Abstract
Introduction
Empirical work has documented a robust and consistent relation between panic attacks and smoking behavior. Theoretical models posit smokers with panic attacks may rely on smoking to help them manage chronically elevated negative affect due to uncomfortable bodily states, which may explain higher levels of nicotine dependence and quit problems.
Methods
The current study examined the effects of panic attack history on nicotine dependence, perceived barriers for quitting, smoking inflexibility when emotionally distressed, and expired carbon monoxide among 461 treatment-seeking smokers. A multiple mediator path model was evaluated to examine the indirect effects of negative affect and negative affect reduction motives as mediators of the panic attack-smoking relations.
Results
Panic attack history was indirectly related to greater levels of nicotine dependence (b=0.039, CI95%=0.008, 0.097), perceived barriers to smoking cessation (b=0.195, CI95%=0.043, 0.479), smoking inflexibility/avoidance when emotionally distressed (b=0.188, CI95%=0.041, 0.445), and higher levels of expired carbon monoxide (b=0.071, CI95%=0.010, 0.230) through the sequential effects of negative affect and negative affect smoking motives.
Conclusions
The present results provide empirical support for the sequential mediating role of negative affect and smoking motives for negative affect reduction in the relation between panic attacks and a variety of smoking variables in treatment-seeking smokers. These mediating variables are likely important processes to address in smoking cessation treatment, especially in panic-vulnerable smokers.
Keywords: Negative affect, negative-reinforcement, panic attacks, smoking, tobacco
Introduction
Panic attacks have been defined as a subjective sense of extreme fear or impending doom accompanied by a massive autonomic surge and strong flight-or-fight action tendency (1). Panic attacks can either be situationally triggered and isolated or perceived as spontaneous and recurrent in nature; the latter is the hallmark characteristic of panic disorder, which can occur with or without situational avoidance (i.e. agoraphobia) (2). Approximately 28% of the general United States population experiences panic attacks at some point in their lifetime, with 23% experiencing panic attacks without ever meeting criteria for panic disorder and/or agoraphobia (3). That is, panic attacks can occur outside the context of panic psychopathology. In fact, panic attacks are common in various other psychological disorders including posttraumatic stress disorder, generalized anxiety disorder, social anxiety disorder, depression, and various substance use disorders (2) and a large body of research suggests that panic attack histories ‘mark’ risk for multiple forms of psychopathology (4-6).
In addition to panic attacks being a relatively common phenomenon (3), empirical evidence suggests that panic attacks co-occur with smoking at rates that exceed those found in the general non-psychiatric population (7-9). In the National Comorbidity Survey, current smoking rates among adults with a history of panic attacks were significantly greater than those reported among respondents with no mental illness and quit rates were significantly lower (10). Other work suggests smokers with panic attacks, compared to those without, are more likely to report greater levels of nicotine dependence and smoking to regulate affective states (11,12), less self-efficacy for remaining abstinent (13), and experience greater pre-quit negative affect and withdrawal symptoms (11,14). Additionally, in a large-scale treatment trial, smokers with a history of panic attacks, compared to smokers with no anxiety psychopathology, were less likely to be abstinent at eight weeks and six months post-quit day (11).
Given the established relation between panic attacks and smoking, a growing body of literature has aimed as explicating the processes underlying these relations (15). For example, anxiety sensitivity (AS; extent to which anxiety and anxiety-related sensations are perceived as harmful (16)) is an individual difference factor that predisposes individuals to the development and maintenance of anxiety psychopathology (17) and has been linked to various smoking processes (see overview; 18). Two additional factors that have consistently been implicated as possible explanatory processes in this context are (i) state/trait levels of negative affect (i.e. non-specific general distress; 19,20) and (ii) smoking motivated at reducing negative affect (21). Models of negative-reinforcement drug use (21,22), in conjunction with panic-smoking comorbidity models (18,23), suggest that smoking may be used as a coping strategy for managing aversive internal bodily states as an attempt to temporarily ameliorate affective distress. In line with this perspective, panic attacks are predictive of coping-oriented smoking motivation (24) and coping motives mediate the relation between anxious arousal symptoms (core symptomatic feature of panic attacks) and increased smoking rate among treatment-seeking smokers (25). Such data suggest that smokers with panic attacks may rely on smoking to manage negative affect states, which may, at least partially, account for a greater severity of nicotine dependence, the inflexible reliance on smoking when emotionally distressed, greater perceived difficulties in quitting, and levels of expired carbon monoxide (a biochemical index of smoking rate).
Together, the overarching aim of the present study was to provide an empirical test of the effect of negative affect and negative affect-management smoking motives in regard to the effect of panic attack history on nicotine dependence, barriers to smoking cessation, smoking-based inflexibility/avoidance, and a biochemical index of smoking; see Figure 1). Specifically, among treatment-seeking smokers, panic attacks were evaluated in relation to (i) nicotine dependence, (ii) perceived barriers for quitting smoking, (iii) and smoking-related inflexibility/avoidance when emotionally distressed (i.e. the tendency to respond inflexibly or with avoidance by smoking in response to difficult thoughts, feelings, and sensations), and (iv) expired carbon monoxide (CO). In line with theoretical models of anxiety and smoking comorbidity (17), it was hypothesized that a history of panic attacks may impact smoking by first increased negative affect followed by increased negative reinforcement-based smoking motivation; that is, the indirect effects of the proposed mechanisms (negative affect and smoking motives) are theorized to sequential impact smoking processes. These effects were expected to be evident above and beyond the variance accounted for by gender, age, marital status, alcohol and cannabis use, depressive symptomology and tobaccorelated medical problems; factors often related to both smoking and panic attacks (9,17,26).
Figure 1.
