Abstract
Adoptive T cell therapy using chimeric antigen receptor (CAR)-modified T cells is a promising cancer immunotherapy. We previously developed a non-viral method of gene transfer into T cells using a piggyBac transposon system to improve the cost-effectiveness of CAR-T cell therapy. Here, we have further improved our technology by a novel culture strategy to increase the transfection efficiency and to reduce the time of T cell manufacturing. Using a CH2CH3-free CD19-specific CAR transposon vector and combining irradiated activated T cells (ATCs) as feeder cells and virus-specific T cell receptor (TCR) stimulation, we achieved 51.4% ± 14% CAR+ T cells and 2.8-fold expansion after 14 culture days. Expanded CD19.CAR-T cells maintained a significant fraction of CD45RA+CCR7+ T cells and demonstrated potent antitumor activity against CD19+ leukemic cells both in vitro and in vivo. Therefore, piggyBac-based gene transfer may provide an alternative to viral gene transfer for CAR-T cell therapy.
Keywords: chimeric antigen receptor, non-viral vector, piggyBac, transposon, virus-specific antigens, acute lymphoblastic leukemia, refractory
Introduction
Adoptive immunotherapy using chimeric antigen receptors (CARs) to target tumor-associated antigens represents a novel approach for the treatment of hematological malignancies. In particular, CD19.CAR-T cells promoted substantial clinical responses in the patients with refractory or relapsed acute lymphoblastic leukemia (ALL).1, 2, 3, 4
CAR expression in T cells is generally obtained via gene transfer with viral vectors. To reduce the costs of manufacturing and potentially enhance the safety of the gene transfer procedure, we developed a non-viral method of gene transfer in T cells using the piggyBac transposon system.5, 6, 7 We found that the piggyBac transposon system allows the generation of highly functional CD19.CAR-T cells.8 However, our in vitro culture procedure for expanding piggyBac-modified CD19.CAR-T cells remains suboptimal since it requires a step of magnetic cell isolation to enrich the T cell product in CAR+ T cells and more than 21 days of culture to generate sufficient numbers of T cells for clinical adoptive transfer. Furthermore, our CAR included a long IgG1-CH2CH3 spacer that might abrogate the in vivo antitumor activity.9, 10, 11
The aim of the present study was to improve the manufacturing of piggyBac-modified CD19.CAR-T cells to achieve high levels of CAR expression and reduce the duration of the in vitro culture. We hypothesized that these goals can be obtained by (1) adding autologous activated T cells (ATCs), which express multiple co-stimulatory molecules, as feeder cells; (2) stimulating T cells via viral antigens rather than mitogenic anti-CD3/CD28 monoclonal antibodies (mAbs); and (3) using a CH2CH3-free CD19.CAR construct to render in vivo persistence and antitumor activity.
Results
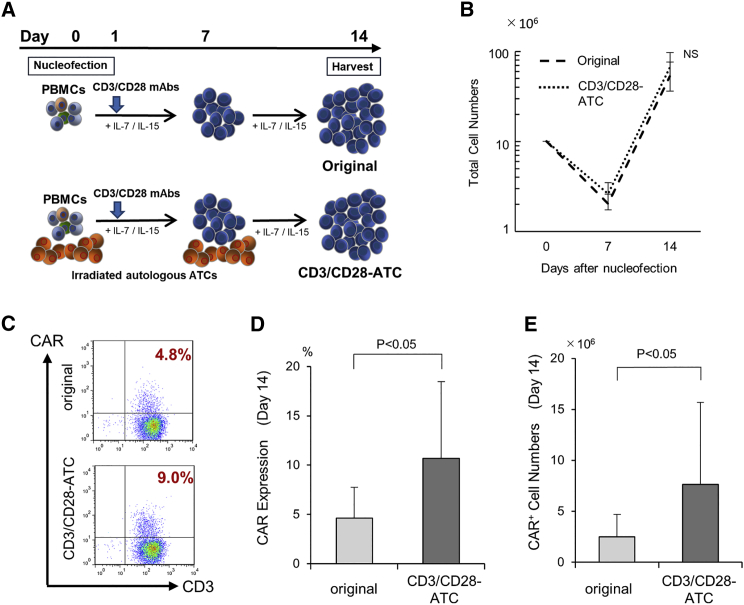
Feeder-Irradiated Autologous ATCs Enhance CAR Expression in piggyBac-Modified CD19.CAR-T Cells
We previously reported that feeder cells enhance the expansion rate of piggyBac-modified T cells.5 To determine whether autologous ATCs can improve the expansion and CAR expression of piggyBac-modified CD19.CAR-T cells, irradiated autologous ATCs were added to the culture on days 0 and 7 after transfection. In brief, peripheral blood mononuclear cells (PBMCs) were transfected with CD19.CAR encoding PB transposon and stimulated on anti-CD3/CD28 mAb-coated plates supplemented with interleukin (IL)-7 (10 ng/mL) and IL-15 (5 ng/mL), in the presence (CD3/CD28-ATC method) or absence (original method) of autologous ATCs (Figure 1A). While T cell proliferation was comparable in the two culture conditions (Figure 1B), T cells generated with feeder ATCs (CD3/CD28-ATC) exhibited significantly higher levels of CAR expression (10.7% ± 7.8%) compared to those with no feeder ATCs (original) (4.6% ± 3.2%) (p = 0.029) (Figures 1C and 1D). As a consequence, the absolute number of CAR+ T cells at the end of the culture expansion increased from 2.6 ± 2.2 × 106 cells (original method) to 7.6 ± 8.0 × 106 cells (CD3/CD28-ATC) (p = 0.049) (Figure 1E). These results suggest that irradiated ATCs helps in increasing the frequency of CAR-expressing T cells.
Figure 1.
Feeder Irradiated Autologous Activated T Cells Enhance CAR Expression in piggyBac-Modified CD19.CAR-T Cells
(A) Schematic explanation of the generation method of PB-modified CD19.CAR-T cells in the original or the CD3/CD28-ATC condition. 1 × 107 of PBMCs were transfected with CD19.CAR via the piggyBac transposon system and stimulated on a CD3/CD28 mAb-coated plate supplemented with IL-7 and IL-15 in the absence (original method) or presence (CD3/CD28-ATC method) of autologous activated T cells (ATCs) as feeder cells. In the CD3/CD28-ATC method, irradiated autologous ATCs were added on day 0 and day 7 following nucleofection. Fourteen days after nucleofection, cells were harvested and analyzed. (B) Ex vivo expansion of PB-modified CD19.CAR-T cells. Cell numbers were determined via a trypan blue exclusion assay on days 7 and 14. Data are presented as the mean ± SD of experiments from nine donors. (C and D) CD19.CAR expression on PB-modified T cells was examined via flow cytometry with the use of a specific anti-idiotype scFv mAbs. Representative (C) and summary (D) results from nine donors are shown. (E) Absolute CAR+ T cell numbers were calculated based on the total cell numbers and CAR+CD3+ percentages by flow cytometry. The data are presented as the mean ± SD from nine donors.
