Summary
Introduction
The trapeziometacarpal (TMC) joint osteoarthritis (OA) is at the origin of important secondary functional disability to pinch as well as a painful grip. Several conservative therapies are often considered in the early stages of TMC OA to decrease pain, recover function and slow the evolution of OA. They include massage therapy, heat applications, stretching of the first web span and assisted mobilization of the TMC joint. However, as with other arthritic joints, many physicians often suggest administering intra-articular corticosteroids. The aim of this study was to assess the effect of 10 sessions of physiotherapy versus a single corticoid intra-articular injection. Both treatments were associated with TMC splinting.
Methods
Two groups of twenty-five patients received either physiotherapy or a corticoid injection. They were followed over a one-year period. All of them were assessed for pain, function, strength at 2, 6 and 12 months and overall satisfaction at the end of the study.
Results
With the infiltrative therapy, the parameters improve more quickly, whereas patients treated with physiotherapy show longer persistence regarding remission of pain. The final functional evaluation scores at one year are similar to pretreatment scores.
Conclusion
In early stages of TMC OA, corticosteroids articular injections and physiotherapy treatments can improve the painful symptoms but treatment with corticosteroids is faster. Although hand functions return to average scores similar to those of pre-treatment, physiotherapy program is associated with a longer remission of pain.
Keywords: osteoarthritis, physiotherapy, steroid injection, trapeziometacarpal joint
Introduction
The trapeziometacarpal (TMC) joint osteoarthritis (OA), or basal joint arthritis of the thumb, is the second most common degenerative joint disease of the hand1–3. Middle-aged and elderly post-menopausal women are the most affected4. Primary OA is usually idiopathic, however jobs involving repetitive use of the thumb are more often associated with TMC OA5,6 and less frequently associated with rheumatoid arthritis or trauma7. The possible role of obesity in hand OA is also well-known and it must be included in the list of risk factors8,9.
TMC OA is often a disabling condition because of the pain and the adduction contracture with the narrowing of the first web space which compromise pinch and grasp. Being instrumental to thumb opposition, TMC joint OA impairs both the kinematics of the first digital ray as well as the overall hand functioning. Differing degrees of OA and pain intensity help the physician decide whether to opt for a conservative or a surgical treatment10–12. Conservative therapy of TMC OA aims at relieving pain while restoring thumb strength and is generally prescribed in patients suffering from early stages of basal joint arthritis or prior to surgical reconstruction of the joint, indicated in more advanced arthritic stages1,10. Management of TMC joint OA can be developed in different ways with local application of heat, motion exercises and muscles strengthening among these. Many physicians also suggest intra-articular injections of drugs such as corticosteroids, hyaluronic acid or PRP13,14. Splinting of the joint has also been proposed as an important part of conservative management of TMC joint OA15–17.
This study intended comparing two groups of patients affected by early stages of TMC joint OA treated with either physiotherapy or a corticoid intra-articular injection. Both treatments were followed by a period of joint splinting. The Authors report the clinical results, to support and verify nonsurgical treatments for the management of this frequent degenerative hand disease.
Materials and methods
This is an open-label trial approved by the local ethical committee conducted between January 2015 and March 2016. The study was conducted according to international standards and as required by the journal, meeting the ethical standards requested18.
Inclusion criteria
Patients presenting a primary TMC joint OA with a radiographic Eaton-Littler stage 1 to 2 and pain were considered for this study. As well known, Eaton-Littler classification1 is a radiographic rating used to define the severity of basal joint arthritis.
Patients selection was based on clinical evaluation including isolated pain at the base of the first metacarpal, tenderness over the TMC joint, a positive grind test result and a radiographic assessment including antero-posterior and lateral views of the TMC joint documented with recent radiographs (<6 months before). Patients suffering from rheumatoid arthritis or from the sequelae of trauma were excluded from the study; patients that underwent any recent treatment for trapeziometacarpal OA and subjects that received previous injections were also excluded.
