Abstract
Purpose
Obesity has been inconsistently linked to increased cervical cancer incidence and mortality; however, the effect of obesity on cervical screening has not been explored. We investigated the hypothesis that increased body mass might decrease detection of cervical precancer and increase risk of cervical cancer even in women undergoing state-of-the-art screening.
Methods
We conducted a retrospective cohort study of 944,227 women age 30 to 64 years who underwent cytology and human papillomavirus DNA testing (ie, cotesting) at Kaiser Permanente Northern California (January 2003 to December 2015). Body mass index was categorized as normal/underweight (< 25 kg/m2), overweight (25 to < 30 kg/m2), or obese (≥ 30 kg/m2). We estimated 5-year cumulative risks of cervical precancer and cancer by category of body mass index using logistic Weibull survival models.
Results
We observed lower risk of cervical precancer (n = 4,489) and higher risk of cervical cancer (n = 490) with increasing body mass index. Specifically, obese women had the lowest 5-year risk of precancer (0.51%; 95% CI, 0.48% to 0.54% v 0.73%; 95% CI, 0.70% to 0.76% in normal/underweight women; P trend < .001). In contrast, obese women had the highest 5-year risk of cancer (0.083%; 95% CI, 0.072% to 0.096% v 0.056%; 95% CI, 0.048% to 0.066% in normal/underweight women; P trend < .001). Results were consistent in subgroups defined by age (30 to 49 v 50 to 64 years), human papillomavirus status (positive v negative), and histologic subtype (glandular v squamous). Approximately 20% of cervical cancers could be attributed to overweight or obesity in the women in our study who underwent routine cervical screening.
Conclusion
In this large, screened population, overweight and obese women had an increased risk of cervical cancer, likely because of underdiagnosis of cervical precancer. Improvements in equipment and/or technique to assure adequate sampling and visualization of women with elevated body mass might reduce cervical cancer incidence.
INTRODUCTION
The obesity epidemic is a significant, worldwide public health challenge, with important implications for global cancer rates.1 This problem is particularly acute in the United States, where obesity rates have tripled over the past three decades.2 Although some studies have reported an association of obesity with increased cervical cancer incidence and mortality, findings have been inconsistent, and the mechanism is unknown.3-10 Importantly, previous studies have lacked cervical precancer end points and failed to account for an effect of obesity on cervical cancer screening, which is less frequent among obese women.11 Even among women who do undergo routine screening, cervical cancers uncommonly occur12; whether obesity is associated with decreased efficacy of screening as a mechanism of increased cervical cancer risk is unknown.
Difficulties in screening and imaging obese patients have been reported for a number of different clinical modalities.13,14 It is plausible that obesity may similarly be a risk factor for cervical cancer because of decreased efficacy of cervical visualization and sampling during routine screening15,16; however, to our knowledge, the effect of excess body weight on the sensitivity of cervical cancer screening has not previously been reported. Thus, we conducted a large-scale, retrospective cohort study to investigate the hypothesis that increased body mass might decrease detection of cervical precancer and increase the risk of cervical cancer in women undergoing routine screening.
METHODS
Patients
This study was conducted at Kaiser Permanente Northern California (KPNC), a large, integrated health care system that implemented an intensive program with triennial cervical cytology and human papillomavirus (HPV) cotesting in 2003 among women age ≥ 30 years. We conducted a retrospective cohort study within KPNC of 1,659,496 women who had undergone screening by conventional cytology and/or SurePath (BD Diagnostics, Burlington, NC) liquid-based cytology combined with Hybrid Capture 2 (Qiagen, Hilden, Germany) HPV testing since January 2003, as previously described.17 For each woman, the baseline screen was defined as the first available screening test in the study period. Histopathology outcomes were abstracted from electronic medical records through December 2015. For the main analysis, women were excluded if they were outside the recommended age range for cotesting (30 to 64 years) at baseline (n = 503,109; 30.3%), were missing body mass index (BMI) data (n = 211,736; 12.8%), or had a BMI measure outside the range of 10 to 80 kg/m2 (n = 415; 0.03%). Cancer cases with uncertainty as to whether the tissue origin was endocervical or endometrial (n = 9) were also excluded, resulting in a total of 944,227 women included in the analysis. As an ancillary validation step, we also tested our hypothesis in women age 25 to 29 years with atypical squamous cells of undetermined significance (ASC-US) cytology (n = 32,668) who underwent cotesting. This study was approved by the KPNC institutional review board and was exempted from institutional review at the National Cancer Institute by the Office of Human Subjects Research Protections.
Cervical Cancer Screening and Management at KPNC
Conventional Papanicolaou (Pap) testing was performed until 2009, when KPNC switched to liquid-based cytology, which has similar clinical performance as conventional cytology.18 Cytology was categorized according to the 2001 Bethesda System.19 Presence or absence of endocervical cells was generally noted in the cytology report. HPV testing was performed at a single KPNC regional laboratory per manufacturer instructions.
