Abstract
Background
CD8+ T cell-eliciting vaccines are being investigated in breast cancer patients. Preclinical data showed that trastuzumab increases the susceptibility of tumor cells to lysis by vaccine-generated CD8+ T cells suggesting potential benefit of a combination immunotherapy strategy. The current trial was undertaken to demonstrate the safety of this approach.
Methods
This study was designed as a dose-escalation trial enrolling clinically disease-free, HLA-A2+ or A3+, HER2-positive breast cancer patients. Patients received six monthly inoculations of GP2+ granulocyte-macrophage colony-stimulating factor (GM-CSF) administered concurrently with standard of care trastuzumab. Local and systemic toxicity as well as left ventricular ejection fraction (LVEF) were monitored. Immunologic responses were assessed in vivo by measuring the local reaction and in vitro using an IFN-γ ELISPOT assay.
Results
Seventeen disease-free breast cancer patients were vaccinated. There were no dose-limiting or grade 3-5 local or systemic toxicities. The median LVEF was unchanged from baseline after vaccination. Mean local reaction at initial inoculation was 28±10 mm and increased to 68±8 mm at the final inoculation (p<0.01). Mean ELISPOT response to GP2 increased from 47±19 at baseline to 144±60 (p=13) after vaccination. Based on safety and immunologic data, the appropriate dose was determined to be 1000 μg of GP2 + 250 μg of GM-CSF.
Conclusion
The GP2+GM-CSF vaccine is safe and stimulates an immunologic response when given concurrently with trastuzumab. An ongoing phase II trial is evaluating the efficacy of combining a CD8 T cell-eliciting vaccine with trastuzumab in HER2-positive breast cancer patients.
Synopsis
Combining trastuzumab with CD8+ T cell-eliciting HER peptide vaccines may provide synergistic immunotherapeutic benefit in breast cancer. This phase I trial demonstrates the GP2 + GM-CSF vaccine given concurrently with trastuzumab is safe and stimulates an immune response.
Introduction
Trastuzumab, a human IgG1 monoclonal antibody that targets the extracellular domain of the HER2 protein, is routinely administered to HER2-positive breast cancer patients. Trastuzumab functions via multiple mechanisms, including decreasing signaling by preventing HER2 dimerization, increasing endocytic destruction of the HER2 receptor, and inhibiting extracellular domain shedding. 1,2 Immune-mediated mechanisms of action have also been described including antibody dependent cellular cytotoxicity (ADCC). 3,4 ADCC leads to antigen release, triggering uptake and cross-presentation by dendritic cells, stimulating an anti-HER2 CD8+ T cell response. 5,6 Trastuzumab also stimulates endogenous anti-HER2 antibody and anti-HER2 CD4+ T cell responses. 7,8
The GP2 (HER2: 654-662) peptide vaccine is comprised of the HLA-A2- and A3-restricted, HER2-derived peptide GP2 combined with the immunoadjuvant granulocyte macrophage colony-stimulating factor (GM-CSF). Early phase trials demonstrated the vaccine to be safe and capable of generating a HER2-specific CD8+ T cell response. 9,10 The phase II trial randomized HLA-A2/A3+ breast cancer patients with any level of HER2 expression (immunohistochemistry [IHC] 1-3+) in their tumor to receive six monthly inoculations of GP2+GM-CSF or GM-CSF alone with booster inoculations every six months thereafter. An intention-to-treat analysis performed at a median follow-up of 34 months, showed an 88% estimated 5-year disease-free survival (DFS) rate in vaccinated patients versus 81% in GM-CSF only patients (p=0.43). 10 In HER2-positive patients (all received trastuzumab) DFS was 94% in the vaccinated patients compared to 89% in GM-CSF only patients (p=0.86). Per-treatment analysis, which excluded recurrences during the primary vaccination series and secondary malignancies, showed 100% DFS in vaccinated HER2-positive patients compared to 89% in GM-CSF only patients (p=0.08). Breast cancer recurrences occurred only during the primary vaccination series, which was given after completing standard therapy to include trastuzumab. Given this, we hypothesized that by administering the vaccine earlier, concurrently with trastuzumab, the stimulated immune response may prevent early recurrences.