Population of the study
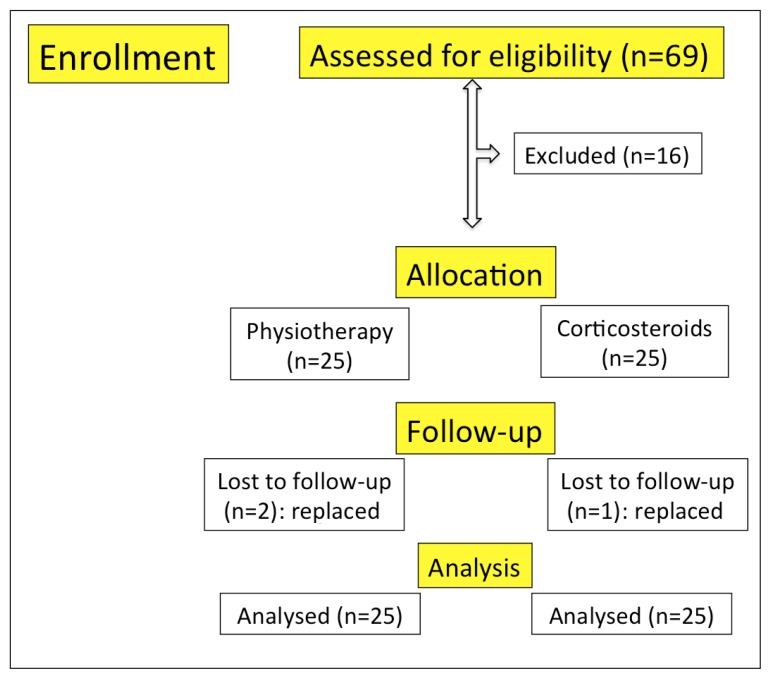
Patients were examined in the out-patient Orthopaedics & Hand Surgery department of The Catholic University School of Medicine, Rome, Italy. All the potential candidates, affected by pain on the radial side of carpus, suggesting a TMC joint AO, were referred to and examined by a hand surgeon. If the patients fulfilled the criteria previously stipulated, they were selected for the study. Sixty-nine patients were recruited consecutively in one year. All of them presented painful primary TMC OA with a radiographic Eaton-Littler stage 1 to 2. Patients were proposed two kinds of treatment: ten sessions of physiotherapy followed by four weeks of joint protection by splinting, or a corticosteroid intra-articular injection, followed by four weeks of splinting. Of the initial group, 40 patients chose the physiotherapy program, 29 the joint injection treatment. The first consecutive 25 patients who chose the physiotherapy were selected for the study as group P, the first consecutive 25 patients which chose the corticoid injection were selected as group C. The remaining patients also received treatment, but they were not included in the study. Three cases (2 from group P and 1 from group C) lost to follow-up and replaced by three more consecutive cases (Fig. 1).
Figure 1.
Patients enrollment.
Upon first examination, among the 50 selected for the study, 19 patients presented an Eaton-Littler stage 1 and 31 patients a stage 2. In 21 cases the TMC joint OA affected both hands, but pain was more intense on the dominant side. The onset of symptoms ranged between 5 and 26 months prior to treatment (with a mean period of 9 +/− 22 SD months). Women prevailed in sex distribution (41 women versus 9 men). The mean age was 62 years +/− 6 SD (range 44–76) (Table I). All patients signed a written informed consent to participate at the study.
Table I.
Demographic characteristics of the study population.
