mechanisms are indirectly involved in the process of AD onset and development.
Oxidative stress, another crucial aspect of the neurodegeneration associated with AD, has become increasingly significant in the pathogenesis of the disease over the past few years and has also been identified as concordant with markers of the cell cycle and its aberrations [3]. While its exact origins are not certain, it has been demonstrated to be one of the primary role-players in the onset of AD and in its development. That is, markers of oxidative stress, such as 8-hydroxyguanosine, precede general signs of AD in immunohistochemically stained neurones by decades [3,30]. Furthermore, Aβ, which has been revealed to be a high-valence metal chelator [31,32] and effective antioxidant in its soluble, non-aggregated form [31,33], may initially exist in the brain as a respondent mechanism for oxidative stress relief. Once oxidized, however, Aβ becomes insoluble and aggregates to impose the cellular burden for which it is known.
Importantly, though, recent research indicates a direct and reciprocally causal relationship between oxidative stress and cell cycle abnormalities [3], and it is this relationship that merits further investigation. In particular, a ‘two-hit’ hypothesis has been suggested whereby AD neurodegeneration becomes manifest as a result of both oxidative stress and cell cycle malfunctioning [3,34,35]. The disease pathogenesis, instigated by either one of the two aforementioned factors, develops as a combined process. For instance, oxidative stress, as one factor, damages neurones to eventually elicit the other factor, in this case cell cycle dysfunction. The effects of these two ‘hits’ ultimately initiate a detrimental cycle of oxidative stress, inflammation, Aβ aggregation, mitotic dysfunction and cell death that is responsible for disease. As such, cell cycle abnormalities offer a target for finding new therapeutic possibilities for patients.
Cell cycle malfunctions in Alzheimer disease
Several lines of evidence indicate the predominant role of cell cycle malfunctioning in the pathogenesis of AD. First, AD neurones exhibit significantly elevated levels of cell cycle markers representative of a departure from quiescence as compared with age-matched controls [3,13,14,36–38]. In particular, the presence of cyclin D, cdk4 and Ki67 in diseased neurones as well as cyclin E/cdk4 complex elevations confirm that the cells have indeed passed the G1 phase and are no longer in G0 [3,13,36]. Moreover, it seems that these indicators of cell cycle activation are located in the cell cytoplasm in AD vulnerable neurones rather than within the nucleus where they normally act [37,39,40]. A successful duplication of DNA in some AD neurones, as well as the presence of S-phase proteins like pmcm2 [41], even suggests a transition through the S-phase, and the appearance of aneuploidy strengthens this possibility [42].
Premature chromosome separation (PCS), a phenomenon that is responsible for diseases such as Robert’s syndrome and various cancers, and whose presence indicates a successful replication of DNA, as well as an abnormal mitotic phenotype presents convincing evidence for cell cycle re-entry in AD neurones [43]. Studies specifically demonstrate PCS appearing directly after DNA replication in G2 phase of the cell cycle, and evidence points to malfunctions of X-chromosome replication as being particularly prevalent: the presence of PCS in women statistically exceeds that in men [44], and women who are at risk for aneuploidy offspring (i.e. Down’s syndrome) exhibit twice the demonstrated relationship between loss of replication control, centromere dysfunction and predisposition to non-disjunction, possibly contributing to AD pathogenesis in these individuals [45,46]. The regulation of centromere and chromosome separation is orchestrated by the multitude of cell cycle proteins, such as cyclins and cyclin-dependant kinases, and thus the dysfunction of this process is another potential consequence of disturbed cellular cycling.
As previously mentioned, the presence of aberrant cell cycle makers in AD neurones significantly precedes the appearance of gross indicators of AD, and mitotic dysfunction is therefore implicated in disease onset and early development or predisposition. As such, there are several possible factors that might elicit vulnerable neurones to inappropriately re-enter the cell cycle. Mitotic signalling, in particular, seems to be partly responsible, as reports have identified an altered expression of the cell cycle-mediating G-protein, Ras, in AD-affected cells [2,47]. This protein is especially involved in the cellular transition from G0 to G1 phase through its interactions with cyclin D1 [10], and its downstream mediators, MAPK, Raf and MEK1/2, have all been identified as activated in AD neurones as compared with controls.