Here we describe a phase I trial (NCT03014076) designed to evaluate the combination of GP2+GM-CSF administered concurrently with trastuzumab. The primary objective was to determine safety of the combination. Secondary objectives were to determine dosing and immunologic response.
Patients and Methods
Patient Characteristics and Clinical Protocol
This single center, phase Ib dose-escalation trial was conducted under an investigational new drug application (BB-IND#11730). Eligible patients had to have histologically confirmed, stage I-III HER2-positive breast cancer and be receiving trastuzumab as part of their therapy. HER2-positive was defined as IHC 3+ or a fluorescence in situ hybridization ratio > 2.0 (study enrolled prior to guideline changes). Enrollment occurred any time after diagnosis, however, initiation of study treatment occurred after completion of surgery, chemotherapy, and radiation such that the vaccination series overlapped with the trastuzumab monotherapy portion of the treatment regimen. Because GP2 is HLA-A2 and HLA-A3 restricted, after initial consent for screening, each patient's HLA-A2 and HLA-A3 status was determined. HLA-A2+ and HLA-A3+ patients were eligible to sign a treatment consent and participate.
The study was a 3+3 phase dose escalation/optimization trial with three patients enrolled in each of four dosing cohorts with an expansion cohort at the maximum delivered dose (MDD) (table). Expansion was performed at the MDD because there was no dose limiting toxicity at any of the lower doses. A higher dose could not be administered due to the volume required to solubilize the peptide for injection. The primary objective was to determine the safety of the combination therapy. Secondary objectives included determining dosing and immunologic responses. The study was approved by The MD Anderson Cancer Center Institutional Review Board.
Table.
Dosing scheme for the 3+3 trial.
| Cohort | Dose | Patients |
|---|---|---|
| 1 | GP2 100 μg + GM-CSF 125 μg | 3 |
| 2 | GP2 500 μg + GM-CSF 125 μg | 3 |
| 3 | GP2 500 μg + GM-CSF 250 μg | 3 |
| 4 | GP2 1000 μg + GM-CSF 250 μg | 3 |
| Expansion Cohort at MDD | GP2 1000 μg + GM-CSF 250 μg | 5 |
GM-CSF = granulocyte-macrophage colony-stimulating factor; MDD = maximum delivered dose
Vaccine and Vaccination Series
Good manufacturing practices grade GP2 peptide was purified to >95%. Sterility, endotoxin, and general safety testing were carried out by the manufacturer. Lyophilized peptide was reconstituted in sterile saline and mixed with GM-CSF (Berlex, Seattle, WA) to a final 1 ml volume. The primary vaccination series consisted of six inoculations given every 21 days with trastuzumab infusion. The 1.0 ml inoculation was divided, with 0.5 ml given intradermally at two sites, 5 cm apart in the same lymph node draining area (upper thigh).
Toxicity
Patients were monitored for one hour after inoculation for hypersensitivity reactions. Local and systemic toxicity was assessed 48-72 hours after each inoculation. Dose-limiting toxicity was considered grade ≥ 3 local or systemic toxicity, as per NCI-CTCAE version 3.0.
Cardiac toxicity was monitored with echocardiograms performed prior to initiation of trastuzumab and vaccination and every three months while on treatment. A left ventricular ejection fraction (LVEF) of ≥50% was required for enrollment. Per protocol, patients were discontinued from study treatment if a decrease in LVEF >10%, symptomatic congestive heart failure, or grade ≥ 3 cardiac toxicity was observed.