Although higher numbers of CAR+ T cells were obtained using feeder ATCs, their frequencies remain suboptimal for the clinical application. These results prompted us to further improve our method of CAR-T cell generation.
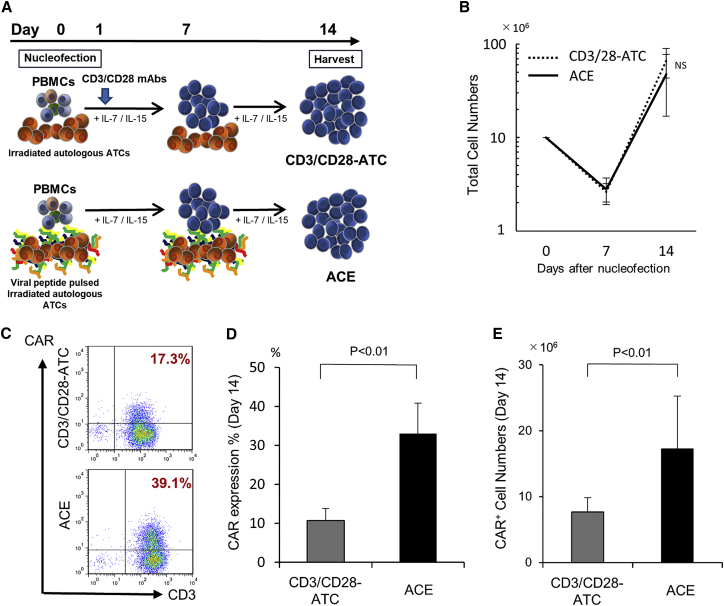
Virus-Specific TCR Stimulation Increases CAR Expression in piggyBac-Modified CD19.CAR-T Cells
To determine whether physiological T cell receptor (TCR) stimulation enhances CAR expression and expansion of piggyBac-modified CD19.CAR-T cells, we used a mix of four common viral antigens (ACE; AdV5 Hexon, CMV pp65, EBV EBNA-1, and BZLF1) for the stimulation of T cells. In brief, piggyBac-modified CD19.CAR-T cells were stimulated twice by either irradiated ATCs pulsed with ACE viral peptides (ACE CAR) or ATCs and anti-CD3/CD28 mAbs (CD3/CD28-ATC CAR) (Figure 2A). T cell expansion rates were comparable for 14 days of culture (Figure 2B). In contrast, ACE CAR-T cells exhibited significantly higher (33.0% ± 9.7%) CAR expression than the CD3/CD28-ATC CAR-T cells (10.7% ± 7.8%; p = 0.001) (Figures 2C and 2D). Furthermore, the mean fluorescence intensity of the CAR expression was significantly higher in ACE CAR-T cells than those of both original and CD3/CD28-ATC CAR-T cells (Figures S1 and S2). As a consequence, ACE CAR-T cells showed higher absolute numbers of CAR+ T cells (17.2 × 106) at the end of the culture period as compared to CD3/CD28-ATC CAR method (7.6 × 106; p = 0.047) (Figure 2E). CAR+ T cell numbers in the ACE CAR-T group were 6.6-fold higher (p = 0.028) than those generated using the original method (2.6 ± 2.2 × 106) (Figures 1E and 2E).
Figure 2.
Viral Antigen Stimulation Significantly Increases CAR Expression in PB-Modified CD19-Specific T Cells
(A) Schematic explanation of the generation method of PB-modified CD19.CAR-T cells in the CD3/CD28-ATC or the ACE condition. 1 × 107 of PBMCs were transfected with CD19.CAR via the piggyBac transposon system and stimulated with either irradiated autologous ATCs and CD3/CD28 mAbs (CD3/CD28-ATC CAR method) or irradiated autologous ATCs pulsed with viral peptides (ACE CAR method) on days 0 and 7 after nucleofection. The cells were harvested and analyzed on day 14. (B) Ex vivo expansion of PB-modified CD19.CAR-T cells. Cell numbers were determined by a trypan blue exclusion assay on days 7 and 14. Data are presented as the mean ± SD of experiments from nine donors. (C and D) CD19.CAR expression on PB-modified T cells was examined by flow cytometry. Representative (C) and summary (D) results from nine donors are shown. The results are presented as the mean ± SD. (E) CAR+ T cell numbers are calculated based on the total cell numbers and CD3+ CAR+ percentages determined by flow cytometry. Data are presented as the mean ± SD from nine donors.
We assessed the secretion of interferon (IFN)-γ in response to the four common viral antigens (ACE; AdV5 Hexon, CMV pp65, EBV EBNA-1, and BZLF1) using the enzyme-linked immunosorbent spot (ELISpot) assay to determine the virus-specific activity of the generated CAR-T cells. Unexpectedly, IFN-γ secretion minimally increased in response to viral antigens by ACE CAR-T cells relative to the background IFN-γ secretion in the negative control (Figure S3).
To determine whether the presence of CAR in T cells attenuated the virus-specific activity, we separately evaluated the virus-specific activity by intracellular cytokine assay in both CAR and NT population of ACE CAR-T cells from donor 1, which demonstrated apparent virus specificity on day 14. Although IFN-γ in response to pp65 antigen was detected in the CAR− population, it was minimally detected in the CAR+ population (Figure S4). To confirm this, we compared the virus specificity between CAR-transduced and non-transduced (NT) T cells, both stimulated by autologous ATCs and ACE viral peptides. As compared to ACE CAR-T cells, ACE NT-T cells demonstrated a tendency of increased virus-specific activities against viral antigens (Figure S5). Furthermore, sequential ELISpot assays showed that ACE CAR-T cells seem to maintain the virus specificity by day 7 but lose their specificity by day 14 as compared to ACE NT-T cells (Figure S6). These results suggested that the presence of CAR might be one of the reasons for the attenuated virus-specific activity in ACE CAR-T cells after the second stimulation of ACE peptides.
