Abstract
Involvement of patients and the public is now recognized to be essential for the good conduct of research. Patient and public involvement in research priority setting and funding decisions is only beginning to be recognized as important, and methods for doing so are nascent. This protocol describes the Research Prioritization by Affected Communities (RPAC) protocol and findings from its use with women at high socio-demographic risk for preterm birth. The goal was to directly involve these women in identifying and prioritizing their unanswered questions about pregnancy, birth and neonatal care, and treatment so that their views could be included in research priority setting by funders and researchers. The RPAC protocol may be used to meaningfully involve under-represented groups at high-risk for specific health problems, or those who face disproportionate burden of disease, in research strategy and funding priority setting.
Keywords: Behavior, Issue 131, Preterm birth, research, uncertainty, patient engagement, patient empowerment, patient and public involvement
Introduction
Patient and public involvement in healthcare research improves relevance and credibility of results, increases enrollment and retention, and accelerates translation into clinical practice.1 Although the terms are often used interchangeably, engagement, participation, and involvement represent three different levels of contact between researchers and individual patients or the general public. Engagement is the lowest level and includes activities of researchers and institutions to share information and knowledge about research with patients and the public. Participation is the activity of study subjects taking part in research studies. Involvement is the highest level of contact, where patients, members of affected communities or of the general public are actively involved in shaping research projects from design to dissemination, including as co-researchers.2,3 The partnership between community members or representatives and researchers or academic institutions in co-development of research questions and co-ownership of research projects is commonly known as community based participatory research.4 These methods have been effective in increasing the level of involvement of patients and the public in research as well as the relevance of research findings to affected communities.5 More recently, research funders have begun to recognize the importance of patient and public involvement in strategic research agenda setting and to seek the engagement/involvement of patients and the public in defining areas of focus for research funding and in prioritizing what research to fund. Patient and public involvement in research priority setting represents the highest level of involvement, and is upstream from community based participatory research. Patient and public involvement in research priority setting is essential for research funding strategy development so that requests for proposals and funding decisions reflect topics of greatest interest to the public as well as to the research community.6 There is a clear and growing international expectation that high quality research be conducted in partnership with patients and communities and not on them solely as research subjects.
Methods for patient and public involvement in research priority setting are relatively new and evolving. Thus far, major funders tend to solicit involvement of representatives from patient advocacy organizations with experience of patient and public involvement rather than directly from members of affected communities or the general public. The involvement of patients or patient representatives is usually as part of larger stakeholder groups that may include frontline healthcare professionals and industry through online survey methods and focus groups with predominantly professional stakeholders7,8,9, or 'town hall' style meetings.9
The most well-established method for research patient and public involvement is the James Lind Alliance (JLA) Priority Setting Partnerships method. Established in 2004, the JLA Priority Setting Partnership method10 is a structured approach, bringing patients, their caregivers and clinician groups together to identify treatment uncertainties (i.e., questions about treatments which cannot be answered by existing research) which are important to all groups. The goals of the Priority Setting Partnerships are to reach consensus on the priority uncertainties and to produce a final list (often a "top 10") of jointly agreed research priorities, and then to publicize the priorities widely to influence researchers and research funders to address them. The JLA Priority Setting Partnership method has been effectively used for a wide range of conditions. The JLA Guidebook10 provides a detailed step-by-step protocol for establishing and conducting Priority Setting Partnerships for any health topic. It consists of a multi-phase approach, beginning with an extensive literature review and online or postal surveys with a wide range of stakeholders to generate a comprehensive list of uncertainties on a particular health topic. Then, if needed, survey consensus methods, such as modified Delphi techniques, wherein repeated rounds of ranking (usually by questionnaires) and reporting back group results are used to achieve consensus and narrow the uncertainty list to a manageable number. The list is then presented to mixed stakeholder focus groups who use group consensus methods, such as Nominal Group technique, to rank the most important research topics and produce a prioritized list.7,8
Notably absent from the published literature on patient and public involvement in research priority setting is the involvement of patients and members of the public from under-represented minority groups. This exacerbates the disparities in patient and public involvement by under-represented minority populations in healthcare research overall,11 and perhaps perpetuates the mistrust resulting from historical misconduct of research, particularly with communities of color.12 Moreover, there has been very little focus on methods to specifically engage individuals from under-represented minority groups in research priority setting.11,13 This is a critical omission because without evidence of the effectiveness of the methods in successfully involving individuals from under-represented minority groups in research prioritization, there may be unintended consequences, such as privileging views of certain stakeholders leading to further disengagement of those minority groups. For example, the JLA Priority Setting Partnership 10 method does not specifically address the challenge of ensuring involvement of under-represented minority groups and there are several phases of the process where their views may be given lesser priority than other stakeholders. First, reliance on the literature and traditional stakeholder representative groups for the first level generation of uncertainties privileges the research that has been conducted based on priorities of the research community and established organizations, which do not represent well the uncertainties and questions of under-represented minority groups. Second, even with skilled facilitators and well-tested methods, holding consensus groups with under-represented minority individuals and healthcare professionals together might unintentionally privilege the voices and views of the professionals. Therefore, new methods are needed that focus on and develop capacity for under-represented minority groups to be involved in research priority setting, especially when they are disproportionately affected by serious health conditions.
