Abstract
Falls are the leading cause of emergency department (ED) visits for fatal and non-fatal injuries among adults 65 years old and older. We aimed to better understand the fall history, risk for further falls, and actions taken to prevent further falls among this higher fall risk population. This cross-sectional study included older adults without cognitive impairment presenting to the Rhode Island Hospital ED from February to May 2017. Of the 76 participants, 35 self-reported no prior falls, and 41 self-reported at least one prior fall, of whom 20 fell on the day of ED presentation. Participants with vs. without self-reported prior falls were similar in age, gender, race, and substance use. Participants with prior falls scored lower on cognitive testing and had more comorbidities associated with falls. Only one quarter of those with prior falls reported making changes and few were evaluated by professionals to prevent future falls. This study highlights that older adult ED patients who sustain a fall are at higher risk for subsequent falls, and that greater fall prevention efforts are needed to protect this vulnerable group.
Keywords: aging, emergency services, prevention, falls, injury
BACKGROUND
Falls by older adults are both preventable and predictable. They are the leading cause of fatal and non-fatal injuries among adults 65 years old and older1 and constitute 13.5% of annual United States (US) emergency department (ED) visits in this age group.2 Falls are a sentinel event in a senior’s life because they frequently result in injury, hospitalization,3 loss of independence,4 and mortality.
Given that the population of older adults in the US is increasing and annual Medicare costs for adult falls are already estimated to be $31.3 billion,5 there have been many efforts to institute fall prevention programs. Overall multifactorial fall risk assessment and management programs have been successful in reducing fall risk among the elderly (adjusted risk ratio 0.82, 95% CI: 0.72–0.94).6 The most successful programs target modifiable risk factors and are tailored to the individual patient. Although many older adults who have a fall seek care in EDs, there is a noticeable lack of research into fall prevention specifically for ED patients. Therefore, the Society of Academic Emergency Medicine (SAEM) has specified falls as one of four high-yield research opportunities.7
In this investigation, we sought to better understand the characteristics of older adults with self-reported prior falls or a fall on the same day as the ED visit, as compared to older adults who present to the ED, but denied prior falls. In addition, we aimed to understand older adults’ prior healthcare interactions, care experiences, and their ideas for ED care improvement. We hypothesized that older adults with a history of falls would have unmet care needs that could be addressed in future ED-specific fall prevention protocols.
METHODS
This cross-sectional study was conducted at the Rhode Island Hospital ED, Rhode Island’s only level I trauma center, from February to May 2017. Eligible individuals were a convenience sample of adults 65 years old or older who were present in the ED during data collection periods, were undergoing an evaluation of any sub-critical illness or injury, were able to communicate in English, were at low risk for cognitive impairment, and could consent to participate. The Six-item Screener, a six-point questionnaire validated in the ED setting8 to measure cognitive impairment, was used to determine cognitive impairment. For the purposes of the study, patients scoring ≥4 on the screener were considered to be at low risk for cognitive impairment and thereby study eligible. Participants did not have to self-report a history of prior falls to be eligible, as we planned to recruit patients with and without prior falls.
Research assistants (RAs) reviewed the ED electronic health record (EHR) to assess for potential study eligibility. Patients who met inclusion criteria by EHR (65 years old or older, English-speaking, not currently residing in the critical care bay) were approached during their ED stay to confirm study eligibility. Following consent, participants underwent an RA-administered questionnaire. Survey questions were drawn from prior studies about older adult health and health care experiences. Participants were asked about their demographic characteristics, self-reported fall history, comorbidities, current medications, activities of daily living (ADL) status, as well as questions about how to improve the ED care experience. The hospital’s institutional review board approved this study.
Definitions
Fall: A fall was classified as coming to rest on the ground or other lower level, but not due to an external force (e.g. struck by car or assault), syncope, or serious illness (e.g. stroke, acute myocardial infarction).
Prior fall: A “prior fall” is a fall that occurred anytime before presentation to the ED that day. This includes falls that occurred immediately prior to coming to the ED, as well as falls that occurred several days to years ago.
