Abstract
Background:
Motivation is necessary in patients with heart failure (HF) who are attempting to become more physically active but may not be sufficient to initiate physical activity. Self-efficacy might explain the relationship between motivation and physical activity.
Objective:
The aim of this study was to examine the role of exercise self-efficacy in the relationship between exercise motivation and physical activity in patients with HF.
Methods:
A total of 100 stable patients with HF (88% in New York Heart Association class II/III; mean age, 67 ± 13 years; 62% men) were studied. Self-efficacy was measured with the Exercise Self-Efficacy Scale; motivation, with the Exercise Motivation Index; and physical activity, with a self-report questionnaire. Logistic regression analyses were made to examine the mediation effect of exercise self-efficacy on the relationship between exercise motivation and physical activity.
Results:
Forty-two percent of the 100 patients reported engaging in less than 60 minutes per week of physical activity. Motivation predicted physical activity (b = 0.58, P < .05), but after controlling for self-efficacy, the relationship between motivation and physical activity was no longer significant (b = 0.76, P = .06), indicating full mediation.
Conclusion:
Motivation to be physically active is important but not sufficient. In addition to a high level of motivation to be physically active, it is important that patients with HF have a high degree of self-efficacy.
KEY WORDS: mediation, moderation, motivation, physical activity, self-efficacy
Being physically active is important for patients with heart failure (HF) because exercise capacity can be increased and deterioration leading to hospitalization can be reduced.1,2 However, despite the benefits of being physically active, most patients with HF are not as active as recommended in guidelines,3–5 that is, 30 minutes of low- to moderate-intensity activity, 5 days a week.6 Barriers for patients with HF to become more physically active include general barriers such as lack of motivation and lack of time, as well as HF-specific barriers such as dyspnea and fatigue.7–9
Being motivated to exercise is an important first step in becoming more physically active. Motivation or intention to be physically active is a key concept in several theories and models that explain healthy behaviors.10–13 However, it is known that there is a gap between intention and physical activity.
Almost half of the people who are motivated and intend to be physically active according to guideline recommendations are still not.14 Motivated patients with HF are more active and better able to describe the benefits of exercise.3,15 Motivations for patients with HF were found to be mainly related to factors associated with the patients themselves (eg, mental state), the social interaction during exercise, the patients' physical condition, and therapy (eg, diuretics). Motivation was seldom related to benefits that were directly related to the patients' HF condition, for example, outcomes or experienced benefits.3,15 Previous research has found that motivation is not enough to improve physical activity. Furthermore, in behavioral research, self-efficacy is considered to be important in patients with HF16,17 and could influence the gap between intention and physical activity.
Self-efficacy is defined as “the belief in one's capabilities to organize and execute the courses of action required to produce given attainment.”12 Self-efficacy is described as a cognitive mechanism that mediates behavior and that can also influence participation in various behaviors. Self-efficacy determines the amount of effort and degree of persistence in pursuing the behavior.12,17
Self-efficacy could be a mediator in the relationship between motivation and physical activity, which implies that motivation results in a change in self-efficacy, which in turn results in increased physical activity. In total mediation, self-efficacy is necessary to complete a cause-effect link between motivation and physical activity. In such cases, future interventions to increase activity might need to focus more on improving self-efficacy before expecting results in motivation.
A better understanding of mediators can help tailor interventions to the needs of patients with HF.18 Therefore, this study aims to examine the possible mediation of exercise self-efficacy in the relationship between exercise motivation and physical activity in patients with HF.
Methods
Design, Setting, and Participants
This is a cross-sectional study. Patients were enrolled from 4 Swedish centers participating in a multicenter HF trial (evaluating the effect of exergaming on exercise capacity19; clinicaltrial.gov identifier, NCT01785121). Eligibility criteria for participation in the study were diagnosis of HF by a cardiologist, age of older than 18 (no upper age limit), and ability to speak/understand the Swedish language. Exclusion criteria were inability to use an exergame platform that was tested in the main study (eg, due to problems with balance or restricted eyesight), inability to fill in questionnaires, and a life expectancy shorter than 6 months.