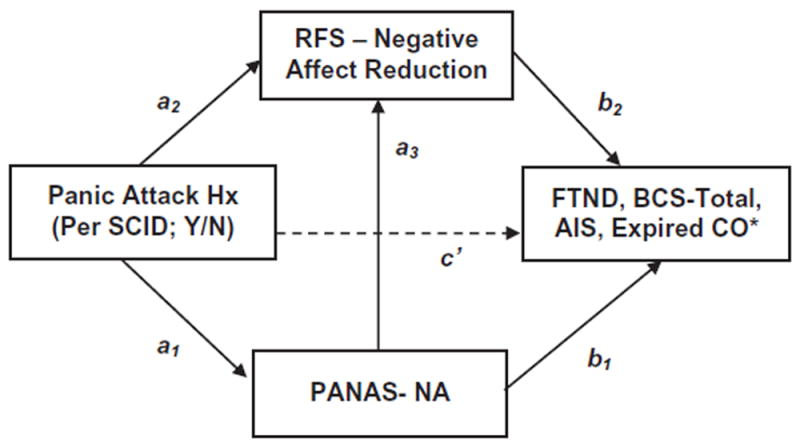
Conceptual path model for the effect of panic attack history on nicotine dependence, barriers to smoking cessation, smoking-based inflexibility/avoidance, and expired carbon monoxide. *Four separate models were conducted for each criterion outcome; a1 and a2=Specific indirect effects of X on M1 and M2; a3=Specific indirect effect of M1 on M2; b1 and b2=Specific indirect effects of M1 and M2 on Yi; c0 =Direct effect of X on Yi controlling for M1 and M2; a1*b1 and a2*b2=Specific indirect effects of M1 and M2; a1*a3*b2=Conditional indirect effect of M1 and M2; Hx=history. Panic Attack Hx: Any history of panic attacks (coded 0=no, 1=yes) as assessed by the SCID-I/NP; PANAS-NA: Positive and Negative Affect Scale-Negative Affect subscale; RFSNegative Affect Reduction=Reasons for Smoking Scale-Negative Affect Reduction subscale; FTND=Fagerström Test of Nicotine Dependence; BCS-Total=Barriers to Smoking Cessation scale; AIS=Avoidance and Inflexibility Scale; Expired CO=Expired carbon monoxide breath sample.
Methods
Participants
Participants (n=461) were adult daily smokers (Mage=36.7, SD=13.58; 48.6% female). For sample characteristics, please see Table 1. Regarding smoking history, the average daily smoking rate of this sample was 16.6 (SD=9.95), and on average, participants reported daily smoking for 18.4 years (SD=13.35). Moderate levels of nicotine dependence were reported among the sample per the Fagerström Test for Nicotine Dependence (M=5.2, SD=2.30) and baseline expired carbon monoxide averaged 19.1 ppm (SD=11.81). Of the sample, 47.7% (n=220) met criteria for a lifetime history of panic attacks: 49.1% reported having only cued panic attacks, 48.2% reported uncued panic attacks, and 2.7% (n=6) had missing information about cued/uncued panic attacks. Additionally, 44.1% met criteria for at least one current psychiatric disorder, and specifically, 5.5% met criteria for panic disorder (with or without agoraphobia).1
Table 1.
Descriptive statistics of sample characteristics
| Descriptive summary | Total n = 461 | Males n = 237 | Females n = 224 | χ2 or t |
|---|---|---|---|---|
| Age M (SD) | 36.7 (13.58) | 35.5 (13.55) | 37.9 (13.53) | −1.918 |
| Racial background n (%) | 1.829 | |||
| White | 396 (85.9) | 205 (86.5) | 191 (85.3) | |
| Black | 358 (8.3) | 21 (8.8) | 17 (7.5) | |
| Hispanic/Latino | 11 (2.4) | 4 (1.7) | 7 (3.1) | |
| Asian | 5 (1.1) | 2 (0.8) | 3 (1.3) | |
| More than one race | 11 (2.4) | 5 (2.1) | 6 (2.7) | |
| Marital status n (%) | 15.562** | |||
| Never married | 202 (43.8) | 121 (51.1) | 81 (36.2) | |
| Married/cohabitating | 154 (33.4) | 69 (29.1) | 85 (37.9) | |
| Divorced | 78 (16.9) | 39 (16.5) | 39 (17.4) | |
| Separated | 18 (3.9) | 7 (3.0) | 11 (4.9) | |
| Widowed | 9 (2.0) | 1 (0.4) | 8 (3.6) | |
| Education | ||||
| At least part college n (%) | 342 (74.2) | 176 (74.3) | 166 (74.1) | 0.001 |
| Smoking history M (SD) | ||||
| Cigarettes per day | 16.6 (9.95) | 17.8 (11.17) | 15.4 (8.30) | 2.627** |
| Age of first use | 17.4 (3.78) | 17.6 (3.84) | 17.2 (3.71) | 1.297 |
| Psychiatric disorders n (%) | ||||
| No disorder | 257 (55.9) | 150 (63.3) | 107 (48.0) | 37.26 |
| Major depressive disorder | 19 (4.1) | 11 (4.6) | 8 (3.8) | |
| Dysthymic disorder | 9 (2.0) | 3 (1.3) | 6 (2.7) | |
| Bipolar I/II | 2 (0.4) | 2 (0.6) | 0 (0) | |
| Depressive disorder NOS | 2 (0.4) | 1 (0.4) | 1 (0.4) | |
| Alcohol use disorder | 20 (4.4) | 13 (5.5) | 7 (3.1) | |
| Cannabis use disorder | 14 (3.0) | 9 (3.8) | 5 (2.2) | |
| Other SUDs | 4 (0.8) | 1 (0.4) | 3 (1.2) | |
| Panic disorder w/wo Agor. | 10 (1.9) | 5 (2.1) | 5 (2.2) | |
| Agoraphobia | 1 (0.2) | 1 (0.4) | 0 (0) | |
| Social phobia | 48 (10.4) | 19 (8.0) | 29 (13.0) | |
| Specific phobia | 19 (4.2) | 8 (3.3) | 11 (4.8) | |
| OCD | 5 (1.1) | 2 (0.8) | 3 (1.3) | |
| PTSD | 13 (2.8) | 5 (2.1) | 8 (3.6) | |
| GAD | 23 (5.0) | 5 (2.1) | 18 (8.1) | |
| Anxiety disorder NOS | 7 (1.5) | 1 (0.4) | 6 (2.7) | |
| Other | 7 (1.5) | 1 (0.4) | 6 (2.6) | |
| Key study variables | Total | Males | Females | χ2 or t |
|
| ||||
| Panic attack history n (%) | 220 (47.7) | 92 (38.8) | 128 (57.1) | 15.499** |
| Medical problems n (%) | 138 (29.9) | 72 (30.4) | 66 (29.5) | 0.046 |
| Cannabis use/30 days n (%) | 256 (55.5) | 139 (58.6) | 117 (52.2) | 1.921 |
| AUDIT total score M (SD) | 6.2 (6.02) | 6.8 (5.84) | 5.5 (6.15) | 2.398* |
| IDAS-Depression M (SD) | 41.0 (13.12) | 39.5 (11.82) | 42.6 (14.22) | −2.541* |
| PANAS-NA M (SD) | 19.1 (7.08) | 18.2 (6.49) | 20.1 (7.62) | −2.962** |
| RFS-NA M (SD) | 3.5 (0.81) | 3.3 (0.78) | 3.7 (0.76) | −5.815** |
| FTND M (SD) | 5.2 (2.29) | 5.2 (2.31) | 5.1 (2.27) | 0.232 |
| BCS-Total M (SD) | 25.0 (11.03) | 22.6 (10.42) | 27.5 (11.11) | −4.899** |
| AIS M (SD) | 45.0 (10.75) | 43.2 (10.83) | 47.0 (10.32) | −3.929** |
| Expired CO at baseline | 19.1 (11.81) | 19.9 (11.50) | 18.6 (12.14) | 1.165 |
p<.05
p<.01
Measures
Demographics Questionnaire
A demographics questionnaire was used to assess age, marital status, and race/ethnicity.