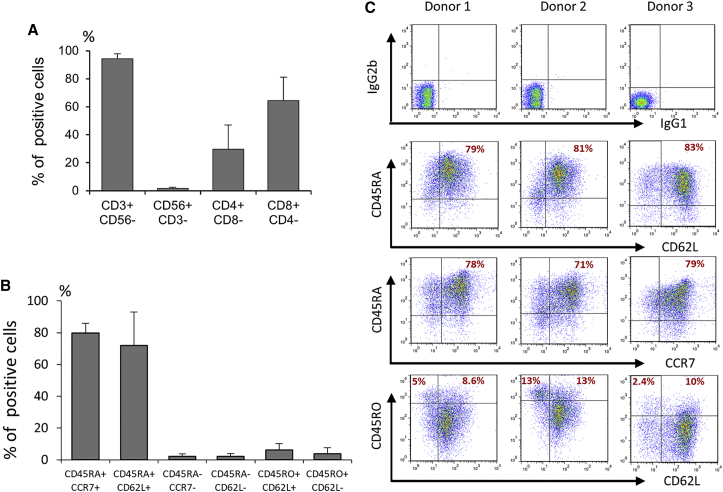
To characterize the immunophenotypic composition of the T cell products, the cells were harvested and analyzed by flow cytometry by day 14 after transfection. As shown in Figure 3A, ACE CD19.CAR-T cells consisted of 94.2% ± 3.7% CD3+ T cells with a higher percentage of CD8+ (79.9% ± 5.9%) than CD4+ (29.6% ± 17.3%) T cells. CD56+CD3− NK cells account for 1.6% ± 1.0% of the total cells as previously described.8 Furthermore, ACE CD19.CAR-T cells contained 79.9% ± 5.9% cells which co-expressed CD45RA and CCR7 (Figures 3B and 3C) that resemble naive or stem cell memory-like T cell phenotype.8 In contrast, ACE NT-T cells exhibited more differentiated phenotype (Figure S7), consistent with their virus-specific activity.
Figure 3.
The Major Subset of ACE CAR-T Cells Was Phenotypically CD8+CD45RA+CCR7+, Closely Related to T-Memory Stem Cells
The phenotypical analysis of ACE CAR-T cells was performed on day 14 after nucleofection. (A) Mean percentages of CD3+CD56−, CD56+CD3−, CD4+CD8−, and CD8+CD4− are shown. Data are represented as the mean ± SD from nine donors. (B) Mean percentages of CD45RA+CCR7+, CD45RA+CD62L+, CD45RA−CCR7−, CD45RO+CD62L+, and CD45RO+CD62L− are shown. Data are represented as the mean ± SD from nine donors. (C) Isotype control, CD45RA/CD62L, CD45RA/CCR7, and CD45RO/CD62L expressions in ACE CAR-T cells. Representative results from three donors are shown.
To investigate whether virus-specific TCR stimulation reduces the rate of activation-induced cell death as compared to anti-CD3/CD28 mAb stimulation, 7 days after stimulation, the frequency of apoptotic cells was evaluated by flow cytometry. As shown in Figure S8, ACE CD19.CAR-T cells showed a trend for a lower frequency of Annexin V+ cells within the CAR+ T cells as compared to CD19.CAR-T cells stimulated with anti-CD3/CD28 mAbs. These results suggest that anti-CD3/CD28 mAb TCR stimulation may induce more apoptosis in T cells leading to an overall lower output of CAR+ T cells.
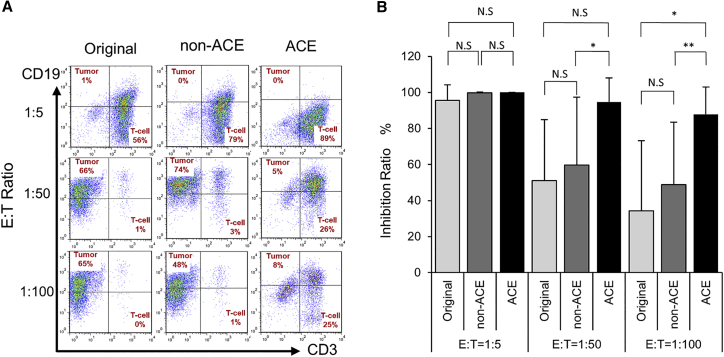
ACE CD19.CAR-T Cells Exert an Anti-leukemic Effect In Vitro
To evaluate the anti-leukemic effects of ACE CD19.CAR-T cells in vitro, we co-cultured ACE CAR-T cells with SU/SR, tyrosine kinase inhibitors-resistant CD19+ ALL cell line.8, 12 As shown in Figures 4A and 4B, ACE CD19.CAR-T cells showed significantly higher elimination of SU/SR cells (94.7% and 87.8%) compared to both CD3/CD28-ATC CAR-T (59.6% and 48.7%) and original CAR-T cells (51% and 34.4%) at the effector:target (E:T) ratios of 1:50 and 1:100, respectively. These results suggest that ACE CD19.CAR-T cells have potent anti-leukemic effect in vitro.
Figure 4.
ACE CD19.CAR-T Cells Exhibited Potent Antitumor Activity against CD19+ Tumors, Even at a Very Low E:T Ratio
CD19.CAR-T cells generated by the original, CD3/CD28-ATC, or ACE CAR methods were co-cultured with CD19+ tumor cells (SU/SR) at effector:target (E:T) ratios of 1:5, 1:50, and 1:100 without cytokines for 5 days. The number of viable cells was determined using a trypan blue exclusion test, and the percentages of T cells and CD19+ cells were determined by flow cytometry. (A) Representative flow cytometry results on day 5 after co-culture are shown. (B) Inhibition ratio were calculated by dividing the input CD19+ cell number by the CD19+ cell numbers in tumor only condition. Data are presented as the mean ± SD of experiments from nine donors. *p < 0.05; **p < 0.01.