One such health condition is preterm birth, defined as birth before completion of 37 weeks of gestation. Preterm birth is a complex condition with both medical and socio-demographic risk factors that is associated with numerous adverse maternal and infant outcomes, affecting the lives of children and families and costing many billions to society.14 African-American race, low socioeconomic status and limited education are among the strong, but largely unexplained risk factors for preterm birth.14,15,16,17 Until recently, there has been very little research on the experiences and views of women at high socio-demographic risk for preterm birth14 and preterm birth research priority setting in the United States has had no direct patient and public involvement. The first patient and public involvement in preterm birth research priority setting was reported in 2014 the United Kingdom (UK).18,19 Although groundbreaking for the field, the UK preterm birth Priority Setting Partnership16 did not include women at high socio-demographic risk for preterm birth, such as those at-risk due to social determinants of health or health disparities. Since these groups bear a disproportionate burden of disease, it is imperative that their view be included in research priority setting.
The UCSF California Preterm Birth Initiative (PTBi-CA) is a multi-year, philanthropically-funded research initiative to reduce the burden of the unchecked preterm birth epidemic in high-disparity regions of California (www.pretermbirth.ucsf.edu). PTBi-CA brings together researchers from across numerous specialties and disciplines, public health agencies and community leaders to work in direct partnership with women and families most affected by the epidemic. Women who have had a preterm birth and those who are at high socio-demographic risk for preterm birth and the frontline clinical and social care providers who work with these women and their families are involved at all stages of the research process — from developing the research priorities, designing research protocols, conducting studies, disseminating results and translation of findings to practice and policy.
Given the limited methods to specifically involve under-represented minority groups in research priority setting, and because it was not known if women of color at high socio-demographic risk for preterm birth would be interested or willing to engage in the research priority setting process, the established JLA Priority Setting Partnership method was not appropriate as a first step in patient and public involvement for this population and topic. This paper describes the protocol for a new method to initiate patient and public involvement, Research Prioritization by Affected Communities (RPAC), and describes its use with women at high socio-demographic risk for preterm birth. The goal of RPAC is to directly involve individuals from under-represented minority groups, in this case women of color, in identifying and prioritizing their unanswered questions about their health condition, in this case pregnancy, birth and neonatal care and treatment. The RPAC method enables discovery of the researchable unanswered research questions of greatest priority to the affected communities so that they can be included in research priority setting by funders and researchers. The UCSF PTBi-CA incorporated the research priorities of women at high socio-demographic risk for preterm birth in their request for proposals and included women who participated in the RPAC process in proposal review and funding decisions (see brief video example: https://www.youtube.com/watch?v=df1qRu4wzJo). The RPAC protocol can lead to meaningful partnership of individuals from communities affected by a health condition in decisions about research foci and funding.
Protocol
The protocol was reviewed and granted exempt status by the University of California, San Francisco Committee on Human Research.
The RPAC protocol involves preparation, facilitated group work (session 1), interim analysis, facilitated group work (session 2) and summary analysis. Suggested roles and time allocation are noted in parentheses for each major section of the session descriptions below. Suggested scripts for each step are shown in quotations. Direct questions to participants are in bold. Follow-up question probes to promote further discussion are in italics.
1. Preparation for Session 1
Identify and form the research team, including collaboration with community-based organizations (CBO) serving the women at high socio-demographic risk for preterm birth [or other CBO serving the under-represented community experiencing a significant health disparity of interest]. The research team should include members of the under-represented community in all aspects of the research, including analysis, presentation and publication. Community based participatory research principles and methods4 are prominent within the RPAC protocol and it is recommended to have expertise on the project team or access to consultation.
Review the RPAC protocol, participant recruitment materials and interview guides for the two sessions with the CBO partners and make any amendments to reflect the local context.
Obtain Institutional Review Board approval or exemption as required by responsible institution.
- Identify roles: a) CBO staff member liaison; b) Session facilitator(s) and project staff member supporting project preparation and in-session support. One or two facilitators (two facilitators recommended) can lead the session. The same person(s) should lead both session 1 and session 2. Facilitators should have previous experience of group facilitation, ideally with the community from which the participants will be recruited, and familiarity with the health condition of interest. We recommend that at least one of the facilitators have some affiliation with the community of interest, for example, having experienced the condition or a member of the under-represented community. Facilitators must refrain from providing their own opinions about the topic or slipping into a teaching or counselling role during the sessions.
- Jointly plan the logistics, including: recruitment, scheduling the two 2-hour sessions 4-to-6 weeks apart, room configuration, session supplies (Table of Materials - Session 1), food, child care and participant travel and reimbursement.
Arrange for audio-recording of the sessions and transcription services so that transcripts are available within 7-10 days of session 1.
- Conduct participant recruitment (CBO staff member), by telephone or in-person. Invite women who are pregnant and at high socio-demographic risk for preterm birth, or who have had a preterm baby, to participate in the two-part sessions. Groups can be a mix of pregnant and non-pregnant women. Invite 10-to-12 participants to ensure attendance of 6-to-10 participants.
