Abstract
Background:
A detailed understanding of facial anatomy, specifically the vascular framework, is crucial for delivering safe nonsurgical aesthetic procedures. To date, there is no core document based on consensus for the teaching of facial anatomy to aesthetic physicians exists. The aim of this study was to ascertain the most critical anatomical structures for avoiding disastrous complications during nonsurgical aesthetic procedures.
Methods:
After a detailed literature review, Delphi questionnaire was developed listing 154 anatomical structures of the face and neck for consensus review. Thirty-five international experts in surgical and nonsurgical facial aesthetics were invited to complete an online survey designed to rank the relevance of each anatomical element on a Likert scale from 1 (not at all important) to 4 (very important) or 5 (no opinion). Consensus for items included in the core syllabus was predefined as achieving a Cronbach’s α ≥ 0.90 and an agreement score of ≥ 80%.
Results:
Thirty-four international experts (97.14%) completed the iterative online Delphi survey. The consensus among the specialists polled was achieved after 1 round of the survey (Cronbach’s α = 0.94). The expert panel reached an agreement score of ≥ 80% on 137 of the 154 anatomical structures listed.
Conclusion:
The outcome of this Delphi study represents an essential first step in systematizing an evidence-based facial anatomy “Core Syllabus” for the teaching of aesthetic physicians and practitioners. This “Core Syllabus” will act as a blueprint for the educators while crafting a program.
INTRODUCTION
The Merriam-Webster dictionary notes that the word anatomy was first used in the 14th century and was defined as “the art of unraveling the parts of an organism to ascertain their position, relations, structure, and function.”1 The study of gross anatomy traditionally epitomizes a crucial stage in the training of prospective physicians. “The Anatomy Lesson,” one of the first portraits by the young Rembrandt in the year 1632, displays assiduous scholars hovering over a corpse under the direction of a praelector or mentor (Dr. Nicolaes Tulp). This famous masterpiece bears witness to the significance of physicians obtaining a sound basis in the anatomical sciences.2
A thorough understanding of anatomy is a primary requisite for physicians to assess, diagnose, select appropriate treatment, and complete clinical procedures safely and more efficiently. For centuries, detailed appreciation of human anatomy has remained a cornerstone of the successful practice of medicine.3 More recently, the method of anatomy teaching in medical schools has undergone significant changes. This is no better exemplified than in the United Kingdom after the publication of the General Medical Council’s Tomorrow’s Doctors. The transformation has brought a range of pedagogic styles including problem-based, patient-centric, self-directed, and system-based teaching, delivered through small group classes or clinical sessions.4 Recent technological advances such as virtual reality, computer-aided learning, and multimedia resources integrated into the classic learning method of prosections have changed the entire perspective of anatomical teaching.
In the literature, many authors have expressed substantial concern about the decline of proper anatomy education and its consequences in undergraduate training.5,6 Applying anatomical expertise requires sequential learning, in which core knowledge developed during preclinical years is contextualized during the clinical years. Inevitably, there is a limited recall of the knowledge, which was gained by learning the 3-dimensional functional anatomy, even in a spiral curriculum where familiarity with anatomical structures is repeated several times during the course.7 This apparent inability to contextualize remote anatomical learnings has led to the questioning of the proficiency of newly graduated physicians. Recent surveys have shown that clinicians in both the United Kingdom and North America perceive modern anatomical education to be inadequate.8,9 A review article published in 2012 added credence by citing 32 cases of blindness as a result of inadvertent cosmetic filler or autologous fat vascular occlusion.10 In a more recent review article, 98 cases of blindness due to cosmetic injection therapy were identified, originating from different facial areas.11
This fundamental lack of anatomical knowledge leads to significant concerns about the competency levels of many aesthetic practitioners and particularly the level of safety in clinical practice.5,8,12 Acknowledging that anatomical familiarity is paramount to safe and efficient clinical practice, the question remains as to “what ought to be taught.”
There is an urgent need to integrate all the available anatomical nomenclature into a mandatory list of critical structural knowledge that is common to all nonsurgical facial aesthetics procedures. Furthermore, there is a lack of a single database to which course directors can refer to ensure that all the attendees have gained the critical knowledge necessary for safe clinical practice; nonpractical superficial memorization through textbooks is not sufficient.