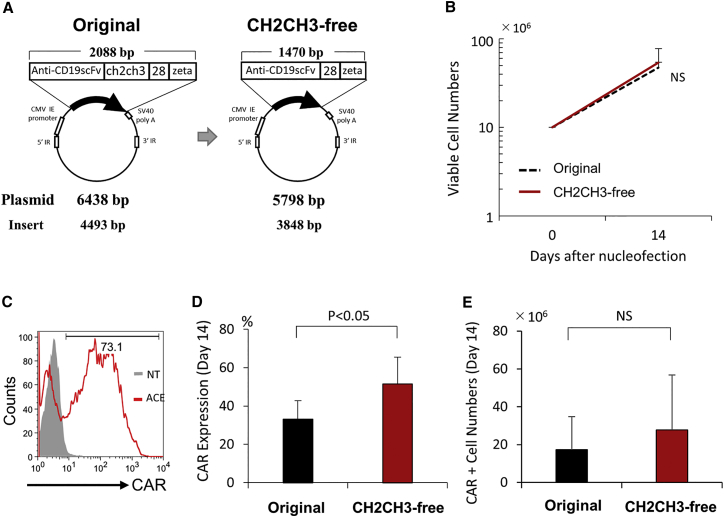
ACE CD19.CAR-T Cells with a New Transposon Vector with No CH2CH3 Hinge Region Show Higher CAR Expression
Recently, several groups have suggested that the long CH2CH3 hinge region may attenuate in vitro lysis of tumor cells9 or induce killing of monocytes10 and in vivo expansion of CAR-T cells.11 To provide better in vivo persistence and antitumor activity, we constructed a new transposon vector (CH2CH3-free) by removing the spacer region from the original CD19.CAR vector (original) based on the construct developed by Kochenderfer et al.13 (GenBank: HM852952.1). Therefore, this new vector is 645 bp shorter than the original vector as a result of the deletion (Figure 5A). We then generated ACE CAR-T cells using either the original or the CH2CH3-free vector (Figure 5A). Overall, T cell expansion was similar (Figure 5B), but the CH2CH3-free construct led to significantly higher CAR expression (51.4% ± 14%) compared to the original construct (33.0% ± 9.7%) (p = 0.034) (Figures 5C and 5D) and a trend of an increase in the absolute number of CAR+ T cells (27.8 ± 28.0 × 106 versus 17.2 ± 17.0 × 106) (p = 0.23) (Figure 5E). Similar to the results from the original vector, ACE CAR-T cells with CH2CH3-free transposon vector contained a significant fraction of CD3+CD45RA+CCR7+ T cells (Figure S9).
Figure 5.
The Use of a New Transposon Vector without CH2CH3 Further Enhances the CAR Expression in PB-Modified T Cells
(A) Schematic representation of the transposon plasmid encoding CD19.CAR (pIRII-CAR.CD19-28-ζ) with (original vector) or without (short vector) IgG-CH2CH3 hinge region. The size of the CD19.CAR plasmid was reduced from 6,438 bp to 5,798 bp by depleting the IgG1-CH2CH3 spacer. Plasmid and insert sizes of each vector are also shown. (B) Ex vivo expansion of ACE CAR-T with the original or the short transposon vector. PBMCs were transfected with either the original or the short transposon vector encoding CD19.CAR and cultured using the ACE CAR-T method. Cell numbers were determined by a trypan blue exclusion assay on days 7 and 14. The data are presented as the mean ± SD of experiments from nine donors. (C and D) CD19.CAR expression on PB-modified T cells was examined by flow cytometry. Representative results (C) and summary results (D) from nine donors are shown.
Although we compared the frequency of apoptotic cells between two CD19.CAR vectors 7 days after stimulation to investigate whether ACE CAR-T cells with CH2CH3-free construct reduced induced apoptotic cell death, no differences were observed in the frequencies of apoptotic cells between the two ACE CAR-T cell lines with either original vector or CH2CH3-free vector (data not shown).
In addition, we co-cultured CD19+ leukemic cells and analyzed them using flow cytometry to evaluate the in vitro antitumor activity of CH2CH3-free ACE CAR-T cells. Figure S10 shows that ACE CAR-T cells with CH2CH3-free vector demonstrated a comparable antitumor activity (Figure S10A) and IFN-γ secretion (Figure S10B) against SU/SR cells. These results suggested an equivalent in vitro antitumor activity of CH2CH3-free ACE CAR-T cells as compared to those with original vector.
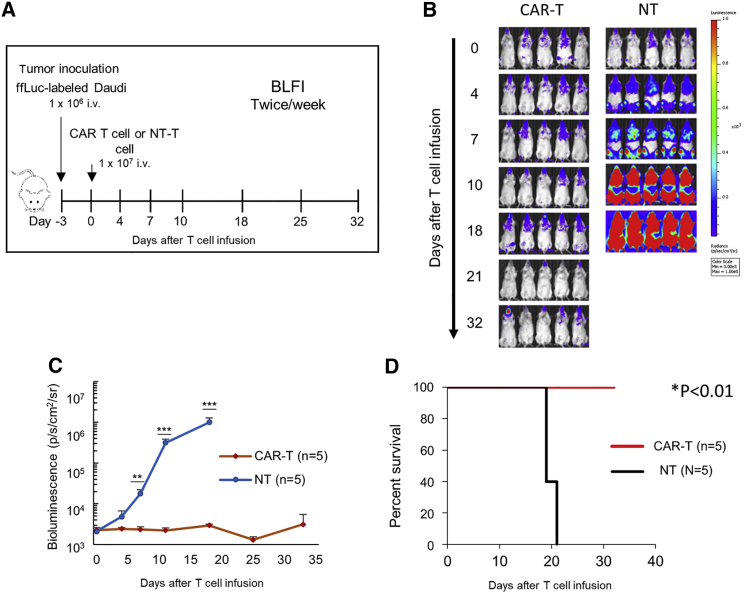
ACE CD19.CAR-T Cells Exhibit an Antitumor Effect In Vivo
To evaluate the antitumor activity of ACE CD19 CAR-T cells in vivo, we intravenously engrafted firefly luciferase (ffLuc)-labeled CD19+ Daudi cells in NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice and subsequently infuse them with either control NT T cells or ACE CH2CH3-free CD19.CAR-T cells 3 days following tumor inoculation (Figure 6A). Mice treated with ACE CD19.CAR-T cells showed significantly lower tumor luminescence on days 7, 11, and 18 after tumor inoculation as compared to the mice in the control T cell group (Figures 6B and 6C). The lower tumor luminescence in mice treated with ACE CD19.CAR-T cells was associated with an improved overall survival rate (p < 0.001) (Figure 6D). These results suggest that ACE CD19.CAR-T cells can control the growth of CD19+ tumor cells in vivo.
Figure 6.
ACE CD19.CAR-T Cells Potently Reject CD19+ Leukemic Cells in a Mouse Xenograft Model
(A) NSG mice received intravenous injections (i.v.) of 1 × 106 Daudi cells co-expressing eGFP and ffLuc and were subsequently intravenously infused with 1 × 107 CD19.CAR-T cells 3 days after tumor cell injection. Control mice were intravenously infused with 1 × 107 non-transduced T cells. (B) Representative bioluminescent imaging (BLI) of tumor progression following the i.v. administration of tumor cells with either non-transduced or ACE CD19.CAR-T cells are shown. (C) The mean radiance of tumor progression imaged with BLI in mice bearing Daudi cells is shown. **p < 0.01; ***p < 0.001. (D) Kaplan-Meier survival curves present the overall survival. Significance was determined using a log-rank test.
