Abstract
Total ankle replacement (TAR) is a valid option for the treatment of ankle osteoarthritis. The traditional surgical approach for TAR is the anterior approach. Recently, the lateral transfibular approach to the ankle has gained popularity since a new TAR implant was designed to be performed via this approach that results in an ideal visualization of the center of rotation of the ankle and curved resections that allow for sparing bone cuts. The aim of the present paper is to present our preoperative, operative, and postoperative protocols for the treatment of the osteoarthritis of the ankle with TAR via lateral approach. We present our preoperative clinical and radiographic protocol. In addition, we describe our surgical technique with some technical tips. Finally, we report our follow-up schedule that includes the collection of clinical, functional, and radiographic data. The results of this procedure are encouraging: TAR through a lateral transfibular approach provides reliable pain relief and improvements in functional outcomes in patients with ankle osteoarthritis.
Keywords: Behavior, Issue 131, Ankle osteoarthritis, ankle replacement, ankle arthroplasty, lateral approach, fixed bearing, talus
Introduction
The most frequent etiology of ankle osteoarthritis is the post-traumatic origin. In fact, it is often secondary to traumatic injuries that typically affect young patients1,2. Ankle osteoarthritis influences patients' quality of life to the same degree as hip osteoarthritis and even more than knee osteoarthritis3. Ankle fusion has been considered the gold-standard for the treatment of ankle osteoarthritis, but some studies show that it confers augmented stress and increased risk of osteoarthritis of the adjacent joints4,5,6,7; furthermore, there still exist a number of complications associated with ankle fusion, such as equinus or talipes deformity and painful non-union8,9. With the evolution of surgical techniques and implant designs, total ankle replacement (TAR) has become an excellent alternative to ankle fusion for a surgeon with a proper learning-curve10,11,12.
TAR allows the preservation of ankle range of motion and protects from adjacent joint degeneration13. The anterior approach permits an optimal visualization of the coronal alignment; at the same time, this approach is inclined to wound-healing complications14,15. Recently, a novel TAR implant was designed to be performed via the lateral transfibular approach that results in an ideal visualization of the center of rotation and curved resections that allow for sparing bone cuts16; moreover, this approach permits the implantation of components perpendicular to the bone trabeculae, thus limiting the shear forces at the level of the bone-implant interface16. This prosthesis consists of a fixed-bearing implant; an alignment coordinate system guides the bone resections and facilitates addressing both coronal and sagittal deformities17. The early results of ankle arthroplasty using this TAR implant have been published 12,16,17,18. The aim of the present paper is to present our preoperative, operative, and postoperative protocols for the treatment of the osteoarthritis of the ankle with TAR via the lateral approach.
Patient selection starts with a careful clinical examination and history. A medical history of inflammatory or vascular disease, neuropathy or neurologic disease and complicated diabetes may modify the indication. Poor soft tissue envelope of the ankle should be carefully evaluated because it may compromise the wound healing: skin and subcutaneous soft-tissue may already have been compromised from injury or previous surgery. The use of drugs that may influence healing must be considered. Muscle and tendon function, ankle and hindfoot alignment, and ankle range of motion should be evaluated: a detailed examination can indicate whether accessory procedures are needed at the time of surgery19.
We suggest always discussing the expectations of the patient concerning the outcomes of the procedure and the need for compliance with post-operative care. TAR is indicated for patients with an ankle joint disease due to post-traumatic, rheumatoid, or primary arthritis not responsive to conservative options that include physical therapy, activity modification, and non-steroidal anti-inflammatory drugs19. Also, lateral ankle instability may represent a cause of joint degeneration defined as ligamentous posttraumatic ankle osteoarthritis20. In addition, secondary osteoarthritis can be associated with systemic diseases: avascular necrosis of the talus, gout, hemophilia, post-infectious arthritis, and hereditary hemochromatosis21,22,23,24.
During the preoperative consultation, we routinely record the following clinical and functional scores: American Orthopaedic Foot & Ankle Society (AOFAS) ankle and hindfoot score25,26,27, 12-Item Short Form Health Survey27,28, and Visual Analogue scale (VAS) pain score29.
