Abstract
Intrauterine hypoperfusion/ischemia is one of the major causes of intrauterine/fetal growth restriction, preterm birth, and low birth weight. Most studies of this phenomenon have been performed in either models with severe intrauterine ischemia or models with gradient degree of intrauterine hypoperfusion. No study has been performed in a model on uniform mild intrauterine hypoperfusion (MIUH). Two models have been used for studies of MIUH: a model based on suture ligation of either side of the arterial arcade formed with the uterine and ovarian arteries, and a transient model based on clipping the bilateral ovarian arteries and aorta having patency. Those two rodent models of MIUH have some limitations, e.g., not all fetuses are subjected to MIUH, depending on their position in the uterine horn. In our MIUH model, all fetuses are subjected to a comparable level of intrauterine hypoperfusion. MIUH was achieved by mild stenosis of all four arteries feeding the uterus, i.e., the bilateral uterine and ovarian arteries.
Arterial stenosis was induced by metal microcoils wrapped around the feeding arteries. Producing arterial stenosis with microcoils allowed us to control, optimize, and reproduce decreased blood flow with very little inter-animal variability and a low mortality rate, thus enabling accurate evaluation. When microcoils with an inner diameter of 0.24 mm were used, the blood flow in both the placenta and fetus was mildly decreased (approximately 30% from the pre-stenosis level in the placenta). The offspring of our MIUH model clearly demonstrates long-lasting alterations in neurological, neuroanatomical and behavioral test results.
Keywords: Neuroscience, Issue 131, Intrauterine hypoperfusion, microcoil, artery stenosis, uterine artery, ovarian artery, rat, fetus, prematurity, prenatal hypoxia-ischemia, fetal growth restriction, intrauterine growth restriction, low birth weight
Introduction
Infants with intrauterine growth restriction (IUGR) (also known as fetal growth restriction) (birth weight <10th percentile for gestational age), preterm birth (born at < 37 weeks of gestation), and/or low birth weight (< 2500 g) account for nearly 10% of all newborns 2,3. Many of these infants present with neurological problems such as cerebral palsy and developmental disorders (e.g., attention-deficit/hyperactivity disorder (ADHD) and learning disorders) 3,4,5. Those conditions have similarities and differences in their etiology and outcomes. The etiology of IUGR is multifactorial, and placental insufficiency associated with intrauterine hypoperfusion is considered to be the most common cause in non-anomalous fetuses 7. The etiology of preterm is multifactorial as well, and chorioamnionitis is the most frequent cause 8.
The influence of mild intrauterine hypoperfusion (MIUH) on the developing brain is unclear. Currently available animal models of intrauterine hypoperfusion/ischemia primarily involve either severe hypoperfusion or gradient degree of hypoperfusion with or without reperfusion 9,10,11. In clinical settings, however, cases of MIUH are considered to be far more frequent than those involving such severe conditions. The currently available models of MIUH are a rodent model involving suture ligation of either the uterine or the ovarian artery and a rodent model involving clipping the bilateral ovarian arteries and aorta having patency 12,13,14,15,16,17. One of the disadvantages of these models is the extensive inter-fetus variability, ranging from fetuses with profound hypoperfusion to fetuses with nearly intact perfusion, depending on the position of the fetus within the arterial arcade of the uterine and ovarian arteries. Another disadvantage of these models is their inability to distinguish the position of each fetus after birth; hence, researchers cannot distinguish the severity of intrauterine hypoperfusion experienced by an individual pup after its birth.
