Abstract
Background
Despite substantial evidence demonstrating clear benefit, rates of preemptive kidney transplantation (PreKTx) remain low in the United States. Our goal was to identify barriers to PreKTx.
Methods
Using a telephone-administered questionnaire including questions about barriers, timing of referral, timing of education, we retrospectively studied first living donor kidney transplant recipients (2006-2010) at Mayo Clinic, Rochester, MN. Of 235 patients, 145 (62%) responded to the questionnaire (74 PreKTx and 71 non-PreKTx). We compared categorical data with Fisher exact test and median times with Wilcoxon rank sum test.
Results
Polycystic kidney disease (PCKD), longer median time between diagnosis and transplant, and time between education about transplant and transplant correlated with PreKTx (P < 0.01). The presence of at least 1 patient-identified barrier (lack of referral, financial barriers, medical barriers, no identified living donor and donor evaluation delays) was associated with non-PreKTx (0.034) though no single barrier predominated. Age, education level, insurance status and source of referral (primary care, nephrology, and nonphysician referral) were not associated with the rate of PreKTx. Univariate logistic regression identified white race, PCKD, and increased time from diagnosis as factors favoring PreKTx; PCKD and increased time remained significant factors after multivariate analysis.
Conclusions
Even among a patient population that is primarily white, educated, and has a spouse or first-degree relative donor, PreKTx rates remain concerningly low. Increased time between diagnosis or education and transplant are predictors of PreKTx. Greater emphasis on transplant education earlier in the stages of chronic kidney disease and community outreach from transplant centers may help to increase the rate of PreKTx.
Preemptive kidney transplant (PreKTx) has been recognized to have a variety of advantages over transplantation after a course of maintenance dialysis therapy, including fewer pretransplant blood transfusions,1 increased rates of patients continuing employment,2 improved long-term graft survival,3 lower rates of delayed graft function,3,4 and fewer episodes of acute rejection.3 Despite these recognized benefits, the utilization of PreKTx remains low with reported rates between 9% and 21% of all patients.5,6 Preemptive kidney transplant also bears benefits to society as a whole through decreased healthcare expenditures. United States Renal Data System 2011 data indicate Medicare and private payer expenses for dialysis are over US $60 000 and US $125 000 per year, respectively,7 not including costs of dialysis access placement which range from US $7000 to US $19 000.8,9 Although kidney transplantation has relatively high initial costs associated with induction immunosuppression and the initial hospitalization, maintenance immunosuppression costs range between US $18 000 and US $23 000 annually.10,11
With clear clinical and economic advantages favoring kidney transplantation over dialysis, it is unclear why PreKTx rates remain low. A Web survey of 460 nephrologists found that 71% of respondents preferred PreKTx as the optimal therapy for end-stage renal disease; however, 81% of those eligible for PreKTx were too ill to avoid dialysis. Additionally, 69% felt patients were referred to nephrology care at an advanced stage of their disease.12 Prior studies have also emphasized the importance of early patient education by providers as a means of increasing rates of PreKTx.13 Indeed, focused interventions consisting of specialized chronic kidney disease clinics have been able to increase the number of eligible patients referred for transplant, including a large number of preemptive referrals.14 However, few studies have asked patients themselves about their perceived barriers to achieving PreKTx. The goal of the current study was to identify patient-perceived barriers to the maximal utilization of PreKTx.
MATERIALS AND METHODS
We retrospectively queried our prospectively maintained transplant database at Mayo Clinic, Rochester to identify recipients of living donor kidney transplants who were not recipients of any prior transplant. We identified 235 recipients of first living donor kidney transplants from 2006 to 2010. We developed a survey that included demographic data, such as education level and source of insurance, but also questions that addressed possible barriers to receiving a PreKTx like timing of transplant referral, relationship to the living donor, and possible medical delays to transplant (Figure 1). This Institutional Review Board-approved survey was administered via telephone after verbal consent was obtained. Health Insurance Portability and Accountability Act forms were collected via postal mail. The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the “Declaration of Istanbul on Organ Trafficking and Transplant Tourism.” Patients who responded to the survey were grouped according to their status as preemptive or non-preemptive. The reported median times are calculated as the number of days between the transplant date and the patient's self-reported date of being diagnosed with kidney disease, being educated about kidney transplant, or being referred to a transplant center. Demographics and characteristics between the 2 groups were compared with Fisher exact test for categorical data and Wilcoxon rank sum test for median times. Univariate and multivariate logistic regression analyses were performed to assess the factors associated with PreKTx. Odds ratios (OR) with 95% confidence intervals (CI) are reported. All analyses were performed with STATA software (version 11.2, College Station, TX).