To determine appropriate content for facial anatomy teaching and learning, the authors conducted a modified Delphi study to build consensus among aesthetic plastic surgeons and dermatologists with global recognition as experts in both the practicing and teaching of nonsurgical facial aesthetics. Author’s objective was to ascertain the most significant anatomical landmarks and structures necessary to avoid disastrous complications during nonsurgical aesthetic procedures. The goal of the present study was to create a facial anatomy core document for postgraduate and continuing medical education in facial aesthetics.
METHODS
Study Design
The study was approved by the Ethics Committee, Faculty of Medical Sciences, Anglia Ruskin University, Chelmsford, United Kingdom. A modified Delphi methodology was used to build the consensus among the expert panel of aesthetic dermatology and plastic surgery educators. The Delphi method is a proven technique commonly used in medical education research for curriculum and competency development.13–15 The process attempts “to assess the extent of agreement (consensus measurement) and to resolve disagreement (consensus development)” where there is either a lack of scientific evidence or contradictory evidence on a particular topic.16 The Delphi method has been established as an effective approach to systematically collecting experts’ opinions to achieve consensus on subjects without bias.13 Based on the assumption that “group opinion is considered more valid and reliable than individual belief,”17 the Delphi method was adopted as the methodological approach to achieve consensus regarding the importance of specific anatomical components of facial assessment and treatment through injection therapy.
Expert Panel
The members of the consensus group were selected based on their experience as global thought leaders in the field of nonsurgical facial aesthetics. This subjective selection was supported by their contribution to education and research through the medical/surgical journal and textbook publications and podium appearances at major aesthetic meetings. Every polled participant required affiliation to an aesthetic plastic surgery or dermatology society within the Americas, Asia, Australia, or Europe (Table 1). Members of the expert panel were invited from 12 countries averaging more than 20 years of experience to represent views from a wide geographical area (Fig. 1).
Table 1.
Geographical Distribution of Expert Panel
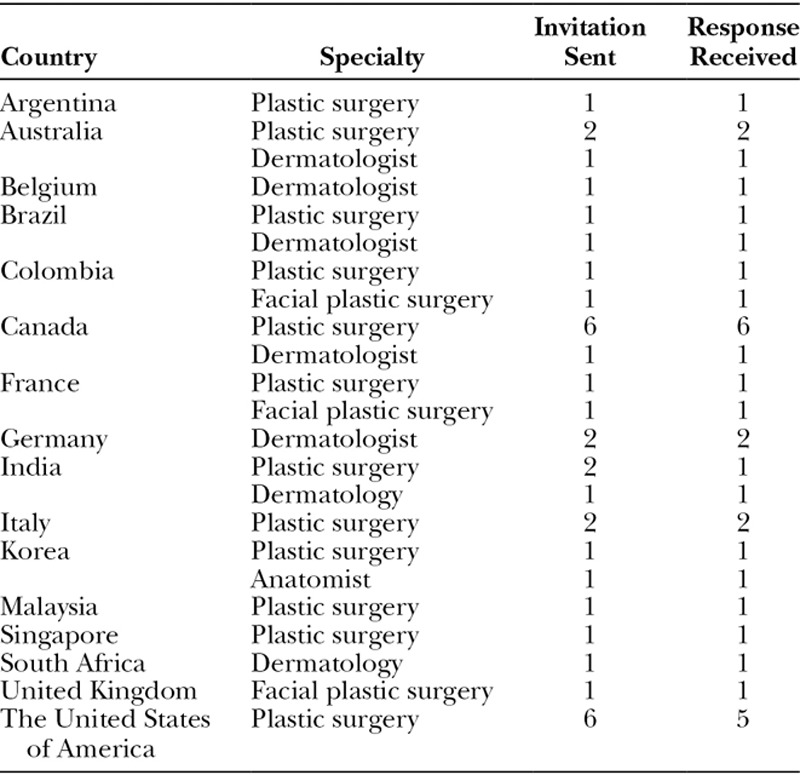
Fig. 1.
