Abstract
Gastroesophageal reflux disease (GERD) is a major digestive health problem with a high and increasing incidence worldwide. Peroral endoscopic cardial constriction (PECC) was developed by our group to provide a less invasive treatment for GERD.
In this preliminary follow-up study, 16 patients were enrolled and 13 patients with GERD were targeted for analysis according to the Los Angeles classification of reflux esophagitis. The GERD health-related quality of life (GERD-HRQL) scale and esophageal pH monitoring were applied to assess clinical efficiency at 3 and 6 months after PECC treatment, respectively.
All GERD patients successively received PECC, and no severe treatment-related complication was reported. Before PECC treatment, the GERD-HRQL scale was 19.92 ± 7.89. At 3 and 6 months after treatment, the GERD-HRQL scale was 4.46 ± 4.31 and 5.69 ± 5.07, respectively. DeMeester score was 125.50 ± 89.64 before PECC treatment, and 16.97 ± 12.76 and 20.32 ± 15.22 at 3 and 6 months after PECC treatment. Furthermore, the fraction time of a pH below 4 significantly decreased at 3 and 6 months after PECC treatment. Fraction time at pH <4 was 35.55 ± 26.20 before PECC treatment and 7.96 ± 13.03 and 4.72 ± 3.78 at 3 and 6 months after PECC treatment, respectively. These results suggest that PECC treatment could significantly reduce the GERD-HRQL scale and DeMeester score (P < .01).
PECC is a feasible, safe, and effective method to treatment GERD through narrowing the diameter of the cardia and preventing the reflux of stomach contents.
Keywords: endoscopic treatment, gastroesophageal reflux disease (GERD), peroral endoscopic cardial constriction (PECC)
1. Introduction
Gastroesophageal reflux disease (GERD) is a common chronic disease that has a variety of clinical manifestations. Typical symptoms include acid reflux and heartburn, which impair life quality. Efficient therapy for GERD may decrease the incidence of GERD-related complications and improve life quality. Therapeutic approaches to GERD include lifestyle modification, medical therapy, endoscopic therapies, and surgical treatments.[1] Due to economic burden, complications of pharmacological treatments and complications of surgical treatments, GERD therapy remain as a challenge.[2–5] Proton pump inhibitors (PPIs) and laparoscopic fundoplication were used constantly for GERD by the main mechanism to inhibit the secretion of gastric acid and anti-reflux effect in esophagogastric junctions. However, PPIs had a poor curative effect and easy recurrence after treatment for some patients.[6] The laparoscopic gastric folding technique can solve the problems of the recurrent symptoms because of its high surgical trauma and the problem of adverse reactions and poor patient compliance. During the development of endoscopic treatment technology, endoscopic radiofrequency and endoscopic gastroplasty replaced traditional treatment minimally invasive technongy.[7–9] Peroral endoscopic cardial constriction (PECC) is new endoscopic technology that is less invasive for GERD. The basic principle of PECC is the ligation of the mucosa, the necrosis of inherent muscular at the submucosal part to form the scarring to increase lower esophageal sphincter (LES) pressure and narrowing of the cardia. In this preliminary study, a new mini-invasive treatment, PECC, was applied to GERD patients to evaluate its safety and short-time clinical efficacy.
2. Patients and methods
2.1. Study design
This study began in March 2014, after which a preliminary follow-up study was conducted until April 2015 on patients treated with PECC in the initial single center. Approval for these studies was granted by the medical ethics committee of Chinese PLA General Hospital (S2013–119–02) and Chinese Clinical Trial Registration (ChiCTR-TRC-14004796). Written informed consent was obtained from all patients. An approval was obtained before the start of the original study and another one was obtained during the short-term follow-up period. All patients have been treated with PPI treatment, and symptoms of the patient are repeated. We compared 24-hour esophageal PH monitoring, esophageal kinetics testing, endoscopy, gastro-esophageal reflux disease-questionnaires, and gastroesophageal reflux disease-health related quality of life before and after surgery. The results were compared with the currently accepted PPI efficacy (standard control). We were enrolled in 16 patients, one of which gave up follow-up to conduct laparoscopic fundoplication in the local hospital. The other 2 patients were missing a review result. So, three cases were removed. The primary study objective was to determine the safety and efficacy of PECC for the treatment of symptomatic GERD. Primary 3- and 6-month efficacy was determined through analysis of the validated GERD-HRQL[10,11] and esophageal pH monitoring. The study design summary is summarized in Tables 1 and 2.