Protocol
All methods described have been approved by our institutional review board and the local ethics committee and they have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
1. Preoperative Radiographic Evaluation
Perform weight bearing radiographs of the ankle and the foot with antero-posterior, lateral, and rearfoot alignment views (Saltzman's view30).
Perform a conventional computed tomography (CT) of the ankle and request any other diagnostic exams (such as magnetic resonance), if necessary, to better clarify the diagnosis.
- Measure the following parameters on the preoperative weight-bearing radiographs.
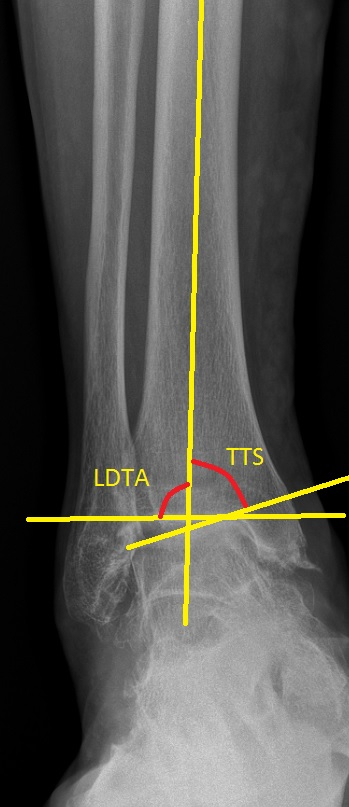
- Measure the lateral distal tibial angle (LDTA, normal value 89.0 ± 3.0 °) on the anteroposterior ankle view: measure the angle subtended between the anatomic axis of the tibia and the line connecting the distal points on the medial and lateral edge of the tibial articular surface (Figure 2)32,33,34.
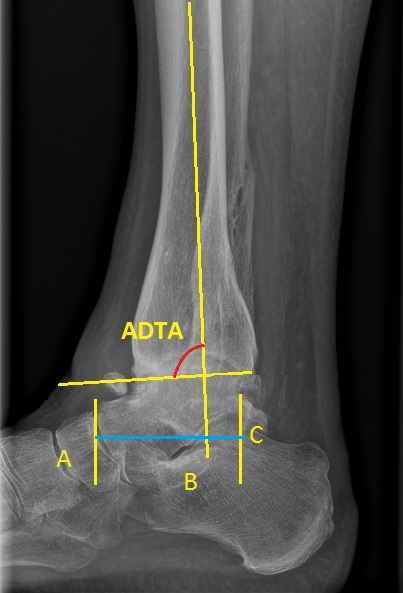
- Measure the tibio-talar ratio (TT ratio, normal value 34.8 ± 3.8%): measure this parameter on the lateral ankle view; it is the ratio between the posterior longitudinal talar length (the length between the posterior talar edge and the intercept of the anatomical tibial axis) and the full longitudinal talar length (Figure 1)33,35,36.
Use the CT to assess the available bone stock and to evaluate the severity of the avascular necrosis of the talus, if present.
2. Surgical Technique17
NOTE: This procedure is performed under general or regional anesthesia (spinal anesthesia).
Place the patient in the supine position with a rigid board under the leg to sustain the alignment stand. Position a thick pad under the ipsilateral hip. Do not use a tourniquet.
Make a longitudinal incision with a scalpel over the lateral malleolus that curves under its tip toward the sinus tarsi (Figure 3). Dissect the fibula and the anterior side of the tibia subperiosteally with the scalpel and the periosteal elevator to obtain a complete view of the osteophytes and the joint.
Release the posterior capsule of the tibia and the fibula using a periosteal elevator.
Make an oblique lateral malleolus osteotomy with a sagittal saw blade: begin from the posterior edge of the fibula, 6-7 cm proximal to the joint line; end on the anterior side of the fibula, 2 cm proximal to the joint line. Rotate the fibular malleolus distally and use a 1.6 mm K-wire to fix it to the calcaneus.
Remove the anterior osteophytes with the sagittal saw blade and a rongeur until the ankle can be easily placed in a neutral position. NOTE: The medial gutter release can be performed later during the tibial preparation.