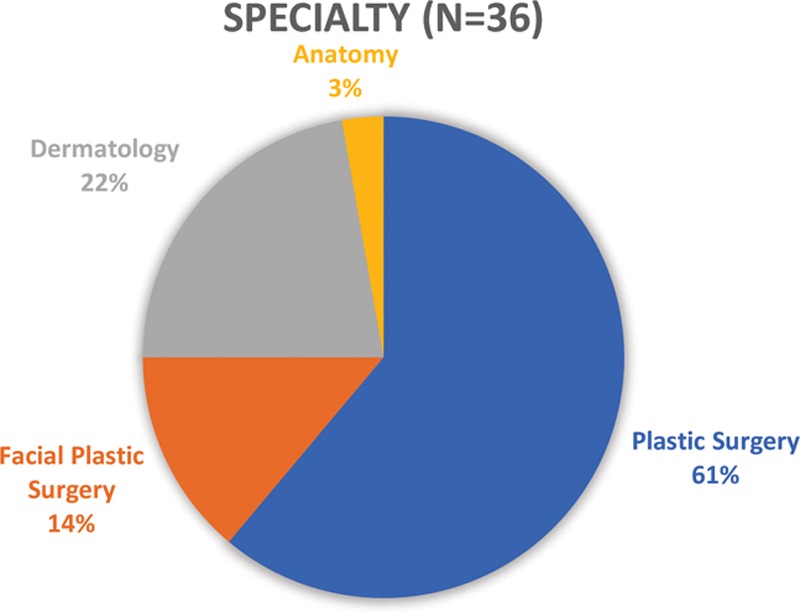
Specialty wise distribution of expert panel.
Questionnaire Development
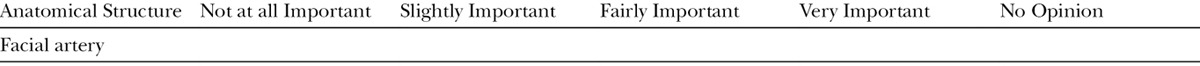
A comprehensive list of vital anatomical structures was developed that was deemed applicable for carrying out nonsurgical aesthetic procedures. This list was prepared from multiple sources including the authors’ extensive experience with surgical anatomy and detailed cadaver dissections, and an in-depth review of published literature and reference textbooks on facial anatomy.10,18–21 The survey questionnaire comprised 154 anatomical structures of the face and neck including topographical landmarks, neurovascular structures, mimetic muscles of facial expression, functional muscles of mastication, superficial and deep fat compartments, true osteocutaneous and false ligaments, fascial planes, and defined anatomical spaces. The online questionnaire was developed using a web-based survey tool (www.surveymonkey.net), and contributors received an e-mail invitation to participate. Panel members were asked to rate the relevance of each of the 154 facial anatomical structures for nonsurgical facial aesthetics on a 5-point Likert-type Scale (1 = Not at all Important; 2 = Slightly Important; 3 = Fairly Important; 4 = Very Important; 5 = No Opinion). The consensus participants were able to provide comments, suggestions, and expand on their reasons for selecting low-level importance (“not at all important”; Table 2).
Table 2.
Example of the Questionnaire (1 = Not at all Important; 2 = Slightly Important; 3 = Fairly Important; 4 = Very Important; 5 = No Opinion)
Determination of Consensus
Delphi method does not have a set rule as to the number of rounds of questionnaires provided; however, 2 or 3 rounds are commonly in practice.22 Internal consistency or the homogeneity of the opinion among group members was defined as consensus. Cronbach’s alpha analysis is 1 of the statistical indices commonly used to determine the reliability at the end of each round. In the statistical literature, an alpha of 0.70 or higher is required to be satisfactory for educational research purposes, whereas for direct clinical applications, it is suggested to obtain a minimum alpha of 0.90.23 For consensus-seeking methodologies, an agreement score of ≥ 80% is considered a significant achievement.24 Therefore, for this study, an agreement score of ≥ 80% and Cronbach’s α ≥ 0.90 was set to represent consensus. Initial survey items that lacked consensus were modified based on the comments from the responders and resubmitted in round 2 for secondary alpha analysis.
Data Collection
Delphi Round 1
The first round of Delphi process triggered with 146 anatomical structures of the face and neck aimed for each panel member to select the critical structures for nonsurgical facial aesthetic procedures. The experts were given the option of the free text box where they could propose additional items.
Delphi Round 2
Items from the first round that were selected by ≥ 80% (consensus) of the experts were essential anatomical structures and were not presented in round 2 for further review. Items with less than 50% consensus were also excluded from round 2. Consequently, only items with an agreement level of 50–79% in the first round were presented to the participants for consensus in round 2. Furthermore, 8 new items proposed by respondents in round 1 were also submitted for the consensus.
RESULTS
The overall response rate was 97.22% (n = 35 of 36) in the first round and 71.4% (n = 25 of 35) in the second round. In the second round, all the comments and suggestions from the panel members were included. The expert panel reached consensus (≥ 80%) on 137 anatomical structures of 154 as critical knowledge for the safe and efficient practice of nonsurgical facial aesthetics. Cronbach’s alpha for the Delphi process was 0.94, which showed a high level of internal consistency and reliability.