KPNC management guidelines generally mirror consensus guidelines of the American Society for Colposcopy and Cervical Pathology.20 Women who cotest as HPV positive with ASC-US or more severe cytologic abnormalities (ASC-US+; ie, Pap positive) are referred to colposcopy, whereas women who are HPV-positive with normal cytology undergo repeat cotesting after 12 months and are referred to colposcopy if either test is positive. Histologic evaluations of colposcopy-directed biopsies at KPNC are based on the cervical intraepithelial neoplasia (CIN) classification, and women diagnosed with cervical CIN grade ≥ 2 (≥ CIN2) are considered to have precancer and undergo treatment or intensive follow-up per national guidelines.
BMI and Other Covariates
Clinical measures of height (in meters) and weight (in kilograms), documented in electronic medical records consistently beginning in 2007, were used to calculate median BMI from values recorded within the preceding 5 years. We categorized BMI as underweight (< 18.5 kg/m2), normal (18.5 to < 25 kg/m2), overweight (25 to < 30 kg/m2), or obese (30 to 80 kg/m2) in accordance with standard cutpoints.21 Because few women were underweight (1.2%), we combined underweight with normal BMI (normal/underweight) and performed a sensitivity analysis excluding the underweight group. Information on race/ethnicity, baseline age, age at diagnosis, and cancer stage was abstracted electronically. To assess the validity of using 5-year median BMI at enrollment, we evaluated the effect of potential misclassification using the full range of longitudinal BMI values in a random subset of approximately 15,000 women with available data (Appendix Table A1, online only).
Statistical Analysis
We evaluated two primary clinical end points—cervical precancer (including CIN grade 3 [CIN3] and adenocarcinoma in situ [AIS]) and cervical cancer (including squamous cell carcinoma [SCC], adenocarcinoma [ADC]/adenosquamous carcinoma, and microinvasive cancer). We focused on risk of CIN3/AIS rather than CIN2 because CIN2 may not accurately reflect true cervical precancer and is unreliably diagnosed by pathologists.22-24 However, because CIN2 remains the typical consensus treatment threshold in most places,20 we evaluated the risk of this end point in a sensitivity analysis. We estimated the 5-year cumulative risks (CRs) and 95% CIs of disease end points using the logistic Weibull model,25 which accounts for prevalent disease at baseline (odds ratio [OR]) and incident (interval-censored) disease detected during screening (hazard ratio [HR]), and for the possibility that some disease found in follow-up may have been undiagnosed prevalent disease.25 Models are presented as unadjusted; however, we explored the potential for confounding by continuous baseline age and race/ethnicity in adjusted analyses. We also stratified analyses by age group (30 to 49 v 50 to 64 years, as a proxy for menopausal status), HPV status (positive v negative), and histology (squamous v glandular).
We calculated the population attributable fraction (PAF) to estimate the proportion of patients with CIN3/AIS and cervical cancer attributed to overweight and obesity. To derive these estimates, we calculated the CRs of CIN3/AIS and cancer, respectively, for the 944,227 women in our study. From this, we subtracted the CR in the normal/underweight group and expressed this quantity as a percentage of the CR in our study population (CRStudyPopulation − CRNormal/Underweight/CRStudyPopulation × 100).
In ancillary analyses, we examined differences in age at precancer and cancer diagnosis and in cancer stage by BMI. Additionally, we evaluated associations of BMI with different components of the cervical cancer screening process, including baseline cotest results by worst histologic diagnosis, potential for mediation by sampling inadequacy using presence of endocervical component as a crude measure, and distribution of colposcopy outcomes by the preceding abnormal screening result. For these ancillary analyses, we combined CIN2 and CIN3 (CIN2/3) because women diagnosed with ≥ CIN2 usually undergo treatment at KPNC. Analyses were conducted using R software (version 3.3.1), and logistic Weibull models were estimated using the PIMixture package (R Foundation).25 All significance tests were two sided.
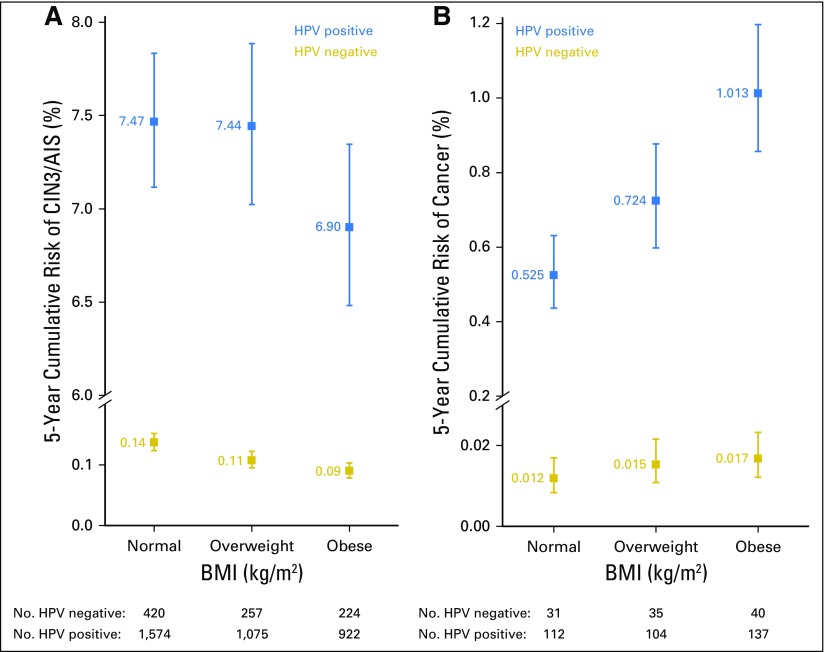
RESULTS
Table 1 lists the baseline characteristics of the 944,227 women in this study. Most women were age 30 to 49 years, and approximately one third were obese. A majority were white; however, overweight and obese women were more likely to be black or Hispanic and less likely to be Asian compared with normal/underweight women. On average, women had 4.4 years of follow-up and 2.9 screening tests; we did not observe meaningful differences by BMI. Approximately 6.3% of women were HPV positive, with a trend toward decreasing HPV prevalence with increasing BMI (P trend < .001), irrespective of age (data not shown).