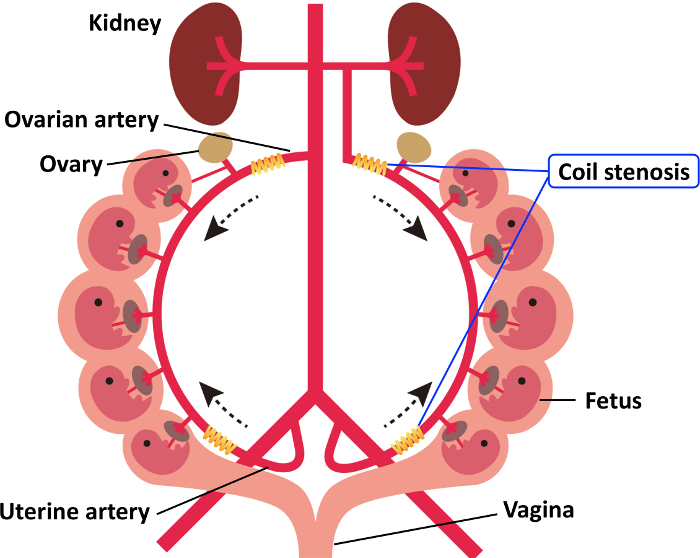
We have developed a rat model of MIUH involving multiple artery stenosis 1. Wrapping metal micro-coils with an inner diameter of 0.24 mm around the ovarian and uterine arteries causes stenosis, but not obstruction, of the blood vessels (Figure 1). Applying these microcoils at the proximal parts of all of the arteries supplying the uterus, i.e., the bilateral uterine and ovarian arteries, on embryonic day 17 (equivalent to embryonic weeks 20-25 in humans 18) induces a significant but mild decrease in blood flow to the placentas and fetuses. The decreases in blood flow after coils are applied to all four arteries feeding the uterus are largely the same across each placenta and fetus. The fetus mortality rate is less than 20%. The pups are born via spontaneous labor 1-2 days earlier (embryonic day 21-22) than normal. Almost all pups are born exhibiting significantly low birth weights 1. Gray and white matter volumes are decreased without obvious tissue damage 1. Pups present with delayed acquisition of newborn reflexes, muscle weakness, and altered spontaneous activity 1. This model mimics the clinical signs and symptoms of children born prematurely or with IUGR; children born preterm exhibit reduced gray and white matter volume with or without white matter injury 6, present delayed milestones of neurological development, and may present behavioral problems such as ADHD 3,5; children with IUGR exhibit minimal neuroanatomical alterations, and have an increased risk of impaired neurological development such as motor and cognitive delay 4,7. Preterm birth and IUGR are different conditions, but the two conditions share the basic mechanism, i.e. insults to immature brains before full-term gestational age.
Protocol
All experiments were performed in accordance with protocols approved by the Experimental Animal Care and Use Committee of the National Cerebral and Cardiovascular Center, Suita, Japan.
1. Prepare the following animals and materials for MIUH surgery
Prepare timed pregnant Sprague-Dawley rats at gestational day 17, i.e., embryonic day 17 (E17). The dams' average body weights are 307.0 ± 40.7 g (mean ± SD, n = 9).
Prepare metal microcoils; inner diameter 0.24 mm, made from gold-coated steel.
Prepare all the materials as per the Table of Materials.
2. Prepare for MIUH surgery
Warm a heating pad at 37 °C for rat placement
Place a sterile diaper on the heating pad
Warm sterile saline at 37 °C in a water bath
3. Perform MIUH surgery
Perform surgical procedures under sterile condition. Sterilize coils, forceps, needle with 70% ethanol before use. Use sterile gloves, and occasionally disinfect by applying ethanol spray.
Place the rat in the anesthesia induction box. Introduce 4% isoflurane into the box (approximately 5 min).
Place the rat onto a sterile diaper on the heating pad in a supine position after the animal is thoroughly anesthetized in the induction box. Check for depth of anesthesia by the lack of a response to a toe pinch. Maintain 1.5-2.0% isoflurane with a nose cone.
Apply depilatory foam onto the abdomen from the navel down to the region of the pelvic arch. After several minutes, wipe off the depilatory foam with a paper towel. A shaver may be used as a substitute for the depilatory foam.
Apply gauze soaked in iodine disinfectant solution to the depilated region of the skin.
Place a surgical drape with a round opening to cover the abdomen other than the area of the surgical incision. Several pieces of gauze may be used as a substitute for the drape.
Using a surgical scalpel, make an incision approximately 2.5 cm long on the lower abdomen from the upper edge of the pubic bone straight up toward the navel. Then, make an incision through the muscle layer underneath.