Measure the medial/lateral talar width with the manufacturer's sizer, choosing the largest size possible while avoiding overhang.
Place the leg in the alignment stand that is assembled at the beginning of the procedure.
Internally rotate the foot and use the trans-calcaneal pin to fix it to the foot plate. Use the 4.0 mm pin to fix the talus to the footplate: put the pin as distal as possible in the talar neck, thus facilitating further correction of talar tilt.
Check the tibial alignment with fluoroscopy using a bar that is parallel to the mechanical tibial axis. Use fluoroscopy with the following parameters: 55 kilovolts, 3 milliampere-seconds.
Insert two 5.0 mm pins on the medial border of the tibia while an assistant pushes the tibia anteriorly if an anterior sagittal talar shifting is present. To increase the rigidity of the construct, an adjunctive carbon fiber bar can be placed in a vertical position.
Verify the level of the desired joint line with the pointer located through the ''Position'' hole of the cutting guide of the selected size. Check the amount of bone resection with the pointer placed in the ''Talus'' and ''Tibia #1'' hole.
Use the 4.0 mm drill through the pre-cutting guide to pre-drill the talus and the tibia surfaces. Assemble the bone burr to the pneumatic handpieces and put the contralateral talar trial of the selected size between the bone burr and the cutting guide to assess the medial depth of the bone cut. Then, use the bone burr to make the definitive bone cuts through the ''Talus'' and the ''Tibia #1'' holes of the guide. Use the ''Tibia #2'' hole to reach the whole tibial cut on the medial side and to release osteophytes of the medial gutter
Position the rail drill guides. Utilize antero-posterior fluoroscopy to verify they are properly placed to avoid lateral overhang. Drill the rails and position the provisional implant, then choose the insert size.
Insert the definitive implants using the talar and tibial inserter.
Use fluoroscopy to check the positioning, and use two or three 3.5 mm lag screws to fix the fibula; alternatively, use a plate-fixation of the lateral malleolus, if the deformity requires a malleolar lengthening or shortening that does not leave sufficient contact for screw fixation.
Check the stability of the syndesmosis with a bone hookapplied to the lateral malleolus. Gently pull the fibula laterally to assess any residual tibiofibular instability. If a lateral movement of the lateral malleolus is present, stabilize it with a syndesmosis screw fixation across four cortices. Test the ankle range of motion.
Repair the anterior talofibular ligament with resorbable suture before routine wound-closure.

3. Postoperative Care
Place the leg into a cast and forbid weight-bearing for four weeks. Then allow weight-bearing with a walker-boot for two weeks.
Allow calf strengthening, proprioceptive training and stretching of the triceps surae six weeks after the surgery.
4. Clinical and Radiographic Follow-Up
Radiologically and clinically evaluate patients at one, two, six, and twelve months after the procedure and, afterward, every twelve months. The follow-up protocol consists of function and pain assessment with SF-12, VAS pain score, and AOFAS ankle and hindfoot scores collected at each time-point.
Perform radiographic examination: request weight-bearing radiographs of the ankle and of the foot with antero-posterior, lateral and Saltzman's view at each end-point.
- Measure the following parameters on the postoperative radiographs at each end-point.
- Measure the Tibio-talar ratio.
- Measure the Tibio-talar surface angle.
Representative Results
We collected the results of a consecutive series of 114 patients (114 ankles) who underwent TAR via lateral transfibular approach between May 2013 and July 2016. All operative procedures were carried out by the senior author.
Data were analyzed with a statistical software (see Table of Materials). The ANOVA and kappa tests were performed40,41. For k-score, the 95% confidence intervals were defined. We considered p-values for tests significant at p<0.05.
The mean AOFAS hindfoot score improved from 32.2 preoperatively (range 7-67) to 85.2 at the latest follow-up (range 59-100). The average Physical Health Composite Scale (PCS) of the SF-12 score improved from 30.7 preoperatively (range 19.4-53.6) to 44.9 at the latest follow-up (range 21.9-61.9); the average Mental Health Composite Scale (MCS) of the SF-12 score improved from 44.3 preoperatively (range 23.5-71.4) to 49.9 at the latest follow-up (range 35.0-65.2). The mean VAS pain score improved from 8.4 preoperatively (range 4-10) to 2.1 at the latest follow-up (range 0-6).