Table 1.
Demographic and Clinical Characteristics of Women in KPNC Study, Overall and by BMI (N = 944,227)
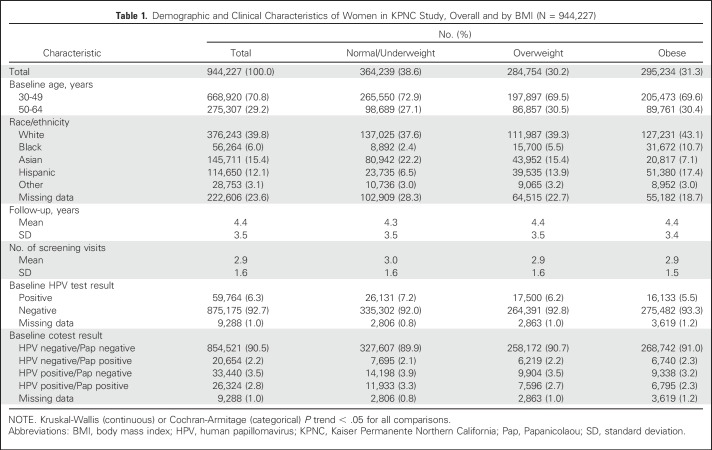
Risk of CIN3/AIS and Cancer by BMI
A total of 4,489 women (0.48%) developed CIN3/AIS. Of these, 1,998 patients were classified as normal/underweight (44.4%), 1,339 as overweight (29.8%), and 1,152 as obese (25.6%). A total of 490 women (0.05%) were diagnosed with cancer. Of these patients with cancer, 149 were classified as normal/underweight (30.4%), 154 as overweight (31.4%), and 187 as obese (38.2%).
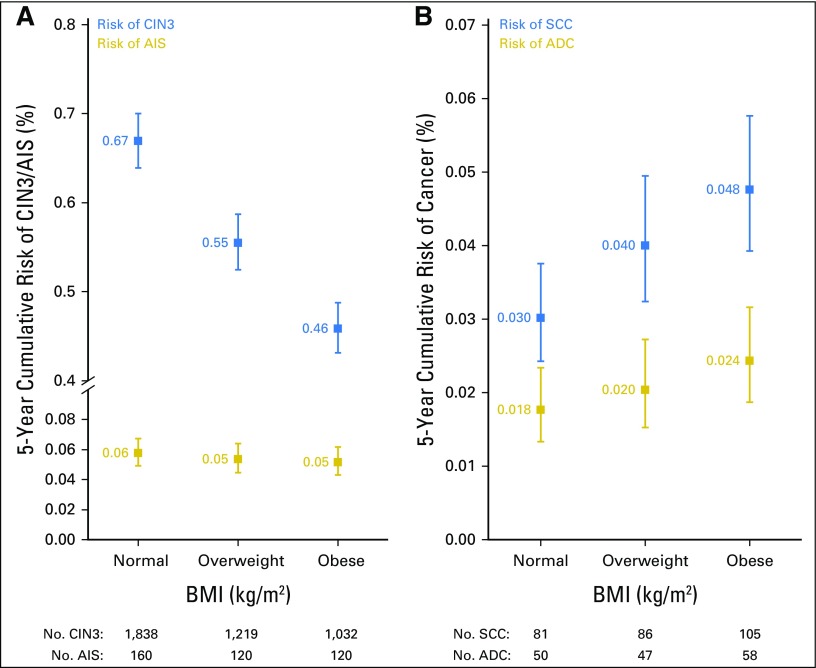
The risk of CIN3/AIS was lower with increasing BMI (P trend < .001). This association was consistent for both prevalent (overweight: OR, 0.86; 95% CI, 0.78 to 0.94 and obese: OR, 0.72; 95% CI, 0.66 to 0.79) and incident CIN3/AIS (overweight: HR, 0.80; 95% CI, 0.70 to 0.90 and obese: HR, 0.66; 95% CI, 0.58 to 0.76). Obese women had the lowest 5-year CR of CIN3/AIS (0.51%; 95% CI, 0.48% to 0.54%), followed by overweight women (0.61%; 95% CI, 0.58% to 0.64%), whereas normal/underweight women had the highest 5-year CR of CIN3/AIS (0.73%; 95% CI, 0.70% to 0.76%; Fig 1). We observed similar trends when adjusting for age and race/ethnicity and excluding underweight women. Findings were also consistent for risk of CIN2 (data not shown). In a subset of approximately 15,000 women, we observed similar trends of lower CIN3/AIS risk with increasing BMI among women who changed BMI category at least once during the study period (54.5%) and among women who remained in the same BMI category over time (45.5%). Stronger associations were observed among women with stable BMI category (Appendix Table A1, online only).