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/NP)
The SCID-I [Non-Patient Version; (27)] was used to assess past year DSM-IV-TR Axis I disorders. Interviews were administered by trained research assistants or doctoral level staff and supervised by independent doctoral-level professionals. All cases were checked by two independent raters for diagnostic accuracy; no cases of diagnostic disagreement were found. History of panic attacks was assessed using the panic disorder section of the SCID-I/NP. Two clinician-rated items were used to indicate a history of panic attacks: (1) “Have you ever had a panic attack, when you suddenly felt frightened, or anxious or suddenly developed a lot of physical symptoms?”; and (2) “Have these attacks ever come on completely out of the blue – in situations where you didn’t expect to be nervous or uncomfortable?” A dichotomous variable was created to reflect those who endorsed either item (n=220; coded=1, positive history of panic attacks). All other participants served as the non-panic attack reference group (n=241; coded=0); this variable was the predictor in all analyses.
Smoking History Questionnaire (SHQ)
The SHQ (28) is a self-report questionnaire that was used to describe the sample in terms of daily smoking rate and number of years smoking.
Alcohol Use Disorders Identification Test (AUDIT)
The AUDIT (29) is a 10-item self-report measure developed to identify individuals with problematic drinking. Total scores range from 0–30, with higher scores reflecting more hazardous drinking. The psychometric properties are well documented (29). The AUDIT total score was used as a covariate in all analyses; internal consistency was good (Cronbach’s α=0.84).
Marijuana Smoking History Questionnaire (MSHQ)
The MSHQ (30) is a 40-item measure that assesses cannabis use history and patterns of use. One item was used in the current study to determine status of cannabis use in the past 30 days: “Please rate your marijuana use in the past 30 days” (Responses range from 0=No use, 4=Once a week, to 8=More than once a day). This itemwas dichotomously coded to reflect a cannabis use status variable (0=No use; 1=Past 30-day use), which was entered as a covariate in all analyses.
Inventory of Depression and Anxiety Symptoms (IDAS)
The IDAS (31) is a 64-item self-report measure of symptoms of major depression and anxiety disorders. Respondents are asked to rate the degree to which they have experienced symptoms in the past two weeks, scored on a 5-point Likert-type scale (1=“not at all” to 5=“extremely”). This measure yields a global General Depression score, and 11 specific anxiety and depression-relevant subscales. The General depression subscale (20 items; possible range 20–100) was used as a covariate in all analyses. The IDAS has strong psychometric properties, including internal consistency and test-retest reliability, and convergent and discriminant validity (31). Internal consistency for the General Depression subscale in the current study was excellent (α=0.89).
Medical history checklist
A medical history checklist was used compute a composite variable as an index of tobacco-related medical problems, which in the current study was entered as a covariate in all models. Items in which participants indicated having ever been diagnosed (heart problems, hypertension respiratory disease and asthma; all coded 0=no, 1=yes) were summed and a total score was created (observed range from 0–3), with greater scores reflecting the occurrence of multiple markers of tobacco-related disease.
Positive and Negative Affect Scale (PANAS)
The PANAS (32) is a self-report measure that requires participants to rate the extent to which they experience each of 20 different feelings and emotions (e.g. nervous, interested) based on a Likert scale that ranges from 1 (“Very slightly or not at all”) to 5 (“Extremely”). The measure yields two factors, negative and positive affect, and has strong documented psychometric properties (32). The negative affectivity subscale was used in the present study as the first mediator variable (M1); internal consistency was excellent (Cronbach’s α=0.90).
Reasons for Smoking (RFS)
The RFS (33) is a 23-item self-report measure that assesses motivations for smoking. Participants are asked to rate their tendency to smoke in each of the circumstances listed, rated on a 5-point Likert scale (1=never to 5=always). The psychometric properties of this scale, including measures of factor structure, internal consistency, and test-retest reliability, are well established (34). In the present study, the negative affect reduction subscale (RFS-NA; e.g. “When I feel uncomfortable or upset about something, I light up a cigarette”) was used as the second mediator variable (M2); internal consistency for the RFS-NA subscale was good (Cronbach’s α=0.89).
Fagerström Test for Nicotine Dependence (FTND)
The FTND (35) is a 6-item scale that assesses gradations in tobacco dependence. Scores range from 0–10, with higher scores reflecting high levels of physiological dependence on nicotine. The FTND has adequate internal consistency, positive relations with key smoking variables (e.g. saliva cotinine), and high test-retest reliability (35,36). Internal consistency in the current study was acceptable (Cronbach’s α=0.64). The FTND total score was used as a criterion variable in the present analyses (Y1).
Barriers to Cessation Scale (BCS)
The BCS (37) is a self-report assessment of perceived barriers, or specific stressors, associated with quitting smoking. The BCS is a 19-item measure on which respondents indicate, on a 4-point Likert scale (0=Not a barrier or not applicable to 3=Large barrier), the degree to which they identify with each listed barriers (e.g. “Weight gain”, “Friends encouraging you to smoke”, “Fear of failing to quit”). Scores are summed and a total score is derived. The BCS has strong psychometric properties, including concurrent and predictive validity, internal consistency, and reliability (37). The BCS total score was used as a criterion variable in the present study (Y2; Cronbach’s α=0.89).
Acceptance and Inflexibility Scale (AIS)
The AIS (38) is a 13-item self-reported measured that assesses the link between internal (affective) triggers and smoking. Instructions ask the respondents to consider how they respond to difficult thoughts that encourage smoking (e.g. “I need a cigarette”), different feelings that encourage smoking (e.g. stress, fatigue, boredom), and bodily sensations that encourage smoking (e.g. “physical cravings or withdrawal symptoms”). Example items include “How likely is it you will smoke in response to [thoughts/feelings/sensations]?”, “How important is getting rid of [thoughts/feelings/sensations]?”, and “To what degree must you reduce how often you have these [thoughts/feelings/sensations] in order not to smoke?”. Items are rated on a 5-point Likert scale (1=Not at all to 5=Very much), with higher scores reflecting more inflexibility/avoidance in the presence of difficult thoughts, feelings and sensations. The AIS has displayed good reliability and validity in pastwork (38,39). The AIS total scorewas used as a criterion variable in the present study (Y3); internal consistency was excellent (Cronbach’s α=0.93).