Some of the key genes already implicated in the pathogenesis of AD may contribute to aberrant cell cycle re-entry and consequent neurodegeneration. In particular, three genes, AβPP, and the homologous genes Presenilin 1 and Presenilin 2 (PS1/2), are associated with early onset AD [48,49] and have been implicated as the role-players in the cell cycle and cell cycle control. AβPP, a single-pass, transmembrane protein, is proteolytically cleaved to yield Aβ peptide; both proteins have been identified as mitogenic in vitro [23,24]. Particularly interesting is that AβPP-BP1, an adaptor protein involved in the cleavage of AβPP, is a cell cycle protein that regulates mitotic transition from S to M-phase. An overexpression of AβPP-BP1 would therefore push neurones into the S-phase and cause DNA replication and expression of corresponding cell cycle markers cdc2/cyclin B [4,10,50]. As these phenotypes are evident in AD neurodegeneration, it is possible that AβPP-BP1-induced cell cycle re-entry could be at least partially responsible.
Likewise, the PS1/2 genes, approximately 67% homologous, are responsible for the proteolytic cleavage of AβPP [10] and are thus also implicated in cell cycle control, as well as in the pathogenesis of AD. In the former scenario, the homologous genes have been associated with the centromere and centrosome of dividing cells [51], thus providing another link to mitogenic alterations in neurodegeneration, aside from the obvious interactions with AβPP. In particular, an overexpression of PS1 and PS2 in transfected HeLa cells resulted in G1 phase arrest in the cell cycle [10,52,53], while its deficiency produced accelerated transgression from G1 to S-phase [54]. As the PS1/2 genes are pivotal in the onset of some familial onset AD, a link between cell cycle aberration and neurodegeneration is possible.
Cell cycle aberrations contribute to neurodegeneration in AD
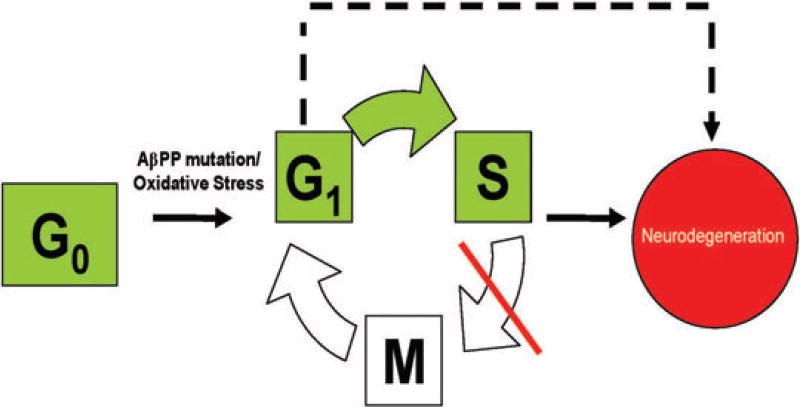
Regardless of the cause of cell cycle abnormalities evident in AD, the consequences are the same. That is, inappropriate re-entry into the cell cycle by already differentiated, adult neurones results in cellular dysfunction, premature cell death, and thus neurodegeneration [3] (Figure 1). Because the cell cycle integrates such a wide variety of cyclins and cyclin-dependant kinases, all with complex interactions within the cell that are vital for cell proliferation and survival, any alterations in their expression, functioning or control is likely to be damaging.
Figure 1.
Terminally differentiated neurones may re-enter the cell cycle via dysregulation induced by mutations in key genes (i.e. amyloid-β protein precursor or Presenilin 1 and Presenilin 2) or alternatively as a consequence of the vulnerability created by an oxidative steady state. Once in the cycle, the cells eventually die via apoptosis as they are unable to enter and complete M-phase (some even arresting after G1-phase completion). Neurodegeneration is thus the result, as shown.