Data Collection
After the patients gave written informed consent, a research assistant/research nurse distributed questionnaires during a clinic visit. Data reported in this study were collected from baseline assessments, before any intervention took place. Ethical approval was obtained (DNR 2012/247-31).
The amount of physical activity was measured by 1 self-reported question: “In the past week (even if it is not a typical week), how much time did you spend exercising or being physically active (eg, strength training, walking, swimming, gardening, or other type of training)?” The response options were (1) none, (2) less than 30 minutes per week, (3) 30 to 60 minutes per week, (4) more than 1 and up to 3 hours per week, and (5) more than 3 hours per week. More than 60 minutes per week was defined as being physically active, whereas less than 60 minutes per week was defined as not being physically active (1, <60-minute activity/wk; 2, >60-minute activity/wk). The single-item question that was used was easy to complete and construct. Face and content validity has previously been established and has been used in several previous studies.20,21
Exercise self-efficacy was measured with the Exercise Self-Efficacy Questionnaire. The questionnaire assesses self-efficacy beliefs specifically related to confidence to exercise related to potential barriers: work schedule, physical fatigue, boredom related to exercise, minor injuries, other time demands, and family and home responsibilities. It consists of 6 situations that might affect participation in exercise. For each situation, the patients used a scale ranging from 1 (not confident) to 10 (very confident) to describe their current confidence in being able to exercise for 20 minutes, 3 times a week. The instrument is reliable and valid22; the Cronbach's α in this study was .89.
Exercise motivation was assessed with the exercise motivation index. The index consists of 15 statements followed by a 5-point rating scale for each statement, ranging from 0 (not important) to 4 (extremely important). Three subscores (0–4) were calculated by summing the scores for physical, psychological, and social motivation and dividing them by the number of statements for each area.23 The Swedish version of the index is found to be valid and reliable.23 The Cronbach's α in this study was .92.
Procedures and Statistical Analyses
All analyses were conducted using SPSS 23. Descriptive statistics were used to characterize the study population. In the descriptive analyses, means and standard deviations were calculated for continuous data, and absolute numbers and percentages were computed for nominal variables.
Self-efficacy functions as a mediator when it meets the following conditions (see Figure 1) in the following steps of Baron and Kenny24:
FIGURE 1.
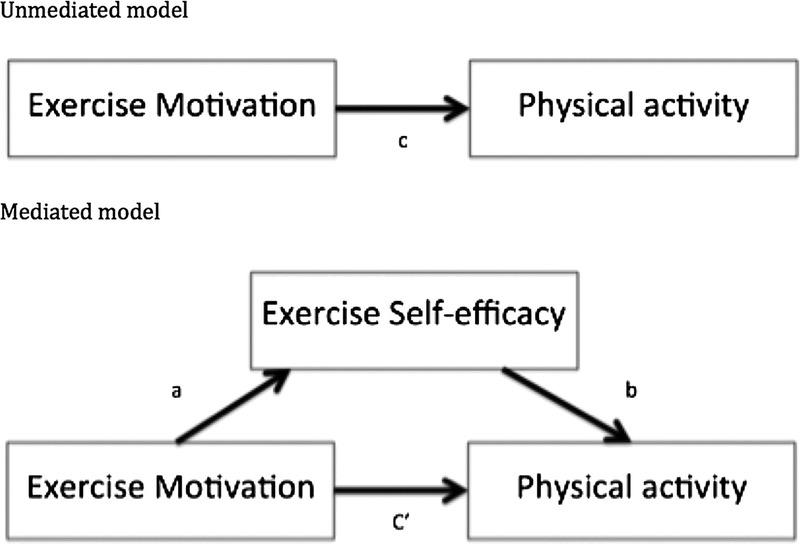
Hypothetical mediation relationship involving exercise motivation, physical activity, and exercise self-efficacy. Path c in the model is the total effect. Path c' is called the direct effect.