Fig 1.
Five-year cumulative risk of (A) cervical intraepithelial neoplasia grade 3 and adenocarcinoma in situ (CIN3/AIS) and (B) cancer by body mass index (BMI). Five-year cumulative risks were estimated using logistic Weibull models. Note that the y-axes have different scales for the left and right panels.
In contrast to CIN3/AIS, the 5-year CR of cancer was higher with increasing BMI (P trend < .001). This association was consistent for both prevalent (overweight: OR, 1.22; 95% CI, 0.94 to 1.57 and obese: OR, 1.48; 95% CI, 1.16 to 1.89) and incident cancer (overweight: HR, 1.64; 95% CI, 0.96 to 2.78 and obese: HR, 1.77; 95% CI, 1.06 to 2.96). Obese women had the highest 5-year CR of cancer (0.083%; 95% CI, 0.072% to 0.096%), followed by overweight (0.071%; 95% CI, 0.060% to 0.082%) and normal/underweight women (0.056%; 95% CI, 0.046% to 0.064%; Fig 1). We observed similar trends when adjusting for age and race/ethnicity and excluding underweight women (data not shown).
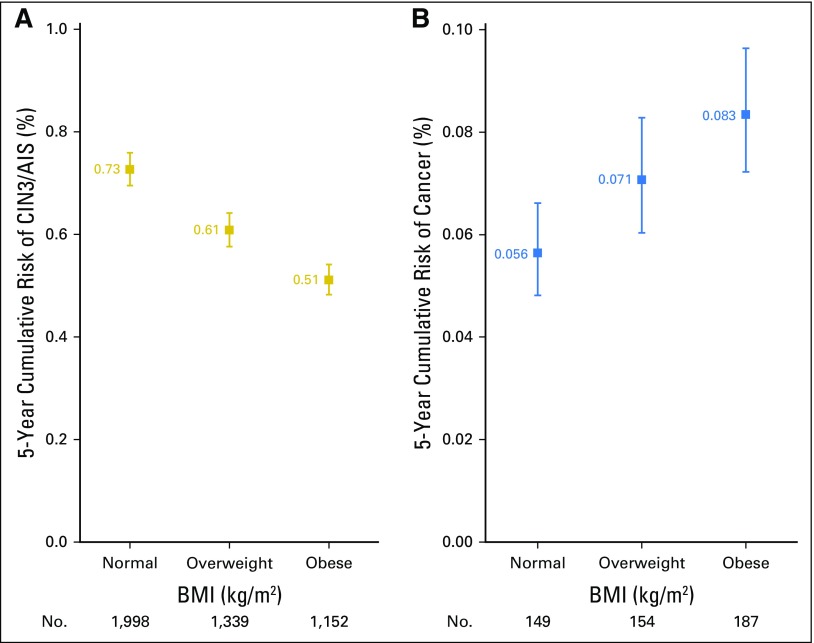
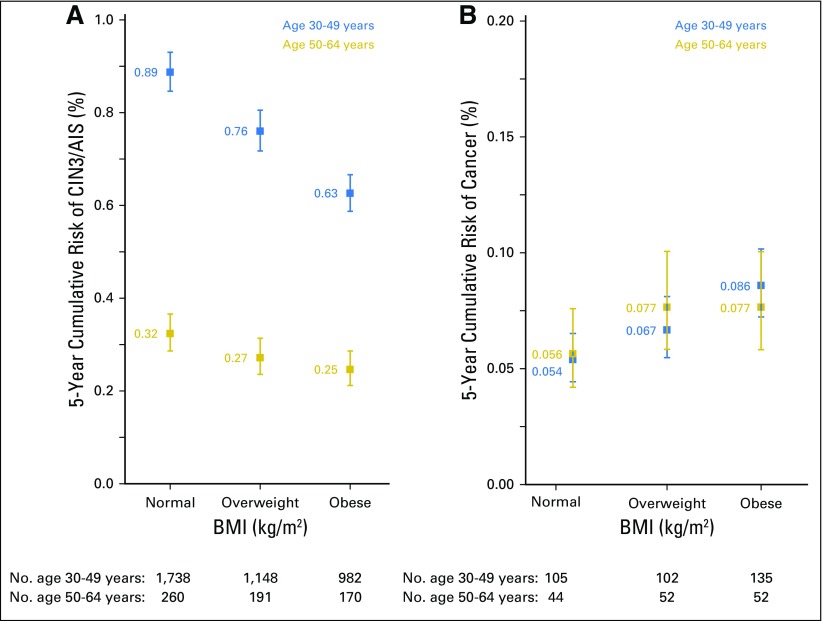
In stratified analyses, results were consistent in subgroups defined by age group (Fig 2), HPV status (Fig 3), and histology, with stronger associations observed for squamous compared with glandular disease, respectively (Fig 4). As a validation step, we evaluated the association of BMI with risk of CIN3/AIS (n = 894) and cancer (n = 14) among 32,668 women age 25 to 29 years with ASC-US cytology. The 5-year CR of CIN3/AIS was lowest in obese women (3.62%; 95% CI, 3.15% to 4.17%), followed by overweight (3.94%; 95% CI, 3.46% to 4.48%) and normal/underweight women (4.85%; 95% CI, 4.43% to 5.31%; P trend < .001). We lacked sufficient power to estimate the 5-year CR of cancer in this group.