| Patients | Sex | Eaton-Littler | Age (months) | Group | Onset |
|---|---|---|---|---|---|
| 1 | f | 1 | 44 | p | 6 |
| 2 | f | 2 | 51 | p | 12 |
| 3 | f | 1 | 56 | c | 5 |
| 4 | f | 2 | 60 | p | 6 |
| 5 | m | 2 | 62 | c | 7 |
| 6 | f | 1 | 68 | c | 7 |
| 7 | f | 1 | 65 | c | 5 |
| 8 | f | 2 | 57 | c | 9 |
| 9 | m | 2 | 67 | c | 8 |
| 10 | m | 2 | 54 | p | 12 |
| 11 | f | 1 | 70 | p | 6 |
| 12 | f | 1 | 54 | c | 9 |
| 13 | f | 2 | 66 | p | 12 |
| 14 | m | 2 | 68 | c | 6 |
| 15 | f | 2 | 68 | c | 6 |
| 16 | f | 2 | 72 | p | 9 |
| 17 | f | 2 | 69 | p | 6 |
| 18 | m | 2 | 73 | c | 10 |
| 19 | m | 2 | 66 | c | 12 |
| 20 | f | 1 | 57 | p | 6 |
| 21 | f | 2 | 62 | p | 12 |
| 22 | f | 1 | 68 | p | 8 |
| 23 | f | 2 | 71 | c | 9 |
| 24 | m | 2 | 67 | p | 7 |
| 25 | f | 2 | 50 | p | 10 |
| 26 | f | 1 | 62 | p | 6 |
| 27 | f | 2 | 47 | c | 12 |
| 28 | f | 2 | 60 | p | 26 |
| 29 | f | 1 | 58 | c | 12 |
| 30 | f | 1 | 67 | p | 8 |
| 31 | f | 1 | 54 | c | 10 |
| 32 | f | 2 | 68 | c | 9 |
| 33 | m | 2 | 62 | c | 6 |
| 34 | f | 1 | 59 | p | 6 |
| 35 | f | 2 | 76 | c | 9 |
| 36 | f | 1 | 57 | c | 24 |
| 37 | f | 2 | 60 | p | 8 |
| 38 | f | 1 | 70 | c | 8 |
| 39 | f | 2 | 59 | p | 6 |
| 40 | f | 2 | 64 | p | 13 |
| 41 | f | 1 | 64 | c | 6 |
| 42 | f | 1 | 57 | p | 5 |
| 43 | f | 1 | 54 | c | 7 |
| 44 | f | 2 | 68 | c | 8 |
| 45 | f | 2 | 55 | c | 9 |
| 46 | f | 2 | 53 | p | 6 |
| 47 | f | 2 | 72 | p | 14 |
| 48 | m | 2 | 66 | c | 12 |
| 49 | f | 2 | 60 | p | 14 |
| 50 | f | 1 | 66 | p | 10 |
Treatment
Group P: The care plan included 10 physical therapy sessions with a hand therapist, monday to friday for two weeks. A physical therapy session (30–40 minutes each) included both physical agent application and therapeutic exercise. The application of heat (paraffin wax and hot pack) was followed by passive and active mobilization of the TMC joint, massage therapy and stretching of the first web span. A thermoplastic custom-made thumb modified spica splint19 (with first metacarpal positioned in slight abduction and free thumb metacarpal-phalangeal and inter-phalangeal joint), was applied during the initial visit (Fig. 2).
Figure 2.
Splint limiting the TMC joint stress while allowing the MCP joint motion.
Group C: Patients were treated in an out-patient surgery. Hand skin was disinfected with betadine (10% povidone-iodine) topical antiseptics solution. The patients’ TMC joint thumbs were manipulated manually. The injection was given with a 25-gauge needle, dorsal to the abductor pollicis longus- extensor pollicis brevis tendons. The needle was placed so as to slip down to the base of the first metacarpal and advanced to pierce the joint capsule (Fig. 3). The same physician (the first Author L.R.) performed all the injections. The methylprednisolone acetate (40 mg/1 mL) (that is the commonly used corticosteroid in our hospital for these pathologies) and lidocaine (10 mg) solution was injected until the joint was full. The hand was then placed in an analogous custom-made thermoplastic splint.
Figure 3.
TMC joint injection.
Post-treatment care
Patients were instructed to keep full-time splinting for four weeks so as to avoid mechanical stresses to the TMC joint and to promote the solution of the inflammation and pain. After this period, they were instructed regarding hand activities which needed avoiding so as to preclude relapse of pain in the TMC joint; these included strong grasping, imbalance between joint movement and rest, exposure of the finger joints to vibrations and using the joint in an unstable plane20.
Functional assessment
Each patient received a subjective assessment for: 1. TMC joint pain and restriction of activities to four degrees: a. no pain or restriction, b. mild pain with use and some restriction, c. pain at rest with some restriction, d. pain at rest with severe restriction; 2. function in daily living activities, by a questionnaire for arm, shoulder and hand disabilities (DASH)21; 3. overall treatment satisfaction, on a scale of 1 to 10 (1=totally dissatisfied and 10=completely satisfied) at 12 months.