The differences between the preoperative scores and the follow-up scores were statistically significant. A summary of the representative results is provided in Table 1.
Figure 1. Preoperative measurements on lateral weight-bearing radiographs. Lateral weight-bearing ankle view of a patient with ankle osteoarthritis. The following measurements are marked: anterior distal tibial angle and tibio-talar ratio. ADTA: anterior distal tibial angle, the angle traced between the line that connects the anterior and posterior tibial edges at the level of the articular surface and the axis of the tibia. Tibio-talar ratio: draw a segment parallel to the ground starting from the posterior edge of the talus (C, corresponding to the intersection of the calcaneal cortex with the posterior subtalar surface) to the anterior edge of the talus (A, corresponding to the projection of the anterior edge of the talus onto the straight line); this segment is divided into two further segments by the axis of the tibia; the tibio-talar ratio is the ratio of the length of the posterior talar segment (BC) to the longitudinal length of the talus (AC), expressed as a percentage. Postoperative tibio-talar ratio is measured with the same technique.
Figure 2. Preoperative measurements on antero-posterior weight-bearing radiographs. Antero-posterior weight-bearing ankle view of a patient with ankle osteoarthritis. The following parameters are measured: the lateral distal tibial angle and the tibio-talar surface angle. LDTA: lateral distal tibial angle, the lateral angle between the tibial axis and the straight line that connects the medial and lateral points of the articular surface of the tibia. Tibio-talar surface angle: the angle subtended medially by the tibial axis and the straight line that connects the medial and lateral edges of the talar articular surface. The postoperative tibio-talar surface angle is measured with the same technique.
Figure 3. Skin incision for lateral transfibular approach to the ankle. The incision is made along the lateral malleolus curving toward the sinus tarsi.
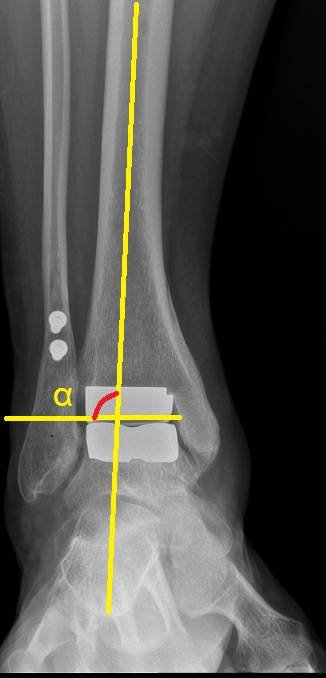
Figure 4. Antero-posterior weight-bearing control radiographs. Postoperative antero-posterior weight-bearing ankle view of TAR implanted through lateral transfibular approach 6 months after the surgery. The following measurement is marked: alpha angle. α: alpha angle, the lateral angle between the anatomical axis of the tibia and the articular surface of the tibial component. The tibio-talar surface angle is also measured during the follow-up with the same technique shown in Figure 2.
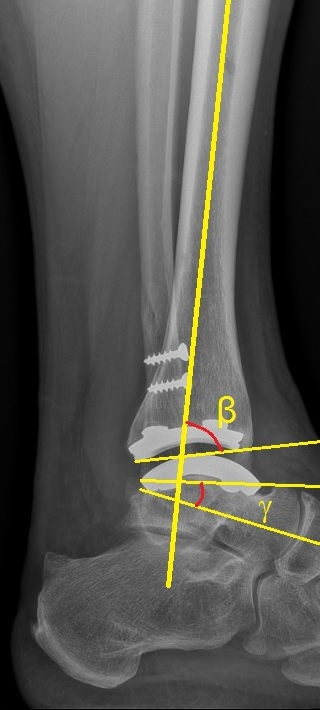
Figure 5. Lateral weight-bearing control radiographs. Postoperative lateral weight-bearing ankle view of TAR implanted through lateral transfibular approach 6 months after the surgery. The following measurements are marked: beta angle, gamma angle. β: beta angle, the angle subtended anteriorly by the anatomical axis of the tibia and the articular surface of the tibial component. γ: gamma angle, it is subtended by a segment connecting the anterior and the posterior points of the talar component and a straight line drawn along the longitudinal axis of the neck of the talus. The tibio-talar ratio is also measured during the follow-up with the same technique shown in Figure 1.