Fig 2.
Five-year cumulative risk of (A) cervical intraepithelial neoplasia grade 3 and adenocarcinoma in situ (CIN3/AIS) and (B) cancer by body mass index (BMI), stratified by baseline age group. Five-year cumulative risks were estimated using logistic Weibull models. Note that the y-axes have different scales for the left and right panels.
Fig 3.
Five-year cumulative risk of (A) cervical intraepithelial neoplasia grade 3 and adenocarcinoma in situ (CIN3/AIS) and (B) cancer by body mass index (BMI), stratified by baseline human papillomavirus (HPV) status. Five-year cumulative risks were estimated using logistic Weibull models. Note that the y-axes have different scales for the left and right panels.
Fig 4.
Five-year cumulative risk of (A) cervical intraepithelial neoplasia grade 3 and adenocarcinoma in situ (CIN3/AIS) and (B) cancer by body mass index (BMI), stratified by histology. Five-year cumulative risks were estimated using logistic Weibull models. Note that the y-axes have different scales for the left and right panels. ADC, adenocarcinoma; SCC, squamous cell carcinoma.
PAF of Cervical Cancer for Overweight and Obesity
Overall, the 5-year CR of CIN3/AIS for the patients in our study was 0.62%. The estimated reduction of CIN3/AIS risk attributable to being overweight or obese for the patients in our study was 16.6%. In contrast, on the basis of an overall 5-year CR of 0.07%, the percentage of cervical cancer attributable to being overweight or obese was 20.0%.
Ancillary Analyses
Overweight and obese women were slightly older at CIN3/AIS diagnosis (41.2 and 41.5 years, respectively) compared with normal/underweight women (40.6 years; P trend = .002). In contrast, there were no significant differences in age at cancer diagnosis by BMI. We observed similar stage distributions by BMI for cancers with available data (n = 342; 70%; data not shown).
HPV and cytology cotesting.
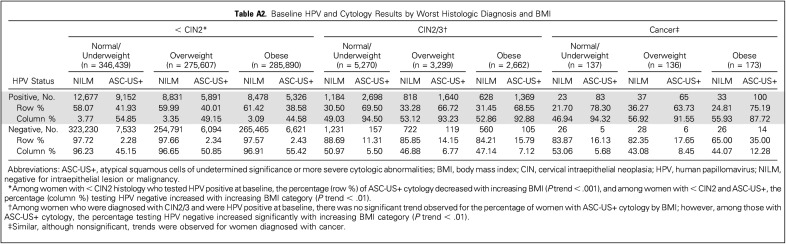
The joint distribution of HPV and cytology cotest results by worst histologic diagnosis and BMI is summarized in Appendix Table A2 (online only). Among HPV-positive women with < CIN2, the percentage with ASC-US+ cytology was lower with increasing BMI (P trend < .001). Among women with < CIN2 or CIN2/3 with ASC-US+ cytology, the percentage with HPV-negative results increased with increasing BMI (P trend < .01). We observed similar, although nonsignificant, trends in women with cancer (Appendix Table A2).
Endocervical component.
Overweight and obese women were more likely to have an endocervical component–negative Pap test compared with normal/underweight women (P trend < .001); however, BMI was still associated with decreased risk of CIN3/AIS and increased risk of cancer after adjusting for endocervical component status (data not shown).
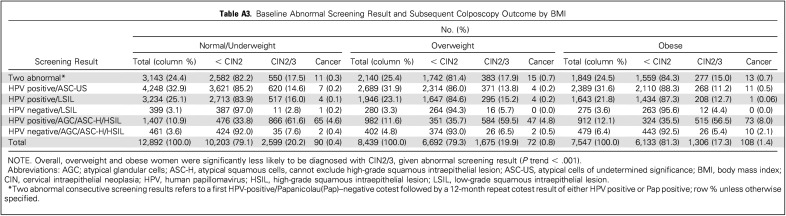
Abnormal screening results and subsequent colposcopy outcomes.
Among those with an available colposcopy result, overweight and obese women were significantly less likely to be diagnosed with CIN2/3 compared with normal/underweight women (P trend < .001; Appendix Table A3, online only). This pattern was consistent across abnormal screening results. In contrast, overweight and obese women were consistently more likely to be diagnosed with cancer compared with normal/underweight women within these groups (P trend < .001).
DISCUSSION
In this analysis of data from a large and state-of-the-art cervical cancer screening program, we present novel and important evidence that suggests that overweight and obese women have a higher risk of cancer, but a lower risk of precancer, compared with normal/underweight women. These findings were consistent irrespective of age, race/ethnicity, HPV status, and histology. Any risk factor associated with increased cervical cancer risk would also be expected to increase precancer risk, and likewise, a decreased precancer risk should lead to a corresponding decreased risk of cancer.26 Thus, the apparent paradoxical association of excess BMI with decreased risk of precancer, but increased risk of cancer, is likely related to underdiagnosis of cervical precancer in overweight and obese patients who were screened for cervical cancer.