FIGURE 1.
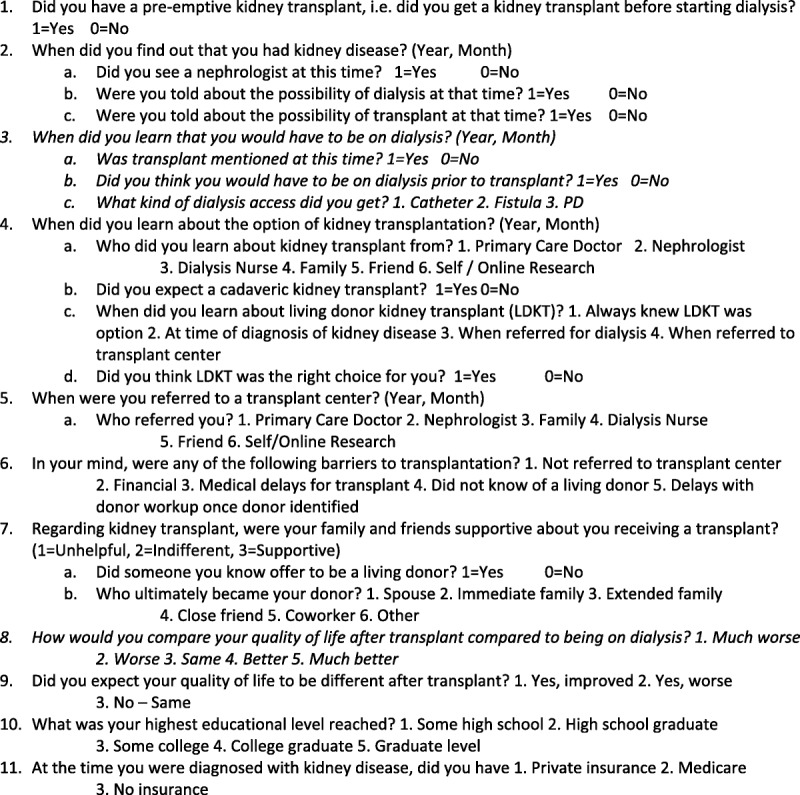
Phone questionnaire administered to recipients of living donor kidney transplants. Questions in italics were asked of recipients who had not undergone PreKTx, that is, were on dialysis.
RESULTS
Of 235 first time recipients of a living donor kidney transplant between 2006 and 2010, 208 (89%) patients were alive at follow-up. Of this group, 186 (79%) patients were contacted, and 145 (62%) patients participated in the study. Among the participants, 71 patients received a PreKTx, whereas 74 received non-PreKTx. The demographics of these 2 groups are shown in Table 1. The most prevalent diagnoses for each group are listed. The “other” category includes amyloidosis, chemotherapy-induced nephritis, Wegener granulomatosis, Goodpasture syndrome, lupus nephritis, hemolytic uremic syndrome, and 10 patients for whom a primary diagnosis was not recorded at the time of transplant.
TABLE 1.