Step 1: The causal variable (exercise motivation) is correlated with the outcome (physical activity). Physical activity was used as the criterion variable in the regression equation; and exercise motivation, as a predictor (estimate and test path c in Figure 1). This step establishes that there is an effect that may be mediated.
Step 2: The causal variable (exercise motivation) is correlated with the mediator (exercise self-efficacy). Exercise self-efficacy was used as the criterion variable in the regression equation; and exercise motivation, as a predictor (estimate and test path a in Figure 1). This step essentially involves treating the mediator as if it were an outcome variable.
Step 3: The mediator (exercise self-efficacy) affects the outcome variable (physical activity). Physical activity was used as the criterion variable in the regression equation; and exercise motivation and exercise self-efficacy, as predictors (estimate and test path b in Figure 1). It is not sufficient to only correlate the mediator with the outcome because the mediator and the outcome may be correlated because they are both caused by the causal variable physical activity. Thus, the causal variable must be controlled in establishing the effect of the mediator on the outcome.
Step 4: To establish that exercise self-efficacy completely mediates the exercise motivation–physical activity relationship, the effect of exercise motivation on physical activity controlling for exercise self-efficacy (path c') should be zero. The effects in both steps 3 and 4 were estimated in the same equation.
The regression model(s) was controlled for age, sex, and New York Heart Association (NYHA) class. These variables were included based on former literature about older adults and patients with HF.4,25,26
Results
Participants
The participants' mean (SD) age was 67 (13) years, and 62% were male (Table). Most of the patients were married or in a relationship (67%), and 88% were in NYHA class II/III (Table). No study patients were in NYHA IV.
TABLE.
Sample Characteristics of 100 Patients With Heart Failure
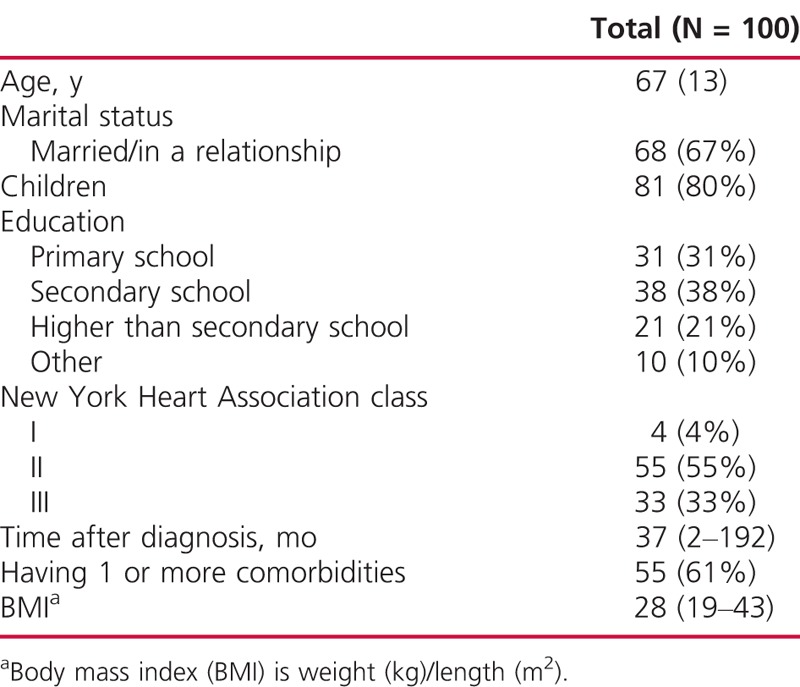
More than half of the HF patients (58%) were physically active for more than 60 minutes a week. Only 3 patients were not active at all, 11% were active for less than 30 minutes a week (n = 11), 28% were active between 30 and 60 minutes a week (n = 28), 32% were active for more than 1 and up to 3 hours a week (n = 32), and 26% were active for more than 3 hours a week (n = 26).
Patients had an average exercise motivation of 2 (±1) (scale ranging from 0 [not important] to 4 [extremely important]), and the mean exercise self-efficacy was 5 (±2) (scale ranging from 1 [not confident] to 10 [very confident]).