An objective assessment was made to evaluate key pinch strength, recorded in kilograms by a Preston pinch meter (Fig. 4).
Figure 4.
Preston pinch meter.
Assessments were performed in four stages: just prior to treatment, then at 2, 6 and 12 months. The same physicians (the second Author A.M.) took care about all these assessments. The complications following therapies were also recorded.
Statistical analysis
All data were initially entered into an Excel database (Microsoft, Redmond, Washington-United States) and the analysis was performed using the Statistical Package for the Social Sciences Windows, version 13.0 (SPSS, Chicago, Illinois, USA). Descriptive statistics consisted of the mean ± standard deviation (SD) for parameter with gaussian distributions (after confirmation with histograms and the Kolgomorov-Smirnov test). Comparison variables in time (pretreatment, 2 months, 6 months, 12 months) was performed with the ANOVA for repeated measures or Kruskal-Wallis (groups >2) or Mann-Whitney (groups =2) for non-parametric variables and the Chi-Square test or Fisher’s exact test (if cells<5) for categorical variables. p value of <0.05 was considered statistically significant.
Results
Pain (Tab. II, panel A)
Table II.
Outcomes.
| panel A. PAIN AND FUNCTIONAL RESTRICTION | pre-treatment | 2 months | 6 months | 12 months | |
|---|---|---|---|---|---|
| no pain or restriction | Group P | 0 | 16 | 16 | 10† |
| Group C | 0 | 20 | 14 | 2 | |
| mild pain under use: some restriction | Group P | 21 | 9 | 8 | 14 |
| Group C | 18 | 4 | 10 | 17 | |
| pain score at rest: same restriction | Group P | 4 | 0 | 1 | 1 |
| Group C | 7 | 1 | 1 | 6 | |
| pain at rest: severe restriction | Group P | 0 | 0 | 0 | 0 |
| Group C | 0 | 0 | 0 | 0 |
| panel B. DASH SCORE AND SATISFACTION | pre-treatment | 2 months | 6 months | 12 months | |
|---|---|---|---|---|---|
| mean DASH ± SD score | Group P | 8,2 ± 1,2 | 7,4(^) ± 1,6 | 4,1 ± 1,4 | 7,2 ± 2,8 |
| Group C | 10,8 ±2,0 | 3,8 (*) ± 1,0 | 5,3 ± 0,6 | 8,6 ± 0,6 | |
| Overall satisfaction | Group P | 8,2 ± 1,8 | |||
| Group C | 6,8 ± 1,4 |
| panel C. | pre-treatment | 2 months | 6 months | 12 months | |
|---|---|---|---|---|---|
| Mean Key Pinch strenght (kg) | Group P | 4,6 ± 2,2 | 5,0 ± 3,4 | 5,8 ± 2,5 | 5,2 ±2,2 |
| Group C | 4,3 ± 1,6 | 5,4 ± 0,4 | 5,2 ± 1,6 | 4,8 ± 1,8 |
p<0,05; to 2 months Group P vs Group C;
p<0,05 pre-treatment vs 2 months;
p<0,05; to 2 months Group P vs Group C
Group P: Prior to treatment 21 patients were recorded with mild pain with use and 4 patients with pain at rest and functional restriction. Between two and six months, 16 patients reported no pain or restriction. One year after treatment, only one patient complained of pain at rest while 14 reported occasional mild pain causing limited restriction. In 10 cases pain was still absent at one year: this value is statistically significant compared to group C (p <0.05).
Group C: Prior to treatment 18 patients reported mild pain with use and 7 reported pain at rest and functional restriction. At two months, 20 patients reported no pain or restriction. Result decreased at six months and, at one year, 17 patients reported some restriction due to pain with use and 6 patients complained of pain at rest.