Demographics and baseline characteristics of kidney transplant recipients
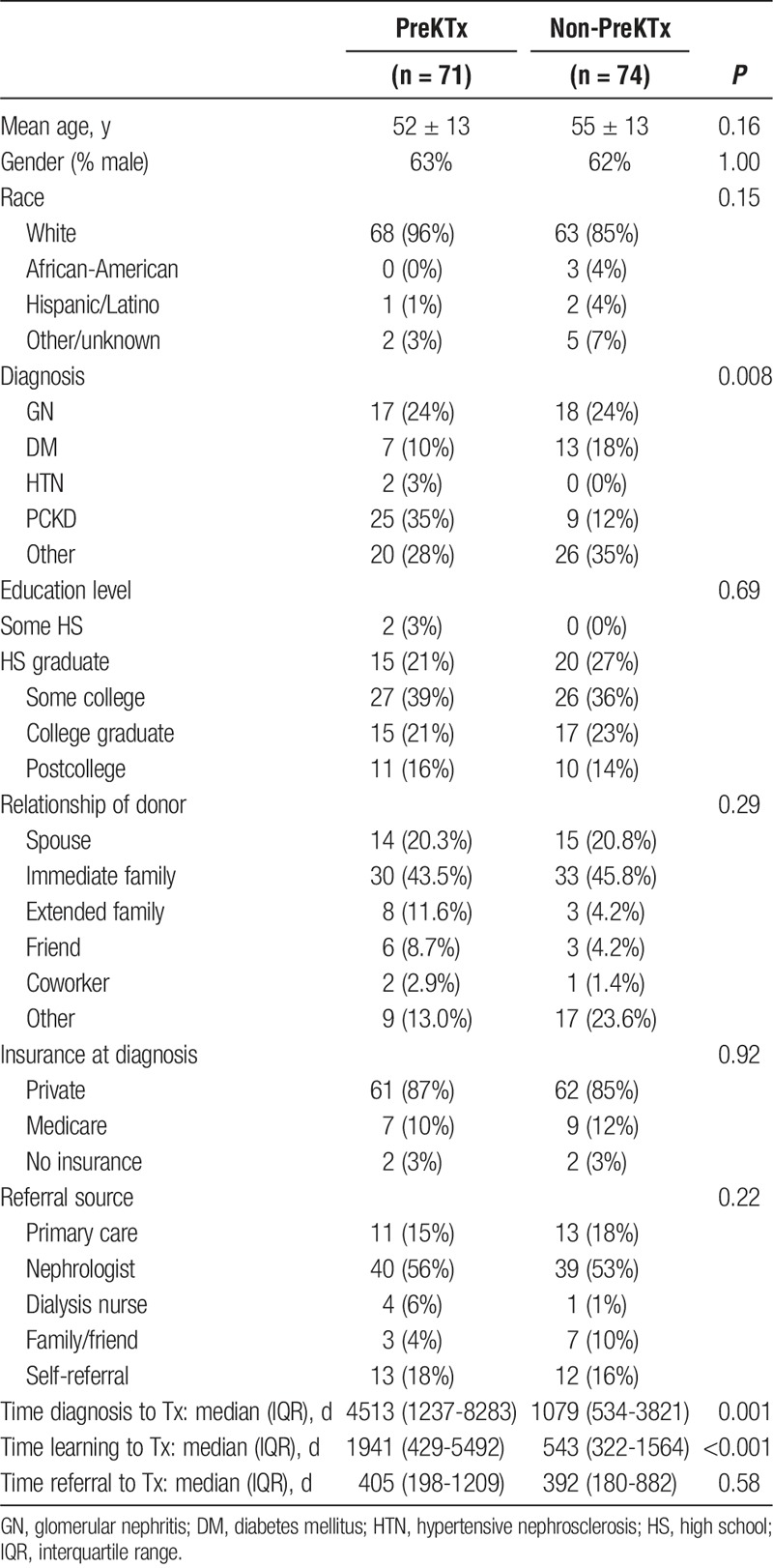
The PreKTx and non-PreKTx populations were of similar composition with respect to sex, race, educational level and insurance status. The overall population was largely white with a higher proportion in the PreKTx cohort (PreKTx 96% vs non-PreKTx 85%, P = 0.046). There was no difference with regard to source of referral to transplant, with the majority of referrals to a transplant center coming from nephrologists (PreKTx 56% vs non-PreKTx 53%, P = 0.93). There was a significant difference between PreKTx and non-PreKTx populations with respect to their diagnosis, primarily because such a large number of patients with polycystic kidney disease (PCKD) received a PreKTx (PreKTx 35% vs non-PreKTx 12%, P = 0.001).