A summary of the final consensus organized by anatomical theme is as follows:
Anatomical Layers of the Face
Of the 14 anatomical layers of the face and neck included in the Delphi process, there was complete consensus (≥ 83%) among the experts that 12 structures were “Very Important” for the inclusion in the core syllabus: mimetic muscles, muscles of mastication (temporalis, masseter, pterygoid), subcutaneous and deep fat layers, true retaining ligaments (osteocutaneous retaining ligaments), anatomical spaces (Ristow’s space, prezygomatic, premaxillary), periosteum (bone), superficial musculoaponeurotic system (Table 3). However, there was no consensus (≤ 71%) on the inclusion of false ligaments (fascia-cutaneous ligaments) and skin histology and thickness.
Table 3.
Summary of consensus of inclusion to Core Syllabus of anatomical layers, topographical landmarks, fold, crease, and grooves of face and neck per Delphi Method Survey identified as “Very Important” by ≥ 80% of experts.
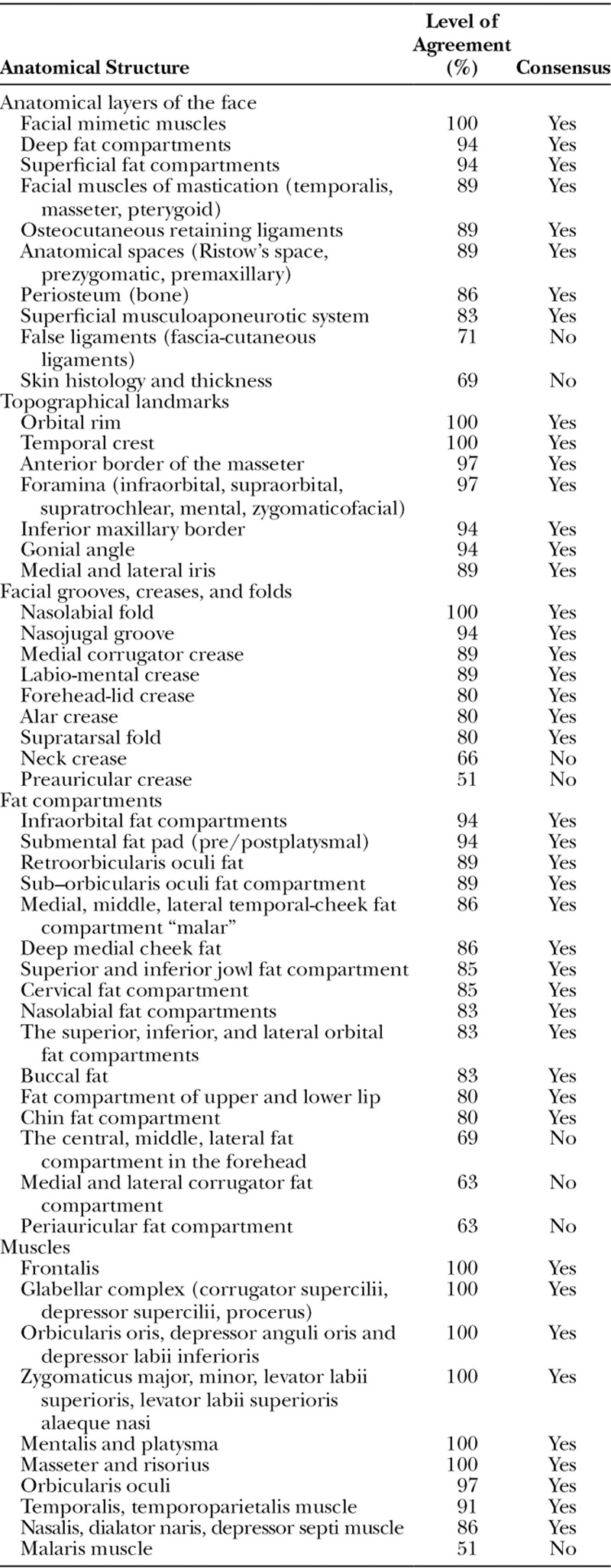
Topographical Landmarks
Of the 13 topographical landmarks of the face and neck included in the Delphi process, there was complete consensus (≥ 89%) to include them all in the core syllabus: temporal crest, orbital rim, inferior maxillary border, pyriform fossa, gonial angle, middle and lateral border of the iris, foramina (infraorbital, supraorbital, supratrochlear, zygomaticofacial, mental), and anterior border of the masseter.