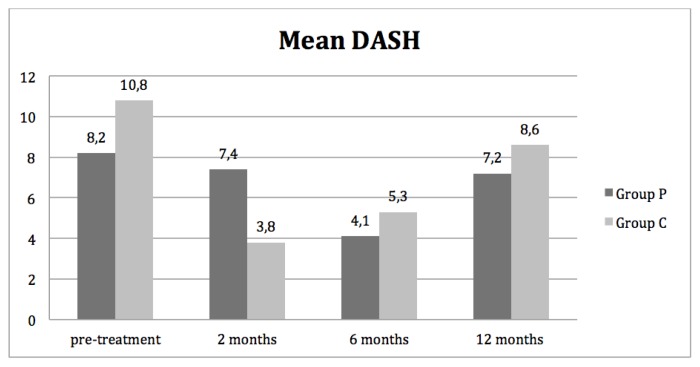
Function in activities of daily living (Tab. II, panel B)
Group P: Subjective assessment of functional disability in daily living activities at pre-treatment amounted to a mean DASH score of 8.2. Six months after therapy, mean DASH score progressively decreased to 4.1 then, at one year, increased to 7.2 (Fig. 5).
Figure 5.
Mean DASH.
Group C: The group scored a mean DASH of 10.8 pre-treatment. Two months post-treatment with corticoid injection and splinting, mean DASH score lowered in statistically significant way (p<0,05) to 3.8; then increased to 5.3 at six months and 8.6 one year post-treatment.
Overall satisfaction at one year
Group P: The group totaled a mean score 8,2 in overall satisfaction.
Group C: The group totaled a mean score 6,8 in overall satisfaction.
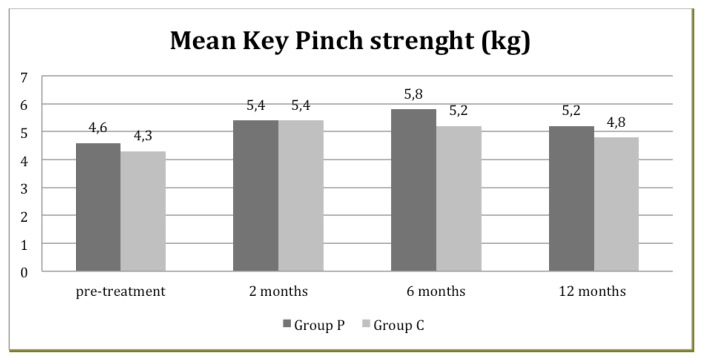
Pinch strength (Tab. II, panel C)
Group P: The group improved from a mean value of 4.6 kg to a top result of 5.8 kg at six months, to a final report of 5.2 kg at one year.
Group C: The group improved from a mean value of 4.3 kg to a top result of 5.4 kg at two months, to 4.8 kg at one year (Fig. 6).
Figure 6.
Mean Key Pinch Strenght.
Complications
Group P: No complications were recorded.
Group C: In six cases, episodes of temporary acute local pain and inflammation were recorded. They started between 1 to 6 hours after the injection and resolved spontaneously, after one-to-two days. Patients were cautioned on this possibility and were instructed to apply a cold pack over the joint when necessary.
Discussion
This study compares prospectively the benefits of physiotherapy treatment, including application of heat and kinesiotherapy, to intra- articular corticosteroid injection. The study group consists of patients with early stages of arthritis of the TMC joint (Eaton stages 1–2). Two months post-treatment, both groups showed an improvement of the considered parameters (pain, function, strength) with total remission of pain in the majority of patients (group P: 16/25; group C: 20/25). Group C patients treated with corticosteroid injection showed a statistically significant improvement (p <0.05) of DASH score compared to both pre-treatment clinical conditions and the group treated with physical therapy.
In treating OA, the benefits of treatment by intra-articular corticosteroid are already known, although Coblyn et al.22 have recently demonstrated that many steroid injections for knee OA (injections were performed several times every three months), might hasten cartilage loss. Day et al.23 reported a study on 30 patients with a mean age similar to our study group (61 years old), suffering from TMC osteoarthritis, treated with corticosteroid infiltration and temporary splinting. A remission of pain for more than 18 months was observed in 6 out of 7 cases with Eaton stage 1 and in 40% of cases with Eaton stage 2–3.