| Preoperative mean (range) | Postoperative mean (range) | p-value | |
| AOFAS | 32.2 (7-67) | 85.2 (59-100) | < 0.001 |
| VAS | 8.4 (4-10) | 2.1 (0-6) | < 0.001 |
| SF-12 PCS | 30.7 (19.4-53.6) | 44.9 (35.0-65.2) | < 0.001 |
| SF-12 MCS | 44.3 (23.5-71.4) | 49.9 (35.0-65.2) | < 0.001 |
Table 1. Summary of the representative results. Comparison of preoperative clinical scores and postoperative clinical scores. Data is presented as mean (range). AOFAS: American Orthopaedic Foot & Ankle Society (AOFAS) ankle and hindfoot score. VAS: Visual Analogue scale pain score. SF-12 PCS: Physical Health Composite Scale of the 12-Item Short Form Health Survey. SF-12 MCS: Mental Health Composite Scale of the 12-Item Short Form Health Survey.
Discussion
We reported the methods and protocol we use performing TAR with lateral transfibular approach. The absolute contraindications for TAR are talar avascular necrosis involving more than 50% of the bone-stock, acute or active infection with or without osteomyelitis, diabetic syndrome with polyneuropathy, high anesthesiologic risks, neuromuscular disorders, peripheral vascular disease, and neuroarthropathy (Charcot arthropathy of the midfoot or hindfoot)19,42. The relative contraindications are diabetic syndrome without polyneuropathy, immunosuppressive therapy and severe osteoporosis19. Patients active in sports and physically demanding activities should be informed about potential increased risk of wear and aseptic loosening43,44,45,46.
We modified the manufacturer's surgical technique with some tips derived from personal experience17. The first modification deals with the incision: the manufacturer's guidelines suggest a straight incision. The straight incision sometimes does not allow for a whole removal of the anterior osteophytes because of a problematic achievement of an appropriate view of the anterior joint line. We prefer to curve the incision toward the sinus tarsi in order to address this problem. This kind of incision permits the removal of all the osteophytes that could obstacle the achievement of the neutral dorsiflexion prior to the bone cuts: this is a key-step to achieve a satisfactory range of motion at the end of the procedure. Moreover, the manufacturer's surgical technique suggests a 1.5-cm oblique fibular osteotomy in the superolateral-inferomedial direction: that kind of osteotomy routinely requires a fixation with the plate and does not require adequate fibular shortening or lengthening for major coronal deformity. We prefer to perform a longer osteotomy beginning at the posterior border of the lateral malleolus (6-7 cm proximal to the joint line), and directing the osteotomy distally toward the anterior border of the lateral malleolus (2 cm proximal to the joint line). This kind of osteotomy facilitates addressing a great number of fibula-length issues and, consequently, a great number of coronal malalignments. Also, it permits a fixation with lag screws, decreasing the risk of hardware removal consequent to subjective discomfort or impaired wound healing. Despite these advantages, the adherences between fibular malleolus and the adjacent soft tissues could make the reflection of the lateral malleolus more complicated in case of long fibular osteotomy. Moreover, the manufacturer's surgical technique includes the use of cement to fix the implants. However, we do not cement the components because an appropriate stability is normally obtained without cementation. Furthermore, the osseointegration features of the implants' material ensure a stable and durable fixation.
Additionally, the manufacturer's guidelines consider the exposure of the medial gutter as part of the surgical technique, while we reserve it only in those cases in which osteophytes are present after the ''Tibia #2'' cut. In fact, the bone cutting through the ''Tibia #2'' hole of the resection guide usually offers a sufficient cleaning of the medial gutter avoiding a medial impingement.