Facial Grooves, Creases, and Folds
Of the 9 facial grooves, creases and folds of the face and neck included in the Delphi process, there was complete consensus (≥ 89%) to include 7 of them in the core syllabus: nasolabial fold, supra-tarsal fold, nasojugal groove, medial corrugator crease, labio-mental crease, forehead lid crease, and alar crease. There was no consensus (≤ 66%) on preauricular and neck crease. One of the experts emphasized the importance of the folds and creases as landmarks for the underlying neuro-vasculature.
Fat Compartments
Of the 23 facial fat compartments of the face and neck included in the Delphi process, there was complete consensus (≥ 86%) to include 20 of them in the core syllabus: orbital (infra, superior, inferior, lateral), temporal cheek (medial, middle, lateral), nasolabial, retro-orbicularis oculi fat, sub–orbicularis oculi fat, deep medial cheek, buccal, upper and lower lip, chin, superior and inferior jowl, submental (pre/postplatysmal) fat compartments. There was no consensus (≤ 69%) on the inclusion of forehead (central, middle, lateral), corrugator (medial, lateral), and periauricular fat compartments in the core syllabus. One of the experts commented that trainees should be required to distinguish the differences in function and morphology of the static (deep) versus the dynamic (superficial) fat pads and the importance of treating a particular fat compartment for a specific indication.
Muscles
Of the 22 muscles (mimetic and mastication) of the face and neck included in the Delphi process, there was complete consensus (≥ 89%) to include 21 of them in the core syllabus: frontalis, corrugator supercilii, depressor supercilii, procerus, orbicularis oculi, zygomaticus major, zygomaticus minor, levator labii superioris, levator labii superioris alaeque nasi, nasalis, dilator naris, depressor septi nasi, orbicularis oris, risorius, depressor anguli oris, depressor labii inferioris, mentalis, platysma, temporalis, temporoparietalis, and masseter. There was no consensus (≤ 51%) on the malaris muscle.
Vasculature and Innervation
Forehead Anatomy
All 9 anatomical structures of the forehead included in the Delphi process achieved complete consensus (≥ 82%) as “critical” structures in the core syllabus (Table 4). These included the supraorbital and supratrochlear foramina, vessels, and nerves; the deep branch of supraorbital nerve and its associated artery; the central forehead artery; and the galea aponeurotica.
Table 4.
A Summary of consensus of inclusion to Core Syllabus of aesthetic zones of face and neck per Delphi Method Survey identi ed as "Very Important" by ≥ 80% of experts.
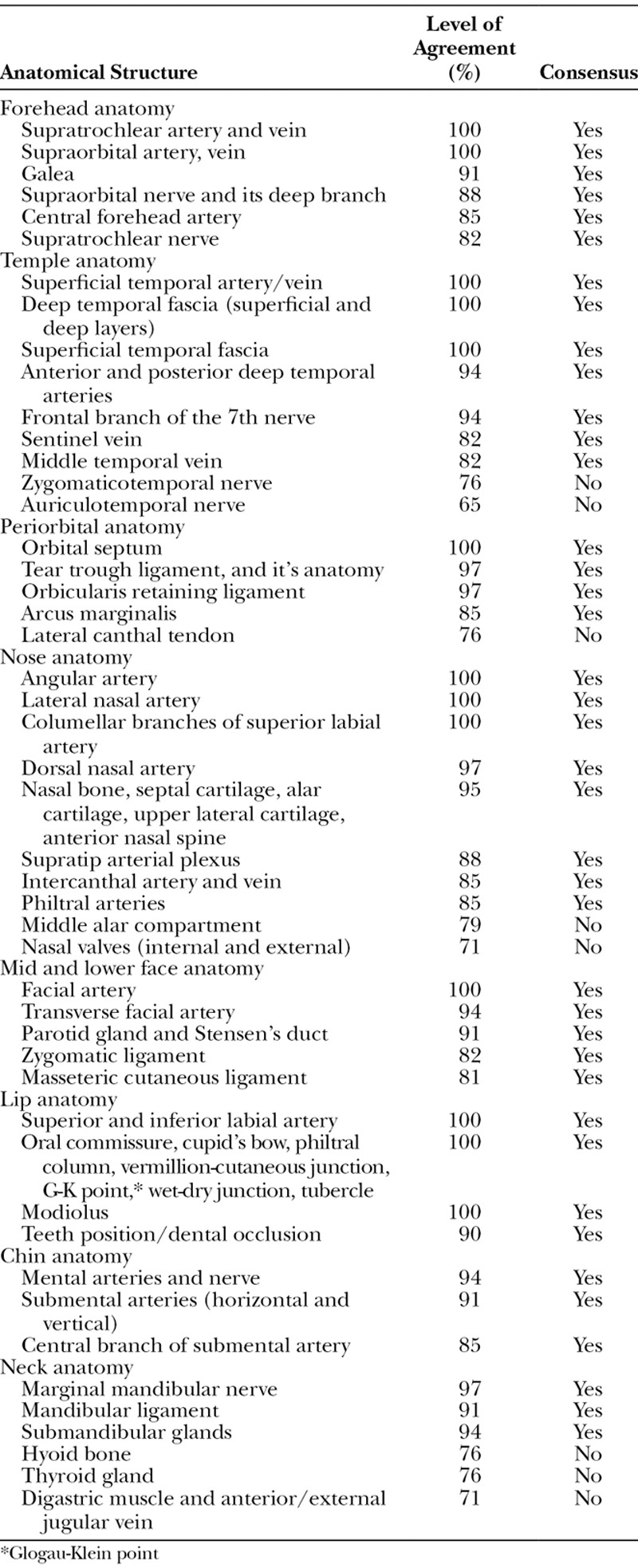
Temple Anatomy