There was a significant difference between the PreKTx and non-PreKTx populations with respect to the median time from renal disease diagnosis and transplant (PreKTx 4513 days vs non-PreKTx 1079 days, P = 0.001). Similarly, there was a significant difference between the median time from learning about kidney transplantation and undergoing transplant (1941 days vs 1543 days, P = 0.0001). The median time between referral to a transplant center and transplantation was not significantly different between the PreKTx and non-PreKTx groups (405 days vs 392 days, P = 0.58). The interval times to transplant are not normally distributed, and the times are graphically represented in Figure 2. Interquartile ranges are available in Table 1. Ironically, almost all patients knew that they had renal disease at least 3 years before undergoing renal replacement in both groups.
FIGURE 2.
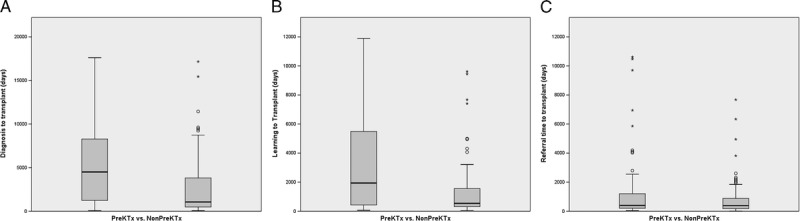
Elapsed time between events and transplantation for PreKTx and non-PreKTx populations. A, The time between diagnosis of renal disease and transplant. B, The time between education about kidney transplantation and transplant. C, The time between referral to a transplant center and transplantation.
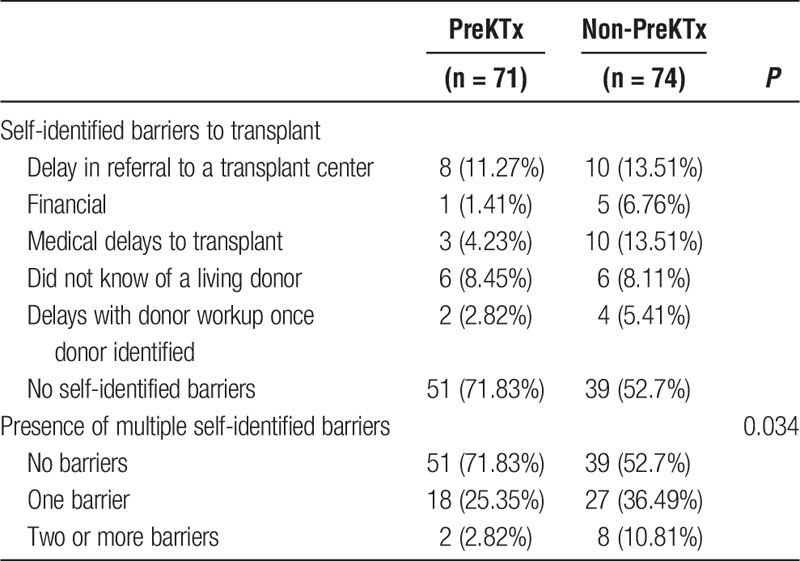
A patient's self-identified barriers to transplant were also not significantly different between the PreKTx and non-PreKTx populations (Table 2). However, the presence of multiple self-identified barriers to transplant did show significance, with increasing barriers to transplant reducing the number of patients able to undergo PreKTx (P = 0.034).
TABLE 2.
Self-identified barriers to transplant
The relationship between the recipient and donor was also not significantly different between PreKTx and non-PreKTx populations (Table 1). The donor category “immediate family” includes a parent/child or sibling relationship, whereas “extended family” includes aunts/uncles, cousins, or in-law relationships. The donor category “other” includes nondirected donors and donors who were assigned as part of a kidney paired donation scenario.