Fall on ED study visit day: This refers to any fall that occurred after midnight on the day of presentation to the ED.
Analysis
The survey responses were reported as the number and proportions of the total responses stratified by two groups, older adults presenting to the ED without any self-reported history of falls vs. those with at least one prior fall (on the day of the ED study visit and/or previously). Patients with at least one prior fall were further stratified into those that had a prior fall vs. those who had a fall on the day of the ED study visit. Any patient who reported falling after midnight on the day of the ED visit was classified as having a “fall on ED study visit day”. Two study team members summarized participant suggestions on how to improve ED care and categorized them into major topics. The study team agreed on illustrative quotes that represented the relevant topics.
RESULTS
Characteristics of Study Subjects
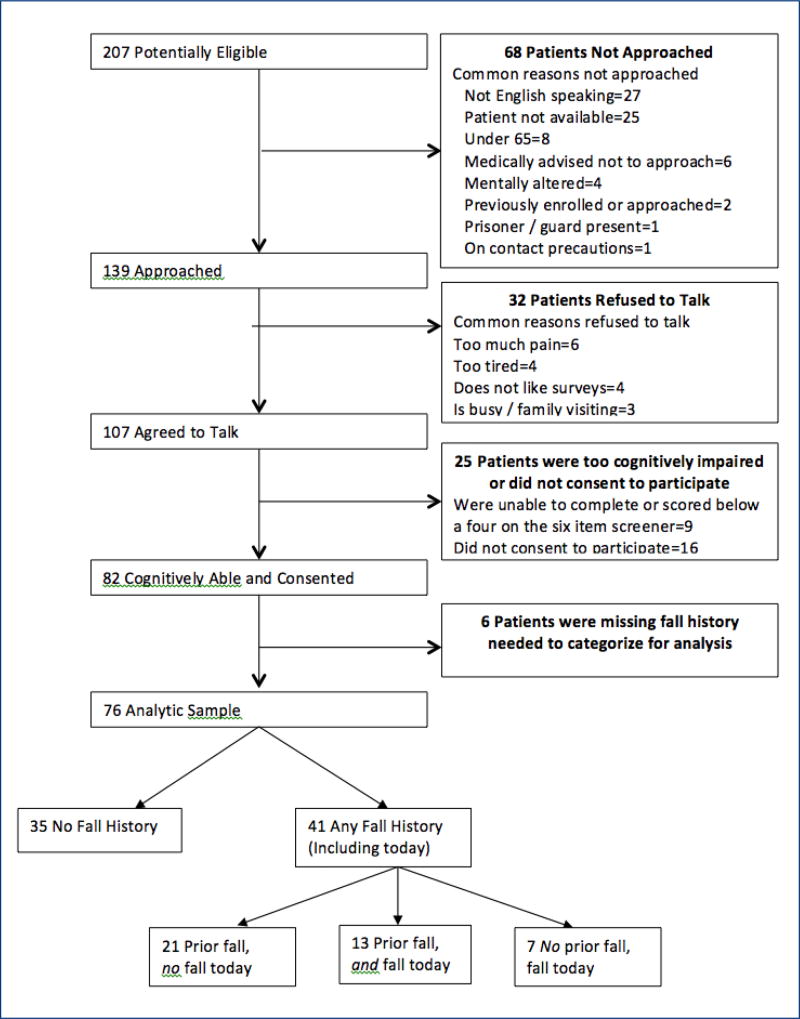
Of 207 potentially eligible subjects, 82 met inclusion criteria and consented to being in the study, and 76 were included in the analysis (Figure 1). Of these, 35 self-reported no prior falls and 41 participants indicated that they had fallen previously (including 20 who had fallen on the ED study visit day).
Figure 1.
Participant Flow Diagram
The mean age of participants was 75 years old among those with and without prior falls (Table 1). Participants were predominantly female, white, and high school graduates. More than two thirds reported having both private and governmental insurance and most were retired and not working. Less than 6% of participants reported living in assisted living or a nursing home. Participants with prior falls scored lower overall on cognitive scores on the Six-item Screener, but had a similar mean functional ability score on the Barthel’s ADL questionnaire.