Of the 12 anatomical structures of the temple region included in the Delphi process, there was complete consensus (≥ 82%) to include 10 of them in the core syllabus: superficial temporal artery and vein, anterior and posterior deep temporal arteries, middle temporal vein, sentinel vein, temporal branch of the facial nerve, superficial temporal fascia, both layers of the deep temporal fascia, the interposed extension of the buccal fat pad, and the temporal bone and pterion. There was no consensus on the inclusion of the zygomaticotemporal and auriculotemporal nerves (≤ 76%).
Periorbital Anatomy
Of the 5 anatomical structure of the periorbital region included in the Delphi process, there was a complete consensus (≥ 85%) to include 4 of them in the core syllabus: orbital septum, tear trough ligament, lid cheek junction, orbicularis retaining ligament, and arcus marginalis. There was no consensus (≤ 76%) on the inclusion of the medial and lateral canthal tendons.
Nose Anatomy
Of the 16 anatomical nasal structures included in the Delphi process, there was complete consensus (≥ 85%) to include 13 of them in the core syllabus: angular arteries, dorsal nasal arteries, lateral nasal arteries, columellar branches of the superior labial artery, intercanthal artery and vein, supratip arterial plexus, philtral arteries, nasal bone, septal cartilage, lower lateral cartilages, upper lateral cartilages, medial crura, and anterior nasal spine. There was an inadequate consensus (≤ 71%) regarding the middle alar compartments and the internal and external nasal valves.
Mid and Lower Face Anatomy
There was complete consensus to include the facial artery (100%), the transverse facial artery (94%), the parotid gland, Stensen’s duct (91%), and the masseteric ligament (81%) into the core syllabus.
Lip Anatomy
All 11 anatomical structures of the lip included in the Delphi process obtained complete consensus (≥ 90%) for inclusion in the core syllabus: modiolus, oral commissure, cupid’s bow and peaks, philtral columns, vermillion-cutaneous junction, Glogau-Klein point (G-K point), wet-dry junction, tubercle of the upper lip, superior labial artery, inferior labial artery, and teeth position/dental occlusion.
Chin Anatomy
All 5 anatomical structures of the chin included in the Delphi process achieved complete consensus for inclusion in the core syllabus: mental foramen, mental artery, submental (horizontal and vertical) arteries, and the central branch of the submental artery.
Neck Anatomy
Of the 8 anatomical structures of the neck included in the Delphi process, there was complete consensus to include 4 of them into the core syllabus: marginal mandibular nerve, submandibular glands, mandibular ligament, and cervical fat compartment. The experts polled did not achieve consensus to include the thyroid gland, hyoid bone, digastric muscles, and anterior/external jugular vein in the syllabus. One of the expert commented that for the treatment of submental fat pad, it is essential to know the position of the hyoid bone and thyroid gland.
Concerning the best approach for organizing the anatomy instructions, no consensus was achieved. Nonetheless, most experts polled preferred to structure the anatomy per aesthetic zones with exploration from superficial to deep.