- CBO staff member invites participants using suggested script (to be modified for local context): "We're partnering with [Insert your organization] to identify uncertainties or unanswered questions about the causes, prevention, treatment and outcomes of preterm birth. A preterm birth occurs when babies are born too soon, before 37 weeks of pregnancy. Preterm birth is associated with numerous adverse infant outcomes, affects quality of life for the entire family and has a large cost to healthcare systems and society. Researchers should investigate questions that are important to people who might be affected by preterm birth, but we don't know very much yet about the views of women in communities at high risk for preterm birth. Our goal is to bring the views of women and families to prioritize the unanswered questions about preterm birth that need more research. This information will help ensure that those who fund health research are aware of what matters to women and families. To do this, we are going to be holding a series of two focus groups, each lasting two hours on [date] and [date] at [location] from [time] to [time] to identify unanswered questions about preterm birth that women think need to be answered by research. I am contacting you to see if you would be interested in joining other women who participate in our programs to share your views on this topic with us. If you participate, you will receive [insert information about participant reimbursement, transportation, child care, refreshments]. I also want to let you know the sessions will be audio-recorded and transcribed to a written record that we can review and summarize to share with researchers, research funders and the public. No names or identifying information will be included in any reports about this work. Would you be interested in participating? Do you have any questions? [if not interested in participating, ask about their concerns, see if they can be addressed, and if not, thank them for their interest].
- Several days prior to scheduled session, confirm attendance of 6-to-10 participants (CBO staff member); arrange for session materials (Table of Materials) (Facilitator).
2. Session 1 Generating Research Questions - Group Facilitator Guide
Greet participants on arrival. Provide name tags and take care of required documentation (e.g. participant reimbursement, photo consents), child care, etc.
- Lead the group in an exercise intended to bring their attention to the present moment in preparation to focus on the task at hand. This can be an exercise commonly used by the CBO partner or a simple guided meditation as described here (CBO staff member; 5 minutes).
- CBO staff member leads group opening exercise: "Hello and thank you for participating in this important group. Prior to beginning, we would ask all cell phones be placed on mute and that you fully bring yourself to this space. We will begin with some cleansing deep breaths where you inhale, hold for 3 seconds and exhale. Place all of your belongings under your seat and place your palms on your lap or knees, whichever is more comfortable. You may close your eyes if you wish. Now become aware of your breath and slowly, over a count of four, inhale in and exhale (repeat three times). Each time you exhale, let go of whatever is going on outside of this room. As you breathe in, become more aware of what is going on in your body and in the present moment in this room. Now, breathe normally, open your eyes if they were closed, and focus your attention on the discussion we are about to have together."
- Welcome and thank participants for coming and introduce the session (CBO staff member and Facilitator; 10 minutes).
- Introduce the session (CBO staff member): "We are [insert role] from [insert organization] are here to listen and learn from you. We invited you to come here today because we are very interested in hearing your ideas and opinions about what research should be done to prevent or treat preterm birth. Government agencies, private foundations, universities and companies all give money to fund research with the goal of improving health. We are committed to partnering with communities that are affected to shape the research that is done to reduce preterm birth in [city or region]. Capturing what is important to the community to know, and learning about your lived experiences, will help us to conduct research that will ultimately protect future generations of this community's children. Researchers want and need to partner with communities to understand and address the underlying causes of preterm birth and together figure out what to do about it. We are grateful to be here today to do this work with you. We will start with asking you to each go around the room and introduce yourself and tell us why you were interested in coming here today. Now let's review the ground rules for this session. Babies Rule! If you need to attend to your child, please do and rejoin when you can. One person should speak at a time, for the recording and to hear all views. Let others finish talking before speaking. Confidentiality is important throughout this process so that you all feel comfortable to talk freely. What is said here should not be repeated elsewhere. Also, please remember that your participation today is completely voluntary and you may stop or refrain at any time from participating in answering any question or participating in the discussion.
- Invite participants to suggest other ground rules and then asks participants if they have any questions (CBO staff member). Once questions have been answered, ask participants' permission to turn on the recorder and begin the session (the CBO staff liaison).
- Continue with session description (Facilitator): "Today's conversation is the first of two discussions we'll have together. In today's group, we'll focus on identifying unanswered questions about why babies are born early and how best to care for them and their families - topics or questions that you think need to be answered by research. We'll come back together in about 6 weeks for the second session to rank these topics and questions according to what you think are most important or should be done first.
- Explore participants' views about research (Facilitator; 15 minutes, approximately).
- Introduce the topic of clinical research and its relevance to an individual's health (Facilitator): "Research is something that most people do not think about on a daily basis but it is something that touches all of our lives and directly affects our healthcare. Researchers are just catching on that it is important to ask individuals and communities what questions or uncertainties about their own health or healthcare should be researched. For example: If you had asthma, you might want to know: Are breathing exercises more helpful in controlling asthma than medication? And if you were to look this up on the Internet or to ask your health care provider, you would find that the answer really isn't known. You might feel strongly that money should be put toward finding out the answer to this question. But a drug company might want to lobby the government to spend more money on drug research instead. So, our goal is to make sure that your voice is heard by the research funders and researchers, not just those who would get paid to do the research or profit from the research. Please introduce yourself, and share your views about research. Have you participated in research projects? Do you know anyone who has participated in a research project? If yes, what was it like? If no, what do you think is involved? What are your thoughts about whether or not research affects your health and well-being or that of other people?" What are your thoughts about how answering questions about preterm birth through research might or might not help women who are pregnant/want to become pregnant?