To date, the influence of BMI on cervical cancer risk has not been well understood. Obesity has been associated with increased cervical cancer incidence and mortality in a few prospective, population-based studies; however, other studies have reported no association.3-8,10,27 Importantly, most studies have lacked screening information and/or have not separately analyzed precancer end points, which, according to our results, would attenuate risk estimates. Indeed, only one moderately sized cross-sectional study reported on the association of obesity with cancer precursors among women who are HPV-positive, showing a similar association of BMI with reduced risk of CIN2/3 but increased risk of cervical cancer.9 It has been previously suggested that obesity may be a risk factor for ADC, potentially through hormonal mechanisms.5 Although much less is known about the natural history of ADC precursors compared with SCC, there is some evidence that suggests that cervical cancer screening may be less effective for detecting glandular compared with squamous lesions.24 In support of this hypothesis, we found stronger associations of BMI with CIN3 and SCC compared with AIS and ADC, respectively, suggesting that BMI may have less influence on detection of precursors of ADC.
A majority of studies that evaluate the association of BMI with cervical cancer screening have been focused on issues related to frequency and compliance, with most reporting reduced screening rates among obese women.11 In our study of women who attended at least one screening visit, the number of screening tests was similar across BMI categories, and our main findings were consistent for both prevalent and incident precancer and cancer end points. Moreover, although obese women tended to be older at CIN3/AIS diagnosis, we observed similar ages at cancer diagnosis and similar distributions in cancer stage by BMI, which suggests that differences in frequency and compliance among screening participants did not strongly influence our findings.
To our knowledge, ours is the first study to evaluate the influence of BMI on the efficacy of cervical cancer screening in a large, routinely screened population of women. This study has implications regardless of whether the screening program uses cytology, HPV testing, or both. By evaluating the joint distribution of baseline cotest results by worst diagnosis and BMI, we found that reduced sensitivity of both HPV and cytology testing may contribute to underdiagnosis of precancer in overweight and obese women. We hypothesized that the absence of endocervical cells, a crude indicator of inadequate cervical sampling,20 could help explain our findings; however, we failed to find evidence to support causal mediation.
In addition to cervical sampling, it is plausible that visualization of the cervix during colposcopy may be more challenging in overweight and obese women because of a lack of appropriately sized equipment and/or vaginal side-wall retraction. In our study, overweight and obese women who attended colposcopy were less likely to be diagnosed with CIN2/3 compared with normal/underweight women, which suggests that colposcopy may also be less sensitive for detecting CIN2/3 in women with elevated BMI.
Although much attention has been paid to the negative health consequences of obesity, less is known about the influence of excess body weight on the feasibility and accuracy of screening and diagnostic testing, with some studies suggesting an association of obesity with underdiagnosis of prostate cancer14,28 and with poor quality of radiologic imaging.13 By calculating the PAF, we estimated that approximately 20% of cancers in our population could potentially be prevented if the sensitivity achieved for detecting cervical precancer in normal/underweight women could be reached for those who are overweight and obese.
Our analysis has several important strengths. The KPNC cohort represents the longest and largest experience with routine cotesting for cervical cancer screening.17 Women enrolled in KPNC represent a generally well-screened population and are observed through an active tracking system to ensure timely management of abnormal test results,20,29,30 thereby reducing the likelihood that our findings could be explained by differences in access to care. Finally, we used clinically measured height and weight and 5-year median BMI to limit misclassification. There are also some important limitations. First, because we do not know the exact timing of cancer development versus detection, our ability to attribute specific false-negative cotest and/or colposcopy results to cancer diagnosis was limited. Second, approximately 13% of women in KPNC were missing BMI data. Although it is possible that BMI may be differentially measured for obese women compared with nonobese women, BMI category distributions in our population were in line with national estimates.31 It is possible that use of 5-year median BMI at enrollment may have introduced misclassification. Women generally tend to gain weight over time,32-34 and in general, misclassification would tend to underestimate a true association. Results from our validation analysis support this hypothesis, demonstrating stronger associations in women with stable BMI over time. Finally, we lacked information about comorbidities; however, women were healthy enough to attend routine screening.
In conclusion, in this large study of more than 900,000 women undergoing cervical cancer screening using state-of-the-art cotesting, excess BMI was associated with an increased risk of invasive cervical cancer, likely because of underdiagnosis of cervical precancer. Although HPV vaccination holds great promise, screening will remain the mainstay of cervical cancer prevention for decades to come.35 Considering this, along with the worldwide obesity epidemic, our findings have significant implications for the secondary prevention of cervical cancer and signify the need for greater awareness and possibly the development of specific clinical recommendations for screening overweight and obese women. Going forward, it will be important to validate which components of the cervical cancer screening process are failing. Currently, there are no standard quality indicators for cervical sampling in clinical practice, and specimen collection techniques have remained unchanged over the past decade.20 Whether existing equipment (eg, speculum size) and procedures are adequate for visualization and sampling of the cervix in overweight and obese women requires further evaluation.