DISCUSSION
This is the first reported global consensus to develop a “Core Syllabus” for teaching facial anatomy to aesthetic practitioners. Rising demand for minimally invasive facial aesthetic treatments such as botulinum toxin and dermal fillers has renewed interest in the detailed understanding of facial anatomy.25,26 A recent global consensus on avoiding complications related to injectable aesthetic procedures has emphasized the understanding of detailed facial anatomy.27 A systematic and structured approach to anatomy teaching to aesthetic physicians is self-evident, as most of the present teaching is occurring outside of formal medical school systems. A lack of guidance in anatomical topic selection for prospective aesthetic specialists has led to a significant disparity in curricula among postgraduate continuing medical education initiatives. In this study, the authors aimed to define a list of essential content for a basic core syllabus.
The modified Delphi method using an online questionnaire has several advantages. It gives the flexibility of recruiting participants across vast geographical locations, and the anonymous construct provides an unbridled opportunity for all the panel members to express their opinion. The Cronbach alpha value of ≥ 0.90 obtained in this study indicates that there were enough members in the polled group to achieve consensus without significant controversy. This lack of divergence can be attributed to the authors’ efforts to include only those anatomical elements that were selected based on genuine evidence.
As the number of the facial aesthetic courses are on the rise across the globe, there is an emergent need to standardize the content of the curriculum to facilitate uniformity in learning experience and activities. Hence, the result of this study can be adopted by the educators as a blue print while road mapping the learning objectives to craft a program. This will in turn help learners to have a comparable learning experience and will help educators to systematically identify the effectiveness or further improvement.
LIMITATIONS
The authors recognize the limitation of the study’s design in that the geographical distribution of the specialities was not equal, and a high proportion of the group members polled were aesthetic plastic surgeons from North America, thereby introducing a perspective bias. Although basic human anatomy is similar in humans, cultural, racial, and ethnic preferences for aesthetic enhancement portend an experiential shift in plastic surgical practices, which could influence the ranking of essential facial anatomical landmarks. Future studies can address this issue by surveying the aesthetic physicians and dermatologists individually using the Delphi method and then pooling the result.
CONCLUSIONS
The outcome of this study has produced a consensus on 137 facial anatomical structures that are the core knowledge necessary for “safer” injection therapy. It represents an essential first step in systematizing a postgraduate evidence-based facial anatomy curriculum directed at aesthetic physicians and practitioners.
ACKNOWLEDGMENTS
The authors acknowledge the expert panel members who participated in the survey completion: W.P. Adams Jr, MD, R. Banegas, MD, L. Belhaouari, MD, A. Benchertrit, MD, D. Bertossi, MD, A. Braz, MD, P. Callan, MD, V. Chatrath, MD, K. De Boulle, MD, M. De Maio, MD, J. Espinosa, MD, S. Fagien, MD, M. Gilardino, MD, G. Goodman, MD, B. Henriquez, MD, I. Heydenrych, MD, D. Hirsch, MD, K.M. Kapoor, MCh, J. Kenkel, MD, H-J Kim, DDS, PhD, A. Labib, MD, D. Lalonde, MD, H-K Lee, MD, S. Liew, MD, M. Mosher, MD, R.S. Mulholland, MD, A. Nikolis, MD, P. Ogilvie, MD, W. Philipp-Dormston, MD, H. Raspaldo, MD, K. Remington, MD, R. Rohrich, MD, M. Signorini, MD, L.K. Siea, MD, J. Stuzin, MD, W. Wu, MD.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Anglia Ruskin University, Chelmsford, United Kingdom.