Place several pieces of sterile gauze around the opening of the drape, and wet the gauze with warmed saline.
Push both lateral sides of the abdomen gently, so that a portion of uterine horn emerges from the incision.
Disinfect the surgeon's hands with 70% ethanol.
Gently pull the entire uterine horn from the abdominal cavity manually without using forceps. Using surgical forceps is not advisable, as they may easily damage the fragile uterus, fetuses, and blood vessels by compressing them strongly and unevenly.
Place the uterine horn on the wet gauze.
Perform the same procedure for the other uterine horn.
Count the number of fetuses.
- Apply warmed saline frequently to keep the uterus warm and wet throughout the surgery.
- Change the diaper when it has absorbed too much saline. To maintain stability, repeat disinfection gloves with 70% ethanol and tips of the instrument with iodine. Keeping the non-sterile fingers away from the sterile tips of the instrument is crucial.
Identify the proximal part of the main arcade of the ovarian and uterine arteries under a stereomicroscope. NOTE: It is crucial to distinguish the main arcade from the branches to the placentas. Note that the surgical operation may be easier when the uterine horn is flipped. Occasionally, applying a coil at the very proximal part of the arcade is difficult, because it is located deep within the abdominal cavity and arteries to the placenta are very close to the proximal part of the arcade. In this case, a coil can be applied to a part of the arcade after the first branch forks off.
Separate the artery from the vein running parallel to it with forceps and make space between them.
Place a piece of string (silk suture 4.0, 5 cm long) underneath the artery.
Lift up both ends of the string with forceps so that the artery is lifted and separated from the fragile vein.
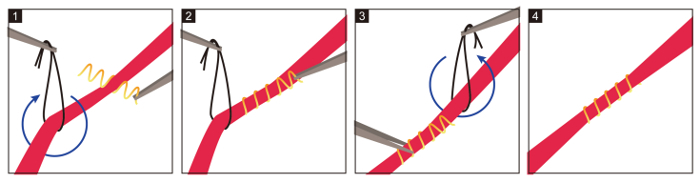
Holding the edge of the microcoil with fine forceps in the other hand, place a microcoil beside the lifted artery (Figure 2.1).
Rotate the lifted artery by using the string around the microcoil to wrap the microcoil around the artery. It is easier to rotate the artery around the coil than to rotate the coil around the artery (Figure 2.2).
After rotating the artery 3 or 4 turns (coils have 5 turns), change the site at which the coil is held to the other edge. Hold the edge of the coil that has been wrapped around the artery with forceps. Change the site at which the string lifts the artery to the other side of coil. Rotate the artery around the coil so that the coil completely (5 turns) wraps the artery (Figure 2.3, 2.4).
Remove the string.
Perform the same procedure for the other three arteries.
Note that frequently applying warmed saline to the uterus is crucial; otherwise, the mortality rate of the fetuses increases, and hypothermia might be neuroprotective.
Gently return the uterine horn into the abdominal cavity. Lifting an edge of the abdominal wall incision with forceps can make this procedure easier.
Stich the abdominal muscle, and then stich the abdominal skin with suture (silk suture 4.0). Tie the suture after each stich, i.e. interrupted single sutures.
Apply gauze soaked in iodine disinfectant solution on and around the surgical incision.
Administer the analgesic meloxicam at 0.5 mg/kg body weight subcutaneously.
Allow for 30 min of recovery in a warmed cage. Check animals if fully awake and moving around the cage, return to home cage.