Table 1.
Participant and visit characteristics
| Characteristics | No Self-reported Falls (n=35) |
Any Self-reported Fall (Not Including ED Study Visit Day) (n=34) |
Fall on ED Study Visit Day (n=20) |
|||
|---|---|---|---|---|---|---|
| N | Mean/% | N | Mean/% | N | Mean/% | |
| Age (Mean, in years) | 33 | 75.3 | 34 | 75.9 | 20 | 78.6 |
| Gender (%) | ||||||
| Female | 20 | 57.1 | 21 | 61.8 | 16 | 80.0 |
| Male | 14 | 40.0 | 12 | 35.3 | 4 | 20.0 |
| Race/Ethnicity (%) | ||||||
| White Non-Hispanic | 29 | 82.9 | 31 | 91.2 | 19 | 95.0 |
| Black/African-American | 2 | 5.7 | 1 | 2.9 | 1 | 5.0 |
| White Hispanic | 1 | 2.9 | 0 | 0.0 | 0 | 0.0 |
| Black Hispanic | 1 | 2.9 | 0 | 0.0 | 0 | 0.0 |
| Asian | 1 | 2.9 | 0 | 0.0 | 0 | 0.0 |
| American Indian/Alaskan Native | 0 | 0.0 | 1 | 2.9 | 0 | 0.0 |
| Educational level (%) | ||||||
| Less than high school graduate | 1 | 2.9 | 6 | 17.6 | 4 | 20.0 |
| High school graduate / GED# | 22 | 62.9 | 16 | 47.1 | 9 | 45.0 |
| Any college | 4 | 11.4 | 5 | 14.7 | 4 | 20.0 |
| College graduate | 6 | 17.1 | 5 | 14.7 | 3 | 15.0 |
| Health insurance status (%) | ||||||
| Private | 5 | 14.3 | 3 | 8.8 | 2 | 10.0 |
| Governmental | 3 | 8.6 | 4 | 11.8 | 5 | 25.0 |
| Private and governmental | 26 | 74.3 | 25 | 73.5 | 13 | 65.0 |
| Employment status (%) | ||||||
| Working full-time | 4 | 11.4 | 4 | 11.8 | 3 | 15.0 |
| Working part-time | 4 | 11.4 | 2 | 5.9 | 0 | 0.0 |
| Retired and not working | 24 | 68.6 | 25 | 73.5 | 15 | 75.0 |
| On disability and not working | 2 | 5.7 | 2 | 5.9 | 2 | 10.0 |
| Living arrangements (%) | ||||||
| Nursing home resident | 0 | 0.0 | 1 | 2.9 | 1 | 5.0 |
| Assisted living resident | 2 | 5.7 | 1 | 2.9 | 1 | 5.0 |
| Lives with others, not in a facility | 23 | 65.7 | 20 | 58.8 | 11 | 55.0 |
| Lives alone, not in a facility | 9 | 25.7 | 11 | 32.4 | 7 | 35.0 |
| Triage acuity (%) | ||||||
| ESI 1° | 2 | 5.7 | 0 | 0.0 | 0 | 0.0 |
| ESI 2 | 9 | 25.7 | 13 | 38.2 | 7 | 35.0 |
| ESI 3 | 21 | 60.0 | 18 | 52.9 | 12 | 60.0 |
| ESI 4 or ESI 5 | 1 | 2.9 | 1 | 2.9 | 1 | 5.0 |
| Unassigned | 0 | 0.0 | 1 | 2.9 | 0 | 0.0 |
| Cognitive and functional ability | ||||||
| Cognitive Six-item Screener score (%) | ||||||
| 4 | 3 | 8.6 | 6 | 17.6 | 6 | 30.0 |
| 5 | 6 | 17.1 | 5 | 14.7 | 5 | 25.0 |
| 6 | 24 | 68.6 | 22 | 64.7 | 8 | 40.0 |
| Barthel’s ADL score (mean) | 33 | 19.0 | 31 | 18.3 | 19 | 18.4 |
| Comorbidities associated with fall risk (%) | ||||||
| Memory loss | 4 | 11.4 | 10 | 29.4 | 5 | 25.0 |
| Arthritis | 11 | 31.4 | 23 | 67.7 | 12 | 60.0 |
| Hypotension | 3 | 8.6 | 8 | 23.5 | 2 | 10.0 |
| Dizziness | 11 | 31.4 | 17 | 50.0 | 7 | 35.0 |
| Anemia | 3 | 8.6 | 4 | 11.8 | 1 | 5.0 |
| Parkinson’s disease | 0 | 0.0 | 1 | 2.9 | 1 | 5.0 |
| Heart disease | 10 | 28.6 | 14 | 41.2 | 4 | 20.0 |
| Stroke | 3 | 8.6 | 3 | 8.8 | 1 | 5.0 |
| Diabetes | 6 | 17.1 | 12 | 35.3 | 2 | 10.0 |