Evidence indicates the re-entrant phenotype as one of inevitable cell death, as cells that inappropriately initiate mitosis fail to complete the M-phase, and thus die [3,10]. Specifically, despite all of the cell cycle markers that have been localized within adult neurones in AD brains, there has been no indication of an entry into or a completion of M-phase. While many cells do exhibit DNA replication, chromosome maintenance protein expression and binucleation events [55] (and thus a completion or at least entrance into S-phase [41,56]), and some cells have been observed in G2-phase [37,38], no study demonstrates an entrance into or completion of M-phase [40]. It seems as though these cells encounter a ‘mitotic catastrophe’ during which they are unable to complete the cell cycle as a result of inadequate control. Unfortunately, because they have already crossed the point of no return in mitosis (i.e. G1-phase/S-phase), affected neurones ultimately die.
It is of interest that the molecular mechanisms behind cell death associated with mitotic re-entry seem to be closely involved with oxidative stress. As both phenomena are manifest early in the pathogenesis of AD, and as advanced cases of AD exhibit markers of both [3], it seems likely that there is a relationship between the two processes in neurodegeneration. The ‘two-hit’ hypothesis proposes this case: either of the two cellular insults (oxidative stress or mitotic dysfunction) can initiate a combined process such that the combination produces cellular dysfunction and ultimately death [3]. In particular, the process involves the initial presence of a ‘steady state’ (following the expression of either oxidative stress or mitotic malfunction) and the corresponding compensatory adaptations that ultimately hinder overall cellular functioning [3].
In regard to mitotic abnormalities, studies with several transgenic mouse models indicate that neuronal cell cycle re-entry (due to mutations in AβPP, PS1 or PS2) precedes amyloid deposition, and thus full AD pathogenesis, by several months and occurs in an anatomical pattern that resembles the neuronal vulnerability seen in AD [3,57]. Although these mice demonstrate significant cell cycle re-entry at as early as 6 months of age, they maintained cognition and cellular functioning at a near-normal level for long periods of time [3]. Such mutant mice demonstrate a ‘mitotic steady state’ phenotype that eventually elicits further insult in the form of a ‘second hit’ of oxidative stress.
In the much more prevalent, sporadic form of AD (or late-onset AD), an ‘oxidative imbalance steady state’ has been demonstrated that predisposes affected neurones to develop cell cycle abnormalities as a ‘second hit’ [3]. Although neurones are capable of compensating for acute levels of oxidative stress in the brain, widespread accumulation of reactive oxidative species eventually requires cellular adaptations that describe a state of oxidative imbalance [58,59]. While these compensations might enable neurones to survive for decades under severe oxidative stress [60], their eventual accumulation leads to secondary cell cycle abnormalities, which lead ultimately to death.
Conclusions
Alterations in cell cycle control system are likely to play a role in neurodegeneration. While the precise origins of such mitotic dysfunction are not fully understood, oxidative defects do provide pathways from which altered cell cycle control could arise. In AD, a complex and reciprocal interaction between oxidative stress and cell cycle re-entry seems likely. Cell cycle dysfunction is a factor in the neuronal dysfunction in neurodegenerative disease with possible therapeutic avenues for disease control.
Acknowledgments
Work in the authors’ laboratories is supported by the National Institutes of Health (AG028679, AG030096, AG031364).