Representative Results
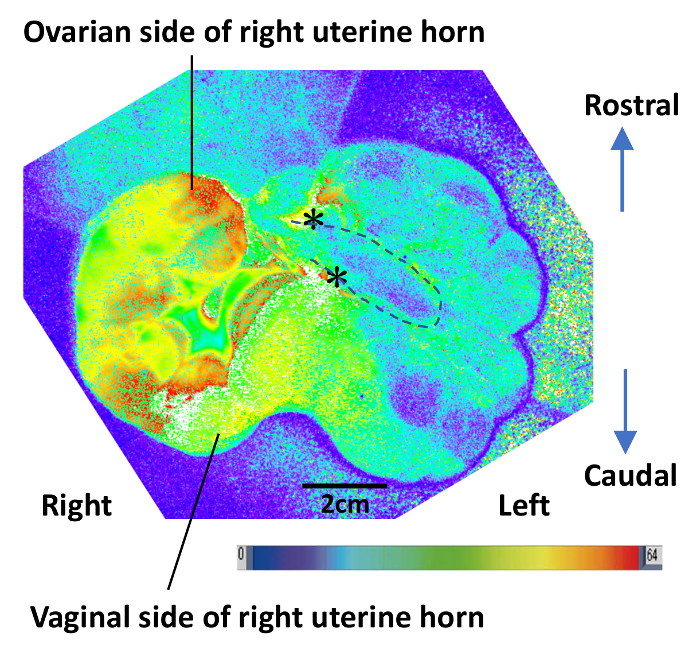
After applying microcoils to all of the arteries feeding the uterus, i.e., the bilateral uterine and ovarian arteries, all fetuses are subjected to comparable levels of hypoperfusion. The application of microcoils with an inner diameter of 0.24 mm causes mild stenosis of those arteries, thereby causing a mild decrease in blood flow to the placentas and fetuses (Figure 3; approximately 30% from the pre-stenosis level in the placenta, see reference 1 for details). Pups born from the dam demonstrate IUGR (Table 1).
The dams seem to be hypoactive during a few days after the surgery. Other than that, the dams do not present any noticeable complications, and fully recover in one week after the surgery. The dams are able to live for a long time after the delivery (mortality is 0 % for observation period), and to nurse pups. The coils remain in the same place.
Table 1. Body weights at birth (Postnatal day 0, P0) and on the day equivalent to embryonic day 29 (E29), which was P6-8. Pups in the no-surgery control group were born on E23, whereas those in the sham-surgery group were born 1 day earlier (E22); those in the mild intrauterine hypoperfusion (MIUH) group were born 1-2 days earlier (E21-22) via spontaneous labor. Therefore, E29 equivalents were P6 to P8 depending on the pup's gestational period. (n = 8-14 in each group, for each sex and each time point) *P < 0.01 vs. a no-surgery control group as well as a sham-surgery group. One-way ANOVA, followed by a Tukey-Kramer test.
Figure 1. Schema of the anatomic arterial system in the uterus. Four microcoils were installed around the arteries upstream of the bilateral ovarian and uterine arteries. The dotted arrows indicate the direction of arterial blood flow. This figure has been modified from the one in our previous publication 1. Please click here to view a larger version of this figure.
Figure 2. Illustration of the application of a coil to an artery. 1. Lift up the artery with a string. Place a microcoil beside the artery. 2. By rotating the artery around the microcoil, the microcoil is wrapped around the artery. 3. After rotating the artery 3 or 4 turns (The coil has 5 turns), change the site at which the coil is held to the other edge. Hold the edge of the coil together with the artery using forceps. Change the site at which the string lifts the artery to the other side of the coil. 4. Rotate the artery around the coil so that the coil completely (5 turns) wraps the artery. Please click here to view a larger version of this figure.
Figure 3. A representative image of a uterus produced with laser speckle flowmetry1. This image demonstrates decreased blood flow in the left uterine horn but not the right, after coil stenosis was performed in the left ovarian and uterine arteries. *: locations of coil stenosis in the arcade of the ovarian and uterine arteries; upper asterisk corresponds to the proximal part of ovarian artery, and lower one corresponds to the proximal part of uterine artery. Dotted line indicates the arcade of the ovarian and uterine arteries in the left uterine horn. Reddish color indicates more blood flow, whereas blueish color indicates less blood flow. Please click here to view a larger version of this figure.