Table 1.
Study design.
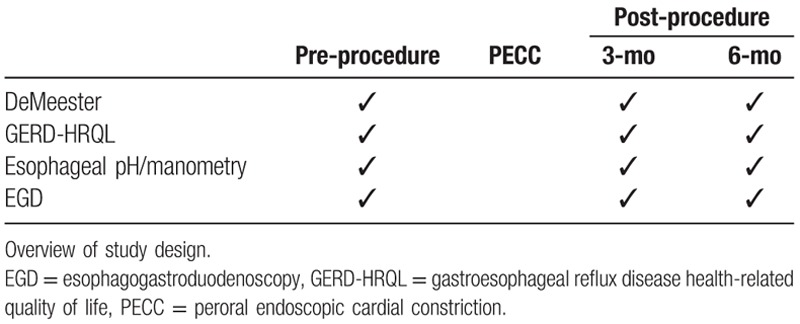
Table 2.
The GERD-HRQL instrument.
2.2. Study eligibility
Patients with a history of heartburn or regurgitation requiring daily PPI therapy were eligible. In addition, all patients met the following inclusion criteria: patients with chronic GERD (>6 months) with typical symptoms (acid regurgitation, heartburn); patients who were aged 18 to 75 years; patients with pathological 24-hour esophageal pH monitoring; patients with a DeMeester score >30.0; patients with normal or hypotonic LES pressure (>5 mm Hg); and patients with recurring typical symptoms and/or not been relieved after 2 months of systematic medical therapy.
Exclusion criteria for the procedure were as follows: patients with Barrett epithelium or early-stage esophagus cancer diagnosed by pathological biopsy; patients with previous endoscopic or surgical anti-reflux procedure and pregnancy; patients with a hiatal hernia diameter of >3 cm; patients with severe cardiopulmonary and infection; patients with nonerosive reflux disease (NERD); PPI was used more than 3 times, and continuous use of PPI for more than 3 days would be removed; and exclude other esophageal motility disorders.
2.3. Baseline assessment and follow-up
During the baseline evaluations, patients completed the gastroscopy, GERD-HRQL, ambulatory pH studies, and esophageal manometer at pre-procedure (Table 3). Baseline upper endoscopy was performed to determine hiatal hernia size and esophagitis grade. The GERD-HRQL score assessed heartburn severity and the impact of GERD-specific symptoms on the quality of life of the patient using the scale. Primary efficacy and treatment response were assessed using the GERD-HRQL score. Patients were considered responsive to PECC treatment at 3 and 6 months when their GERD-HRQL score improved by 50% or more beyond the pretreatment baseline. Ambulatory endoscopy and esophageal manometry were also conducted for patients who had undergone these tests within the previous 6 months. Patients were reevaluated by completing the GERD-HRQL score, endoscopy, esophageal pH, and manometry studies at 3 and 6 months post-procedure. The patients were satisfactory with the improvement of GERD symptoms by telephonic follow-up. Satisfaction: symptom relief rate ≥60%; basic satisfaction: remission rate of 59% to 21%; dissatisfied: remission rate ≤20%. The difference between satisfied and dissatisfied patients was statistically significant 3 months and 6 months before and after surgery.
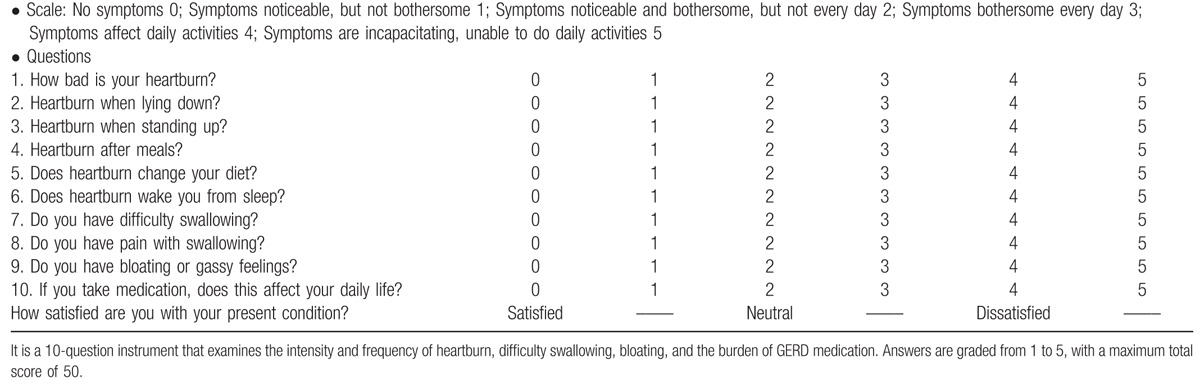
Table 3.