References
- 1.McShea A, Wahl AF, Smith MA. Re-entry into the cell cycle: a mechanism for neurodegeneration in Alzheimer disease. Med Hypotheses. 1999;52:525–7. doi: 10.1054/mehy.1997.0680. [DOI] [PubMed] [Google Scholar]
- 2.McShea A, Lee HG, Petersen RB, Casadesus G, Vincent I, Linford NJ, Funk JO, Shapiro RA, Smith MA. Neuronal cell cycle re-entry mediates Alzheimer disease-type changes. Biochim Biophys Acta. 2007;1772:467–72. doi: 10.1016/j.bbadis.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Zhu X, Lee HG, Perry G, Smith MA. Alzheimer disease, the two-hit hypothesis: an update. Biochim Biophys Acta. 2007;1772:494–502. doi: 10.1016/j.bbadis.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Zhu X, Raina AK, Smith MA. Cell cycle events in neurons. Proliferation or death? Am J Pathol. 1999;155:327–9. doi: 10.1016/S0002-9440(10)65127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee HG, Casadesus G, Zhu X, Castellani RJ, McShea A, Perry G, Petersen RB, Bajic V, Smith MA. Cell cycle re-entry mediated neurodegeneration and its treatment role in the pathogenesis of Alzheimer’s disease. Neurochem Int. 2009;54:84–8. doi: 10.1016/j.neuint.2008.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meikrantz W, Schlegel R. Apoptosis and the cell cycle. J Cell Biochem. 1995;58:160–74. doi: 10.1002/jcb.240580205. [DOI] [PubMed] [Google Scholar]
- 7.Wang W, Bu B, Xie M, Zhang M, Yu Z, Tao D. Neural cell cycle dysregulation and central nervous system diseases. Prog Neurobiol. 2009;89:1–17. doi: 10.1016/j.pneurobio.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Vincent I, Zheng JH, Dickson DW, Kress Y, Davies P. Mitotic phosphoepitopes precede paired helical filaments in Alzheimer’s disease. Neurobiol Aging. 1998;19:287–96. doi: 10.1016/s0197-4580(98)00071-2. [DOI] [PubMed] [Google Scholar]
- 9.Grana X, Reddy EP. Cell cycle control in mammalian cells: role of cyclins, cyclin dependent kinases (CDKs), growth suppressor genes and cyclin-dependent kinase inhibitors (CKIs) Oncogene. 1995;11:211–19. [PubMed] [Google Scholar]
- 10.Zhu X, Casadesus G, Raina AK, Perry G, Smith MA. Neuronal cell cycle re-entry: a doomed journey in Alzheimer disease? In: Özben T, Chevion M, editors. Frontiers in Neurodegenerative Disorders and Aging: Fundamental Aspects, Clinical Perspectives and New Insights. Amsterdam: IOS Press; 2004. pp. 200–6. [Google Scholar]
- 11.Sherr CJ. G1 phase progression: cycling on cue. Cell. 1994;79:551–5. doi: 10.1016/0092-8674(94)90540-1. [DOI] [PubMed] [Google Scholar]
- 12.Udvardy A. The role of controlled proteolysis in cell-cycle regulation. Eur J Biochem. 1996;240:307–13. doi: 10.1111/j.1432-1033.1996.0307h.x. [DOI] [PubMed] [Google Scholar]
- 13.McShea A, Harris PL, Webster KR, Wahl AF, Smith MA. Abnormal expression of the cell cycle regulators P16 and CDK4 in Alzheimer’s disease. Am J Pathol. 1997;150:1933–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Nagy Z, Esiri MM, Smith AD. Expression of cell division markers in the hippocampus in Alzheimer’s disease and other neurodegenerative conditions. Acta Neuropathol (Berl) 1997;93:294–300. doi: 10.1007/s004010050617. [DOI] [PubMed] [Google Scholar]
- 15.Smith TW, Lippa CF. Ki-67 immunoreactivity in Alzheimer’s disease and other neurodegenerative disorders. J Neuropathol Exp Neurol. 1995;54:297–303. doi: 10.1097/00005072-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Smith MA. Alzheimer disease. Int Rev Neurobiol. 1998;42:1–54. doi: 10.1016/s0074-7742(08)60607-8. [DOI] [PubMed] [Google Scholar]