ACKNOWLEDGMENT
The association of high BMI with invasive cervical cancer at Kaiser Permanente Northern California (KPNC) was suggested by B.F. based on astute, routine reviews of case histories. This is one of her many contributions to improving cervical screening. She was central to the conception and maintenance of the KNPC–National Cancer Institute collaborative epidemiologic analysis of routine cervical screening program data.
Appendix
Ancillary Analysis of the Validity of 5-Year Median Body Mass Index
Rationale.
In our main analysis, we focused on the 5-year median body mass index (BMI) preceding the screening visit to minimize the concern for reverse causality and to approximate a relevant time window for when BMI might affect screening (ie, when precancer should be present and detectable, before cancer develops); however, we acknowledge that using 5-year median BMI at enrollment could potentially lead to misclassification if women were changing BMI categories over time.
Methods.
To assess the validity of using 5-year median BMI at enrollment, we evaluated the effect of potential misclassification of BMI using the full range of longitudinal BMI values in a random subset of approximately 15,000 women in our Kaiser Permanente Northern California study population. BMI was categorized as normal/underweight, overweight, or obese for each time point, and women were then classified into two categories—those who changed BMI categories at least once during the study period (n = 8,609; 54.5%) versus those who remained in the same BMI category throughout the study period (ie, stable; [n = 7,188]; 44.5%). We analyzed the effect of potential misclassification of BMI by stratifying our analysis by change in BMI category versus stable BMI category.
Results.
As shown in Appendix Table A1, we observed similar trends, indicating a lower risk of CIN3/AIS with increasing BMI in both strata, with stronger associations among women with stable BMI throughout the study period.
Discussion.
Results of this validation analysis demonstrate that our results were stronger among women with a stable BMI category over the entire study period, which suggests that our findings may be further strengthened if misclassification were not present.
Table A1.
Five-Year Risk of CIN3/AIS by BMI, Stratified by BMI Category Change

Table A2.
Baseline HPV and Cytology Results by Worst Histologic Diagnosis and BMI
Table A3.
Baseline Abnormal Screening Result and Subsequent Colposcopy Outcome by BMI
Footnotes
Supported by the Intramural Research Program of the National Cancer Institute.
Presented as interim analysis at the 31st International Papillomavirus Conference Cape Town, South Africa, February 28-March 4, 2017.
Processed as a Rapid Communication manuscript.
AUTHOR CONTRIBUTIONS
Conception and design: Megan Clarke, Barbara Fetterman, Nicolas Wentzensen, Walter K. Kinney, Thomas S. Lorey, Philip E. Castle, Mark Schiffman
Collection and assembly of data: Barbara Fetterman, Nancy E Poitras
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Epidemiologic Evidence That Excess Body Weight Increases Risk of Cervical Cancer by Decreased Detection of Precancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Megan A. Clarke
No relationship to disclose
Barbara Fetterman
No relationship to disclose
Li C. Cheung
No relationship to disclose
Nicolas Wentzensen
Other Relationship: Roche (Inst), Becton Dickinson (Inst)
Julia C. Gage
Other Relationship: Roche (Inst), Becton Dickinson (Inst)
Hormuzd A. Katki
No relationship to disclose
Brian Befano
No relationship to disclose
Maria Demarco
No relationship to disclose
John Schussler
No relationship to disclose
Walter K. Kinney
No relationship to disclose
Tina R. Raine-Bennett
Consulting or Advisory Role: TEVA Pharmaceuticals Industries (Inst)
Research Funding: Bayer HealthCare Pharmaceuticals (Inst)
Thomas S. Lorey
No relationship to disclose
Nancy E. Poitras
No relationship to disclose
Philip E. Castle
No relationship to disclose
Mark Schiffman
Other Relationship: Roche (Inst), Becton Dickinson (Inst)
REFERENCES
- 1.Afshin A, Forouzanfar MH, Reitsma MB, et al. : Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377:13-27, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Kruszon-Moran D, Carroll MD, et al. : Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315:2284-2291, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reeves GK, Pirie K, Beral V, et al. : Cancer incidence and mortality in relation to body mass index in the Million Women Study: Cohort study. BMJ 335:1134, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poorolajal J, Jenabi E: The association between BMI and cervical cancer risk: A meta-analysis. Eur J Cancer Prev 25:232-238, 2016 [DOI] [PubMed] [Google Scholar]