Discussion
In the present study, we developed a novel method of piggyBac transposon-based generation of CAR-T cells that has high potential for the clinical translation since it achieves high expression of the CAR in T cells and adequate expansion of T cells that retain memory phenotype.
Non-viral gene transfer methodologies, including piggyBac transposon, are usually characterized by low transfection efficiency, thus requiring magnetic purification of CAR+ cells and long-term ex vivo culture for generating CAR-T cells for clinical use.8 In this study, by adding ATCs as a feeder and using alternative means of TCR stimulation using viral antigens, more than 30% of the expanded T cells expressed the CAR. In addition, CAR expression significantly increased to approximately 50% by just reducing the size of the CAR cassette, eliminating the long IgG1.CH2CH3 spacer. Our experiments also indicate that 27.8 ± 28.0 × 106 CAR+ T cells can be expanded starting from 10 × 106 PBMCs in 14 days of culture. As several studies have shown that of 1 − 3 × 106/kg CD19. CAR+ T cells can induce clinical responses,4, 14, 15 our proposed strategy seems sufficiently scalable to produce CAR-T cell products for clinical use.
PB-mediated gene transfer requires electroporation, which may cause cell death. Therefore, the maintenance of an appropriate cell density is required for the generation of PB-modified T cells.5 Several approaches can be used to provide feeder cells to PB-modified T cells that include engineered tumor cell lines such as K562 expressing co-stimulatory molecules or total unfractionated PBMCs.5 However, including tumor cell lines in culture might lead to a more complicated approval process for clinical trials to fulfill the regulations in our country. Furthermore, obtaining sufficient number of PBMCs is relatively challenging as compared to the activated ATCs, which can easily be expanded, while PBMCs are a solid option for feeder cells or simulant for T cells. Thus, in addition to that and ATCs reportedly expressing adequate levels of HLA class I, II, and co-stimulatory molecules,16 we selected ATCs as a feeder cell and simulator for CAR-T cells in this study.
The final output of T cells activated and expanded ex vivo is the result of a balance between T cell expansion and T cell death. In the present study, we found that, upon CAR piggyBac gene transfer, T cell stimulation obtained via TCR engagement with viral peptides had less induced activation and cell death, which ultimately led to a significant increase in CAR-T cell counts rather than cross-linking with mAbs. Anti-CD3/CD28 mAb stimulation has been successfully used to generate and expand CAR-T cells for clinical use14, 15, 17, 18 using either retroviral or lentiviral vectors to insert the CAR into T cells. A critical step in the procedure of non-viral gene transfer is represented by the electroporation of T cells. Although we do not have a mechanistic explanation, our data suggest that the methodology used to engage the TCR may affect the outcome of electroporated T cells causing more death when antibodies are cross-linking TCR molecules. By contrast, TCR engagement with peptide presented in the context of the major histocompatibility complex (MHC) by ATCs may preserve the physiology of electroporated cells.
Unexpectedly, ACE CAR-T cells did not secrete IFN-γ against viral peptides, although they were simulated by viral antigens during the culture. Recently, Ghosh et al.19 elucidated the mechanism whereby allogeneic CD19-targeted CAR-T cells provided anti-lymphoma activity without causing an increased incidence of graft-versus-host-disease in the past clinical trials. In their study, alloreactive T cells expressing CD19.CAR with CD28 co-stimulatory domains experienced enhanced stimulation, leading to the progressive loss of their alloreactive effector function. In our study, although ACE CAR-T cells seemed to maintain the virus specificity by day 7, they lost it by day 14. In addition, the virus-specific population seemed to be limited in the CAR− population and ACE NT-T cells maintained the virus specificity on day 14. Together with the naive or stem-cell memory-like phenotype in ACE CAR-T cells, one possible explanation for this is that virus-specific TCR stimulation might have enhanced the expansion of CAR and virus-specific TCR dual-positive T cells and simultaneously downregulated their virus-specific TCR after the second stimulation of ACE peptides. Further studies are warranted to investigate the precise mechanism.
Cytokines’ use to expand CAR-T cells seems also important in determining not only the expansion rate of these cells but also their immunologic composition. By using the combination of IL-7 and IL-15, 94% of the ex vivo expanded ACE CAR-T cells expressed CD3 and contained both CD4+ and CD8+ T cells, with a slightly higher percentage of CD8+. Moreover, most CAR+ T cells exhibited a CD45RA+CCR7+ or a CD45RA+CD62L+ phenotype in our final product, suggesting that most ACE CAR+ T cells exhibit a naive (Tn) or stem-cell memory (Tscm) T cell phenotype20, 21 that are considered favorable phenotypic characteristics to ensure persistence and antitumor effects upon infusion into patients, as demonstrated by the potent anti-leukemia effects of ACE CAR-T cells in our experiments in vitro and in vivo. Recently Barnett et al.22 compared the phenotype of CAR-T cells transduced by either lentivirus or PB transposon and revealed that the majority of PB-modified CAR-T cells showed CD45RA+CD62L+, similar to our results. In contrast, lentivirus-transduced CAR-T cells did not show an augmented memory phenotype. Although the precise mechanism is still unclear, PB gene transfer system may induce expansion of CAR-T cells with Tn/Tscm phenotype.
Although our novel method significantly improved the efficiency of CAR-T cell generation, the efficiency was still low as compared to another report of CAR-T cells generated by the non-viral gene transfer system such as Sleeping beauty23, 24 and piggyBac25 transposon. Perhaps this could be attributed to the electroporation condition of piggyBac-modified CAR-T cells. Recently, Ramanayake et al.25 rigorously optimized their electroporation condition and determined that the optimal voltage setting (2400 V) provided a 1.71-fold increase of their CAR-T generation efficiency. Although our electroporation method (4D-Nucleofector device) has a limited option of electroporation conditions as compared to those (Neon Transfection System) presented,25 the efficiency of CAR-T generation could be potentially improved by further optimization of the electroporation condition in piggyBac-modified CAR-T cells.