- 17.Korenberg JR, Pulst SM, Neve RL, West R. The Alzheimer amyloid precursor protein maps to human chromosome 21 bands q21.105-q21.05. Genomics. 1989;5:124–7. doi: 10.1016/0888-7543(89)90095-5. [DOI] [PubMed] [Google Scholar]
- 18.Hellstrom-Lindahl E, Viitanen M, Marutle A. Comparison of Abeta levels in the brain of familial and sporadic Alzheimer’s disease. Neurochem Int. 2009;55:243–52. doi: 10.1016/j.neuint.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moreira PI, Santos MS, Oliveira CR, Shenk JC, Nunomura A, Smith MA, Zhu X, Perry G. Alzheimer disease and the role of free radicals in the pathogenesis of the disease. CNS Neurol Disord Drug Targets. 2008;7:3–10. doi: 10.2174/187152708783885156. [DOI] [PubMed] [Google Scholar]
- 20.Morgan D. The role of microglia in antibody-mediated clearance of amyloid-beta from the brain. CNS Neurol Disord Drug Targets. 2009;8:7–15. doi: 10.2174/187152709787601821. [DOI] [PubMed] [Google Scholar]
- 21.Piazza A, Lynch MA. Neuroinflammatory changes increase the impact of stressors on neuronal function. Biochem Soc Trans. 2009;37:303–7. doi: 10.1042/BST0370303. [DOI] [PubMed] [Google Scholar]
- 22.Ong WY, Farooqui AA. Iron, neuroinflammation, and Alzheimer’s disease. J Alzheimers Dis. 2005;8:183–200. doi: 10.3233/jad-2005-8211. discussion 9–15. [DOI] [PubMed] [Google Scholar]
- 23.Schubert D, Cole G, Saitoh T, Oltersdorf T. Amyloid beta protein precursor is a mitogen. Biochem Biophys Res Commun. 1989;162:83–8. doi: 10.1016/0006-291x(89)91965-7. [DOI] [PubMed] [Google Scholar]
- 24.Milward EA, Papadopoulos R, Fuller SJ, Moir RD, Small D, Beyreuther K, Masters CL. The amyloid protein precursor of Alzheimer’s disease is amediator of the effects of nerve growth factor on neurite outgrowth. Neuron. 1992;9:129–37. doi: 10.1016/0896-6273(92)90228-6. [DOI] [PubMed] [Google Scholar]
- 25.Copani A, Condorelli F, Caruso A, Vancheri C, Sala A, Giuffrida Stella AM, Canonico PL, Nicoletti F, Sortino MA. Mitotic signaling by beta-amyloid causes neuronal death. FASEB J. 1999;13:2225–34. [PubMed] [Google Scholar]
- 26.Iqbal K, Zaidi T, Thompson CH, Merz PA, Wisniewski HM. Alzheimer paired helical filaments: bulk isolation, solubility, and protein composition. Acta Neuropathol (Berl) 1984;62:167–77. doi: 10.1007/BF00691849. [DOI] [PubMed] [Google Scholar]
- 27.Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI. Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci USA. 1986;83:4913–17. doi: 10.1073/pnas.83.13.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brion JP. Immunological demonstration of tau protein in neurofibrillary tangles of Alzheimer’s disease. J Alzheimers Dis. 2006;9:177–85. doi: 10.3233/jad-2006-9s321. [DOI] [PubMed] [Google Scholar]
- 29.Brion JP, Octave JN, Couck AM. Distribution of the phosphorylated microtubule-associated protein tau in developing cortical neurons. Neuroscience. 1994;63:895–909. doi: 10.1016/0306-4522(94)90533-9. [DOI] [PubMed] [Google Scholar]
- 30.Nunomura A, Perry G, Pappolla MA, Friedland RP, Hirai K, Chiba S, Smith MA. Neuronal oxidative stress precedes amyloid-beta deposition in Down syndrome. J Neuropathol Exp Neurol. 2000;59:1011–17. doi: 10.1093/jnen/59.11.1011. [DOI] [PubMed] [Google Scholar]
- 31.Nunomura A, Moreira PI, Lee HG, Zhu X, Castellani RJ, Smith MA, Perry G. Neuronal death and survival under oxidative stress in Alzheimer and Parkinson diseases. CNS Neurol Disord Drug Targets. 2007;6:411–23. doi: 10.2174/187152707783399201. [DOI] [PubMed] [Google Scholar]