- Explore participants' questions and uncertainties about pregnancy and childbirth (Facilitator; 25 minutes, approximately).
- Introduce process for eliciting questions and uncertainties (Facilitator): "Let's now talk about questions or uncertainties about anything related to why babies are sometimes born early. It can be easiest to come up with possible questions by remembering your conversations or consultations with health care providers before, during or after pregnancy. I'm going to ask each of you to share with us your experience and I will be listening for unanswered questions or uncertainties that you have. As you say them, we will write them on these cards and put them on the board. We will work together to get the wording just as you want it. We will not try to answer the questions today. Our goal is simply to get all of the questions you might have out onto this board. When we are done, we will talk about what we will do with them in our next session. Let's get started. What things did you want to know that your health care provider couldn't answer for you? What things did you wonder about after talking with family or friends or after reading about them? Can you describe the experience(s) seeking health care during your pregnancy that stands out in your mind? What would you change about this experience? What would you do differently? What would you have wanted that you didn't receive? Do you have any unanswered questions about pregnancy?"
- Ask further questions if there is limited discussion in response to above. Script: "To help you, here are some examples of unanswered questions about other health problems: What is the evidence for gargling with aspirin to relieve a sore throat? Which medications are the most effective and have the least side effects after an operation? Can you think of a question about pregnancy or childbirth?"
- Explore participants' questions and uncertainties about preterm birth and care of preterm babies (Facilitator; 40 minutes, approximately). NOTE: if questions about preterm birth emerge in the earlier discussion, continue on. Periodic refocusing on discussion of questions about preterm birth or care of preterm babies may be needed.
- Direct participants to focus on questions and uncertainties about preterm birth (Facilitator): "Now let's talk more specifically about when babies are born early. Do you have any unanswered questions or an uncertainty about the causes and prevention of preterm birth? What about treatment of babies and support for families?" NOTE: If after several attempts with examples generated from above or from other conditions, the group is not able to generate questions or uncertainties related to preterm birth, then read a few of the examples from the JLA preterm birth research priorities list generated from parents, charities and front-line clinicians.19
While conducting steps 2.4 to 2.6, ask clarifying questions as needed to encourage deeper discussion and reveal underlying questions or uncertainties (Facilitator). Examples: Can you tell me more about that? Say more about that. Do others feel this way? Could you give me an example of what you mean? What was your response? What did (specify person) say to you? Is there anything else you would like to add?
While conducting steps 2.4 to 2.6, observe participants to see that all are participating and redirect conversations back to the topic as needed (Facilitator). Examples: Wait until dominant participant pauses to inhale and redirect the conversation as follows: "Thank you, XXX, for your comments. We can see that you've had a lot of experience with XYZ and we appreciate your point of view. Now, it's important that we hear from the rest of the group. YYY, what do you think about XYZ?"
- Bring closure to the discussion and explain next steps. (Facilitator; 15 minutes, approximately).
- Review the list of posted questions. "Is this an accurate summary of our conversation? The goals of our discussion today were to identify what research means to each of you and to develop a list of possible questions that you think need to be investigated to improve healthcare for pregnant women and babies and to prevent or improve outcomes from preterm birth. You have certainly achieved these goals. Is there anything we missed? There are some very important questions here that if we had answers to them would really improve how pregnant women are cared for during pregnancy and childbirth and also could prevent early birth and improve outcomes for early born babies and their families. Thank you. If you think of additional questions after you leave today, please note them down to share in session 2, or share them with [CBO staff liaison or facilitator, as agreed by prior arrangement]. Are there any parting thoughts or comments?"
- Invite participants to give closing remarks focused on gratitude (Facilitator). "We would like to close this session in the spirit of gratitude and hope. "In a few words, can each of you describe something you are grateful for about today's session and how you hope this work we are doing together will help you or other women and babies." Invite participants to come to the wall and take a photo of them standing next to all the questions they generated.
3. Session 1 analysis
Members of the research team: Transcribe all of the potentially researchable questions that were written on the cards by the paticipants during the session into an electronic document.
Obtain session 1 transcript from the audiorecording. Review the transcript and the audiorecording multiple times to identify additional questions that were not written on the cards and add these to the electronic potentially researchable questions document generated in step 3.1.
Remove any questions for which there are definitive answers from systematic reviews or professional guidelines or regulations. Label a new document with these questions as "Research questions with answers" and set aside for later dissemination.
Conduct a thematic analysis20 of the potentially researchable question document to organize the questions under main topic themes. Prepare new cards with these questions and topic headings (one per card, at least 40 size font) to be used in session 2.
4. Preparation for session 2
- Contact CBO partner well in advance and confirm timing, logistics and staffing for session 2.
- Contact participants and confirm their attendance at session 2, making any necessary transportation and childcare arrangements (CBO staff member).
- Arrange for session materials (Table of Materials - Session 2) (Facilitator).
5. Session 2 Prioritizing Research Questions and Topics - Group Facilitator Guide
Greet participants (CBO staff member). See step 2.1 to 2.2 above.