Immune Monitoring
In vivo immune monitoring involved measuring the local reactions in two dimensions at the inoculation site using the sensitive ball-point pen test 48-72 hours after each inoculation 11. In vitro immune monitoring was performed using an enzyme-linked immunosorbent spot (ELISPOT) assay for interferon-γ secretion in response to GP2 and a second HER2-derived peptide, AE36, to determine epitope spreading. 5×105 cells/200μL/well freshly isolated peripheral blood mononuclear cells (PBMC) in culture medium supplemented with interleukin-7 (20ng/mL) were added into flat-bottom wells of antihuman interferon (IFN)-γ ELISPOT plates (PD Pharmingen). Duplicate wells of PBMC were stimulated in the absence (culture medium only) or presence of 25μg/mL GP2 or AE36 overnight at 37°C + 5% CO2. The plate was then processed and developed per manufacturer instructions. IFN-γ-secreting cells were enumerated using the ELISPOT analyzer and Immunospot Professional Software (CTL Analyzers LLC). GP2 peptide-specific IFN-γ-secreting cells were calculated by subtracting the total number of spots in the control wells from the total number of spots in GP2-stimulated wells. Results are presented as number of spots per 106 PBMCs. Laboratory staff performing the biologic assays were blinded to the patient's assigned dose level as well as inoculation number.
Statistical Analysis
Median values were compared using the Wilcoxon rank sum test for matched samples, and means were compared with paired or unpaired t-test, as appropriate.
Results
Patients
Seventeen HER2-positive patients were enrolled and vaccinated. Median age was 47 years (range 30-56). Thirteen patients (76%) had tumors larger than 2cm, 13 (76%) were node positive, 11 (65%) were grade 3, and 10 were either estrogen or progesterone receptor positive. Eleven (65%) were HLA-A2 positive and 6 (35%) were HLA-A3 positive.
Safety
The vaccine was well tolerated with only grade 1 and 2 local and systemic toxicity observed. As shown in figure 1A, for 82% of patients, the maximum local toxicity was grade 1. The remaining patients (18%) experienced grade 2 local toxicity. The most common local toxicities included induration (100%) and pruritis (76%) at the injection site. The maximum systemic toxicity was grade 1 for 35% and grade 2 for 18% of patients. Most common symptoms included headache (29%) and fatigue (29%). 47% of patients did not experience systemic toxicity. No dose-limiting toxicities were found.
Figure 1. Toxicity associated with the combination of GP2+GM-CSF vaccine and trastuzumab.
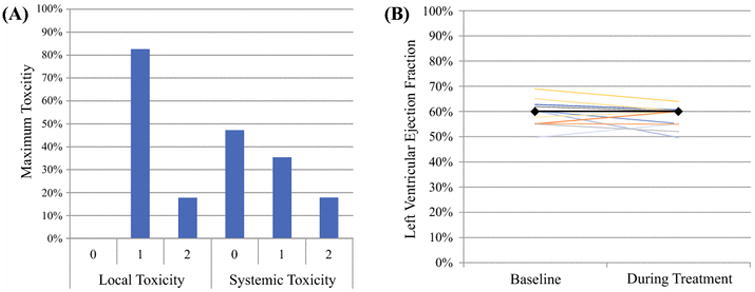
(A) Local and systemic toxicity depicted as the percentage of patients in whom their highest grade toxicity was the designated grade. No grade 3 or 4 local toxicity was observed. (B) Results of LVEF prior to starting treatment with the GP2+GM-CSF vaccine and trastuzumab as well as during treatment as assessed per study protocol. The median ejection fraction (solid black line) did not change during the course of treatment.
Baseline echocardiograms were obtained a median of 68 days prior to the first inoculation. The median LVEF was 60% (range 53-69%). Midway through the vaccination series (median 99 days after enrollment), the median LVEF remained at 60% (range 52-62 (Figure 1B)). One patient experienced an asymptomatic 10% drop in LVEF (60% to 50% at 73 days after enrollment) that did not require holding or stopping treatment per protocol or published recommendations. Fourteen patients had echocardiograms a median of 61 days after vaccination series completion. The median LVEF was 60% (range 50-60%).
Immunologic Response
Mean local reaction after the initial inoculation was 28±10 mm which increased after each subsequent inoculation (p<0.02 compared to baseline). The local reaction plateaued after the fourth inoculation at a mean of 70±8 mm (p=0.001 versus baseline) that decreased slightly to a mean of 68±8 mm after the final inoculation (p<0.001 versus baseline) (Figure 2A). Although the differences did not reach statistical significance, patients receiving the maximum dose, GP2 1000μg + GM-CSF 250μg, had larger local reactions at all time points than patients in lower dose cohorts (Figure 2B). HLA-A2+ patients (n=11) had larger local reactions compared to HLA-A3+ (n=6) patients with significant differences observed after the third (71±7 versus 39±13 mm, p=0.03) and fifth inoculations (75±9 versus 36±17, p=0.04) (Figure 2C).