Another reason could be the differences in the culture strategy between others and ours regarding the numbers of stimulation and the presence of stimulation through the CAR. We stimulated T cells only two times to reduce the culture period and avoid T cell differentiation and exhaustion. Moreover, we used autologous ATCs for the stimulation of CAR-T cells, which may minimally stimulate T cells through the CAR because ATCs included minimal CD19+ cells as compared to PBMCs. In contrast, Ramanayake et al.25 stimulated their piggyBac-modified CAR-T cells three times with PBMCs. In their method, CD19.CAR-T cells could be stimulated through the CAR owing to the CD19+ population in PBMCs, and they achieved 765-fold expansion and 72% of the CAR expression in their CD19.CAR-T cells. Similarly, Kebriaei et al.23 generated Sleeping beauty-modified CAR-T cells by stimulating with CD19 and co-stimulatory molecules expressing K562 cells. Although most of their CAR+ T cells exhibited a differentiated effector memory phenotype and an increased expression of LAG3, PDCD1LG2, and E2F mRNA15 related to exhaustion, they achieved high CAR expression (84%) and fold expansion (2,200–2,500) for 4 weeks of culture and presented promising results from their clinical trials.23, 24 Even though the culture strategies and efficiencies of CAR-T cell generation were different, these findings supported that a non-viral gene transfer system could be an alternative option for generating CAR-T cells for clinical use.
In conclusion, we developed a novel method of generating PB-modified CD19.CAR-T cells using minimal manipulation and reagents that are good manufacture compliant for clinical application. Together with the simple manufacturing process and cost-effectiveness of DNA transposon technology, piggyBac-based gene transfer provides an alternative to retroviral or lentiviral gene transfer for CAR-T cell therapy. Based on these encouraging data, we currently planning to conduct a clinical trial of PB-modified CD19.CAR-T cells using our ACE CAR-T method.
Materials and Methods
Plasmids
The piggyBac transposase plasmid (pCMV-piggyBac) and transposon plasmid for CD19.CAR (pIRII-CAR.CD19-28-ζ, 6,438 bp) have been described previously.5, 6, 7, 8 In brief, pIRII-CAR.CD19-28-ζ encodes a single-chain variable fragment from the CD19 antibody (FMC63) linked to the hinge CH2CH3 domain of human IgG1, the endodomains of a CD28 molecule, and a TCR ζ chain. Both vectors are transcriptionally regulated by the cytomegalovirus (CMV) immediate early gene enhancer/promoter sequence. To provide better in vivo persistence and antitumor activity, we constructed a new transposon vector (short) that does not have the IgG1-CH2CH3 spacer region based on the construct reported by Kochenderfer et al.13 (GenBank: HM852952.1).
Cell Lines
SU/SR were derived from SU-Ph2 by culture with imatinib as described previously12 and maintained in RPMI 1640 medium, supplemented with GlutaMAX and 10% fetal bovine serum (Hyclone, Laboratories, Logan, USA). No cytokines were fed to the co-culture.
Gene Transfer into T Cells and Expansion of Transgenic T Cells
PBMCs were freshly isolated from peripheral blood of healthy donors and then immediately transfected after the isolation. Healthy volunteers gave written informed consent according to protocols approved by the institutional review board of Shinshu University School of Medicine, and all experiments involving human participants were performed in accordance with the guidelines established by the Declaration of Helsinki. A 4D-Nucleofector device (Program EO-115) and P3 Primary Cell 4D-Nucleofector X Kit (Lonza, Basel, Switzerland) were used to electroporate 1 × 107 PBMCs with a pIRII-CD19.CD28.ζ−CAR transposon plasmid with or without the IgG1-CH2CH3 spacer (5 μg) and a pCMV-piggyBac transposase plasmid (5 μg) according to the manufacturer’s instructions. All cells were cultured in animal-derived component-free T cell culture medium (TexMACS Medium; Miltenyi Biotec, Auburn, CA, USA) containing IL-7 (10 ng/mL, Miltenyi Biotec) and IL-15 (5 ng/mL, Miltenyi Biotec) in 24-well plates at 37°C in a humidified 5% CO2 incubator.
In the original method (Figure 1A), the electroporated cells were transferred to CD3/CD28 mAb (Miltenyi Biotec)-coated plates the day following electroporation without feeder ATCs (original).
We compared two other different culture conditions. In CD3/CD28-ATC condition, electroporated cells were co-cultured with feeder ATCs on day 0 and then transferred to CD3/CD28 mAb-coated plates on day 1. In ACE condition, electroporated cells were stimulated with feeder ATCs pulsed with four viral peptide pools (MACS GMP PepTivator; AdV5 Hexon, CMV pp65, EBV EBNA-1, and BZLF1) on day 0.
On day 7, 2 × 106 cells were transferred into G-Rex10 culture flasks (Wilson Wolf Manufacturing, New Brighton, MN, USA) with 30 mL of IL-7 (10 ng/mL)/IL-15 (5 ng/mL)-containing TexMACS with 2 × 106 of ACE-pulsed irradiated ATCs for the ACE CAR-T and with 2 × 106 of unpulsed irradiated ATCs for CD3/CD28-ATC condition, or without stimulation for original condition. On day 14, CAR-T cells cultured under all conditions were collected and analyzed.
Preparing Feeder ATCs
For preparing feeder ATCs, PBMCs were stimulated on CD3/CD28mAb-coated plates for 3 days then transferred to regular plates and maintained for 6–8 days supplemented with IL-7 (10 ng/mL)/IL-15 (5 ng/mL). The cells were then harvested and cryopreserved on days 9–11 after initial stimulation. ATCs were thawed 2–3 days before use and re-stimulated on CD3/CD28mAbs-coated plates for 2–3 days then irradiated at 30 Gy just before being added to the culture, as previously reported.16
Flow Cytometry
With the use of the BD FACSCalibur with BD Cell-Quest Pro software (BD Biosciences, Franklin Lakes, NJ, USA), the surface markers of the expanded CAR-T cells were analyzed using allophycocyanin (APC)-conjugated CD3 mAbs, phycoerythrin (PE)-conjugated CD4 mAbs, APC-conjugated CD8 mAbs, APC-conjugated CD45RA mAbs, PE-conjugated CD56 mAbs, PE-conjugated CD62L mAbs, and PE-conjugated CCR7 mAbs (all mAbs were purchased from Miltenyi Biotec). T cell expression of CAR was examined using a specific anti-idiotype single-chain variable fragment (scFV) mAbs, which was kindly provided by Dr. Lawrence Cooper (MD Anderson Cancer Center).26 The data were analyzed using FlowJo software (TreeStar; http://www.flowjo.com/).
ELISpot Assay
We performed the ELISpot assay to examine viral antigen-specific IFN-γ production by either ACE CAR-T or ACE NT-T cells using the human IFN-γ ELISpot PLUS kit (Mabtech, Nacka Strand, Sweden) according to the manufacturer’s instructions. In brief, we cultured ACE CAR-T or NT-T cells (5 × 104 cells/well) in the presence of pp65, hexon, EBNA1, BZLF1, or medium alone (control). After 20 hr of incubation, the spots were counted by an automated ELISpot reader (Autoimmun Diagnostika, Strassberg, Germany).