Baseline patient characteristics.
2.4. Peroral endoscopic cardial constriction (PECC) protocol
All procedures were performed in our institution. All procedures were performed by the same endoscopist. The procedure was carried out using a forward-viewing endoscope of outer diameter 9.8 mm (GIFH260; Olympus, Tokyo, Japan) and an endoscopic ligation device (MBL-6-F; COOK Ireland Limited; National Technongy Park Limerick, Ireland) and resolution clips (Resolution Clip; Boston Scientific’corporation, Massachusetts, Natikeshi).
(1) Preparation before procedures: without diet and water for 6 hours.
(2) General anesthesia: All procedures were performed under intravenous propofol and ketamine sedation with the continuous monitoring of vital signs [blood pressure, electrocardiograph (ECG), and SO2; propofol: 6–12 mg/kg per hour; ketamine: 1–2 mg/kg was instituted].
(3) PECC: esophagogastroduodenoscopy (EGD) was performed using a video-endoscope, and esophageal varices ligation equipment was fixed upon endoscopy. Two single-band ligation devices (Fujinon, Japan) were placed at the greater curvature and lesser curvature of the far-end of the esophagus under endoscopy guidance, respectively. The first plication was positioned approximately 1.0 cm above the cardia along the lesser curvature. A second plication was placed 1.0 cm above greater curvature.
(4) Fixation: fixed the 2 ends of the ligation devices with Resolution clips (Boston Scientific).
(5) Medical therapy after treatment: oral administration of 20 mg of omeprazole twice a day for 2 weeks. The process was performed by 2 experienced digestion physicians.
2.5. Statistical analysis
Primary efficacy was based on the results of the GERD-HRQL questionnaire score. Quantitative data were expressed as mean ± standard deviation (SD). Patients were considered treatment responders if they achieved at least 50% improvement in their 3- and 6-month GERD-HRQL score, compared with their off-medication baseline. The GERD-HRQL and DeMeester score were analyzed using Student 2-tailed t test. P < .05 was considered statistically significant. The PECC treatment was considered a success for a given study outcome when the statistical test rejected the null hypothesis at a 1-sided P value of .05 or less. These statistical analyses were performed using SPSS 17.0 software package (SPSS Inc., Chicago, IL).
3. Results
3.1. Patients and baseline characteristics
Patient baseline characteristics are summarized in Table 3. A total of 13 patients successfully underwent the PECC procedure and completed the 3- and 6-month follow-up. To date, none of these patients reported any severe complication related with the PECC treatment. However, 5 patients experienced slight chest pain symptoms that disappeared 1 day after treatment without medical therapy. The GERD-HRQL scale and esophageal pH monitoring were applied to assess its clinical efficiency at 3 and 6 months after PECC treatment, respectively. The 13 GERD patients who were diagnosed according to the International Consensus of GERD diagnosis and Management for GERD (9 males and 4 females; range: 40–70 years, with a mean 53.31 ± 10.45 years) were enrolled into this preliminary study conducted from March 2014 to April 2015. There were 7 patients with more than 5 years of chronic GERD history and 6 patients with 6 months to 5 years of chronic GERD history. All PECC treatments were performed at our institution with approval from the institutional ethics committee. Written informed consent was obtained from all patients upon enrollment (Figs. 1–3).