- Welcome and thank participants for coming back and introduce the session (Facilitator; 10 minutes).
- Introduce session 2 (Facilitator): "As you remember, in our first session we talked about your questions and uncertainties about pregnancy, childbirth and preterm birth that you think should to be answered by research. Here on the wall are the questions you shared last time. You generated [number] questions in two hours - that is incredible! When we listened to the audio recording, we heard [number] additional questions that we hadn't written and they are now on the wall here (point to new questions). What you don't see here, are the [number] questions you raised last time for which there is strong research evidence. We will share those later with you and [CBO partner] so that more women can learn this information. Our focus today is to prioritize the large list of unanswered questions that you generated so that research funders and researchers know what questions are most important to women. Today's focus group will occur in two phases. First, we will review the list of questions to make sure we got the wording right, that they truly captured what you said, and to merge or move any of them. You will notice that we created some topic headings and grouped the questions and we want to check in with you to see what you think about the way that we have grouped and labeled your questions. Since we last met, or in this review process, you may have other questions and we will add those questions to cards and put them on the wall. In the second phase of today's session, we will ask you to work individually and then together to select the most important questions and topics and put the top 10 to 15 in order from most to least importance. Does anyone have any questions?
- Review and amend research question list and topic headings (Facilitator; 20 minutes)
- Provide each participant with a paper copy of the list. Read each topic heading and question out loud. Pause every few questions and at each topic heading and ask participants if they agree with the wording, believe the question to be important and, if not, to make any edits. Intermittentlyask if the discussion so far has caused them to think of or remember any other questions they have. If so, write them on a card and ask participants to place it under the appropriate topic heading (or ask participants to create a new topic heading, as appropriate).
- Conduct round 1 of prioritization (Facilitator; 10 minutes)
- Ask participants to individually mark the top 15 questions on their question list.
- Ask participants to take their 15 sticky dots and go up to the wall and put a dot onto each card corresponding to one of their top 15 questions.
- Conduct topic ranking and removal of lower priority questions (CBO staff member and Facilitator; 10 minutes).
- While participants are performing the prior step, lay out a second set of topic headings on the tables (CBO staff member).
- Once participants return to their seats, engage them in placing the topic headings in order of importance (Facilitator). Ask prompting questions such as: Do you think this topic is more or less important than that topic? Should this topic be nearer the bottom or nearer the top of the list? Once all of the topics have been placed in order of importance, confirm that there is consensus. If any disagreements, continue the discussion, with prompting questions to uncover reasons for the differences in priority and to promote reaching a final consensus.
- Concurrent to the above activity, remove all of the questions from the board that do not have dots placed on them by the participants and set these aside (CBO staff member).
- Conduct round 2 of prioritization with group voting on the top 10 to 15 most important research questions (Facilitator; 10 to 15 minutes).
- Ask participants to return to the wall and take their new 5 dots and put them on the cards with the questions they feel are most important. Point out that they are to use a different technique when deciding this time what questions are most important. They may put all of their dots on one question if they choose. They may talk with each other and lobby each other.
- Once participants have placed all of their dots and returned to their seats, remove the questions with the fewest number of dots from both rounds and set these aside, leaving the top 5 to 15 questions. There may be an obvious breakpoint in the number of dots separating the question clusters, or there may not. If not, further work will be needed to engage the group in deciding where the breakpoint is so that only 5 to 15 questions remain on the board.
- Rank order the top priority questions (Facilitator; 5 to 10 minutes).
- Stand at the wall and move questions up or down in the order list based on the participants' responses. This is similar to the table exercise to rank order the topic headings. Ask prompting questions as needed (see 6.2.2).
- Once the final order of the questions is agreed, add in the topic headings where appropriate. NOTE: Some topic headings may have no questions under them. Review the list with the participants, prompting them to notice what is there and what is not. Emphasize that although this list of topics and questions on the wall represents their most pressing questions at this time, the many other questions that they generated are still important and will be shared with researchers and funders. Ask participants to share any names of research organizations or funders they particularly would like the project team to inform about the research priorities.
- Take a photo of the wall. Invite participants to come up and take a photo of the participants standing next to the questions (CBO staff member).
- Debrief about the experience of participating in the sessions and closing (CBO staff member and facilitator; 10 minutes).
- Ask participants to provide feedback on the experience of participating in these sessions. Ask participants to elaborate on what worked well, and what they wish there was more or less of. Discuss how the results from this work will be summarized and shared with participants and presented to CBO partners, researchers and funders, and to the local community. Ask if participants would be interested in participating in these dissemination activities and/or in future collaboration with researchers.
- Facilitator invites participants to give closing remarks focused on gratitude: "We would like to close this session in the spirit of gratitude and hope. "We invite you to describe in a few words something you are grateful for about today's session and how you hope this work we are doing together will help you or other women and babies."
6. Synthesis
Obtain session 2 transcript from the audiorecording. Review the transcript and the audiorecording multiple times to identify additional questions that were not written on the cards. Amend the question document from session 1 with the additional questions written on cards in session 2 or from the session 2 transcript and audiorecording.
Prepare a document with the top priority topics and questions from session 2.