Carbon monoxide
Biochemical verification of smoking status was completed by carbon monoxide (CO) analysis of breath samples. Expired air CO levels were assessed using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.). Baseline CO breath samples were used a criterion variable in the current study (Y4), as a complimentary index of smoking behavior.
Procedure
Participants were daily smokers who responded to community-based advertisements (e.g. flyers, newspaper ads, radio announcements) to participate in a larger study examining the efficacy of two smoking cessation interventions: a novel 4-session smoking cessation behavioral intervention that focused on vulnerability to panic (Panic-Smoking Program), and a standard smoking cessation program. Participants were recruited at two sites (University of Vermont and Florida State University); the study procedures have been described elsewhere (24). Due to the nature of the parent study, participants were recruited by flyers indicating a study for smoking-based anxiety-reduction program. The current study is based on secondary analyses of a sub-sample of people who provided data during the study’s baseline assessment session, which took place prior to the commencement of the intervention. Cases with available data on all examined variables were included in the present sample. After providing written informed consent, participants were interviewed using the SCID-I/NP and completed a computerized self-report assessment battery as well as biochemical verification of smoking status. All participants provided informed consent and the study protocol was approved by the Institutional Review Boards at both universities.
Data analytic strategy
The present data have not been previously reported. Analyses were conducted in PASW Statistics 21.0 (IBM SPSS Inc.). First, zero-order correlations among predictor (panic attack history [X]), proposed mediators (PANAS-NA [M1] and RFSNA [M2], and criterion variables (FTND [Y1], BCS [Y2], AIS [Y3], and expired CO [Y4]) were examined. Next, a serial multiple mediator model was conducted to examine the impact of RFS-NA through PANAS-NA as mediators of the relation between panic attack history (X) and the criterion variables (FTND, BCS, AIS, expired CO). This analytic approach allows for examination of two mediators, in a causal or sequential fashion, while simultaneously testing the indirect effects of each mediator independently (40). That is, the model estimates each specific indirect effect (a1*b1 and a2*b2); however, in order to test for sequential mediation effects, the indirect effect of path a1*a3*b2 was also estimated and tested for statistical significance. Gender, age, marital status, alcohol use (per AUDIT), past 30-day cannabis use status (per MSHQ), tobacco-related medical problems, and depressive symptoms (per IDAS-General Depression scale) were included as covariates in all models. Analyses were conducted using PROCESS, a conditional process modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (40). The 95-percentile confidence intervals (CI) for R2 indices were obtained analytically; the CIs for the specific and conditional indirect effects were estimated with bootstrap analyses (10 000 resamples; as recommended, 41-43).
Results
Zero-order correlations
Bivariate associations between study variables are presented in Table 2. Panic attacks were significantly associated with female gender, past 30-day cannabis use, depressive symptoms, negative affectivity, negative affect reduction smoking motives, and perceived barriers for smoking cessation. Descriptively, independent sample t-test revealed that those smokers with a history of panic attacks, relative to those without, reported greater depressive symptoms, greater general negative affect, more negative-reduction smoking motives, and greater perceived barriers to quitting smoking (all p’s<0.05). Those smokers with a panic attack history were rated as having an overall lower GAF score (Global Assessment of Functioning), relative to those with no panic attack history (M=70.7, SD=10.94 versus M=75.8, SD=10.61; t=4.551, p<0.0001). Additionally, both mediator variables were significantly inter-correlated, and all criterion variables were significantly related with the exception of BCS and expired CO; correlations were low to moderate in strength. Male gender was also significantly associated with higher AUDIT scores, whereas female gender was related to higher scores on the IDAS-Depression, PANAS-NA, RFS-NA, BCS, and AIS.
Table 2.
Correlations for predictor, mediating, and criterion variables.
| Variable | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gendera | 0.087 | −0.113* | −0.062 | 0.001 | 0.118* | 0.181** | 0.139** | 0.265** | −0.015 | 0.224** | 0.181** | −0.056 |
| 2. Agea | 1 | −0.309** | −0.243** | 0.235** | −0.154** | −0.017 | −0.189** | −0.077 | 0.320** | −0.080 | 0.143** | 0.361** |
| 3. AUDIT Totala | 1 | 0.190** | −0.116* | 0.237** | 0.043 | 0.246** | 0.088 | −0.111* | 0.090 | 0.032 | −0.160** | |
| 4. Cannabis usea | 1 | 0.042 | 0.039 | 0.106* | 0.072 | −0.015 | −0.063 | −0.003 | −0.070 | −0.088 | ||
| 5. Medical problemsa | 1 | −0.016 | 0.039 | 0.009 | −0.074 | −0.021 | 0.001 | 0.056 | 0.041 | |||
| 6. IDAS-Depressiona | 1 | 0.281** | 0.741** | 0.388** | 0.088 | 0.381** | 0.311** | −0.026 | ||||
| 7. PA historyb | 1 | 0.321** | 0.143** | −0.046 | 0.150** | 0.074 | −0.021 | |||||
| 8. PANAS-NAc | 1 | 0.375** | 0.051 | 0.368** | 0.242** | −0.068 | ||||||
| 9. RFS-NAc | 1 | 0.360** | 0.543** | 0.485** | 0.098* | |||||||
| 10. FTNDd | 1 | 0.194** | 0.254** | 0.404** | ||||||||
| 11. BCSd | 1 | 0.580** | 0.041 | |||||||||
| 12. AISd | 1 | 0.116* | ||||||||||
| 13. Expired COd,e | 1 |
p<0.05;
p<0.01;
Covariates;
Predictor;
Mediators;
Criterion variables;
Available data for this variable is 237 (23 missing cases).
Gender =Gender coded 0 =male, 1 =female; Age =per demographics form; AUDIT Total =Alcohol Use Disorders Identification Test; Cannabis use =Past 30 days cannabis use status per the Marijuana Smoking History Questionnaire (MSHQ); Medical problems =Tobacco-related medical problems coded from a Medical History Checklist (count 0–4); IDAS-Depression =Inventory of Depression and Anxiety Symptoms-General Depression Subscale (IDAS); PA History =Panic Attack History per the Structured Clinical Interview of DSM-IV Disorders (SCID-I); PANAS-NA =Positive and Negative Affect Scale – Negative Affect subscale; RFS-NA =Reasons for Smoking scale =Negative affect reduction subscale; FTND =Fagerström Test for Nicotine Dependence – total score; BCS =Barriers to Cessation Scale – Total score; AIS =Acceptance and Inflexibility Scale – Total score; Expired CO =Expired carbon monoxide breath sample. Columns numbers 2–13 correspond to the variables numbers in the left column.