Figure 2. In vivo immunologic response to vaccination as determined by local reaction measurements.
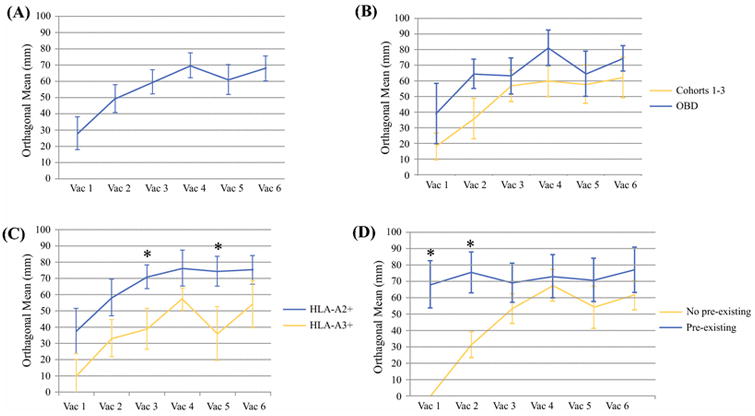
(A) Local reactions to inoculations throughout the vaccination measured as the orthogonal mean. (B) Local reactions comparing those in dosing cohorts 1-3 versus those in cohort 4 who received the maximum delivered dose. (C) Local reactions in HLA-A2+ patients compared to HLA-A3+ patients. (D) Local reactions in patients with pre-existing immunity defined as any reaction to the initial inoculation compared to patients without pre-existing immunity.
Ten patients had no discernable local reaction to the initial inoculation and were considered to have no pre-existing GP2 immunity. Seven patients had a measurable response to their initial inoculations, with a mean local reaction of 68±14 mm. Patients without pre-existing immunity had increasingly larger local reactions over the first two inoculations. The mean local reaction plateaued at a size similar to those with pre-existing immunity after the second inoculation. For patients with pre-existing immunity, the mean local reaction size did not change significantly (Figure 2D).
In vitro immunologic responses were assessed using the ELISPOT assay. The mean number of IFN-γ secreting spots in response to GP2 increased to 144±60 after completion of the vaccination series versus 46±19 at baseline (p=0.13). The spots subsequently decreased to near baseline 6-months after completion of the vaccine series, suggesting waning immunity (Figure 3A). No difference in ELISPOT reactions between any dosing cohorts or based on HLA-A2 versus HLA-A3 status was found. ELISPOT responses against the HER2-derived epitope AE37 were assessed for evidence of epitope spreading. There was an increase in the mean number of IFN-γ secreting spots from pre-vaccination (25±9 spots) to mid-vaccination (61±27, p=0.23), post-vaccination (71±36, p=0.16), and 6-months post-vaccination (67±44, p=0.30) (Figure 3B).
Figure 3. In vitro immunologic response to vaccination as determined by ELISPOT assay.
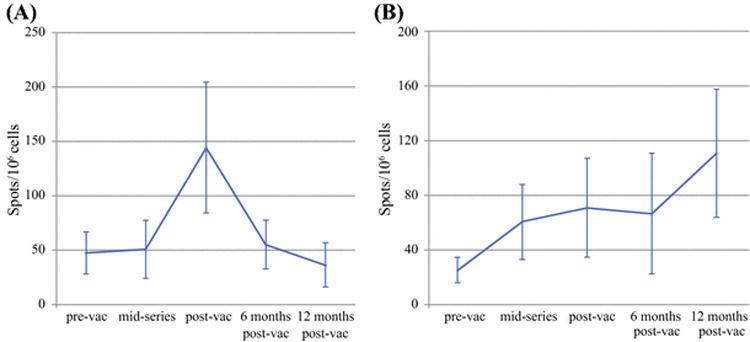
(A) Immune response against the immunizing peptide GP2. (B) Immune response against AE36, another HER2-derived epitope. Generation of an immune against this peptide that was not part of the immunizing mix confirms epitope spreading.