Exercise motivation predicted physical activity (b = 0.58, P = .02). Exercise motivation and exercise self-efficacy were significantly correlated (r = 0.15, P < .01). Exercise self-efficacy was significantly correlated to the amount of physical activity (r = 0.46, P < .01). After controlling for exercise self-efficacy, the effect of exercise motivation on physical activity was zero (b = 0.76, P = .06), indicating full mediation (Figure 2). Sex (b = 0.55, P = .36), age (b = −0.03, P = .22), and NYHA class (b = −0.41, P = .46) did not have a significant association with the amount of physical activity, but adding them to the model increased the explanatory value (R2). Together, 24% of the variance in the amount of physical activity was explained (R2 = 0.17 if sex, age, and NYHA class were not included as covariates) (Figure 2).
FIGURE 2.
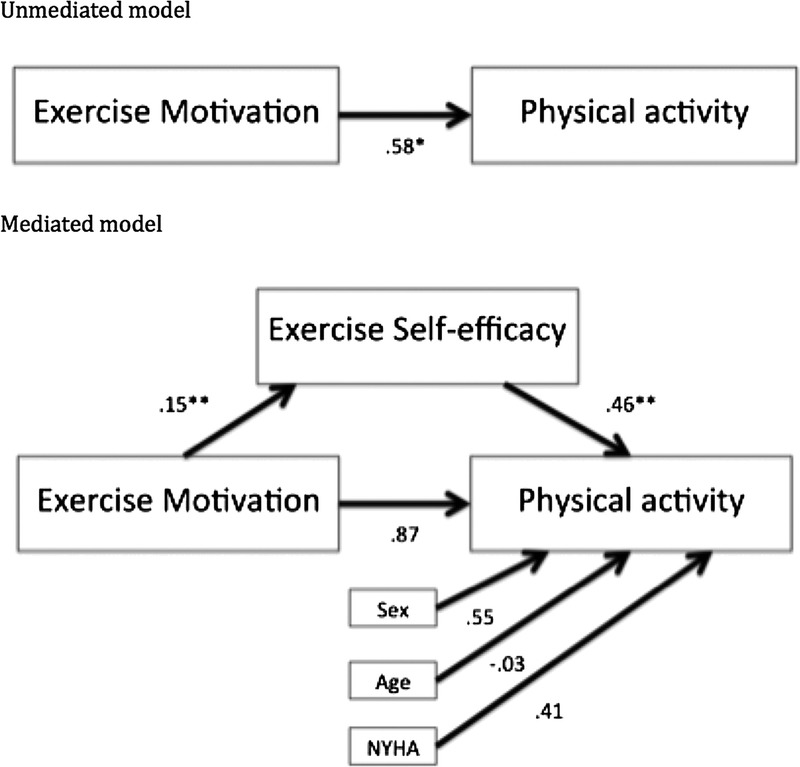
Mediation model in 100 heart failure patients. Control variables were sex (men, 1; women, 2), age, and New York Heart Association (NYHA) class. *P < .05. **P < .01.
Discussion
To date, no previous investigators have evaluated the relationships between self-efficacy, motivation, and physical activity in patients with HF. We found that self-efficacy mediated the relationship between motivation and physical activity in patients with HF. Indeed, motivation did not make a significant contribution to the prediction of physical activity after self-efficacy had been introduced into the model. This finding suggests that, when self-efficacy is low, high motivation might not lead to an increase in physical activity. However, in instances where self-efficacy is high, motivation is more likely to lead to higher physical activity. This result shows that the challenge of increasing physical activity in patients with HF goes beyond simply motivating patients and extends to increasing self-efficacy for engaging in exercise.27,28
From earlier studies, it also is known that it is important not only to motivate patients concerning potential benefits for their disease but also to aim at improving the intrinsic motivations. Other studies have shown that there are differences in motivations between men and women.3,28 For these reasons, it is important to tailor physical activity for each patient and to look specifically at their motivations and barriers and investigate which motivations could be increased to decrease barriers, essentially to improve self-efficacy for exercise. In addition, it is important to look at barriers that are difficult for motivations to overcome.