Mediation analyses
Four path models were constructed in order to test the impact of panic attack history on each criterion variable, through negative affect (M1) and negative affect reduction smoking motives (M2).2 Regression weights for paths a, b, c, and c0 are presented in Table 3 for each of the four models. The estimates of the specific and conditional indirect effects were the paths tested for mediation, which are presented in Table 4.
Table 3.
Regression results for three mediation models.
| Y | Path | b | SE | T |
|---|---|---|---|---|
| FTND | a1 | 1.617 | 0.461 | 3.511** |
| a2 | −0.026 | 0.072 | −0.361 | |
| a3 | 0.020 | 0.007 | 2.785** | |
| b1 | −0.001 | 0.020 | −0.027 | |
| b2 | 1.213 | 0.129 | 9.419** | |
| c′ | −0.372 | 0.195 | −1.903 | |
| c | −0.357 | 0.211 | −1.695 | |
| BCSa | b1 | 0.134 | 0.092 | 1.452 |
| b2 | 6.012 | 0.598 | 10.054** | |
| c′ | 0.168 | 0.909 | 0.185 | |
| c | 0.425 | 0.997 | 0.426 | |
| AISa | b1 | −0.043 | 0.093 | −0.459 |
| b2 | 5.794 | 0.601 | 9.642** | |
| c′ | −0.795 | 0.913 | −0.870 | |
| c | −0.825 | 0.988 | −0.835 | |
| COb | a1 | 1.668 | 0.471 | 3.540** |
| a2 | −0.030 | 0.073 | −0.407 | |
| a3 | 0.018 | 0.007 | 2.432* | |
| b1 | −0.067 | 0.113 | −0.593 | |
| b2 | 2.373 | 0.736 | 3.222** | |
| c′ | −0.121 | 1.109 | −0.110 | |
| c | −0.232 | 1.103 | −0.211 |
p<0.05;
p<0.01.
Paths a1, a2, and a3 do not change across criterion outcomes 1–3 (n =461). To eliminate redundancy, these paths are only presented for Model 1.
Paths a1, a2, and a3 are presented for criterion outcome 4 separately because of the smaller sample size for these analyses (n =237). Note: FTND (Nicotine dependence; Y1), BCS (Barriers to Smoking Cessation total score; Y2), AIS (Affective inflexibility; Y3), and CO (Expired carbon monoxide; Y4).
Table 4.
Bootstrap estimates of the standard errors and 95% confidence intervals for the indirect effects.
| Indirect effects | b | SE | CI (lower) | CI (upper) |
|---|---|---|---|---|
| Model 1: FTND | ||||
| PANIC → PANAS →FTND (a1*b1) | −0.001 | 0.031 | −0.061 | 0.065 |
| PANIC → RFS-NA →FTND (a2*b2) | −0.023 | 0.085 | −0.199 | 0.136 |
| PANIC → PANAS → RFS-NA → FTND (a1*a3*b2) | 0.039 | 0.022 | 0.008 | 0.097 |
| Model 2: BCS | ||||
| PANIC → PANAS → BCS (a1*b1) | 0.257 | 0.443 | −0.613 | 10.147 |
| PANIC → RFS-NA → BCS (a2*b2) | −0.156 | 0.421 | −10.001 | 0.662 |
| PANIC → PANAS → RFS-NA → BCS (a1*a3*b2) | 0.195 | 0.105 | 0.043 | 0.479 |
| Model 3: AIS | ||||
| PANIC → PANAS → AIS (a1*b1) | −0.030 | 0.417 | −0.866 | 0.770 |
| PANIC → RFS-NA → AIS (a2*b2) | −0.150 | 0.400 | −0.947 | 0.630 |
| PANIC → PANAS → RFS-NA → AIS (a1*a3*b2) | 0.188 | 0.099 | 0.041 | 0.445 |
| Model 4: CO | ||||
| PANIC → PANAS → CO (a1*b1) | −0.111 | 0.272 | −0.721 | 0.367 |
| PANIC → RFS-NA → CO (a2*b2) | −0.070 | 0.181 | −0.497 | 0.240 |
| PANIC → PANAS → RFS-NA → CO (a1*a3*b2) | 0.071 | 0.050 | 0.010 | 0.230 |
Models 1–3 (n = 461); Models 4 (n = 437).
PANIC (Panic attack history; 0 =no, 1 = yes) is the independent variable (X), PANAS (PANAS-Negative Affect; M1) and RFS-NA (RFS-Negative Affect Reduction subscale; M2) are the mediators, and FTND (Nicotine dependence; Y1), BCS (Barriers to Smoking Cessation total score; Y2), AIS (Affective inflexibility; Y3), and CO (Expired CO breath sample; Y4) are the outcomes. a1*b1 and a2*b2 = Specific indirect effects of M1 and M2; a1*a3*b2 = Conditional indirect effect of M1 and M2. The 95% CIs for indirect effects were obtained by bootstrapping with 10 000 resamples. CI (lower) = lower bound of a 95% confidence interval; CI (upper) =upper bound; → =affects.
In the first analysis (Y1=FTND), both the total effect model , df=8, 452, F=10.330, p<0.0001) and the full model with the mediators , df=10, 450, F=18.889, p<0.0001) were significant, however the specific total effect of panic attack history on FTND (path c) and the direct effect of panic attack history in relation to FTND, controlling for the mediators (path c′) were nonsignificant. In the full model, male gender (b= −0.738, t= −3.813, p=0.0002), being older in age (b=0.059, t=7.223, p<0.0001) and having fewer tobacco-related medical problems (b= −0.321, t= −2.109, p=0.036) were significant covariates. Regarding the test of the indirect (mediational) effects (as shown in Table 4, Model 1), a history of panic attacks was predictive of greater levels of nicotine dependence indirectly through the sequential effect of negative affect and negative affect reduction smoking motives (effect a1*a3*b2), but not indirectly through either specific mediator alone (effects a1*b1 or a2*b2).
In the second analysis, (Y2=BCS), both the total effect model , df=8, 452, F = 12.587 p<0.0001) and the full model with mediators , df = 10, 450, F = 23.331, p<0.0001) accounted for a significant amount of variance. The specific total effect or direct effect of panic attack history on BCS was non-significant. In the full model, female gender (b=1.801, t=1.999, p=0.046) and greater level of depressive symptoms (b=0.110, t=2.253, p=0.025) were significant covariates. Regarding the test of the indirect effects (Table 4, Model 2), a history of panic attacks was predictive of greater perceived barriers to smoking cessation indirectly through the sequential effects of negative affect and negative affect reduction smoking motives (effect a1*a3*b2), but not through either mediator alone.