The main limitation of this technique is that the lateral transfibular approach required systematically a fibular malleolus osteotomy that is not routinely necessary in TAR performed through an anterior approach47. The disadvantages are: a lengthening of the operative time (also in consideration of the need for fibular fixation at the end of the procedure) and the risk of subsequent hardware removal in case of patient discomfort. Despite these disadvantages, the fibular osteotomy allows the management of the coronal malalignments consequent to fibula-length issues. Moreover, the osteotomy technique presented in our protocol usually allows for a stable fixation with screws alone, thus dramatically decreasing the need for further hardware removal due to plate discomfort, even if it makes the fibular reflection more complicated. Another limitation is that, though some studies regarding the results of TAR with lateral transfibular approach have already been published, the encouraging results of this technique must be confirmed by long-term follow-up studies12,16,17,18.
A critical step of this protocol is a correct preoperative evaluation in order to properly plan the surgical procedure. The preoperative clinical and radiographic evaluation aims to identify any foot and ankle malalignment that should be addressed in order to achieve a well-balanced implant. Restoring the appropriate position of the tibial and talar components and the correct foot and ankle alignment are essential for the long-term success of the implant35,48,49. Another critical step is represented by the postoperative care: postoperative steps must be carefully followed in order to protect the healing of fibular osteotomy and to avoid early postoperative complications.
In conclusion, in consideration of the early results of this prosthesis reported in previous studies16,17, and of the functional and postoperative pain scores reported in this article, the treatment of ankle osteoarthritis with TAR via lateral transfibular approach can provide reliable pain relief and improvements in range of motion and functional outcomes.
Disclosures
Dr. Usuelli receives grants and personal fees from Zimmer. Dr. D'Ambrosi, Dr. Maccario, Dr. Manzi and Dr. Indino have nothing to disclose.
Acknowledgments
The procedures are performed using the Zimmer Trabecular Metal Total Ankle prosthesis (Zimmer, Warsaw, IN).
References
- Saltzman CL, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46. [PMC free article] [PubMed] [Google Scholar]
- Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Rel Res. 2009;467:1800–1806. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raikin SM, Rasouli MR, Espandar R, Maltenfort MG. Trends in treatment of advanced ankle arthropathy by total ankle replacement or ankle fusion. Foot Ankle Int. 2014;35:216–224. doi: 10.1177/1071100713517101. [DOI] [PubMed] [Google Scholar]
- Abdo RV, Wasilewski SA. Ankle arthrodesis: a long-term study. Foot Ankle. 1992;13:307–312. doi: 10.1177/107110079201300602. [DOI] [PubMed] [Google Scholar]
- Lynch AF, Bourne RB, Rorabeck CH. The long-term results of ankle arthrodesis. J Bone Joint Surg Br. 1988;70:113–116. doi: 10.1302/0301-620X.70B1.3339041. [DOI] [PubMed] [Google Scholar]
- Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979;61:964–975. [PubMed] [Google Scholar]
- Takakura Y, Tanaka Y, Sugimoto K, Akiyama K, Tamai S. Long-term results of arthrodesis for osteoarthritis of the ankle. Clin Orthop Relat Res. 1999;361:178–185. doi: 10.1097/00003086-199904000-00023. [DOI] [PubMed] [Google Scholar]
- Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for posttraumatic arthritis. J Bone Joint Surg Am. 2001;83:219–228. doi: 10.2106/00004623-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Felix NA, Kitaoka HB. Ankle arthrodesis in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1998;349:58–64. doi: 10.1097/00003086-199804000-00008. [DOI] [PubMed] [Google Scholar]