Use the top priority topics and question document and the complete question document in research priority setting and funding decisions and to influence local, national and international research priority setting for preterm birth. NOTES: a) The protocol steps for sessions 1 and 2 can be repeated within and across geographic regions. If this is done, then additional thematic analysis can be done to merge the question list and to explore similarities or differences in priority topics and questions across groups with similar or differing sociodemographic characteristics; b) Over the course of the two sessions, rich qualitative data about the participants' health and healthcare experiences will be generated in the discussion. These data are audiorecorded and transcribed along with the research questions and topics. These data may be subjected to qualitative analysis, using thematic analysis or another framework.
Representative Results
The following results were derived from an ongoing project to involve women at high sociodemographic risk for preterm birth in the research strategy and funding priorities for the PTBI-CA in San Francisco, Oakland and Fresno, California. The representative results are from two CBOs serving women in San Francisco, CA: the Homeless Prenatal Program (HPP) and the Black Infant Health Program (BIH). The organizations either directly deliver or host a variety of services including prenatal, childbirth preparation and post-partum classes. Additional free services include case management, individualized life and goal planning, public health nurse consultation, referral services for medical, social, economic and mental health services and transportation. Staff at each organization invited clients who were pregnant or who had young preterm children to participate in the project.
There were 14 participants in total, 6 from HPP and 8 from BIH, ranging in age from 20 to 42. Of the participants' total of 44 children (range 1 to 5 each), 21% (n=9) were born preterm. Participants self-identified as African-American (n=12), Latina (n=1), or Asian/Pacific Islander (n=1). Three of the women were pregnant at the time of the focus groups, 2 in the HPP groups and 1 in the BIH groups. Participants were compensated for their time. There was no attrition during the study period.
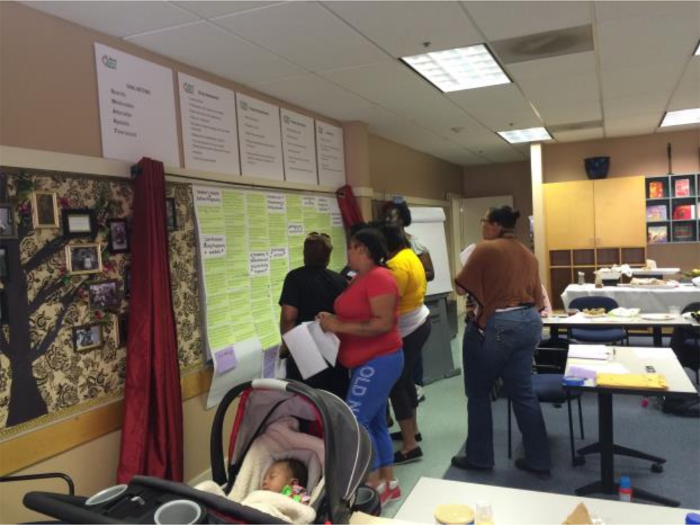
After removing questions posed by participants that had strong evidence from systematic reviews or national guidelines as well as duplicate questions between the two groups, a combined list of 135 unique research questions had been generated from the session 1 activities at the two sites. Using thematic analysis, the questions were grouped under 11 overarching research topic themes. These questions and topics were presented to each of the groups in session 2 and the top 10 (HPP) and top 15 (BIH) research questions were agreed by group consensus. Figure 1 shows the participants performing the dot voting to indicate their round 2 top priority research questions. The results from both groups were again examined together and duplicates removed, resulting in the final list of the combined top 10 specific research questions (Table 1) and top 9 research topics (Table 2).
During the course of the two-session protocol, participants spoke intimately about their own health and healthcare experiences. Participants reported that hearing other women tell their stories prompted them to share more about themselves. During each of the sessions there was discussion among participants about the impact of the women's healthcare experiences personally and on their community. These data were recorded and transcribed as part of the sessions and later subjected to qualitative analysis, adding context, meaning and, on occasion, suggestions for further research on the research priority topics identified as important by the women (data not shown). In the debriefing discussions at the close of session 2 at each site, all of the women reported that participation was a positive learning experience and all expressed interest in continued involvement with researchers.
Figure 1. Participants in Session 2 performing the dot voting to indicate their round 2 top priority research questions. Please click here to view a larger version of this figure.