Discussion
Combined with trastuzumab, the GP2+GM-CSF vaccine is safe, with no local or systemic toxicity greater than grade 2, and no increase in cardiotoxicity. The combination induces a dose- and HLA-type-dependent immunologic response as well as intra-antigenic epitope spreading, suggesting a broad immune response.
The mild toxicity seen in this study parallels previous trials of GP2+GM-CSF alone, and is consistent with injection site reactions and systemic symptoms generated by immunologic responses to vaccinations. 9,10 No clinically significant cardiac toxicity was observed. Transient asymptomatic declines in LVEF were seen in three patients, similar to the expected rate for trastuzumab alone. In a trial evaluating HER2-targeted vaccination using a dendritic cell vaccine as monotherapy in patients with ductal carcinoma in situ, a transient, asymptomatic decline in cardiac function corresponding with induction of HER2-specific cellular mediated immune responses was observed. 12 This occurred in three of 27 (11%) vaccinated patients. In all cases, circulating anti-HER2 antibodies were measurable before vaccination. In our trials investigating other HER2-directed vaccines, including E75+GM-CSF (NCT00841399, NCT00584789) and AE37+GM-CSF (NCT00524277), we did not see clinically significant cardiac toxicity. 13-16 Additionally, HER2-directed vaccination with concurrent trastuzumab administered in the metastatic setting demonstrated a similar, low incidence of transient, asymptomatic decline in LVEF. 17-19
Here we show that the GP2 vaccine plus trastuzumab is capable of stimulating immunologic responses. Immunity is dose dependent and increases rapidly in response to the initial inoculations and then plateaus later in the vaccination series, as shown in previous peptide vaccine trials. 20 Some patients experienced large local reactions to the initial inoculation. We believe this represents pre-existing immunity against GP2. In a phase II trial evaluating the GP2 peptide vaccine as monotherapy (NCT00524277), large local reactions were associated with lower recurrence rates in breast cancer patients (unpublished data). We made a similar observation in our phase II study evaluating the AE37+GM-CSF vaccine (NCT00524277), where a robust initial local reaction was associated with a lower recurrence rate (unpublished data). The size of the local reaction after vaccination may serve as a biomarker to predict immunologic response. One limitation of this study is that we cannot compare the immune response generated by vaccine alone to that stimulated by vaccine plus trastuzumab, or the response generated by trastuzumab alone to that stimulated by vaccine plus trastuzumab. Our ongoing phase II trials randomizing patients to trastuzumab or trastuzumab plus vaccine will provide insight to this question.
Interestingly, the local reaction to GP2 vaccine given concurrently with trastuzumab was less robust in HLA-A3+ patients than HLA-A2+ patients. In a previous trial of the CD8 T cell-eliciting E75 vaccine, HLA-A3+ patients had immunological and clinical responses similar to HLA-A2+ patients.21 E75 has a higher predicted binding affinity to HLA-A2 and HLA-A3 than GP2.22 Because GP2 is not predicted to bind as well as E75 to HLA-A2, it is considered a subdominant epitope. Despite this, in preclinical studies, our group demonstrated GP2 immunogenicity using a T2 model and by demonstrating epitope spreading to the GP2 antigen in blood samples collected from E75+GM-CSF-vaccinated HLA-A2+ patients. 23,24 Crystallographic analysis of the GP2 structure shows that the peptide center does not make stabilizing contacts with the binding cleft of the MHC class I molecule. 25 It is therefore possible that the peptide assumes multiple conformations that can generate additional molecular surfaces recognized by various T cell receptors. 24 Decreased affinity may lead to less immunologic tolerance. In this study, the data suggest that, for HLA-A3+ patients, the binding of GP2 may not be sufficient to generate an effective immune response.