At the onset of a TMC degenerative disease and the painful symptoms that it causes, work activity factors an important role. Moreover, some occupations such as tailors, milliners, sewers, embroiderers and jobs requiring hand positions such as tip, lateral, palmar or forceful pinch causing high pressure patterns in the TMC joint are frequently associated with the development of OA in the TMC joint6.
From a functional point of view, physiotherapy treatment shows less evident results in the early stages. However, on final inspection, a significantly greater number of patients (p<0.05) in group P (10/25) showed persistence of painful symptomatology remission compared to patients in group C.
In a large systematic review of the literature Valdes and Marik16 outlined moderate evidence in scientific literature upholding the effectiveness of the application of heat, hand exercises, adaptive equipment, the use of carpometacarpal orthotics for pain relief, restoration of the joint articulation and hand function. The longer duration of time spent by the physiotherapist with the patient, and the stronger therapeutic relationship this brought about, in comparison to the joint infiltration therapy, may have improved the patients’ knowledge regarding the conditions which determine pain recurrence24,25. On this aspect, Berggreen et al.26 in a seven year prospective study, suggest patients with OA of the TMC joint should be offered access to splints preoperatively, as well as occupational therapy.
This is a first study regarding two among the many possibilities of conservative treatments available for patients with OA of TMC joint. When interpreting the data of this study, two limitations must be taken into account: the lack of knowledge regarding the work performed by the patients and the lack of a control group to distinguish the effects of the application of the orthosis from the effects of other therapies. Moreover, the continuous application of an orthosis for the reduction of painful symptoms is known to be effective.
Conclusion
The results obtained in this study suggest that both measures are effective as temporary treatments for the TMC OA. Patient satisfaction was rated good after both procedures. The goals were to provide a temporary mobility and pain-free thumb and these were achieved in both groups.
The study has therefore shown that patients treated with corticosteroid injection achieved, on average, rapid improvement of pain and strength although these results were short-lived and group C patients returned to pre-treatment levels after one year. On the other hand, patients treated by application of heat, passive and active mobilization of the arthritic joint, massage therapy and stretching experienced a more gradual improvement of symptoms. However, although these group P patients scored a final DASH similar to those treated with infiltration, their pain relief, on average, lasted longer.
References
- 1.Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis: staging as a rationale for treatment. Hand Clin. 1987;3:455–471. [PubMed] [Google Scholar]
- 2.Pellegrini D. Pathomechanics of the thumb trapeziometacarpal joint. Hand Clin. 2001;17(2):175–184. [PubMed] [Google Scholar]
- 3.Tomaino MM. Suspensionplasty for basal joint arthritis: why and how. Hand Clin. 2006;22(2):171–175. doi: 10.1016/j.hcl.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong AL, Hunter JB, Davis TRC. The prevalence of degenerative arthritis of the base of the thumb in postmenopausal women. J Hand Surg. 1994;19B:340–341. doi: 10.1016/0266-7681(94)90085-x. [DOI] [PubMed] [Google Scholar]
- 5.Bettinger PC, Linscheid RL, Cooney WP, 3rd, An KN. Trapezial tilt: a radiographic correlation with advanced trapeziometacarpal joint arthritis. J Hand Surg Am. 2001;26(4):692–697. doi: 10.1053/jhsu.2001.26187. [DOI] [PubMed] [Google Scholar]