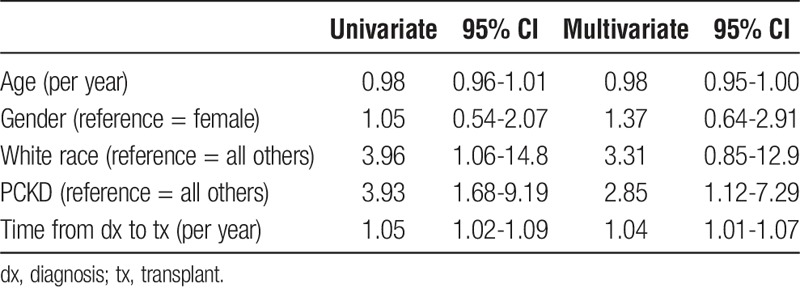
Univariate analysis of the cohort demonstrates a likelihood for PreKTx among whites (OR, 3.96; 95% CI, 1.06-14.8), patients with PCKD (OR, 3.93; 95% CI, 1.68-9.19), and patients diagnosed with renal disease earlier relative to their transplant date (OR, 1.05; 95% CI, 1.02-1.09). When these factors were included in our multivariate logistic regression model, white race was no longer significant although these patients were still over 3 times more likely to undergo PreKTx than nonwhite counterparts. PCKD (OR, 2.85; 95% CI, 1.12-7.29) and a longer time from diagnosis of renal disease (OR, 1.04; 95% CI, 1.01-1.07) remained significant predictors of PreKTx on multivariate analysis (Table 3). Educational status and source of insurance were not found to be significant factors.
TABLE 3.
Univariate and multivariate ORs for PreKTx
DISCUSSION
There has been a lack of research directed at patient-perceived barriers to PreKTx. Our study addresses this critical gap by surveying kidney transplant recipients about their self-perceived barriers to PreKTx. The results show that recipients of PreKTx were more likely to have PCKD and were more likely to have a longer time between kidney disease diagnosis or education about transplantation and the date of transplant. Being referred by a nephrologist versus other type of healthcare provider did not affect the rate of PreKTx. Similarly, educational level and insurance status did not affect the rate of PreKTx. Knight and colleagues13 also reported the importance of patient education to achieve PreKTx, though their data also emphasized referral by a transplant nephrologist. In the current study, individual self-identified barriers to transplantation did not adversely affect the rate of PreKTx, but the presence of multiple self-identified barriers was more strongly associated with non-PreKTx. Our finding that half of the non-PreKTx patients did not identify a barrier to transplant was surprising and could reflect an expectation among patients and providers that dialysis should precede renal transplantation.
Kutner et al15 examined United States Renal Data System survey responses to determine factors associated with preemptive listing for kidney transplant, a prerequisite for PreKTx. Their work determined that two thirds of patients who were preemptively waitlisted received nephrology care more than 12 months before starting dialysis. Patients were 3 times more likely to be preemptively listed when kidney transplant was discussed more than 12 months before starting dialysis. Kutner et al also found that higher hemoglobin and albumin levels were significantly associated with preemptive listing (P < 0.0001), which may reflect closer follow-up or improved access to healthcare.
A study by Weng and Mange16 found that increasing length of time under the care of a nephrologist and having a spouse as a potential living donor were both associated with higher odds of preemptive evaluation. However, the relationship between our donors and recipients was similar between the PreKTx and non-PreKTx groups. A notable finding is that over 70% of both groups ultimately had a living donor who was either a spouse or an immediate or extended family member. This fact is important because the vast majority of our living donor recipients knew their donor for years prior to the transplant—in other words, they did not have to search far and wide for a donor or endure long wait times for a deceased donor kidney.
There are several limitations to the current study. Our sample size was not large enough to perform multivariate survival analysis. Our center performs a high percentage of living donor KTx and a large proportion of PreKTx, and our patient population may not be representative of a national sample. Because most of our recipients were white, this may limit the applicability to other transplant centers. Although PCKD remained a significant predictor of PreKTx on multivariate analysis, it is plausible that PCKD is associated with some other factor which was not accounted for on our survey. Perhaps those with PCKD have families who have previously been transplanted, accounting for earlier education, or the slow progression of PCKD to end-stage renal disease allows for more lead time in the transplant workup. This survey was administered between 4 to 8 years after transplantation, and patients may have had recall bias or difficulty remembering specific dates or details regarding their pretransplant care, and the times to transplant are patient reported and not controlled for based on patient characteristics. Lastly, because this survey focused on a multiple-choice response for patient-perceived barriers to transplantation, recipients may not have responded with their most significant perceived barrier.