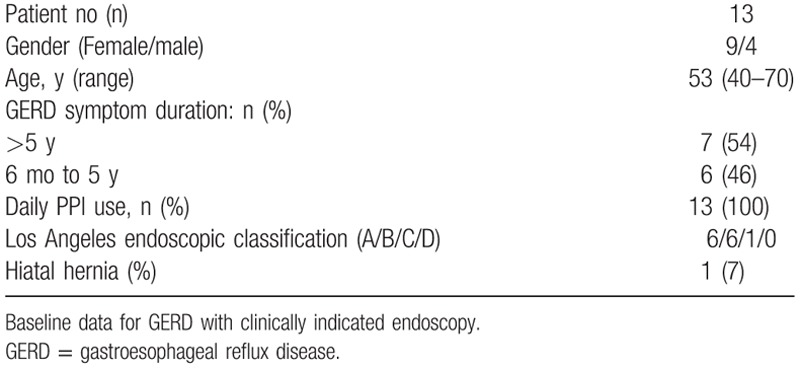
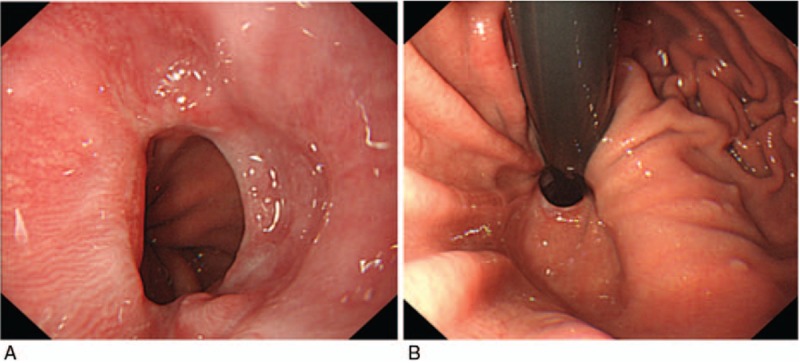
Figure 1.
Move up of dentate line and the relaxation of cardiac ostium were shown under endoscopy in (A), and esophageal hiatus is shown in (B).
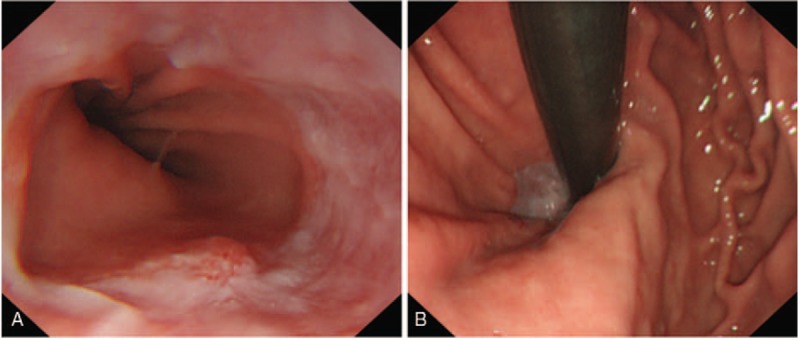
Figure 3.
Chrysanthemum pattern of scars were shown at the greater curvature and lesser curvature of cardia, respectively (A), and the shrink of cardiac ostium under endoscopy (B).
Figure 2.
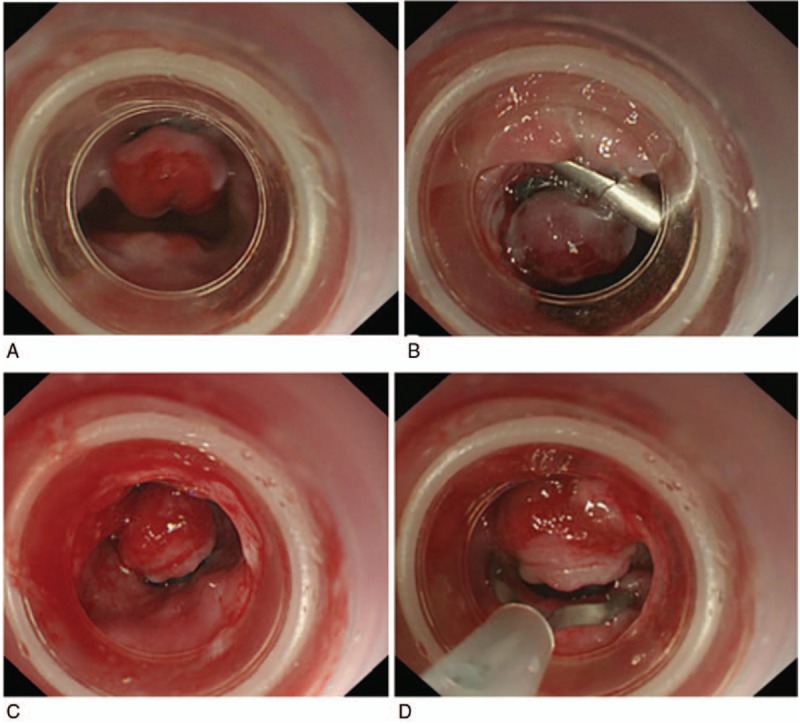
Two single-band ligation devices were placed at the greater curvature and lesser curvature of cardia (A, C) and fixed 2 resolution clips at 2 ends of the ligation devices (B, D).