- 32.Zou K, Gong JS, Yanagisawa K, Michikawa M. A novel function of monomeric amyloid beta-protein serving as an antioxidant molecule against metal-induced oxidative damage. J Neurosci. 2002;15:4833–41. doi: 10.1523/JNEUROSCI.22-12-04833.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kontush A, Berndt C, Weber W, Akopyan V, Arlt S, Schippling S, Beisiegel U. Amyloid-beta is an antioxidant for lipoproteins in cerebrospinal fluid and plasma. Free Radic Biol Med. 2001;30:119–28. doi: 10.1016/s0891-5849(00)00458-5. [DOI] [PubMed] [Google Scholar]
- 34.Zhu X, Castellani RJ, Takeda A, Nunomura A, Atwood CS, Perry G, Smith MA. Differential activation of neuronal ERK, JNK/SAPK and p38 in Alzheimer disease: the ‘two hit’ hypothesis. Mech Ageing Dev. 2001;123:39–46. doi: 10.1016/s0047-6374(01)00342-6. [DOI] [PubMed] [Google Scholar]
- 35.Zhu X, Raina AK, Perry G, Smith MA. Alzheimer’s disease: the two-hit hypothesis. Lancet Neurol. 2004;3:219–26. doi: 10.1016/S1474-4422(04)00707-0. [DOI] [PubMed] [Google Scholar]
- 36.Vincent I, Rosado M, Davies P. Mitotic mechanisms in Alzheimer’s disease? J Cell Biol. 1996;132:413–25. doi: 10.1083/jcb.132.3.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vincent I, Jicha G, Rosado M, Dickson DW. Aberrant expression of mitotic cdc2/cyclin B1 kinase in degenerating neurons of Alzheimer’s disease brain. J Neurosci. 1997;17:3588–98. doi: 10.1523/JNEUROSCI.17-10-03588.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagy Z, Esiri MM, Cato AM, Smith AD. Cell cycle markers in the hippocampus in Alzheimer’s disease. Acta Neuropathol (Berl) 1997;94:6–15. doi: 10.1007/s004010050665. [DOI] [PubMed] [Google Scholar]
- 39.Ogawa O, Lee HG, Zhu X, Raina A, Harris PL, Castellani RJ, Perry G, Smith MA. Increased p27, an essential component of cell cycle control, in Alzheimer’s disease. Aging Cell. 2003;2:105–10. doi: 10.1046/j.1474-9728.2003.00042.x. [DOI] [PubMed] [Google Scholar]
- 40.Ogawa O, Zhu X, Lee HG, Raina A, Obrenovich ME, Bowser R, Ghanbari HA, Castellani RJ, Perry G, Smith MA. Ectopic localization of phosphorylated histone H3 in Alzheimer’s disease: a mitotic catastrophe? Acta Neuropathol (Berl) 2003;105:524–8. doi: 10.1007/s00401-003-0684-3. [DOI] [PubMed] [Google Scholar]
- 41.Bonda DJ, Evans TA, Santocanale C, Llosa JC, Vina J, Bajic VP, Castellani RJ, Siedlak SL, Perry G, Smith MA, Lee HG. Evidence for the progression through S-phase in the ectopic cell cycle re-entry of neurons in Alzheimer disease. Aging (Milano) 2009;1:382–8. doi: 10.18632/aging.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taupin P. Alzheimer’s disease, aneuploidy and neurogenesis. Med Sci Monit. 2008;14:LE6. [PubMed] [Google Scholar]
- 43.Spremo-Potparevic B, Zivkovic L, Djelic N, Plecas-Solarovic B, Smith MA, Bajic V. Premature centromere division of the X chromosome in neurons in Alzheimer’s disease. J Neurochem. 2008;106:2218–23. doi: 10.1111/j.1471-4159.2008.05555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bajic VP, Spremo-Potparevic B, Zivkovic L, Bonda DJ, Siedlak SL, Casadesus G, Lee HG, Smith MA. The X-chromosome instability phenotype in Alzheimer’s disease: a clinical sign of accelerating aging? Med Hypotheses. 2009;73:917–20. doi: 10.1016/j.mehy.2009.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Amiel A, Reish O, Gaber E, Kedar I, Diukman R, Fejgin M. Replication asynchrony increases in women at risk for aneuploid offspring. Chromosome Res. 2000;8:141–50. doi: 10.1023/a:1009246603868. [DOI] [PubMed] [Google Scholar]