Goal setting, graphic feedback, problem-solving support, peer teaching, skills mastery, reinterpretation of symptoms, social persuasion, and motivational interviewing are known techniques that could increase motivation and self-efficacy for physical activity in patients with HF.29–34
In a meta-analysis35 in which the contribution of specific intervention techniques was compared with changes in both self-efficacy and physical activity behavior outcomes in “healthy adults,” it was found that action planning (specific detailed planning of when, where, and how the specific behavior is going to be performed) produced significantly higher self-efficacy and physical activity behavior scores. Providing instruction and reinforcing effort toward a behavior were associated with significantly higher levels of both self-efficacy and physical activity. Although self-efficacy is seen as important for changing physical activity in patients with HF,17 there is limited research in patients with HF and interventions specifically targeting self-efficacy in physical activity. The techniques described for increasing motivation and self-efficacy could be helpful in the development of interventions aiming at increasing physical activity in patients with HF.
To increase motivation and self-efficacy in physical activity, it is important to offer more than only cardiac rehabilitation in the hospital.28 Looking at the literature, new physical activity programs could be useful among patients with HF, such as dancing,36 yoga,37,38 tai chi,39,40 and exergaming.19,41
Using self-assessment of the amount of physical activity is a limitation in this study. Although this single-item question has been tested and used previously,20,21 it would have been a strength if convergent validity had been established, correlating the self-assessed item with objective measures of physical activity. Using an objective method, such as an accelerometer, would have provided considerable greater precision in the measurement of physical activity. An objective measurement would also have provided patterns of activity on a minute-by-minute basis.
The patients with HF in this study were enrolled in a physical activity interventional study, and therefore, they might possibly have been more motivated to become more physically active than the general population of patients with HF. In addition, these patients were all selected from Swedish centers, and for this reason, generalizing the results to all patients with HF should be done with caution.
Finally, the simple mediation model only explained 24% of the variance in physical activity among patients with HF. Other variables that could influence physical activity in patients with HF are, for example, more social support and better knowledge of the benefits, adverse effects of medication, and comorbidities.27,28,42
The clinical implications of our findings are that motivation might not be enough to engage patients with HF in physical activity. Instead of trying to convince people how important it is to be active, healthcare professionals need to spend time assessing barriers for physical activity and help patients to increase their confidence in overcoming those barriers. This assessment may help health professionals to identify barriers that they could decrease immediately to increase patients' self-efficacy. An example of such a barrier is the distance to the sport facility; healthcare professionals could discuss physical activities at home, thus increasing self-efficacy. To increase confidence in overcoming barriers, healthcare professionals could focus on specific detailed planning of when, where, and how physical activity is going to be performed and providing instruction and reinforcing effort toward physical activity.35 These techniques could guide patients toward the most appropriate physical activity program method for their particular case.
Conclusion
This research contributes to the body of knowledge on psychological mechanisms in physical activity in HF patients. The results demonstrate that exercise motivations in physical activity, as well as self-efficacy beliefs, are important when performing physical activity. Higher levels of motivation lead patients with HF to a higher level of self-efficacy (thereby experiencing less barriers), which in turn leads them to a higher level of physical activity.
What's New and Important
Motivation to be physically active is important, but not sufficient in becoming more physical active in patients with heart failure.
Motivation leads to a higher degree of self-efficacy, which in turn leads patients with heart failure to a higher level of physical activity.
It is important to tailor physical activity on patients' motivations and self-efficacy to physical activity and offer a variety of formats.