We observed an increased immunologic response to AE36, an immunogenic epitope from the HER2 intracellular domain, indicating epitope spreading, a broader immunologic response from proteolysis, and presentation of additional HER2 epitopes for recognition by the immune system. We have previously reported that vaccination with the E75+GM-CSF vaccine induces intra- and inter-antigenic epitope spreading and have hypothesized that, for peptide vaccines to elicit a strong anti-tumor immune response, epitope spreading is likely essential. 23
The data from this study supports further evaluation of combination strategies employing a CD8+ T cell-eliciting vaccine with trastuzumab. We are currently conducting two such trials. One evaluates the E75+GM-CSF vaccine in combination with trastuzumab in patients with high risk, HER2-positive breast cancer (NCT02297698).26 High risk patients have residual disease following neoadjuvant systemic therapy that includes anti-HER2 targeted therapy with trastuzumab (with or without pertuzumab) or, for those undergoing surgery as an initial intervention, significant nodal disease defined as any positive nodes in patients with hormone receptor negative, HER2-positive tumors or four or more positive nodes in patients with hormone receptor positive, HER2-positive tumors. After completing surgical therapy, patients are randomized to receive either trastuzumab alone to complete one year (standard practice) or to receive trastuzumab with the vaccine administered concurrently for six inoculations administered every 3 weeks × 6. Booster inoculations are administered every six months out through 3 years to address waning immunity which could contribute to late recurrences. The second trial assesses the same combination in patients with HER2 low-expressing tumors, i.e., IHC 1+ or 2+ (NCT01570036).27 Patients are eligible if they are node-positive, regardless of hormone receptor status or if they are node-negative and hormone receptor negative. While trastuzumab is clearly active in patients with HER2-positive breast cancer, 28 it is not currently approved for use in patients with HER2 low-expressing tumors. We noted in our previous phase I/II trials evaluating HER2-derived, CD8 T cell-eliciting vaccines (enrolled patients who had tumors with any degree of HER2 expression) that vaccination resulted in stronger immunologic responses in patients with HER2 1+ or 2+ tumors. 19 This correlated with a decreased disease recurrence rate. We hypothesize that lower HER2 expression levels may lead to less immunologic tolerance. However, it is possible that low and intermediate HER2-expressing tumors could have insufficient antigen presentation, causing decreased recognition by peptide-stimulated cytotoxic T lymphocytes. The concurrent use of trastuzumab may create a synergistic effect via ADCC promoting cross-presentation 5,6 by promoting HER2 receptor internalization with a subsequent increase in antigen processing and presentation 29 leading to enhanced epitope spreading, and by stimulating an anti-HER2 CD4+ helper T cell response. 8
Acknowledgments
This work was funded by a Clinical Investigator Award from the Society of Surgical Oncology and Komen for the Cure Foundation to Elizabeth A. Mittendorf and Norwell Inc through a grant to George E. Peoples via the Henry M. Jackson Foundation. Additional funding was provided by the United States Military Cancer Institute and the Nancy Owens Memorial Foundation. Elizabeth A. Mittendorf is a R. Lee Clark Fellow at The University of Texas MD Anderson Cancer Center, supported by the Jeanne F. Shelby Scholarship Fund. The study was conducted at The University of Texas MD Anderson Cancer Center which is supported by a Cancer Center Support Grant from the National Institutes of Health (CA016672).
Funding sources were not involved with the study design; in the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Disclosures: Drs. Peoples and Ponniah have partial inventor rights to GP2. If licensed, they are entitled to financial proceeds associated with this license per Federal policy. Dr. Peoples also consults in the development of the vaccine. All other authors have no relevant financial disclosures.
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense or the U.S. Government.