Discussion
The microcoil stenosis of both ovarian and uterine arteries in both uterine horns produces consistent and reproducible intrauterine hypoperfusion in all placentas and fetuses. The level of hypoperfusion can be modified by using microcoils with different inner diameters. Rat pups born from a dam on which artery stenosis has been performed with microcoils 0.24 mm in inner diameter demonstrate IUGR and premature birth (see reference 1 for details). The pups exhibit neuroanatomical and behavioral alterations that resemble the signs and symptoms observed in preterm children. These neuroanatomical alterations include ventricular enlargement, thinning of the cortex and corpus callosum, and decreased brain weight but no obvious cell loss or cystic lesions 1. The behavioral alterations observed include a delayed neonatal reflex, decreased muscle strength and altered spontaneous activity 1.
To study intrauterine ischemia, animal models based on severe ischemia over a short duration with reperfusion are frequently used 10,11. When both ends of the artery arcade formed from the ovarian and uterine arteries are blocked by clipping, the blood supply to the uterine horn (including the placentas and fetuses) is completely halted. Hence, the duration of clipping must be short, or the fetuses will die. In a clinical setting, however, we speculate that prolonged mild hypoperfusion may be more frequently encountered rather than abrupt blockade of blood flow to the uterus and its complete recovery within an hour.
Rodent models involving suture ligation of one or both side(s) of the arcade of the uterine artery and those involving clipping that leaves some inner space between the bilateral ovarian arteries and the aorta have been the only available models of mild prolonged intrauterine hypoperfusion 13,14,16,19,20. These ligation and clipping models have low reproducibility, i.e., only a few fetuses survive and suffer from hypoperfusion. When the blood flow at the ovarian artery is blocked by suture ligation, the fetuses located closest to the ovary, i.e., at the top of the uterine horn, is subjected to profound ischemia, whereas the fetuses located closer to the cervix and vagina are subjected to minimal or no decreases in blood supply 12.
There are three critical steps in the protocol. Identifying the proximal portion of the main arcade of the ovarian and uterine arteries is essential. The main arterial arcade has numerous branches to the placentas. Some of these branch arteries are large in diameter, and occasionally are almost as large as the main artery. Therefore, distinguishing the main artery from among several other branching arteries can be confusing. Note that the main arterial arcade is not large in diameter. The vein running beside the arcade is several times larger in diameter than the artery. Arteries may become even narrower, owing to constriction in response to surgical stimulation. Separating the artery from the vein running alongside it is a delicate task. The adventitia of the artery is in close contact with the vein throughout most of the arcade. Be aware that the vein bleeds easily when touched by forceps. Keeping the uterus warm and wet is critical; otherwise, the dam and fetuses may suffer from stress and dehydration, and many fetuses may be lost before delivery. The limitation of this coil stenosis model technique is the long surgical duration required. A period of approximately 60 min is required to complete the surgery by applying four coils. This long surgical duration may cause additional stress to the fetuses and the dam.
We believe that the model presented in this paper is the most clinically relevant and reproducible model of MIUH. This model allows for assessment of the temporal and longitudinal impact of MIUH on IUGR.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This work was supported by the FY 2013 Research Exchange Program between JSPS and CNRS, JSPS KAKENHI Grant Number 26860858, and the Narishige Neuroscience Research Foundation. We thank Drs. Mariko Harada-Shiba and Kyoko Shioya for helpful discussions. We thank Mari Furuta, Mutsumi Sakamoto, Ritsuko Maki, and Dr. Emi Tanaka for excellent technical assistance.
References
- Ohshima M, et al. Mild intrauterine hypoperfusion reproduces neurodevelopmental disorders observed in prematurity. Sci Rep. 2016;6:39377. doi: 10.1038/srep39377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Specified Report on Vital Statistics in FY2010, Ministry of Health, Labour and Welfare, Japan. 2010. Available from: http://www.mhlw.go.jp/english/database/db-hw/FY2010/live_births.html.