Intracellular Cytokine Assay
We performed intracellular cytokine staining to determine whether the CAR+ population could respond to viral antigens. In brief, ACE CAR-T cells were stimulated with pp65, hexon, EBNA1, BZLF1, or medium alone (control). After 4 hr of incubation, cells were harvested and stained with the anti-idiotype scFV mAbs described earlier. Then, the cells were fixed and permeabilized according to the manufacturer’s instruction. Finally, the cells were stained with IFN-γ and analyzed by flow cytometry.
Annexin V Apoptosis Assay
Electroporated cells were stimulated with either viral peptides (ACE) or CD3/CD28 mAbs (CD3/CD28-ATC) in the presence of autologous ATCs. Seven days after stimulation, the cells were harvested, stained with Annexin V (IMMUNOCYTO Cytotoxicity Detection Kit; MBL International Corporation, Woburn, MA, USA), APC-conjugated CD3, and Alexa Fluor 488-conjugated specific anti-idiotype scFV mAbs, and analyzed via flow cytometry.
Co-culture Experiments
To examine the anti-leukemic activity of CAR-T cells, ACE CD19.CAR-T cells, CD3/CD28-ATC CD19.CAR-T cells, and the original CD19.CAR-T cells were added to 5 × 105 CD19+ leukemic cells (SU/SR) at E:T ratios of 1:5, 1:50, and 1:100 into the wells of a 48-well culture plate containing RPMI 1640 medium plus 10% fetal bovine serum without cytokines and cultured for 5 days. At the indicated points, the number of viable cells was determined using a trypan blue exclusion test, and the percentage of T cells and CD19+ cells were determined by flow cytometry using APC-conjugated CD3 mAbs and PE-conjugated CD19 mAbs. IFN-γ levels in culture media were measured by ELISA assay (R&D Systems, Minneapolis, MN)
In Vivo Experiments
NSG mice were originally generated by Jackson Laboratory (Bar Harbor, ME, USA) and purchased from Charles River Laboratories Japan (Yokohama, Japan). All mouse experiments were performed in accordance with the Animal Husbandry and Institutional Animal Care and Use Committee guidelines of the Nagoya University Graduate School of Medicine.
NSG mice received intravenous injections of 1 × 106 luciferase-transduced Daudi cells. Three days later, they were intravenously infused with 1 × 107 CD19.CAR-T cells. The cell counts of the infused cells were based on the total cell number. Untreated animals served as controls.
Biodistribution of Daudi cells was assessed twice weekly using the In Vivo Imaging System (Xenogen Corporation, Alameda, CA, USA) as described previously.27, 28 Mice were euthanized at predefined endpoints or when euthanasia criteria were met in accordance with the Center for Comparative Medicine at the Nagoya University Graduate School of Medicine.
Statistical Analysis
The results from three culture experiments were expressed as the means ± SD. An unpaired t test was used to identify any significant differences among the three independent groups. Statistical significance was defined as p < 0.05.
Author Contributions
Conceptualization, Y.N.; Methodology, D.M., N.N., M.T., Y.N.; Investigation, D.M., N.N., M.T., N.K., Y.O., Y.N.; Resources, M.H.W., G.D., C.M.R.; Writing – Original Draft, D.M., S.S.; Writing – Review & Editing, S.S., N.N., M.H.W., G.D., C.M.R., Y.T., Y.N.; Funding Acquisition, Y.T., Y.N.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
The authors thank Ms. Yūka Miyajima for preparing the manuscript and for secretarial assistance. This research is supported by grants from the Ministry of Health, Labor and Welfare (201438063A), Japan Agency for Medical Research and Development (AMED) (15ck0106067h0002, 16ck0106067h0003, 16lm0103009j0005, and 17ck0106291h0001), Nagoya University Hospital Funding for Clinical Research (716910), and Nagoya University Hospital Funding for Clinical Development (71004212).
Footnotes
Supplemental Information includes ten figures and can be found with this article online at https://doi.org/10.1016/j.omtm.2017.12.003.
Supplemental Information
References
- 1.Davila M.L., Riviere I., Wang X., Bartido S., Park J., Curran K., Chung S.S., Stefanski J., Borquez-Ojeda O., Olszewska M. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci. Transl. Med. 2014;6:224ra25. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maude S.L., Frey N., Shaw P.A., Aplenc R., Barrett D.M., Bunin N.J., Chew A., Gonzalez V.E., Zheng Z., Lacey S.F. Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med. 2014;371:1507–1517. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee D.W., Kochenderfer J.N., Stetler-Stevenson M., Cui Y.K., Delbrook C., Feldman S.A., Fry T.J., Orentas R., Sabatino M., Shah N.N. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385:517–528. doi: 10.1016/S0140-6736(14)61403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turtle C.J., Hanafi L.A., Berger C., Gooley T.A., Cherian S., Hudecek M., Sommermeyer D., Melville K., Pender B., Budiarto T.M. CD19 CAR-T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J. Clin. Invest. 2016;126:2123–2138. doi: 10.1172/JCI85309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakazawa Y., Huye L.E., Dotti G., Foster A.E., Vera J.F., Manuri P.R., June C.H., Rooney C.M., Wilson M.H. Optimization of the PiggyBac transposon system for the sustained genetic modification of human T lymphocytes. J. Immunother. 2009;32:826–836. doi: 10.1097/CJI.0b013e3181ad762b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakazawa Y., Huye L.E., Salsman V.S., Leen A.M., Ahmed N., Rollins L., Dotti G., Gottschalk S.M., Wilson M.H., Rooney C.M. PiggyBac-mediated cancer immunotherapy using EBV-specific cytotoxic T-cells expressing HER2-specific chimeric antigen receptor. Mol. Ther. 2011;19:2133–2143. doi: 10.1038/mt.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakazawa Y., Saha S., Galvan D.L., Huye L., Rollins L., Rooney C.M., Wilson M.H. Evaluation of long-term transgene expression in piggyBac-modified human T lymphocytes. J. Immunother. 2013;36:3–10. doi: 10.1097/CJI.0b013e3182791234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saito S., Nakazawa Y., Sueki A., Matsuda K., Tanaka M., Yanagisawa R., Maeda Y., Sato Y., Okabe S., Inukai T. Anti-leukemic potency of piggyBac-mediated CD19-specific T cells against refractory Philadelphia chromosome-positive acute lymphoblastic leukemia. Cytotherapy. 