Footnotes
This work is supported through the Swedish National Science Council (K2013-69X-22302-01-3), the Swedish Heart and Lung Association (E085/12), the Swedish Heart-Lung Foundation (20130340), the Vårdal Foundation (2014-0018), and FORSS (474681) and by the Swedish National Science Council/Swedish Research Council for Health, Working Life and Welfare (VR-FORTE) (2014-4100).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Lewinter C, Doherty P, Gale CP, et al. Exercise-based cardiac rehabilitation in patients with heart failure: a meta-analysis of randomised controlled trials between 1999 and 2013. Eur J Prev Cardiol. 2015;22(12):1504–1512. [DOI] [PubMed] [Google Scholar]
- 2.Taylor RS, Sagar VA, Davies EJ, et al. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;(4):CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klompstra L, Jaarsma T, Stromberg A. Physical activity in patients with heart failure: barriers and motivations with special focus on sex differences. Patient Prefer Adherence. 2015;9:1603–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dontje ML, van der Wal MH, Stolk RP, et al. Daily physical activity in stable heart failure patients. J Cardiovasc Nurs. 2014;29(3):218–226. [DOI] [PubMed] [Google Scholar]
- 5.Jaarsma T, Stromberg A, Ben Gal T, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient Educ Couns. 2013;92(1):114–120. [DOI] [PubMed] [Google Scholar]
- 6.Piepoli MF, Conraads V, Corrà U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13(4):347–357. [DOI] [PubMed] [Google Scholar]
- 7.Corvera-Tindel T, Doering LV, Woo MA, Khan S, Dracup K. Effects of a home walking exercise program on functional status and symptoms in heart failure. Am Heart J. 2004;147(2):339–346. [DOI] [PubMed] [Google Scholar]
- 8.Evangelista LS, Berg J, Dracup K. Relationship between psychosocial variables and compliance in patients with heart failure. Heart Lung. 2001;30(4):294–301. [DOI] [PubMed] [Google Scholar]
- 9.Pihl E, Fridlund B, Mårtensson J. Patients' experiences of physical limitations in daily life activities when suffering from chronic heart failure; a phenomenographic analysis. Scand J Caring Sci. 2011;25(1):3–11. [DOI] [PubMed] [Google Scholar]
- 10.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. [DOI] [PubMed] [Google Scholar]
- 11.Resnick B, Nigg C. Testing a theoretical model of exercise behavior for older adults. Nurs Res. 2003;52(2):80–88. [DOI] [PubMed] [Google Scholar]
- 12.Bandura A. Self-efficacy—towards a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 13.Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114. [DOI] [PubMed] [Google Scholar]
- 14.Rhodes RE, Bruijn GJ. How big is the physical activity intention-behaviour gap? A meta-analysis using the action control framework. Br J Health Psychol. 2013;18(2):296–309. [DOI] [PubMed] [Google Scholar]
- 15.Tierney S, Elwers H, Sange C, et al. What influences physical activity in people with heart failure?: a qualitative study. Int J Nurs Stud. 2011;48(10):1234–1243. [DOI] [PubMed] [Google Scholar]
- 16.Tierney S, Mamas M, Skelton D, et al. What can we learn from patients with heart failure about exercise adherence? A systematic review of qualitative papers. Health Psychol. 2011;30(4):401–410. [DOI] [PubMed] [Google Scholar]
- 17.Du H, Everett B, Newton PJ, Salamonson Y, Davidson PM. Self-efficacy: a useful construct to promote physical activity in people with stable chronic heart failure. J Clin Nurs. 2012;21(3–4):301–310. [DOI] [PubMed] [Google Scholar]
- 18.Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(2 suppl):5–14. [DOI] [PubMed] [Google Scholar]
- 19.Jaarsma T, Klompstra L, Ben Gal T, et al. Increasing exercise capacity and quality of life of patients with heart failure through Wii gaming: the rationale, design and methodology of the HF-Wii study; a multicentre randomized controlled trial. Eur J Heart Fail. 2015;17(7):743–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hjelm C, Strömberg A, Årestedt K, Broström A. Association between sleep-disordered breathing, sleep-wake pattern, and cognitive impairment among patients with chronic heart failure. Eur J Heart Fail. 2013;15(5):496–504. [DOI] [PubMed] [Google Scholar]