- 6.Fontana L, Neel S, Claise JM, Ughetto S, Catilina P. Osteoarthritis of the thumb carpometacarpal joint in women and occupational risk factors: a case-control study. J Hand Surg Am. 2007;32(4):459–465. doi: 10.1016/j.jhsa.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Turker T, Thirkannad S. Trapezio-metacarpal arthritis: The price of an opposable thumb! Indian J Plast Surg. 2011;44(2):308–316. doi: 10.4103/0970-0358.85352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reyes C, Leyland KM, Peat G, Cooper C, Arden NK, Prieto-Alhambra D. Association Between Overweight and Obesity and Risk of Clinically Diagnosed Knee, Hip, and Hand Osteoarthritis: A Population-Based Cohort Study. Arthritis Rheumatol. 2016 Aug;68(8):1869–1875. doi: 10.1002/art.39707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulkarni K, Karssiens T, Kumar V, Pandit H. Obesity and osteoarthritis. Maturitas. 2016;89:22–28. doi: 10.1016/j.maturitas.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Glickel SZ. Clinical assessment of the thumb trapeziometacarpal joint. Review. Hand Clin. 2001;17(2):185–195. [PubMed] [Google Scholar]
- 11.Parvex PO, Egloff DV. Surgery for root arthrosis: retrospective study and search for an algorithm. Chir Main. 2001;20(5):351–361. doi: 10.1016/s1297-3203(01)00058-0. [DOI] [PubMed] [Google Scholar]
- 12.Rocchi L, Merolli A, Cotroneo C, Morini A, Brunelli F, Catalano F. Abductor pollicis longus hemitendon looping around the first intermetacarpal ligament as interposition following trapeziectomy: a one-year follow-up study. Orthop Trauma, Surg Res. 2011;97(7):726–733. doi: 10.1016/j.otsr.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Frizziero A, Maffulli N, Masiero S, Frizziero L. Six-months pain relief and functional recovery after intra-articular injections with hyaluronic acid (mw 500–730 KDa) in trapeziometacarpal osteoarthritis. Muscles Ligaments Tendons J. 2014 Jul 14;4(2):256–261. [PMC free article] [PubMed] [Google Scholar]
- 14.Loibl M, Lang S, Dendl LM, Nerlich M, Angele P, Gehmert S, Huber M. Leukocyte-Reduced Platelet-Rich Plasma Treatment of Basal Thumb Arthritis: A Pilot Study. Biomed Res Int. 2016;2016:9262909. doi: 10.1155/2016/9262909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colditz JC. The biomechanics of a thumb carpometacarpal immobilization splint: design and fitting. J Hand Therapy. 2000;13:228–235. doi: 10.1016/s0894-1130(00)80006-x. [DOI] [PubMed] [Google Scholar]
- 16.Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther. 2010;23(4):334–350. doi: 10.1016/j.jht.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Wolock BS, Moore R, Weiland AJ. Arthritis of the basal joint of the thumb. A critical analysis of treatment options. J Arthropl. 1989;4(1):65–78. doi: 10.1016/s0883-5403(89)80055-5. [DOI] [PubMed] [Google Scholar]
- 18.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research: 2016 update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rocchi L, Merolli A, Morini A, Monteleone G, Foti C. A modified spica-splint in postoperative early-motion management of skier’s thumb lesion: a randomized clinical trial. Eur J Phys and Rehab Med. 2014 Feb;50(1):49–57. [PubMed] [Google Scholar]
- 20.Stamm TA, Machold KP, Smolen S, Fischer S, Redlich K, Graninger W, Ebner W, Erlacher L. Joint protection and home exercises improve hand function in patients with hand osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2002;47:44–49. doi: 10.1002/art1.10246. [DOI] [PubMed] [Google Scholar]
- 21.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 22.Coblyn JS. Reviewing McAlindon TE, et al., Steroid Injections for Knee Osteoarthritis Might Hasten Cartilage Loss. JAMA. 2017 May 16;317:1967. [Google Scholar]
- 23.Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI. Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. J Hand Surg Am. 2004;29(2):247–251. doi: 10.1016/j.jhsa.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Jeffels K, Foster N. Can Aspects of Physiotherapist Communication Influence Patients’ Pain Experiences? A Systematic Review. Physical Therapy Reviews. 2003;8(4):197–210. [Google Scholar]
- 25.Klaber Moffett JA, Richardson PH. The influence of the physiotherapist-patient relationship on pain and disability. Physiother Theory Pract. 1997;13(1):89–96. [Google Scholar]
- 26.Berggreen M, Joost-Davidsson A, Lindstrand J, Nylander G, Povlsen B. Reduction in the need for operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: a seven year prospective study. Scand J Plast Reconstr Hand Surg. 2001;35:415–441. doi: 10.1080/028443101317149381. [DOI] [PubMed] [Google Scholar]