2014;16:1257–1269. doi: 10.1016/j.jcyt.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudecek M., Lupo-Stanghellini M.T., Kosasih P.L., Sommermeyer D., Jensen M.C., Rader C., Riddell S.R. Receptor affinity and extracellular domain modifications affect tumor recognition by ROR1-specific chimeric antigen receptor T cells. Clin. Cancer Res. 2013;19:3153–3164. doi: 10.1158/1078-0432.CCR-13-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watanabe N., Bajgain P., Sukumaran S., Ansari S., Heslop H.E., Rooney C.M., Brenner M.K., Leen A.M., Vera J.F. Fine-tuning the CAR spacer improves T-cell potency. OncoImmunology. 2016;5:e1253656. doi: 10.1080/2162402X.2016.1253656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almåsbak H., Walseng E., Kristian A., Myhre M.R., Suso E.M., Munthe L.A., Andersen J.T., Wang M.Y., Kvalheim G., Gaudernack G., Kyte J.A. Inclusion of an IgG1-Fc spacer abrogates efficacy of CD19 CAR T cells in a xenograft mouse model. Gene Ther. 2015;22:391–403. doi: 10.1038/gt.2015.4. [DOI] [PubMed] [Google Scholar]
- 12.Hirase C., Maeda Y., Takai S., Kanamaru A. Hypersensitivity of Ph-positive lymphoid cell lines to rapamycin: possible clinical application of mTOR inhibitor. Leuk. Res. 2009;33:450–459. doi: 10.1016/j.leukres.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Kochenderfer J.N., Feldman S.A., Zhao Y., Xu H., Black M.A., Morgan R.A., Wilson W.H., Rosenberg S.A. Construction and preclinical evaluation of an anti-CD19 chimeric antigen receptor. J. Immunother. 2009;32:689–702. doi: 10.1097/CJI.0b013e3181ac6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X., Rivière I. Clinical manufacturing of CAR T cells: foundation of a promising therapy. Mol. Ther. Oncolytics. 2016;3:16015. doi: 10.1038/mto.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kochenderfer J.N., Dudley M.E., Kassim S.H., Somerville R.P., Carpenter R.O., Stetler-Stevenson M., Yang J.C., Phan G.Q., Hughes M.S., Sherry R.M. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J. Clin. Oncol. 2015;33:540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngo M.C., Ando J., Leen A.M., Ennamuri S., Lapteva N., Vera J.F., Min-Venditti A., Mims M.P., Heslop H.E., Bollard C.M. Complementation of antigen-presenting cells to generate T lymphocytes with broad target specificity. J. Immunother. 2014;37:193–203. doi: 10.1097/CJI.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed N., Brawley V.S., Hegde M., Robertson C., Ghazi A., Gerken C., Liu E., Dakhova O., Ashoori A., Corder A. Human epidermal growth factor receptor 2 (HER2)-specific chimeric antigen receptor-modified T cells for the immunotherapy of HER2-positive sarcoma. J. Clin. Oncol. 2015;33:1688–1696. doi: 10.1200/JCO.2014.58.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brentjens R.J., Davila M.L., Riviere I., Park J., Wang X., Cowell L.G., Bartido S., Stefanski J., Taylor C., Olszewska M. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci. Transl. Med. 2013;5:177ra38. doi: 10.1126/scitranslmed.3005930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghosh A., Smith M., James S.E., Davila M.L., Velardi E., Argyropoulos K.V., Gunset G., Perna F., Kreines F.M., Levy E.R. Donor CD19 CAR T cells exert potent graft-versus-lymphoma activity with diminished graft-versus-host activity. Nat. Med. 2017;23:242–249. doi: 10.1038/nm.4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu Y., Zhang M., Ramos C.A., Durett A., Liu E., Dakhova O., Liu H., Creighton C.J., Gee A.P., Heslop H.E. Closely related T-memory stem cells correlate with in vivo expansion of CAR.CD19-T cells and are preserved by IL-7 and IL-15. Blood. 2014;123:3750–3759. doi: 10.1182/blood-2014-01-552174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sommermeyer D., Hudecek M., Kosasih P.L., Gogishvili T., Maloney D.G., Turtle C.J., Riddell S.R. Chimeric antigen receptor-modified T cells derived from defined CD8+ and CD4+ subsets confer superior antitumor reactivity in vivo. Leukemia. 2016;30:492–500. doi: 10.1038/leu.2015.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnett B.E., Hermanson D.L., Smith J.B., Wang X., Tan Y., Martin C.E. piggyBac™-produced CAR-T cells exhibit stem-cell memory phenotype. Blood. 2016;128:2167. [Google Scholar]
- 23.Kebriaei P., Singh H., Huls M.H., Figliola M.J., Bassett R., Olivares S., Jena B., Dawson M.J., Kumaresan P.R., Su S. Phase I trials using Sleeping Beauty to generate CD19-specific CAR T cells. J. Clin. Invest. 2016;126:3363–3376. doi: 10.1172/JCI86721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maiti S.N., Huls H., Singh H., Dawson M., Figliola M., Olivares S., Rao P., Zhao Y.J., Multani A., Yang G. Sleeping beauty system to redirect T-cell specificity for human applications. J. Immunother. 2013;36:112–123. doi: 10.1097/CJI.0b013e3182811ce9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramanayake S., Bilmon I., Bishop D., Dubosq M.C., Blyth E., Clancy L., Gottlieb D., Micklethwaite K. Low-cost generation of Good Manufacturing Practice-grade CD19-specific chimeric antigen receptor-expressing T cells using piggyBac gene transfer and patient-derived materials. Cytotherapy. 2015;17:1251–1267. doi: 10.1016/j.jcyt.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 26.Jena B., Maiti S., Huls H., Singh H., Lee D.A., Champlin R.E., Cooper L.J. Chimeric antigen receptor (CAR)-specific monoclonal antibody to detect CD19-specific T cells in clinical trials. PLoS ONE. 2013;8:e57838. doi: 10.1371/journal.pone.0057838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vera J., Savoldo B., Vigouroux S., Biagi E., Pule M., Rossig C., Wu J., Heslop H.E., Rooney C.M., Brenner M.K., Dotti G. T lymphocytes redirected against the kappa light chain of human immunoglobulin efficiently kill mature B lymphocyte-derived malignant cells. Blood. 2006;108:3890–3897. doi: 10.1182/blood-2006-04-017061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishio N., Diaconu I., Liu H., Cerullo V., Caruana I., Hoyos V., Bouchier-Hayes L., Savoldo B., Dotti G. Armed oncolytic virus enhances immune functions of chimeric antigen receptor-modified T cells in solid tumors. Cancer Res. 2014;74:5195–5205. doi: 10.1158/0008-5472.CAN-14-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.