REFERENCES
- 1.Merriam-Webster Dictionary. 2017Massachusetts,USA: Merriam-Webster, Incorporated. [Google Scholar]
- 2.Tubbs RS, Sorenson EP, Sharma A, et al. The development of a core syllabus for the teaching of head and neck anatomy to medical students. Clin Anat. 2014;27:321–330.. doi:10.1002/ca.22353. [DOI] [PubMed] [Google Scholar]
- 3.Kumar N, Rahman E. Effectiveness of teaching facial anatomy through cadaver dissection on aesthetic physicians’ knowledge. Adv Med Educ Pract. 2017:475–480.. http://dx.doi.org/10.2147/AMEP.S139893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swamy M, Venkatachalam S, McLachlan J. A Delphi consensus study to identify current clinically most valuable orthopaedic anatomy components for teaching medical students. BMC Med Educ. 2014;14:230 doi:10.1186/1472-6920-14-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Older J. Anatomy: a must for teaching the next generation. Surgeon. 2004;2:79–90.. [DOI] [PubMed] [Google Scholar]
- 6.Estai M, Bunt S. Best teaching practices in anatomy education: a critical review. Ann Anat. 2016;208:151–157.. [DOI] [PubMed] [Google Scholar]
- 7.McHanwell S, Davies DC, Morris J, et al. A core syllabus in anatomy for medical students—adding common sense to need to know. Eur J Anat. 2007;11:3–18.. [Google Scholar]
- 8.Waterston SW, Stewart IJ. Survey of clinicians’ attitudes to the anatomical teaching and knowledge of medical students. Clin Anat. 2005;18:380–384.. [DOI] [PubMed] [Google Scholar]
- 9.Cottam WW. Adequacy of medical school gross anatomy education as perceived by certain postgraduate residency programs and anatomy course directors. Clin Anat. 1999;12:55–65.. [DOI] [PubMed] [Google Scholar]
- 10.Carruthers JDA, Fagien S, Rohrich RJ, et al. Blindness caused by cosmetic filler injection. Plast Reconstr Surg. 2014;134:1197–1201.. doi:10.1097/PRS.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 11.Lazzeri D, Agostini T, Figus M, et al. Blindness following cosmetic injections of the face. Plast Reconstr Surg. 2012;129:995–1012.. [DOI] [PubMed] [Google Scholar]
- 12.Singh R, Shane Tubbs R, Gupta K, et al. Is the decline of human anatomy hazardous to medical education/profession?—A review. Surg Radiol Anat. 2015;37:1257–1265.. [DOI] [PubMed] [Google Scholar]
- 13.Williams PL, Webb C. The Delphi technique: a methodological discussion. J Adv Nurs. 1994;19:180–186.. [DOI] [PubMed] [Google Scholar]
- 14.Penciner R, Langhan T, Lee R, et al. Using a Delphi process to establish consensus on emergency medicine clerkship competencies. Med Teach. 2011;33:e333–e339.. [DOI] [PubMed] [Google Scholar]
- 15.Flynn L, Verma S. Fundamental components of a curriculum for residents in health advocacy. Med Teach. 2008;30:e178–e183.. [DOI] [PubMed] [Google Scholar]
- 16.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–380.. doi:10.2164/jandrol.111.015065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keeney S, Hasson F, McKenna H. The Delphi Technique in Nursing and Health Research. 2011. Oxford,UK: John Wiley & Sons; doi:10.1002/9781444392029.ch1. [Google Scholar]
- 18.Pessa JE, Rohrich RJ. Facial Topography: Clinical Anatomy of the Face. 20122012th ed St. Louis, Missouri: Quality Medical Publishing Inc. [Google Scholar]
- 19.Cotofana S, Mian A, Sykes JM, et al. An update on the anatomy of the forehead compartments. Plast Reconstr Surg. 2017;139:864e–872e.. doi:10.1097/PRS.0000000000003174. [DOI] [PubMed] [Google Scholar]
- 20.Braz A, Humphrey S, Weinkle S, et al. Lower face: clinical anatomy and regional approaches with injectable fillers. Plast Reconstr Surg. 2015;136:235S–257S.. [DOI] [PubMed] [Google Scholar]
- 21.Sykes JM, Cotofana S, Trevidic P, et al. Upper face: clinical anatomy and regional approaches. Plast Reconstr Surg. 2015;136:204S–218S.. doi:10.1097/PRS.0000000000001830. [DOI] [PubMed] [Google Scholar]
- 22.Green B, Jones M, Hughes D, et al. Applying the Delphi technique in a study of GPs’ information requirements. Health Soc Care Community. 1999;7:198–205.. [DOI] [PubMed] [Google Scholar]
- 23.Graham B, Regehr G, Wright JG. Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol. 2003;56:1150–1156.. [DOI] [PubMed] [Google Scholar]
- 24.Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314:572 doi:10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gladstone HB, Cohen JL. Adverse effects when injecting facial fillers. Semin Cutan Med Surg. 2007;26:34–39.. [DOI] [PubMed] [Google Scholar]
- 26.de Maio M, Swift A, Signorini M, et al. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers. Plast Reconstr Surg. 2017;140:265e–276e.. doi:10.1097/PRS.0000000000003544. [DOI] [PubMed] [Google Scholar]
- 27.Signorini M, Liew S, Sundaram H, et al. ; Global Aesthetics Consensus Group. Global aesthetics consensus: avoidance and management of complications from hyaluronic acid fillers-evidence- and opinion-based review and consensus recommendations. Plast Reconstr Surg. 2016;137:961e–971e.. [DOI] [PMC free article] [PubMed] [Google Scholar]