3.2. Efficiency evaluation and follow-up
The GERD-HRQL questionnaire score, gastroscopy, 24-hour esophageal pH monitoring, and dynamic inspection were used to evaluate short-time clinical efficiency at 3 and 6 months, as well as every 6-month interval, subsequently after PECC treatment, respectively.
3.3. Comparisons of the GERD-HRQL questionnaire score before and 3 and 6 months after PECC treatment in GERD patients
The GERD-HRQL questionnaire score was used to evaluate the frequency and serious degree of heartburn and acid regurgitation for diagnosing GERD in clinic. Although the GERD-HRQL questionnaire score is a subjective index, it reflects the life quality of GERD patients. In this study, GERD-HRQL questionnaire scores decreased significantly after PECC treatment, compared with before. As summarized in Table 4, the mean GERD-HRQL questionnaire score was 18.92 ± 7.89 before PECC treatment, and 4.46 ± 4.31 and 5.69 ± 5.07 at 3 and 6 months after PECC treatment, respectively. There was a significant difference between before and after 3 months and before and after 6 months after PECC treatment (P < .05). Furthermore, there was no significant change in GERD-HRQL scores between 3 and 6 months after PECC treatment (P > .05). This result suggests that PECC treatment could change the life quality of GERD patients, and its clinical efficiency was stable.
Table 4.
Results of 24-h esophageal pH monitoring and GERD-HRQL.
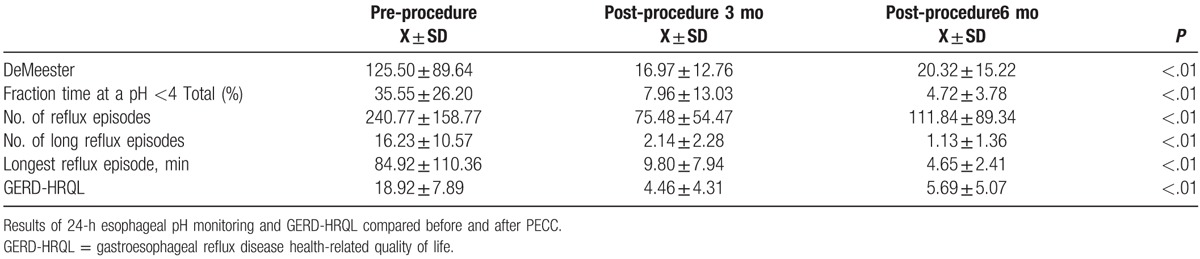
3.4. Comparisons of results of 24-hour esophageal pH monitoring before and at 3 and 6 months after PECC treatment in GERD patients
The DeMeester score (composite score of pH <4 for upright, recumbent and total, number of reflux episodes in 24 hours, number of reflux episodes >5 minutes, and the longest episode) is used by many gastroenterologists and gastrointestinal surgeons in the final interpretation of pH-metry.[12] The DeMeester score is an objective index to reflect the severity of GERD, and is often used to evaluate the clinical efficiency of therapies. In this study, the DeMeester score was detected to have a significant decreasing trend after PECC treatment in GERD patients compared with before treatment. The DeMeester score was 125.50 ± 89.64 before PECC treatment, and 16.97 ± 12.76 and 20.32 ± 15.22 at 3 and 6 months after PECC treatment, respectively. Furthermore, the difference between before treatment and at 3 months after PECC treatment, as well as before treatment and at 6 months after PECC treatment was statistically significant (P < .05). However, there was no significant changes between 3 and 6 months after PECC treatment in DeMeester scores (P > .05). In the pre-procedure esophageal pH monitoring of patients, the fraction times of a pH of <4 was 35.55 ± 26.20. This indicates the presence of severe acid reflux. Furthermore, these were 7.96 ± 13.03% and 4.72 ± 3.78% at 3 and 6 months post-procedure, respectively. Moreover, for the number of reflux episodes, the number of long reflux episodes, and the longest reflux episode, these results suggest that PECC treatment could change the status of gastric acid secretion and the acid environment of the esophagus in GERD patients, and clinical efficiency was stable.