- 46.Amiel A, Litmanovich T, Gaber E, Lishner M, Avivi L, Fejgin MD. Asynchronous replication of p53 and 21q22 loci in chronic lymphocytic leukemia. Hum Genet. 1997;101:219–22. doi: 10.1007/s004390050619. [DOI] [PubMed] [Google Scholar]
- 47.Gartner U, Holzer M, Arendt T. Elevated expression of p21ras is an early event in Alzheimer’s disease and precedes neurofibrillary degeneration. Neuroscience. 1999;91:1–5. doi: 10.1016/s0306-4522(99)00059-7. [DOI] [PubMed] [Google Scholar]
- 48.Manzano S, Gonzalez J, Marcos A, Matias-Guiu J. Genetics and Alzheimer’s disease. Neurologia. 2009;24:83–9. [PubMed] [Google Scholar]
- 49.Prat MI, Adamo AM, Gonzalez SA, Affranchino JL, Ikeda M, Matsubara E, Shoji M, Smith MA, Castano EM, Morelli L. Presenilin 1 overexpressions in Chinese hamster ovary (CHO) cells decreases the phosphorylation of retinoblastoma protein: relevance for neurodegeneration. Neurosci Lett. 2002;326:9–12. doi: 10.1016/s0304-3940(02)00298-7. [DOI] [PubMed] [Google Scholar]
- 50.Yang Y, Geldmacher DS, Herrup K. DNA replication precedes neuronal cell death in Alzheimer’s disease. J Neurosci. 2001;21:2661–8. doi: 10.1523/JNEUROSCI.21-08-02661.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dewji NN, Singer SJ. Cell surface expression of the Alzheimer disease-related presenilin proteins. Proc Natl Acad Sci USA. 1997;94:9926–31. doi: 10.1073/pnas.94.18.9926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Janicki SM, Stabler SM, Monteiro MJ. Familial Alzheimer’s disease presenilin-1 mutants potentiate cell cycle arrest. Neurobiol Aging. 2000;21:829–36. doi: 10.1016/s0197-4580(00)00222-0. [DOI] [PubMed] [Google Scholar]
- 53.Janicki SM, Monteiro MJ. Presenilin overexpression arrests cells in the G1 phase of the cell cycle. Arrest potentiated by the Alzheimer’s disease PS2(N141I)mutant. Am J Pathol. 1999;155:135–44. doi: 10.1016/S0002-9440(10)65108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Soriano S, Kang DE, Fu M, Pestell R, Chevallier N, Zheng H, Koo EH. Presenilin 1 negatively regulates beta-catenin/T cell factor/lymphoid enhancer factor-1 signaling independently of beta-amyloid precursor protein and notch processing. J Cell Biol. 2001;19:785–94. doi: 10.1083/jcb.152.4.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu X, Siedlak SL, Wang Y, Perry G, Castellani RJ, Cohen ML, Smith MA. Neuronal binucleation in Alzheimer disease hippocampus. Neuropathol Appl Neurobiol. 2008;34:457–65. doi: 10.1111/j.1365-2990.2007.00908.x. [DOI] [PubMed] [Google Scholar]
- 56.Mosch B, Morawski M, Mittag A, Lenz D, Tarnok A, Arendt T. Aneuploidy and DNA replication in the normal human brain and Alzheimer’s disease. J Neurosci. 2007;27:6859–67. doi: 10.1523/JNEUROSCI.0379-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang Y, Varvel NH, Lamb BT, Herrup K. Ectopic cell cycle events link human Alzheimer’s disease and amyloid precursor protein transgenic mouse models. J Neurosci. 2006;26:775–84. doi: 10.1523/JNEUROSCI.3707-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu X, Lee HG, Casadesus G, Avila J, Drew K, Perry G, Smith MA. Oxidative imbalance in Alzheimer’s disease. Mol Neurobiol. 2005;31:205–17. doi: 10.1385/MN:31:1-3:205. [DOI] [PubMed] [Google Scholar]
- 59.Ogawa O, Zhu X, Perry G, Smith MA. Mitochondrial abnormalities and oxidative imbalance in neurodegenerative disease. Sci Aging Knowledge Environ. 2002;2002:16. doi: 10.1126/sageke.2002.41.pe16. [DOI] [PubMed] [Google Scholar]
- 60.Morsch R, Simon W, Coleman PD. Neurons may live for decades with neurofibrillary tangles. J Neuropathol Exp Neurol. 1999;58:188–97. doi: 10.1097/00005072-199902000-00008. [DOI] [PubMed] [Google Scholar]