| How does a mother’s stress affect the baby? |
| What are the most effective ways to improve patient-provider communication, particularly when patients perceive insensitive and rude comments from health care workers? |
| What is the most effective care for pregnancy and high-risk pregnancy? For example, if African American women are at higher risk, why isn’t there specialized care to improve outcomes? |
| What causes Sudden Infant Death Syndrome? |
| Does the type of insurance you have determine the type of care that you get, or the quality of your care and is care different based on insurance status or race? |
| What could make hospital visits and in-hospital stays easier for families and what supports are most helpful for moms with children at home? |
| What medicines are safe to take during pregnancy? |
| How do birth plans help and how can the health care team better follow a woman’s birth plan? |
| How do health care providers decide to involve Child Protective Services during pregnancy care when abuse and neglect are not clearly present? |
| Could experienced moms be used more effectively for breastfeeding support? |
Table 1. Top 10 specific research questions of women at high sociodemographic risk for preterm birth
| Priority | Research topic |
| 1 | Stress during pregnancy and its impact on women and infants |
| 2 | Standards for monitoring and care of women with high risk pregnancies |
| 3 | Impact of employment and insurance coverage on care and outcomes |
| 4 | Safety of drugs and substances during pregnancy and for newborns |
| 5 | Provider-patient communications and decision-making |
| 6 | Breastfeeding support |
| 7 | Standards for referral of women and families to social services |
| 8 | Causes and prevention of Sudden Infant Death Syndrome |
| 9 | Support for mothers and babies at home |
Table 2. Priority research topics for women at high sociodemographic risk for preterm birth
Discussion
The RPAC protocol was specifically developed to guide initial, exploratory research priority setting involvement with under-represented minority individuals who are at high risk for health problems and who face disproportionate burden of disease. It was first trialed with women at high socio-demographic risk for preterm birth to generate a prioritized list of researchable questions and topics about pregnancy, birth and neonatal care and treatment. The prioritized lists resulting from RPAC can then be included in research priority setting by funders and researchers. The RPAC follows the principles of national-level patient engagement rubrics, such as the Patient Centered Outcome Research Institute9,21 in the US and the UK JLA Priority Setting Partnership.10 The RPAC uses elements of the Priority Setting Partnership prioritization protocol, but differs from the Priority Setting Partnership protocol in significant ways. First, the RPAC focuses solely on members of communities affected by a health condition and does not include front-line clinicians whose voices might be privileged in the discussion (even unconsciously by the participants themselves). Second, the RPAC protocol is designed to generate the initial question list de novo from within the group, rather than from prior research literature or surveys. Third, the RPAC is designed to probe more deeply the priorities, experiences and context in which those priorities develop, of a small number of individuals with expertise in the condition by virtue of their individual and community experience, whereas the Priority Setting Partnership protocol is designed to engage a large number of individuals and organizational representatives with broad knowledge of the condition and its impact on patients and families in the research priority setting process. However, the use of RPAC and the JLA Priority Setting Partnerships are not mutually exclusive and RPAC could naturally lead to the formation of a JLA-style Priority Setting Partnership or, conversely JLA Priority Setting Partnership work might lead to use of RPAC for deeper involvement of specific communities affected by a health condition. Once research priorities have been established with patient and public involvement by one or both of these methods, community based participatory research methods can be used to co-design and carry out specific research projects.3,4
The representative results described in this paper illustrate the power of the RPAC protocol to rapidly and deeply engage with women at high socio-demographic risk for preterm birth in identifying the specific research questions and broader research topics of greatest importance to them and their community. These women had no prior research experience and had no prior relationship with the facilitators or their organization. None of them worked in a clinical setting or had any scientific training. Yet, by the end of the first two-hour session, they had generated over 135 unique, researchable questions based on their own experience of care and unanswered health questions as well as from their general curiosity about maternal and infant health that was awakened in the group discussion with other women like themselves. Moreover, as part of the two-session protocol, participants engaged in deep discussion about their own health and healthcare experiences during pregnancy, childbirth and parenting. These data provided a rich substrate for further qualitative analysis of these experiences, with a particular focus on patient-provider and patient-health system interactions.
The RPAC protocol is new and there are a number of issues to consider in evaluating whether or not it is appropriate for other investigations. First, having a clear intention and plan for how the research priorities will inform research strategy and funding decisions is essential, as failure to do so will compromise credibility focus group sessions between the researchers and community. Second, having a CBO partner who is trusted and well-integrated into the community of interest is also essential for success. Third, researchers should be prepared to engage in discussion with the CBO and with RPAC participants about personal and historical misconduct in research because this may arise when the topic of research is raised with communities of color.12 The RPAC protocol has been used thus far only with African-American and Latina women in California at high socio-demographic risk for preterm birth. Therefore, the generalizability of the method requires further evaluation. Nonetheless, it is a promising approach for exploratory research priority setting involvement with under-represented minority individuals who are at high risk for and are disproportionately affected by other health problems.
Partnership with a trusted CBO and skilled facilitation are essential to quickly building and transferring trust among the participants so that they feel comfortable to speak freely and to generate rich data. As with all facilitated group activities, the quality of the output is greatly dependent on the skills of the facilitator to engage the participants in the topic and with each other. Because of the focus on health research, at least one of the facilitators should have a strong working knowledge of clinical care and of the research evidence for the specific health condition under discussion. This is important so that the facilitator can provide example questions if necessary to stimulate discussion or steer the conversation to explore other aspect of the health condition that are not spontaneously brought forth by the participants. At the same time, the facilitators must refrain from providing answers to any research questions posed by the participants or from engaging in any teaching or counseling during this session. Such actions can quickly stifle participants from developing further questions or exploring uncertainties and is to be avoided at all costs. Facilitators should work with the CBO partner to offer participants health information or research evidence after the completion of session 2.
Several important outcomes emerged from the use of RPAC with women at high social-demographic risk for preterm birth. First, the research priority lists generated from the RPAC work in San Francisco, Oakland and Fresno California were included in request for proposals issued by PTBi-CA. Second, some of the women who participated in RPAC applied to and were selected for the PTBi-CA Community Advisory Board and participated in proposal review and recommendation for funding of proposals submitted in response to the request for proposals. This input has been invaluable for the PTBi-CA, ensuring that the commissioned research addresses questions of importance to science and to the community the science is intended to benefit (see brief video example: https://www.youtube.com/watch?v=df1qRu4wzJo).