- 5.Lacey JV, Jr, Swanson CA, Brinton LA, et al. : Obesity as a potential risk factor for adenocarcinomas and squamous cell carcinomas of the uterine cervix. Cancer 98:814-821, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Kizer NT, Thaker PH, Gao F, et al. : The effects of body mass index on complications and survival outcomes in patients with cervical carcinoma undergoing curative chemoradiation therapy. Cancer 117:948-956, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frumovitz M, Jhingran A, Soliman PT, et al. : Morbid obesity as an independent risk factor for disease-specific mortality in women with cervical cancer. Obstet Gynecol 124:1098-1104, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calle EE, Rodriguez C, Walker-Thurmond K, et al. : Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348:1625-1638, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Lee JK, So KA, Piyathilake CJ, et al. : Mild obesity, physical activity, calorie intake, and the risks of cervical intraepithelial neoplasia and cervical cancer. PLoS One 8:e66555, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhaskaran K, Douglas I, Forbes H, et al. : Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5·24 million UK adults. Lancet 384:755-765, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maruthur NM, Bolen SD, Brancati FL, et al. : The association of obesity and cervical cancer screening: A systematic review and meta-analysis. Obesity (Silver Spring) 17:375-381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castle PE, Kinney WK, Cheung LC, et al. : Why does cervical cancer occur in a state-of-the-art screening program? Gynecol Oncol 146:546-553, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uppot RN, Sahani DV, Hahn PF, et al. : Effect of obesity on image quality: Fifteen-year longitudinal study for evaluation of dictated radiology reports. Radiology 240:435-439, 2006 [DOI] [PubMed] [Google Scholar]
- 14.Bañez LL, Hamilton RJ, Partin AW, et al. : Obesity-related plasma hemodilution and PSA concentration among men with prostate cancer. JAMA 298:2275-2280, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Amy NK, Aalborg A, Lyons P, et al. : Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes 30:147-155, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Bates CK, Carroll N, Potter J: The challenging pelvic examination. J Gen Intern Med 26:651-657, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katki HA, Kinney WK, Fetterman B, et al. : Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: A population-based study in routine clinical practice. Lancet Oncol 12:663-672, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arbyn M, Bergeron C, Klinkhamer P, et al. : Liquid compared with conventional cervical cytology: A systematic review and meta-analysis. Obstet Gynecol 111:167-177, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Solomon D, Davey D, Kurman R, et al. : The 2001 Bethesda System: Terminology for reporting results of cervical cytology. JAMA 287:2114-2119, 2002 [DOI] [PubMed] [Google Scholar]
- 20.Massad LS, Einstein MH, Huh WK, et al. 2012 ASCCP Consensus Guidelines Conference : 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 17:S1-S27, 2013. (suppl 1) [DOI] [PubMed] [Google Scholar]
- 21.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive summary—Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr 68:899-917, 1998 [DOI] [PubMed] [Google Scholar]
- 22.Stoler MH, Schiffman M, Atypical Squamous Cells of Undetermined Significance-Low-grade Squamous Intraepithelial Lesion Triage Study (ALTS) Group : Interobserver reproducibility of cervical cytologic and histologic interpretations: Realistic estimates from the ASCUS-LSIL triage study. JAMA 285:1500-1505, 2001 [DOI] [PubMed] [Google Scholar]
- 23.Castle PE, Stoler MH, Solomon D, et al. : The relationship of community biopsy-diagnosed cervical intraepithelial neoplasia grade 2 to the quality control pathology-reviewed diagnoses: An ALTS report. Am J Clin Pathol 127:805-815, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Schiffman M, Wentzensen N: Human papillomavirus infection and the multistage carcinogenesis of cervical cancer. Cancer Epidemiol Biomarkers Prev 22:553-560, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheung LC, Pan Q, Hyun N, et al. : Mixture models for undiagnosed prevalent disease and interval-censored incident disease: Applications to a cohort assembled from electronic health records. Stat Med 36:3583-3595, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schatzkin A, Freedman LS, Dorgan J, et al. : Surrogate end points in cancer research: A critique. Cancer Epidemiol Biomarkers Prev 5:947-953, 1996 [PubMed] [Google Scholar]
- 27.Song YM, Sung J, Ha M: Obesity and risk of cancer in postmenopausal Korean women. J Clin Oncol 26:3395-3402, 2008 [DOI] [PubMed] [Google Scholar]
- 28.Kaplan SA: Re: The impact of obesity on the predictive accuracy of PSA in men undergoing prostate biopsy. J Urol 194:394-395, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Wright TC, Jr, Massad LS, Dunton CJ, et al. : 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. J Low Genit Tract Dis 11:223-239, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Wright TC, Jr, Cox JT, Massad LS, et al. : 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. J Low Genit Tract Dis 7:154-167, 2003 [DOI] [PubMed] [Google Scholar]
- 31. https://www.cdc.gov/nchs/products/databriefs/db219.htm Ogden CL, Carroll MD, Fryar CD, et al: Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief 219:1-8, 2015. [PubMed]
- 32.Sternfeld B, Wang H, Quesenberry CP, Jr, et al. : Physical activity and changes in weight and waist circumference in midlife women: Findings from the Study of Women’s Health Across the Nation. Am J Epidemiol 160:912-922, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Lee IM, Djoussé L, Sesso HD, et al. : Physical activity and weight gain prevention. JAMA 303:1173-1179, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Drøyvold WB, Nilsen TI, Krüger O, et al. : Change in height, weight and body mass index: Longitudinal data from the HUNT Study in Norway. Int J Obes 30:935-939, 2006 [DOI] [PubMed] [Google Scholar]
- 35.Bosch FX, Broker TR, Forman D, et al. : Comprehensive control of human papillomavirus infections and related diseases. Vaccine 31:I1-I31, 2013. (suppl 8) [DOI] [PMC free article] [PubMed] [Google Scholar]