- 21.Liljeroos M, Ågren S, Jaarsma T, Årestedt K, Strömberg A. Long term follow-up after a randomized integrated educational and psychosocial intervention in patient-partner dyads affected by heart failure. PLoS One. 2015;10(9):e0138058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dzewaltowski D. Toward a model of exercise motivation. J Sport Exerc Psychol. 1989;11:215–269. [Google Scholar]
- 23.Stenström CH, Boestad C, Carlsson M, Edström M, Reuterhäll A. Why exercise?: a preliminary investigation of an exercise motivation index among individuals with rheumatic conditions and healthy individuals. Physiother Res Int. 1997;2(1):7–16. [DOI] [PubMed] [Google Scholar]
- 24.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 25.Crombie IK, Irvine L, Williams B, et al. Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age Ageing. 2004;33(3):287–292. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Facts about Physical Activity. 2012. https://www.cdc.gov/physicalactivity/data/facts.htm. Accessed January 30, 2015. [Google Scholar]
- 27.van der Wal MH, van Veldhuisen DJ, Veeger NJ, Rutten FH, Jaarsma T. Compliance with non-pharmacological recommendations and outcome in heart failure patients. Eur Heart J. 2010;31(12):1486–1493. [DOI] [PubMed] [Google Scholar]
- 28.Conraads VM, Deaton C, Piotrowicz E, et al. Adherence of heart failure patients to exercise: barriers and possible solutions: a position statement of the Study Group on Exercise Training in Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2012;14(5):451–458. [DOI] [PubMed] [Google Scholar]
- 29.Barbour KA, Miller NH. Adherence to exercise training in heart failure: a review. Heart Fail Rev. 2008;13(1):81–89. [DOI] [PubMed] [Google Scholar]
- 30.Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabil Nurs. 2003;28(4):117–122. [DOI] [PubMed] [Google Scholar]
- 31.Smeulders ES, van Haastregt JC, Ambergen T, Janssen-Boyne JJ, van Eijk JT, Kempen GI. The impact of a self-management group programme on health behaviour and healthcare utilization among congestive heart failure patients. Eur J Heart Fail. 2009;11(6):609–616. [DOI] [PubMed] [Google Scholar]
- 32.Brodie DA, Inoue A, Shaw DG. Motivational interviewing to change quality of life for people with chronic heart failure: a randomised controlled trial. Int J Nurs Stud. 2008;45(4):489–500. [DOI] [PubMed] [Google Scholar]
- 33.Brodie DA, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. J Adv Nurs. 2005;50(5):518–527. [DOI] [PubMed] [Google Scholar]
- 34.Du HY, Newton PJ, Zecchin R, et al. An intervention to promote physical activity and self-management in people with stable chronic heart failure The Home-Heart-Walk study: study protocol for a randomized controlled trial. Trials. 2011;12:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams SL, French DP. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour—and are they the same? Health Educ Res. 2011;26(2):308–322. [DOI] [PubMed] [Google Scholar]
- 36.Neto MG, Menezes MA, Carvalho VO. Dance therapy in patients with chronic heart failure: a systematic review and a meta-analysis. Clin Rehabil. 2014;28(12):1172–1179. [DOI] [PubMed] [Google Scholar]
- 37.Krishna BH, Pal P, Pal GK, et al. Yoga improves quality of life and functional capacity in heart failure patients. Biomed Res. 2014;25(2):178–182. [Google Scholar]
- 38.Cramer H, Lauche R, Haller H, Dobos G, Michalsen A. A systematic review of yoga for heart disease. Eur J Prev Cardiol. 2015;22(3):284–295. [DOI] [PubMed] [Google Scholar]
- 39.Pan L, Yan J, Guo Y, Yan J. Effects of Tai Chi training on exercise capacity and quality of life in patients with chronic heart failure: a meta-analysis. Eur J Heart Fail. 2013;15(3):316–323. [DOI] [PubMed] [Google Scholar]
- 40.Yeh GY, McCarthy EP, Wayne PM, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171(8):750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klompstra L, Jaarsma T, Stromberg A. Exergaming to increase the exercise capacity and daily physical activity in heart failure patients: a pilot study. BMC Geriatr. 2014;14:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Santaularia N, Jaarsma T. Motivational factors for exercise in cardiac patients? A literature review. Eur J Prev Med. 2013;1(1):1–19. [Google Scholar]