References
- 1.Hudis CA. Trastuzumab--mechanism of action and use in clinical practice. NEJM. 2007;357(1):39–51. doi: 10.1056/NEJMra043186. [DOI] [PubMed] [Google Scholar]
- 2.Vu T, Claret FX. Trastuzumab: updated mechanisms of action and resistance in breast cancer. Front Oncol. 2012;2:62. doi: 10.3389/fonc.2012.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beano A, Signorino E, Evangelista A, et al. Correlation between NK function and response to trastuzumab in metastatic breast cancer patients. J Transl Med. 2008;6:25. doi: 10.1186/1479-5876-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohrt HE, Houot R, Weiskopf K, et al. Stimulation of natural killer cells with a CD137-specific antibody enhances trastuzumab efficacy in xenotransplant models of breast cancer. J Clin Invest. 2012;122(3):1066–1075. doi: 10.1172/JCI61226. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Dhodapkar KM, Krasovsky J, Williamson B, Dhodapkar MV. Antitumor monoclonal antibodies enhance cross-presentation ofcCellular antigens and the generation of myeloma-specific killer T cells by dendritic cells. J Exp Med. 2002;195(1):125–133. doi: 10.1084/jem.20011097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rafiq K, Bergtold A, Clynes R. Immune complex-mediated antigen presentation induces tumor immunity. J Clin Invest. 2002;110(1):71–79. doi: 10.1172/JCI15640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knutson KL, Clynes R, Shreeder B, et al. Improved Survival of HER2+ Breast Cancer Patients Treated with Trastuzumab and Chemotherapy Is Associated with Host Antibody Immunity against the HER2 Intracellular Domain. Cancer Res. 2016;76(13):3702–3710. doi: 10.1158/0008-5472.CAN-15-3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor C, Hershman D, Shah N, et al. Augmented HER-2 specific immunity during treatment with trastuzumab and chemotherapy. Clin Cancer Res. 2007;13(17):5133–5143. doi: 10.1158/1078-0432.CCR-07-0507. [DOI] [PubMed] [Google Scholar]
- 9.Carmichael MG, Benavides LC, Holmes JP, et al. Results of the first phase 1 clinical trial of the HER-2/neu peptide (GP2) vaccine in disease-free breast cancer patients: United States Military Cancer Institute Clinical Trials Group Study I-04. Cancer. 2010;116(2):292–301. doi: 10.1002/cncr.24756. [DOI] [PubMed] [Google Scholar]
- 10.Mittendorf EA, Ardavanis A, Litton JK, et al. Primary analysis of a prospective, randomized, single-blinded phase II trial evaluating the HER2 peptide GP2 vaccine in breast cancer patients to prevent recurrence. Oncotarget. 2016;7(40):66192–66201. doi: 10.18632/oncotarget.11751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jordan TJ, Sunderam G, Thomas L, Reichman LB. Tuberculin reaction size measurement by the pen method compared to traditional palpation. Chest. 1987;92(2):234–236. doi: 10.1378/chest.92.2.234. [DOI] [PubMed] [Google Scholar]
- 12.Bahl S, Roses RE, Sharma A, et al. Asymptomatic changes in cardiac function can occur in ductal carcinoma-in-situ patients following treatment with HER-2/neu-pulsed dendritic cell vaccines. Am J Surg. 2009;198(4):488–494. doi: 10.1016/j.amjsurg.2009.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes JP, Benavides LC, Gates JD, et al. Results of the first phase I clinical trial of the novel II-key hybrid preventive HER-2/neu peptide (AE37) vaccine. J Clin Oncol. 2008;26(20):3426–3433. doi: 10.1200/JCO.2007.15.7842. [DOI] [PubMed] [Google Scholar]
- 14.Mittendorf EA, Ardavanis A, Symanowski J, et al. Primary analysis of a prospective, randomized, single-blinded phase II trial evaluating the HER2 peptide AE37 vaccine in breast cancer patients to prevent recurrence. Ann Oncol. 2016;27(7):1241–1248. doi: 10.1093/annonc/mdw150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mittendorf EA, Clifton GT, Holmes JP, et al. Final report of the phase I/II clinical trial of the E75 (nelipepimut-S) vaccine with booster inoculations to prevent disease recurrence in high-risk breast cancer patients. doi: 10.1093/annonc/mdu211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peoples GE, Holmes JP, Hueman MT, et al. Combined clinical trial results of a HER2/neu (E75) vaccine for the prevention of recurrence in high-risk breast cancer patients: U.S. Military Cancer Institute Clinical Trials Group Study I-01 and I-02. Clin Caner Res. 2008;14(3):797–803. doi: 10.1158/1078-0432.CCR-07-1448. [DOI] [PubMed] [Google Scholar]