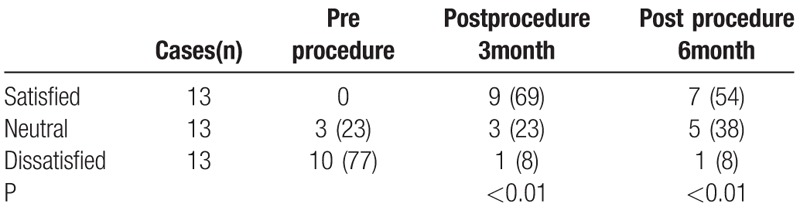
3.5. Patient satisfaction at baseline
For patients on GERD medications, 77% of these patients were dissatisfied with the management of their GERD symptom. At 3 and 6 months post-treatment, 69% and 54% of patients reported satisfaction with the management of their GERD symptom, respectively (Table 5). Patients satisfaction had significant differences at the follow-up times compared with preoperational ones (P < .01) (Table 6).
Table 5.
Patient satisfaction.
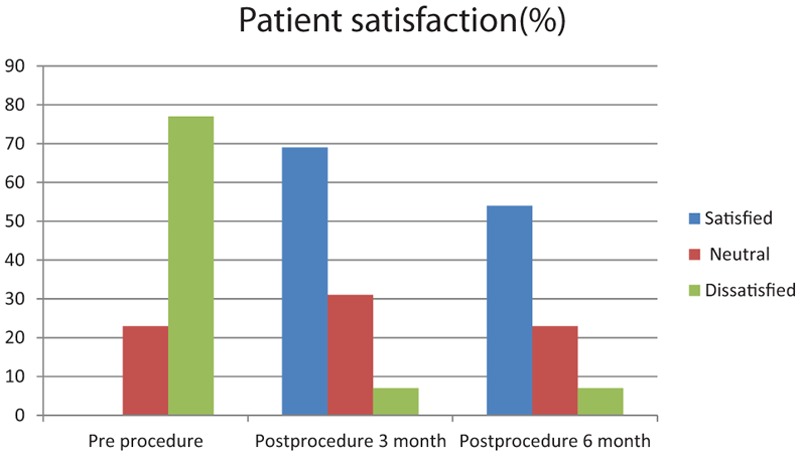
Table 6.
Patient satisfaction (n%).
3.6. Safety
There was no serious complication or death in our study. After PECC, a slight retrosternal pain and dysphagia occurred in 3 patients (13%). Endoscopy at 1 year after PECC revealed that the mucosal breaks disappeared in patients.