Third, the total effects model accounted for significant variance in AIS (Y3; , df=8, 452, F=10.298, p<0.0001); however, the specific total effect of panic attack history on AIS was non-significant. The full model with the mediators predicted significant variance in AIS , df=10, 450, F=19.270, p<0.0001) yet there was a non-significant direct effect of panic attack history on AIS controlling for the mediators. In the full model, being older in age (b=0.155, t=4.055, p=0.0001) and greater level of depressive symptoms (b=0.159, t=3.235, p=0.001) were significant covariates. To test mediation, the indirect effects were estimated (see Table 4, Model 3); a history of panic attacks was predictive of greater levels of smoking-based inflexibility/avoidance when emotionally distressed indirectly through negative affect and negative affect reduction smoking motives (effect a1*a3*b2), but not indirectly through either specific mediator alone.
Fourth, panic attack history was tested in terms of expired CO (n=237, due to missing expired CO data). The total effects model accounted for significant variance in expired CO (Y4; , df=8, 428, F=10.709, p<0.0001); however, the specific total effect was panic attack history on expired CO was non-significant. The full model with the mediators predicted significant variance in expired CO , df=10, 426, F=9.779, p<0.0001); yet, there was a non-significant direct effect of panic attack history in regard to expired CO controlling for the mediators. In the full model, male gender (b= −3.390, t= −3.088, p=0.002), being older in age (b=0.265, t=5.655, p<0.0001), and being married/cohabitating (b= −1.008, t= −2.948, p=0.003) were significant covariates. To test mediation, the indirect effects were estimated (see Table 4, Model 4); a history of panic attacks was predictive of greater expired CO levels indirectly through the sequential effect of negative affect and negative affect reduction smoking motives (effect a1*a3*b2), but not indirectly through either specific mediator alone.
Specificity analyses
Despite the theoretically-driven model guiding the research questions, as a method of further strengthening the interpretation, alternative mediation models were tested by reversing the two proposed mediators. Tests of the indirect effects were estimated based on 10 000 bootstrapped re-samples. Results of the alternative path models were non-significant when RFS-NA was entered as M1 and PANAS-NA was entered as M2 for nicotine dependence (b=0.001, CI95%= −0.003, 0.002), barriers to smoking cessation (b=0.001, CI95%=− 0.014, 0.032), smoking-related inflexibility/avoidance (b= −0.001, CI95%= −0.019, 0.009), and expired CO (b=0.001, CI95%= −0.017, 0.016).
Discussion
The present study provided an empirical test as to whether panic attack history is related to various smoking processes indirectly via the sequential effects of negative affect and negative affect reduction smoking motives. First, there was no observed direct effect of panic attacks on the smoking-relevant variables. However, findings suggested that among adult daily smokers, a history of panic attacks was predictive of greater levels of nicotine dependence, greater perceived barriers to smoking cessation, greater inflexibility/avoidance in the presence of distressing thoughts, feeling, sensations related to smoking, and greater expired CO values; and that these effects were observed only indirectly through the sequential effects of greater levels of negative affect followed by greater negative affect reduction smoking motives. Notably, the indirect effects of negative affect or coping motives alone were not predictive of any of the examined smoking variables. Additionally, the specificity analyses further support these findings: the sequential effect of negative affect reduction smoking motives and negative affect (a reversed meditational effect) did not indirectly explain the panic attack-smoking relations for any of the tested criterion variables.
This set of findings suggests that for daily cigarette smokers with a history of panic attacks, those with higher levels of negative affect are more vulnerable to copingoriented smoking motivation, which may, in part, account for greater reliance on smoking. Specifically, smoking reliance was indexed by higher levels of nicotine dependence, greater perceived barriers to smoking cessation, greater inflexibility/avoidance in the presence of smoking-related distress, and higher levels of expired CO.
Together, the present findings have a number of implications for smoking cessation assessment and treatment. First, given we found that smokers with a history of panic attacks report both greater levels of general negative affect and negative affect reduction motivations for smoking, this particular group of smokers may benefit from tailored smoking cessation interventions. Such interventions would ideally (a) teach skills to manage panic attack symptoms and general negative emotional states (e.g. aggression, low mood, irritability) and (b) target maladaptive beliefs about the effects of smoking (44). For example, a tailored treatment plan may include the combination of (1) psychoeduction about the cyclical nature of smoking-anxiety, (2) panic-specific interventions (e.g. interoceptive exposure), (3) general negative affect management techniques (e.g. relaxation, behavioral activation), and (4) standard cognitive restructuring to address maladaptive beliefs/motives for smoking (44).
Second, greater physiological dependence on nicotine and higher smoking rates (verified through levels of expired CO) are associated with greater reliance on smoking and poorer cessation success (45). Thus, for this group of smokers, the use of pharmacological intervention (e.g. nicotine replacement therapy, varenicline) may be particularly important for smoking cessation success (46). Additionally, emerging research suggests that use of a personal CO monitor to provide regular biochemical feedback may assist in smoking cessation (47).
Third, based on the research suggesting perceived barriers to cessation are highly predictive of poorer cessation outcomes (37), smoking cessation interventions for these vulnerable smokers may be bolstered by assessing perceived barriers to quitting, challenging maladaptive cognitions regarding these perceived barriers, and the developing problem-solving skills to cope with actual barriers. Moreover, the tendency to inflexibly seek out opportunities to escape, avoid, or reduce distressing states through smoking is conceptualized as a smoking-specific form of experiential avoidance (48). For such vulnerable smokers, it appears that it may be important to enhance “psychological flexibility” related to smoking (49) through use of acceptance-based techniques (e.g. experiential awareness, openness, willingness, mindfulness, cognitive diffusion) (50).
Although not the primary aim of the current study, it is noteworthy that there were several significant covariates across statistical models, namely, gender differences, being older in age, and greater depressive symptoms being predictive of the smoking indices. These findings are consistent with non-panic specific research suggesting that while males are more likely to be heavy smokers (51), female smokers appear to be more vulnerable to negative affect during periods of smoking deprivation (52). Additionally, a history of depression is associated with the experience of nicotine withdrawal symptoms, specifically among women (51). Older smokers are also more likely to be heavier smokers, although may be particularly motivated to quit smoking when also experiencing high levels of distress (53). The current findings further underscore the importance of comprehensive individual difference models in understanding the nature of panic attacks and smoking comorbidity (18,26).