- Daniels TR, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96:135–142. doi: 10.2106/JBJS.L.01597. [DOI] [PubMed] [Google Scholar]
- Zaidi R, et al. The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J. 2013;95:1500–1507. doi: 10.1302/0301-620X.95B11.31633. [DOI] [PubMed] [Google Scholar]
- Usuelli FG, Maccario C, Pantalone A, Serra N, Tan EW. Identifying the learning curve for total ankle replacement using a mobile bearing prosthesis. Foot Ankle Surg. 2016. In Press. [DOI] [PubMed]
- Valderrabano V, Hintermann B, Niggm BM, Stefanyshyn D, Stergiou P. Kinematic changes after fusion and total replacement of the ankle: part 2: Movement transfer. Foot Ankle Int. 2003;24:888–896. doi: 10.1177/107110070302401203. [DOI] [PubMed] [Google Scholar]
- Bleazey ST, Brigido SA, Protzman NM. Perioperative complications of a modular stem fixed-bearing total ankle replacement with intramedullary guidance. J Foot Ankle Surg. 2013;52(1):36–41. doi: 10.1053/j.jfas.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Myerson MS, Mroczek K. Perioperative complications of total ankle arthroplasty. Foot Ankle Int. 2003;24(1):17–21. doi: 10.1177/107110070302400102. [DOI] [PubMed] [Google Scholar]
- Tan EW, Maccario C, Talusan PG, Schon LC. Early complications and secondary procedures in transfibular total ankle replacement. Foot Ankle Int. 2016;37(8):835–841. doi: 10.1177/1071100716644817. [DOI] [PubMed] [Google Scholar]
- Usuelli FG, Indino C, Maccario C, Manzi L, Salini V. Total ankle replacement through a lateral approach: surgical tips. SICOT J. 2016;2(38) doi: 10.1051/sicotj/2016029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usuelli FG, Maccario C, Indino C, Manzi L, Gross CE. Tibial slope in total ankle arthroplasty: anterior or lateral approach. Foot Ankle Surg. 2016. In Press. [DOI] [PubMed]
- Usuelli FG, et al. Total ankle arthroplasty and secondary hindfoot arthrodesis. Minerva Ortop Traumatol. 2017;68:64–73. [Google Scholar]
- Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61:354–361. [PubMed] [Google Scholar]
- Kofoed H, Sorensen TS. Ankle arthroplasty for rheumatoid arthritis and osteoarthritis: Prospective long-term study of cemented replacements. J Bone Joint Surg Br. 1998;80:328–332. doi: 10.1302/0301-620x.80b2.8243. [DOI] [PubMed] [Google Scholar]
- Cracchiolo A, 3rd, Cimino WR, Lian G. Arthrodesis of the ankle in patients who have rheumatoid arthritis. J Bone Joint Surg Am. 1992;74:903–909. [PubMed] [Google Scholar]
- Doets HC, Brand R, Nelissen RG. Total ankle arthroplasty in inflammatory joint disease with use of two mobile-bearing designs. J Bone Joint Surg Am. 2006;88:1272–1284. doi: 10.2106/JBJS.E.00414. [DOI] [PubMed] [Google Scholar]
- Heide HJ, Schutte B, Louwerens JW, van den Hoogen FH, Malefijt MC. Total ankle prostheses in rheumatoid arthropathy: Outcome in 52 patients followed for 1-9 years. Acta Orthop. 2009;80:440–444. doi: 10.3109/17453670903153568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyton GP. Theoretical limitations of AOFAS scoring system: an analysis using Monte Carlo modeling. Foot Ankle Int. 2001;22(10):779–787. doi: 10.1177/107110070102201003. [DOI] [PubMed] [Google Scholar]
- Kitaoka HB, et al. Clinical rating systems for the ankle- hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- Madeley NJ, et al. Responsiveness and validity of the SF-36, ankle osteoarthritis scale, AOFAS ankle hindfoot score and foot function index in end stage ankle arthritis. Foot Ankle Int. 2012;33(1):57–63. doi: 10.3113/FAI.2012.0057. [DOI] [PubMed] [Google Scholar]
- Jenkinson C, et al. A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med. 1997;19:179–186. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- Saltzman CL, El-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16:572–576. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- Barg A, Elsner A, Chuckpaiwong B, Hintermann B. Insert position in three-component total ankle replacement. Foot Ankle Int. 2010;31:754–759. doi: 10.3113/FAI.2010.0754. [DOI] [PubMed] [Google Scholar]