- Anderson P, Doyle LW, Victorian Infant Collaborative Study G. Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. JAMA. 2003;289(24):3264–3272. doi: 10.1001/jama.289.24.3264. [DOI] [PubMed] [Google Scholar]
- Levine TA, et al. Early childhood neurodevelopment after intrauterine growth restriction: a systematic review. Pediatrics. 2015;135(1):126–141. doi: 10.1542/peds.2014-1143. [DOI] [PubMed] [Google Scholar]
- Sucksdorff M, et al. Preterm Birth and Poor Fetal Growth as Risk Factors of Attention-Deficit/ Hyperactivity Disorder. Pediatrics. 2015;136(3):e599–e608. doi: 10.1542/peds.2015-1043. [DOI] [PubMed] [Google Scholar]
- Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardozza LM, et al. Fetal growth restriction: current knowledge. Arch Gynecol Obstet. 2017;295(5):1061–1077. doi: 10.1007/s00404-017-4341-9. [DOI] [PubMed] [Google Scholar]
- Chang E. Preterm birth and the role of neuroprotection. Bmj. 2015;350:g6661. doi: 10.1136/bmj.g6661. [DOI] [PubMed] [Google Scholar]
- Coq JO, Delcour M, Massicotte VS, Baud O, Barbe MF. Prenatal ischemia deteriorates white matter, brain organization, and function: implications for prematurity and cerebral palsy. Dev Med Child Neurol. 2016;58(Suppl 4):7–11. doi: 10.1111/dmcn.13040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jantzie LL, Corbett CJ, Firl DJ, Robinson S. Postnatal Erythropoietin Mitigates Impaired Cerebral Cortical Development Following Subplate Loss from Prenatal Hypoxia-Ischemia. Cereb Cortex. 2015;25(9):2683–2695. doi: 10.1093/cercor/bhu066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubo KI, et al. Association of impaired neuronal migration with cognitive deficits in extremely preterm infants. JCI Insight. 2017;2(10) doi: 10.1172/jci.insight.88609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delcour M, et al. Mild musculoskeletal and locomotor alterations in adult rats with white matter injury following prenatal ischemia. Int J Dev Neurosci. 2011;29(6):593–607. doi: 10.1016/j.ijdevneu.2011.02.010. [DOI] [PubMed] [Google Scholar]
- Gilbert JS, Babcock SA, Granger JP. Hypertension produced by reduced uterine perfusion in pregnant rats is associated with increased soluble fms-like tyrosine kinase-1 expression. Hypertension. 2007;50(6):1142–1147. doi: 10.1161/HYPERTENSIONAHA.107.096594. [DOI] [PubMed] [Google Scholar]
- Granger JP, et al. Reduced uterine perfusion pressure (RUPP) model for studying cardiovascular-renal dysfunction in response to placental ischemia. Methods Mol Med. 2006;122:383–392. doi: 10.1385/1-59259-989-3:381. [DOI] [PubMed] [Google Scholar]
- Mazur M, Miller RH, Robinson S. Postnatal erythropoietin treatment mitigates neural cell loss after systemic prenatal hypoxic-ischemic injury. J Neurosurg Pediatr. 2010;6(3):206–221. doi: 10.3171/2010.5.PEDS1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivier P, Baud O, Evrard P, Gressens P, Verney C. Prenatal ischemia and white matter damage in rats. J Neuropathol Exp Neurol. 2005;64(11):998–1006. doi: 10.1097/01.jnen.0000187052.81889.57. [DOI] [PubMed] [Google Scholar]
- Robinson S, et al. Developmental changes induced by graded prenatal systemic hypoxic-ischemic insults in rats. Neurobiol Dis. 2005;18(3):568–581. doi: 10.1016/j.nbd.2004.10.024. [DOI] [PubMed] [Google Scholar]
- Rice D, Barone S., Jr Critical periods of vulnerability for the developing nervous system: evidence from humans and animal models. Environ Health Perspect. 2000;108(Suppl 3):511–533. doi: 10.1289/ehp.00108s3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basilious A, Yager J, Fehlings MG. Neurological outcomes of animal models of uterine artery ligation and relevance to human intrauterine growth restriction: a systematic review. Dev Med Child Neurol. 2015;57(5):420–430. doi: 10.1111/dmcn.12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delcour M, et al. Neuroanatomical, sensorimotor and cognitive deficits in adult rats with white matter injury following prenatal ischemia. Brain Pathol. 2012;22(1):1–16. doi: 10.1111/j.1750-3639.2011.00504.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