- 17.Chen G, Gupta R, Petrik S, et al. A feasibility study of cyclophosphamide, trastuzumab, and an allogeneic GM-CSF-secreting breast tumor vaccine for HER2+ metastatic breast cancer. Cancer Immunol Res. 2014;2(10):949–961. doi: 10.1158/2326-6066.CIR-14-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Disis ML, Wallace DR, Gooley TA, et al. Concurrent trastuzumab and HER2/neuspecific vaccination in patients with metastatic breast cancer. J Clin Oncol. 2009;27(28):4685–4692. doi: 10.1200/JCO.2008.20.6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benavides LC, Gates JD, Carmichael MG, et al. The impact of HER2/neu expression level on response to the E75 vaccine: from U.S. Military Cancer Institute Clinical Trials Group Study I-01 and I-02. Clin Cancer Res. 2009;15(8):2895–2904. doi: 10.1158/1078-0432.CCR-08-1126. [DOI] [PubMed] [Google Scholar]
- 20.Benavides LC, Sears AK, Gates JD, et al. Comparison of different HER2/neu vaccines in adjuvant breast cancer trials: implications for dosing of peptide vaccines. Expert Rev Vaccines. 2011;10(2):201–210. doi: 10.1586/erv.10.167. [DOI] [PubMed] [Google Scholar]
- 21.Patil R, Clifton GT, Holmes JP, et al. Clinical and immunologic responses of HLA-A3+ breast cancer patients vaccinated with the HER2/neu-derived peptide vaccine, E75, in a phase I/II clinical trial. J Am Coll Surg. 2010;210(2):140–147. doi: 10.1016/j.jamcollsurg.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 22.Peoples GE, Goedegebuure PS, Smith R, Linehan DC, Yoshino I, Eberlein TJ. Breast and ovarian cancer-specific cytotoxic T lymphocytes recognize the same HER2/neu-derived peptide. Proc Natl Acad Sci U S A. 1995;92(2):432–436. doi: 10.1073/pnas.92.2.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mittendorf EA, Gurney JM, Storrer CE, Shriver CD, Ponniah S, Peoples GE. Vaccination with a HER2/neu peptide induces intra- and inter-antigenic epitope spreading in patients with early stage breast cancer. Surgery. 2006;139(3):407–418. doi: 10.1016/j.surg.2005.06.059. [DOI] [PubMed] [Google Scholar]
- 24.Mittendorf EA, Storrer CE, Foley RJ, et al. Evaluation of the HER2/neu-derived peptide GP2 for use in a peptide-based breast cancer vaccine trial. Cancer. 2006;106(11):2309–2317. doi: 10.1002/cncr.21849. [DOI] [PubMed] [Google Scholar]
- 25.Kuhns JJ, Batalia MA, Yan S, Collins EJ. Poor binding of a HER-2/neu epitope (GP2) to HLA-A2.1 is due to a lack of interactions with the center of the peptide. J Biol Chem. 1999;274(51):36422–36427. doi: 10.1074/jbc.274.51.36422. [DOI] [PubMed] [Google Scholar]
- 26.Phase II trial of combination immunotherapy with NeuVax and Trastuzumab in high-risk HER2+ breast cancer patients. [Accessed February 15, 2017]; https://clinicaltrials.gov/ct2/show/NCT02297698.
- 27.Combination immunotherapy with Herceptin and the HER2 vaccine NeuVax. [Accessed February 15, 2017]; https://clinicaltrials.gov/ct2/show/NCT01570036.
- 28.Perez EA, Romond EH, Suman VJ, et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2-positive breast cancer: planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. J Clin Oncol. 2014;32(33):3744–3752. doi: 10.1200/JCO.2014.55.5730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mittendorf EA, Storrer CE, Shriver CS, Ponniah S, Peoples GE. Investigating the combination of trastuzumab and HER2/neu peptide vaccines for the treatment of breast cancer. Ann Surg Oncol. 2006;13(8):1085–1098. doi: 10.1245/ASO.2006.03.069. [DOI] [PubMed] [Google Scholar]