4. Discussion
GERD is a major digestive health problem due to its high and increasing incidence and its serious complications. Furthermore, it is one of the most frequent causes of gastroenterological consultations in out-patients, which significantly compromises the quality of life of patients.[13] The management for GERD includes lifestyle modifications and weight reduction, anti-reflux medications and reduction of gastric acidity, endoscopic radiofrequency ablation and fundoplication, and laparoscopic fundoplication.[14–17] Although these treatments have improved the prognosis of GERD, the management of GERD patients remains a very challenging task. For long-term complications and the economic burden brought about by anti-reflux medications and transient LES reducers led to the reduction of quality of life and brought inconveniences to the life of patients. The causes of GERD may include the following aspects. At first, reflux was synonymous with esophagitis and hiatus hernia. Second, it was a motility disorder defined by sphincter or peristaltic dysfunction. Third, it was an acid-peptic disorder. PECC is a new endoscopic method. The mechanism of PECC is through narrowing the diameter of the cardia, increasing the pressure of the esophageal sphincter, and preventing the reflux of stomach contents. In this preliminary study, there was no serious treatment-related complication reported. This suggests that PECC is a feasible and safe method for the treatment GERD. GERD-HRQL scores and results of 24-hour esophageal pH monitoring are commonly used in diagnoses and the evaluation of the efficiency of subjective and objective indexes in clinic.[18–21] Hence, in this study, we analyzed the 2 indexes to assess the clinical efficiency of PECC for the treatment GERD. Results revealed that GERD-HRQL scores and results of the 24-hour esophageal pH monitoring significantly decreased after PECC, and clinical efficiency lasted for a long period of time. Furthermore, the frequency and degree of heartburn and acid regurgitation in GERD patients was reduced, and the quality of life of patients was significantly improved. In addition, DeMeester scores were reduced by PECC, which was reflected by the 24-hour esophageal pH monitoring and was an index for the acid environment in the esophagus. All these results suggest that PECC is an efficient method for the treatment GERD. For 2 GERD patients, the evaluation of the GERD-HRQL score decreased, but the DeMeester score increased. The reason may be the examination sequence of 24-hour esophageal pH monitoring and gastroscopy. For 2 patients, the gastroscopy examination was performed before the 24-hour esophageal pH monitoring. On the first day, esophageal motility and 24-hour esophageal PH monitoring was conducted on the patient. On the second day, after completing the 24-hour esophageal PH monitoring, patients underwent endoscopy in order to avoid endoscopic stimulation of vomiting, which could cause a transient esophageal kinetics, to change the effect of the inspection.
Inoue et al[22] described the technique of the anti-reflux mucosectomy (ARMS) procedure that targets circumferential mucosectomy at the cardia to induce constriction and reduce acid reflux. There are similarities with PECC. The incidence of postoperative stenosis was higher in ARMS, especially in circumferential ARMS. The surface of the wound in ARMS was larger, and operation time was longer, which even lasted for 176 minutes, while the operation time for PECC was shorter. Operating time on average was 76 minutes (42–124 minutes, n = 3) in the piecemeal EMR group and 127 minutes on average (98–176 minutes, n = 7) in the ESD group. PECC is simple and easy to put into effect, and it can relieve reflux symptoms effectively.
The main factor influencing the efficacy was the depth of ligation, so we conducted animal experiments on the depth of ligation. Ligation technology is very mature, which has been widely used in endoscopic varicose veins ligation, esophageal intraepithelial neoplasia EMR. Because the depth of ligation is the main factor affecting the therapeutic effect, we have done animal experiments on the depth of ligation.
There are several limitations in this study. First, this is a preliminary clinical study and the number of GERD patients is relatively small. Only 13 patients were targeted for analysis of 16 patients who were enrolled in this study. Hence, further studies should enlarge the sample size and add comparison group to draw more convictive conclusions about PECC. Second, patients were followed up for a short observation period. A long-term follow-up is needed to prove the feasibility, safety, adverse reaction, and curative effect. Third, more evaluation measures and consistency standard procedure should be established to assess for clinical efficiency and decrease bias for endoscopist and estimator so as to be clinically popularized and applied.
In conclusion, PECC is a new endoscopic method, and its mechanism is through narrowing the diameter of the cardia, increasing the pressure of the esophageal sphincter, and preventing the reflux of stomach contents. In this preliminary study, results suggest that PECC is a feasible, safe, and efficient method for the treatment of GERD.
Author contributions
Conceptualization: H-Q. Hu.
Data curation: E-Q. Ling-Hu, H-Q. Hu, H-K. Li, J-L. Zhi, X-B. Zhang, X-X. Wang, Y. Xiong.
Formal analysis: J-L. Zhi, X-X. Wang.
Funding acquisition: J-L. Zhi, X-X. Wang.
Methodology: H-K. Li, J-L. Zhi, X-B. Zhang, X-X. Wang, Y. Xiong.
Validation: H-K. Li, Y. Xiong.
Writing – original draft: H-Q. Hu.
Writing – review & editing: E-Q. Ling-Hu, H-Q. Hu.