There are limitations of the present model that are worth considering when interpreting the existing findings. First, the data utilized here were cross-sectional in design, which limits the ability to establish causal relations between the tested variables; however, by sequentially modeling the mediator variables (the effect of M1 is tested as occurring prior to M2), we attempted to examine temporal associations (40). Additionally, data were unavailable on the onset of panic attacks among participants in the sample. Thus, is it unknown whether smoking temporally preceded panic attack onset. The current study also relied solely on self-report measures to assess the examined mediator variables. Given that acute nicotine withdrawal can impact subjective reporting of affect (54), it is important to consider the recency of cigarette use relative to when assessment of state affect is conducted. The present findings could be meaningfully further extended through multi-method laboratory/experimental studies or prospective tests of these relations to further strengthen the present findings. For example, experimental provocation procedures such as emotion elicitation via biological challenge could be useful in examining the present relations in response to aversive interoceptive states elicited in real time.
Second, panic attack history was used as the predictor in the current study. Therefore, the results may not necessarily generalize to smokers with panic disorder. It is worth noting though that we tested the sample model among participants reporting only spontaneous panic attacks (as seen in panic disorder) compared to all others and found an identical pattern of results (footnote 2); however, it would be important to test this same model among a sample of smokers with panic disorder.
Third, the sample consisted of community-recruited, treatment-seeking daily cigarette smokers with moderate levels of nicotine dependence. Future studies may benefit by sampling from lighter and heavier smoking populations to ensure the generalizability of the results to the general smoking population. It is also noteworthy that the internal consistency for the FTND was relatively low, a problem that frequently occurs with this measure (55). However, Cronbach alpha values are fairly sensitive to the number of items in each scale and it is not uncommon to find lower Cronbach values with shorter scales (e.g. scales with <10 items; 56). Finally, the sample was largely comprised of a relatively homogenous group of treatment-seeking smokers. To rule out selection bias and increase the generalizability of these findings, it will be important for future studies to recruit a more ethnically/racially diverse sample of smokers.
Overall, the present findings empirically document the importance of negative affect and smoking for negative affect reduction in accounting for the relations between panic attacks and smoking. When considered in the larger context of other research (e.g. 11), the present findings suggest that there may be a need for specialized smoking cessation interventions for smokers with panic attacks (44).
Acknowledgments
This work was supported by a National Institute of Mental Health grant awarded to Drs Michael J. Zvolensky and Norman B. Schmidt (R01-MH076629-01A1). Ms. Farris is supported by a cancer prevention fellowship through the University of Texas MD Anderson Cancer Center funded by the National Cancer Institute (R25T-CA057730), and a predoctoral National Research Service Award from the National Institute of Drug Abuse (F31-DA035564-01). The content does not necessarily represent the official views of the National Institutes of Health. Please note that the funding sources had no other role other than financial support.
Footnotes
Rates of lifetime panic attack history were reported higher in the current sample (47.7%) relative to other community estimations [38.1%; (10)]. The current sample of community daily smokers rates of panic attacks. The rates of current (past year) Axis I psychopathology in the current sample are consistent with community-based estimations (10).
The regression models were conducted with a more conservative panic attack history variable that was coded to include those with recurrent and uncued panic attacks (=1) and all others (=0). An identical pattern of results emerged with panic attack history predicting all four criterion variables indirectly through the sequential effects of PANAS-NA and RFS-NA (effects a1*a3*b2). Full results are available upon request from the corresponding author.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper. This study was not supported by grant funds.
References
- 1.Barlow DH, Brown TA, Craske MG. Definitions of panic attacks and panic disorder in the DSM-IV: implications for research. J Abnorm Psychol. 1984;103:553–564. doi: 10.1037//0021-843x.103.3.553. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.Kessler R, Chiu W, Jin R, Ruscio A, Shear K, Walters E. The epidemiology of panic attacks, panic disorder, and agoraphobia in the national comorbidity survey replication. Arch Gen Psychiat. 2006;63:415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baillie A, Rapee R. Panic attacks as risk markers for mental disorders. Soc Psych Psych Epid. 2005;40:240–244. doi: 10.1007/s00127-005-0892-3. [DOI] [PubMed] [Google Scholar]
- 5.Goodwin R, Hamilton S. Panic attack as a marker of core psychopathological processes. Psychopathology. 2001;34:278–288. doi: 10.1159/000049326. [DOI] [PubMed] [Google Scholar]
- 6.Batelaan N, Rhebergen D, de Graaf R, Spijker J, Beekman A, Penninx B. Panic attacks as a dimension of psychopathology: evidence for associations with onset and course of mental disorders and level of functioning. J Clin Psychiat. 2012;73:1195–1202. doi: 10.4088/JCP.12m07743. [DOI] [PubMed] [Google Scholar]
- 7.Breslau N, Klein D. Smoking and panic attacks: an epidemiologic investigation. Arch Gen Psychiat. 1999;56:1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin R, Hamilton S. The early-onset fearful panic attack as a predictor of severe psychopathology. Psychiat Res. 2002;109:71–79. doi: 10.1016/s0165-1781(01)00357-2. [DOI] [PubMed] [Google Scholar]
- 9.Mathew AR, Norton PJ, Zvolensky MJ, Buckner JD, Smits JJ. Smoking behavior and alcohol consumption in individuals with panic attacks. J Cog Psych. 2011;25:61–70. doi: 10.1891/0889-8391.25.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lasser K, Boyd J, Woolhandler S, Himmelstein D, McCormick D, Bor D. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 11.Piper M, Cook J, Schlam T, Jorenby D, Baker T. Anxiety diagnoses in smokers seeking cessation treatment: relations with tobacco dependence, withdrawal, outcome and response to treatment. Addiction. 2011;106:418–427. doi: 10.1111/j.1360-0443.2010.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vujanovic A, Marshall E, Gibson L, Zvolensky M. Cognitiveaffective characteristics of smokers with and without posttraumatic stress disorder and panic psychopathology. Addict Behav. 2010;35:419–425. doi: 10.1016/j.addbeh.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zvolensky M, Lejuez C, Kahler C, Brown R. Nonclinical panic attack history and smoking cessation: an initial examination. Addict Behav. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Marshall E, Johnson K, Bergman J, Gibson L, Zvolensky M. Anxiety sensitivity and panic reactivity to bodily sensations: relation to quit-day (acute) nicotine withdrawal symptom severity among daily smokers making a self-guided quit attempt. Exp Clin Psychopharm. 2009;17:356–364. doi: 10.1037/a0016883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kassel JD, Veilleux JC. Introduction: the complex interplay between substance abuse and emotion. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 3–12. [Google Scholar]