- Braito M, et al. Effect of coronal and sagittal alignment on outcome after mobile-bearing total ankle replacement. Foot Ankle Int. 2015;36(9):1029–1037. doi: 10.1177/1071100715583383. [DOI] [PubMed] [Google Scholar]
- Usuelli FG, et al. Sagittal tibiotalar translation and clinical outcomes in mobile and fixed-bearing total ankle replacement. Foot Ankle Surg. 2016. In Press. [DOI] [PubMed]
- Stufkens SA, et al. Measurement of the medial distal tibial angle. Foot Ankle Int. 2011;32:288–293. doi: 10.3113/FAI.2011.0288. [DOI] [PubMed] [Google Scholar]
- Tochigi Y, Suh JS, Amendola A, Saltzman CL. Ankle alignment on lateral radiographs. Part 2: Reliability and validity of measures. Foot Ankle Int. 2006;27(2):88–92. doi: 10.1177/107110070602700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usuelli FG, Maccario C, Manzi L, Tan EW. Posterior talar shifting in mobile-bearing total ankle replacement. Foot Ankle Int. 2016;37(3):281–287. doi: 10.1177/1071100715610426. [DOI] [PubMed] [Google Scholar]
- Nosewicz TL, Knupp M, Bolliger L, Hintermann B. The reliability and validity of radiographic measurements for determining the three-dimensional position of the talus in varus and valgus osteoarthritic ankles. Skeletal Radiol. 2012;41:1567–1573. doi: 10.1007/s00256-012-1421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barg A, Knupp M, Henninger HB, Zwicky L, Hintermann B. Total ankle replacement using HINTEGRA, an unconstrained, three-component system: surgical technique and pitfalls. Foot Ankle Clin. 2012;17(4):607–635. doi: 10.1016/j.fcl.2012.08.006. [DOI] [PubMed] [Google Scholar]
- Lee KB, Cho SG, Hur CI, Yoon TR. Perioperative complications of HINTEGRA total ankle replacement: our initial 50 cases. Foot Ankle Int. 2008;29:978–984. doi: 10.3113/FAI.2008.0978. [DOI] [PubMed] [Google Scholar]
- Hogg RV, Ledolter J. Engineering Statistics. New York: MacMillan; 1987. [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960;20:37–46. [Google Scholar]
- Easley ME, Vertullo CJ, Urban WC, Nunley JA. Total ankle arthroplasty. J Am Acad Orthop Surg. 2002;10:157–167. doi: 10.5435/00124635-200205000-00002. [DOI] [PubMed] [Google Scholar]
- Horterer H, Miltner O, Muller-Rath R, Phisitkul P, Barg A. Sports Activity in Patients with Total Ankle Replacement. Sports Orthop Traumatol. 2015;31:34–40. [Google Scholar]
- Macaulay AA, VanValkenburg SM, DiGiovanni CW. Sport and activity restrictions following total ankle replacement: A survey of orthopaedic foot and ankle specialists. Foot Ankle Surg. 2015;21:260–265. doi: 10.1016/j.fas.2015.01.014. [DOI] [PubMed] [Google Scholar]
- Naal FD, Impellizzeri FM, Loibl M, Huber M, Rippstein PF. Habitual physical activity and sports participation after total ankle arthroplasty. Am J Sports Med. 2008;18:95–102. doi: 10.1177/0363546508323253. [DOI] [PubMed] [Google Scholar]
- Bonnin MP, Laurent JR, Casillas M. Ankle function and sports activity after total ankle arthroplasty. Foot Ankle Int. 2009;30:933–944. doi: 10.3113/FAI.2009.0933. [DOI] [PubMed] [Google Scholar]
- Barg A, Knupp M, Henninger HB, Zwicky L, Hintermann B. Total Ankle Replacement Using HINTEGRA, an Unconstrained, Three-Component System Surgical Technique and Pitfalls. Foot Ankle Clin N Am. 2012;17:607–635. doi: 10.1016/j.fcl.2012.08.006. [DOI] [PubMed] [Google Scholar]
- Conti SF, Wong YS. Complications of total ankle replacement. Foot Ankle Clin. 2002;7:791–807. doi: 10.1016/s1083-7515(02)00050-5. [DOI] [PubMed] [Google Scholar]
- Hintermann B, Valderrabano V, Dereymaeker G, Dick W. The HINTEGRA ankle: rationale and short-term results of 122 consecutive ankles. Clin Orthop Relat Res. 2004;68:424–457. doi: 10.1097/01.blo.0000132462.72843.e8. [DOI] [PubMed] [Google Scholar]