Footnotes
Abbreviations: ECG = electrocardiograph, EGD = esophagogastroduodenoscopy, ESD = endoscopic submucosal dissection, GERD = gastroesophageal reflux disease, GERD-HRQL = gastroesophageal reflux disease health-related quality of life, LES = lower esophageal sphincter, PECC = peroral endoscopic cardial constriction.
H-QH and H-KL these two authors equally contributed to this work.
The authors have no conflict of interest.
References
- [1].Henry MA. Diagnosis and management of gastroesophageal reflux disease. Arq Bras Cir Dig 2014;27:210–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Subramanian CR, Triadafilopoulos G. Refractory gastroesophageal reflux disease. Gastroenterol Rep 2015;3:41–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Singhal V, Khaitan L. Gastroesophageal reflux disease: diagnosis and patient selection. Indian J Surg 2014;76:453–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Takeuchi T, Oota K, Harada S, et al. Characteristics of refractory gastroesophageal reflux disease (GERD) symptoms: is switching proton pump inhibitors based on the patient's CYP2C19 genotype an effective management strategy? Intern Med 2015;54:97–105. [DOI] [PubMed] [Google Scholar]
- [5].Becher A, El-Serag H. Systematic review: the association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2011;34:618–27. [DOI] [PubMed] [Google Scholar]
- [6].Subramanian CR, Triadafilopoulos G. Refractory gastroesophageal reflux disease. Gastroenterol Rep (Ofx) 2015;3:41–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Galmiche JP, Hatlebakk J, Attwood S, et al. Laparoscsopic antireflux surgery vs esomeprazole treatment for chronic GERD, the LOTUS randomized clinical trial. JAMA 2011;5:1969–77. [DOI] [PubMed] [Google Scholar]
- [8].Tam WC, Schoeman MN, Zhang Q, et al. Delivery of radiofrequency energy to the lower oesophageal sphincter and gastric cardia inhibits transient lower oesophageal sphincter relaxations and gastro-oesophageal reflux in patients with reflux disease. Gut 2003;52:479–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Aziz AM, El-Khayat HR, Sadek A, et al. A prospective randomized trial of sham, single-dose Stretta, and double-dose Stretta for the treatment of gastroesophageal reflux disease. Surg Endosc 2010;24:818–25. [DOI] [PubMed] [Google Scholar]
- [10].Lippmann QK, Crockett SD, Dellon ES, et al. Quality of life in GERD and Barrett's esophagus is related to gender and manifestation of disease. Am J Gastroenterol 2009;104:2695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 2007;20:130–4. [DOI] [PubMed] [Google Scholar]
- [12].Mainie I, Tutuian R, Castell DO, et al. Comparison between the combined analysis and the DeMeester score to predict response to PPI therapy. J Clin Gastroenterol 2006;40:602–5. [DOI] [PubMed] [Google Scholar]
- [13].Yadlapati R, Gawron AJ, Bilimoria K, et al. Development of quality measures for the care of patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2015;13:874–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Henry MA. Diagnosis and management of gastroesophageal reflux disease. Arq Bras Cir Dig 2014;2013:210–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bredenoord AJ, Pandolfino JE, Smout AJ. Gastro-oesophageal reflux disease. Lancet 2013;381:1933–42. [DOI] [PubMed] [Google Scholar]
- [16].Boeckxstaens G, El-Serag HB, Smout AJ, et al. Symptomatic reflux disease: the present, the past and the future. Gut 2014;63:1185–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Fass R. Therapeutic options for refractory gastroesophageal reflux disease. J Gastroenterol Hepatol 2012;27:3–7. [DOI] [PubMed] [Google Scholar]
- [18].El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014;63:871–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2013;108:308–28. [DOI] [PubMed] [Google Scholar]
- [20].Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006;101:1900–20. [DOI] [PubMed] [Google Scholar]
- [21].Mainie I, Tutuian R, Castell DO. Comparison between the combined analysis and the DeMeester Score to predict response to PPI therapy. J Clin Gastroenterol 2006;40:602–5. [DOI] [PubMed] [Google Scholar]
- [22].Inoue H, Ito H, Ikeda H. Anti-reflux mucosectomy for gastroesophageal reflux disease in the absence of hiatus hernia: a pilot study. Ann Gastroenterol 2014;27:346–51. [PMC free article] [PubMed] [Google Scholar]