In summary, the RPAC protocol is a useful method for generating rapid, in-depth knowledge of the research priorities of women at high socio-demographic risk for preterm birth. The RPAC protocol provides a strong foundation for ongoing patient and public involvement in research and can lead to meaningful partnership in research funding decisions to better address the epidemic of preterm birth. The protocol may be further customized for use with underserved minority individuals from communities affected by other health condition to achieve meaningful involvement in decisions about research foci and funding to address those health conditions.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This research was supported by the UCSF California Preterm Birth Initiative. The authors wish to thank Brittany Edwards, Lisa Edwards and Olga Nunez for their assistance and the participants for sharing their experiences and views.
References
- Mullins CD, Abdulhalim AM, Lavallee DC. Continuous patient engagement in comparative effectiveness research. JAMA. 2012;307(15):1587–1588. doi: 10.1001/jama.2012.442. [DOI] [PubMed] [Google Scholar]
- INVOLVE. Briefing notes for researchers: public involvement in NHS, public health and social care research. Eastleigh: INVOLVE; 2012. Available from: http://www.invo.org.uk/resource-centre/libraries/publications-by-involve/ [Google Scholar]
- Global Advocacy for HIV Prevention. Good Participatory Practice Guidelines. 2011. Available from: http://www.avac.org/good-participatory-practice.
- Belone L, Lucero JE, Duran B, Tafoya G, Baker EA, Chan D, et al. Community-based participatory research conceptual model: Community partner consultation and face Validity. Qual Health Res. 2016;26(1):117–135. doi: 10.1177/1049732314557084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, Griffith D, et al. Community-based participatory research: Assessing the evidence. Evid Rep Technol Assess (Summ) 2004. pp. 1–8. [PMC free article] [PubMed]
- Selby JV, Forsythe L, Sox HC. Stakeholder-Driven Comparative Effectiveness Research: An Update From PCORI. JAMA. 2015;314(21):2235–2236. doi: 10.1001/jama.2015.15139. [DOI] [PubMed] [Google Scholar]
- Reay H, Arulkumaran N, Brett SJ. Priorities for future intensive care research in the UK: results of a James Lind Alliance Priority Setting Partnership. J Intens Care Soc. 2014;15(4):288–296. doi: 10.1177/1751143715609954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald HL, Leykum LK, Mattison ML, Vasilevskis EE, Meltzer DO. A patient-centered research agenda for the care of the acutely ill older patient. J Hosp Med. May. 2015;10(5):318–327. doi: 10.1002/jhm.2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient-Centered Outcomes Research Institute. How We Select Research Topics. PCORI website. 2017. Available from: http://www.pcori.org/research-results/how-we -select-research-topics.
- James Lind Alliance. James Lind Alliance Guidebook. 2004. Available from: http://www.jlaguidebook.org/
- INVOLVE. Strategies for diversity and inclusion in public involvement: Supplement to the briefing notes for researchers. Eastleigh: INVOLVE; 2012. Available from: http://www.invo.org.uk/wp-content/uploads/2012/06/INVOLVEInclusionSupplement1.pdf. [Google Scholar]
- Reverby SM. Listening to narratives from the Tuskegee syphilis study. Lancet. 2011;377(9778):1646–1647. doi: 10.1016/s0140-6736(11)60663-6. [DOI] [PubMed] [Google Scholar]
- Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25:626–632. doi: 10.1136/bmjqs-2015-004839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman RE, Butler AS. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: Institute of Medicine, The National Academies Press; 2007. [PubMed] [Google Scholar]
- MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol. 2011;35(4):200–208. doi: 10.1053/j.semperi.2011.02.017. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Heck K, Egerter S, Marchi KS, Dominguez TP, Cubbin C, Fingar K, Pearson JA, Curtis M. The role of socioeconomic factors in Black-White disparities in preterm birth. Am J Public Health. Apr. 2015;105(4):694–702. doi: 10.2105/AJPH.2014.302008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker Edmonds B, Mogul M, Shea JA. Understanding low-income African American women's expectations, preferences, and priorities in prenatal care. Fam Comm Health. 2015;38(2):149–157. doi: 10.1097/FCH.0000000000000066. [DOI] [PubMed] [Google Scholar]
- Duley L, Uhm S, Oliver S Preterm Birth Priority Setting Partnership Steering Group. Top 15 UK research priorities for preterm birth. Lancet. 2014;383(9934):2041–2042. doi: 10.1016/S0140-6736(14)60989-2. [DOI] [PubMed] [Google Scholar]
- Ulm S, Crowe S, Dowling I, Oliver S. The process and outcomes of setting research priorities about preterm birth - a collaborative partnership. Infant. 2014;10(6):178–181. [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Frank L, Forsythe L, Ellis L, Schrandt S, Sheridan S, Gerson J, Konopka K, Daugherty S. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research institute. Qual Life Res. 2015;24(5):1033–1041. doi: 10.1007/s11136-014-0893-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