The findings of this study suggest that the majority of patient-identified barriers to PreKTx are outside of the direct influence of transplant centers. Although transplant centers should continue to focus on performing efficient evaluations of transplant candidates and potential donors, we would submit that earlier, more timely education regarding the advantages of living donor transplantation and PreKTx will be necessary to increase rates of PreKTx. Transplant centers need to take a more active leadership role in their communities to educate care providers regarding early referral for kidney transplantation. The fact that almost all the recipients in this study learned they had kidney disease 3 years before transplantation suggests that there was sufficient time to prepare for transplantation. This further emphasizes the potential benefits of more vigorous education regarding PreKTx, as demonstrated in small studies.17 To increase the rate of PreKTx, we conclude that changes are needed in national polices to encourage early referral to transplant centers before referral to dialysis and ensure early education of patients and potential donors.
Footnotes
Published online 20 March, 2018.
The authors declare no funding or conflicts of interest.
R.A.H. participated in research design, drafting of the article, performance of the research, data analysis and critical review and revision. C.L.J. participated in data analysis and critical review and revision. B.A.P. participated in performance of the research and critical review and revision. P.G.D. participated in research design and writing of the paper and critical review and revision. M.D.S. participated in research design and writing of the paper and critical review and revision.
REFERENCES
- 1.John AG, Rao M, Jacob CK. Preemptive live-related renal transplantation. Transplantation. 1998;66:204–209. [DOI] [PubMed] [Google Scholar]
- 2.Abou Ayache R, Bridoux F, Pessione F, et al. Preemptive renal transplantation in adults. Transplant Proc. 2005;37:2817–2818. [DOI] [PubMed] [Google Scholar]
- 3.Malho A, Malheiro J, Fonseca I, et al. Advantages of kidney transplant precocity in graft long-term survival. Transplant Proc. 2012;44:2344–2347. [DOI] [PubMed] [Google Scholar]
- 4.Friedewald JJ, Reese PP. The kidney-first initiative: what is the current status of preemptive transplantation? Adv Chronic Kidney Dis. 2012;19:252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grams ME, Chen BP, Coresh J, et al. Preemptive deceased donor kidney transplantation: considerations of equity and utility. Clin J Am Soc Nephrol CJASN. 2013;8:575–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jay CL, Washburn K, Dean PG, et al. Survival benefit in older patients associated with earlier transplant with high KDPI kidneys. Transplantation. 2017;101:867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Renal Data System, USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States 2013., authors [Google Scholar]
- 8.Rosas SE, Feldman HI. Synthetic vascular hemodialysis access vs native arteriovenous fistula: a cost-utility analysis. Ann Surg. 2012;255:181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu FX, Ghaffari A, Dhatt H, et al. Economic evaluation of urgent-start peritoneal dialysis versus urgent-start hemodialysis in the United States. Medicine (Baltimore). 2014;93:e293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnieh L, Yilmaz S, McLaughlin K, et al. The cost of kidney transplant over time. Prog Transplant. 2014;24:257–262. [DOI] [PubMed] [Google Scholar]
- 11.Tanriover B, Stone PW, Mohan S, et al. Future of Medicare immunosuppressive drug coverage for kidney transplant recipients in the United States. Clin J Am Soc Nephrol. 2013;8:1258–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pradel FG, Jain R, Mullins CD, et al. A survey of nephrologists' views on preemptive transplantation. Clin J Am Soc Nephrol CJASN. 2008;3:1837–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knight RJ, Teeter LD, Graviss EA, et al. Barriers to preemptive renal transplantation: a single center questionnaire study. Transplantation. 2015;99:576–579. [DOI] [PubMed] [Google Scholar]
- 14.Khosla N, Gordon E, Nishi L, et al. Impact of a chronic kidney disease clinic on preemptive kidney transplantation and transplant wait times. Prog Transplant. 2010;20:216–220. [DOI] [PubMed] [Google Scholar]
- 15.Kutner NG, Zhang R, Huang Y, et al. Impact of race on predialysis discussions and kidney transplant preemptive wait-listing. Am J Nephrol. 2012;35:305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weng FL, Mange KC. A comparison of persons who present for preemptive and nonpreemptive kidney transplantation. Am J Kidney Dis. 2003;42:1050–1057. [DOI] [PubMed] [Google Scholar]
- 17.Boulware LE, Hill-Briggs F, Kraus ES, et al. Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Di. 2013;61:476–486. [DOI] [PMC free article] [PubMed] [Google Scholar]