- 16.Reiss S, Peterson R, Gursky D, McNally R. Anxiety sensitivity, anxiety frequency and the predictions of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 17.McNally RJ. Anxiety sensitivity and panic disorder. Biol Psychiat. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- 18.Zvolensky M, Bernstein A. Cigarette smoking and panic psychopathology. Curr Dir Psychol Sci. 2005;14:301–305. [Google Scholar]
- 19.Brown T, Chorpita B, Barlow D. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 20.Clark L, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 21.Baker T, Piper M, McCarthy D, Majeskie M, Fiore M. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy D, Curtin J, Piper M, Baker T. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. Negative reinforcement: possible clinical implications of an integrative model; pp. 15–42. [Google Scholar]
- 23.Zvolensky M, Schmidt N, Stewart S. Panic disorder and smoking. Clin Psychol Sci Pr. 2003;10:29–51. [Google Scholar]
- 24.Johnson K, Farris S, Schmidt N, Smits J, Zvolensky M. Panic attack history and anxiety sensitivity in relation to cognitive-based smoking processes among treatment-seeking daily smokers. Nicotine Tob Res. 2013;15:1–10. doi: 10.1093/ntr/ntr332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson K, Stewart S, Zvolensky M, Steeves D. Evaluating the mediating role of coping-based smoking motives among treatment-seeking adult smokers. Nicotine Tob Res. 2009;11:1296–1303. doi: 10.1093/ntr/ntp134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zvolensky MJ, Bernstein A, Marshall EC, Feldner MT. Panic attacks, panic disorder, and agoraphobia: associations with substance use, abuse, and dependence. Curr Psychiatry Rep. 2008;8:279–285. doi: 10.1007/s11920-006-0063-6. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP) New York, NY: Biometrics Research; 2002. [Google Scholar]
- 28.Brown R, Lejuez C, Kahler C, Strong D. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–185. [PubMed] [Google Scholar]
- 29.Babor TF, de la Fuente JR, Saunders J, Grant M. Revision, WHO Document No WHO/PSA/92.4. Geneva: World Health Organization; 1992. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. [Google Scholar]
- 30.Bonn-Miller M, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addiction. 2009;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- 31.Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez E, et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psych Assess. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- 32.Watson D, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 33.Ikard F. A scale to differentiate between types of smoking as related to the management of affect. Int J Addict. 1969;4:649–659. [Google Scholar]
- 34.Shiffman S. Assessing smoking patterns and motives. J Consult Clin Psyc. 1993;61:732–742. doi: 10.1037//0022-006x.61.5.732. [DOI] [PubMed] [Google Scholar]
- 35.Heatherton T, Kozlowski L, Frecker R, Fagerström K. The Fagerström Test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Brit J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 36.Pomerleau C, Carton S, Lutzke M, Flessland K, Pomerleau O. Reliability of the Fagerström Tolerance Questionnaire and the Fagerström Test for nicotine dependence. Addict Behav. 1994;19:33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 37.Macnee C, Talsma A. Development and testing of the barriers to cessation scale. Nurs Res. 1995;44:214–219. [PubMed] [Google Scholar]
- 38.Gifford E, Ritsher J, McKellar J, Moos R. Acceptance and relationship context: a model of substance use disorder treatment outcome. Addiction. 2006;101:1167–1177. doi: 10.1111/j.1360-0443.2006.01506.x. [DOI] [PubMed] [Google Scholar]
- 39.Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behav Ther. 2004;35:689–705. [Google Scholar]
- 40.Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guildford Press; 2013. [Google Scholar]
- 41.Hayes A. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76:408–420. [Google Scholar]
- 42.Preacher K, Hayes A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behv Res Meth Ins C. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 43.Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behv Res Meth Ins C. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 44.Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Integrating an interoceptive exposure-based smoking cessation program into the cognitive-behavioral treatment of panic disorder: theoretical relevance and clinical demonstration. Cogn Behav Pract. 2003;10:347–357. [Google Scholar]
- 45.Hatsukami D, Stead L, Gupta P. Tobacco addiction. Lancet. 2008;371:2027–2038. doi: 10.1016/S0140-6736(08)60871-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fiore MC, Jae’n CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update (Clinical Practice Guideline) Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 47.Beard E, West R. Pilot study of the use of personal carbon monoxide monitoring to achieve radical smoking reduction. J Smoking Cessation. 2012;7:12–17. [Google Scholar]
- 48.Gifford EV, Lillis J. Avoidance and inflexibility as a common clinical pathway in obesity and smoking treatment. J Health Psych. 2009;14:992–996. doi: 10.1177/1359105309342304. [DOI] [PubMed] [Google Scholar]
- 49.Zvolensky MJ, Farris SG, Schmidt NB, Smits JAJ. The role of smoking inflexibility/avoidance in the relation between anxiety sensitivity and tobacco use and beliefs among treatment-seeking smokers. Exp Clin Psychopharm. 2014 doi: 10.1037/a0035306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bricker JB, Mann SL, Marek PM, Liu J, Peterson AV. Telephonedelivered acceptance and commitment therapy for adult smoking cessation: a feasibility study. Nicotine Tob Res. 2010;12:454–458. doi: 10.1093/ntr/ntq002. [DOI] [PubMed] [Google Scholar]
- 51.Weinberger A, Maciejewski P, McKee S, Reutenauer E, Mazure C. Gender differences in associations between lifetime alcohol, depression, panic disorder, and posttraumatic stress disorder and tobacco withdrawal. Am J Addiction. 2009;18:140–147. doi: 10.1080/10550490802544888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pang RD, Leventhal AM. Sex differences in negative affect and lapse behavior during acute tobacco abstinence: a laboratory study. Exp Clin Psychopharm. 2013;21:269–276. doi: 10.1037/a0033429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sachs-Ericsson N, Schmidt NB, Zvolensky MJ, Mitchell M, Collins N, Blazer DG. Smoking cessation behavior in older adults by race and gender: the role of health problems and psychological distress. Nicotine Tob Res. 2009;11:433–443. doi: 10.1093/ntr/ntp002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Leyro T, Zvolensky M. The interaction of nicotine withdrawal and panic disorder in the prediction of panic-relevant responding to a biological challenge. Psych Addict Behav. 2013;27:90–101. doi: 10.1037/a0029423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Korte KJ, Capron DW, Zvolensky MJ, Schmidt NB. The Fagerström scales: does altering the scoring enhance the psychometric properties? Addict Behav. 2013;38:1757–1763. doi: 10.1016/j.addbeh.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DeVellis RF. Scale development: theory and applications. 2. Thousand Oaks, California: Sage Publications; 2003. [Google Scholar]