| None | 9 | 25.7 | 1 | 2.9 | 5 | 25.0 |
| Substance use (%) | ||||||
| Smoke ≥ 1 pack of cigarettes a week | ||||||
| No | 32 | 91.4 | 31 | 91.2 | 17 | 85.0 |
| Yes | 0 | 0.0 | 3 | 8.8 | 3 | 15.0 |
| Drink ≥ 1 alcoholic drink per week | ||||||
| No | 29 | 82.9 | 27 | 79.4 | 14 | 70.0 |
| Yes | 4 | 11.4 | 5 | 14.7 | 6 | 30.0 |
| Number of fall-risk increasing medications taken* (%) | ||||||
| 0 | 11 | 31.4 | 12 | 35.3 | 7 | 35.0 |
| 1 | 9 | 25.7 | 8 | 23.5 | 3 | 15.0 |
| 2 | 2 | 5.7 | 2 | 5.9 | 1 | 5.0 |
| 3 | 0 | 0.0 | 3 | 8.8 | 1 | 5.0 |
Note: Percentages do not add up to 100% due to refused, don’t know, and missing responses.
GED – General Education Diploma
ESI – Emergency Severity Index – is a triage scoring tool used in Emergency Departments, with ESI 1 designation given to the most critical patients.
Beers criteria fall-risk increasing medications: anticonvulsants, antipsychotics, benzodiazepines, nonbenzodiazepine / benzodiazepine receptor agonist, hypnotics, eszopiclone, zaleplon, zolpidem, tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), opioids
Compared to participants who denied having a prior fall, those who had fallen previously reported more comorbidities, including memory loss, arthritis, hypotension, dizziness, heart disease and diabetes. Participants in both the self-reported prior fall and no self-reported prior fall groups were equally as likely to be taking fall risk-increasing medications; however, approximately one third of participants were unable or unwilling to provide an accounting of their current medications. Most participants in both groups did not smoke or drink alcohol.
Health Care Utilization History After Prior Falls
Table 2 summarizes the timing and frequency of prior falls and the health care use of the 34 participants self-reporting any prior falls, excluding those who reported falling on the day of the ED study visit. As shown, slightly over one third had fallen within the past year, and over one quarter had fallen more than once during this time period. Similar percentages reported having been evaluated initially in the ED vs. by their primary care provider after their last fall. Less than 10% reported being evaluated by a geriatrician, a physical therapist, occupational therapist or pharmacist after that fall, and none by a case manager. Over two thirds reported making no preventive changes after their prior fall.
Table 2.
Fall and post-fall care history among those self-reporting prior falls before the ED visit
| Any Self-reported Fall (Not Including ED Study Visit Day) (n=34) |
||
|---|---|---|
| Time since last fall | n | Mean/% |
| Less than 1 month ago | 2 | 5.9 |
| 1 month to less than 6 months ago | 7 | 20.6 |
| 6 months to less than 12 months ago | 9 | 26.5 |
| 12 months or more ago | 13 | 38.2 |
| Don’t know | 2 | 5.9 |
| Times fallen in the past 12 months | ||
| Once | 21 | 61.8 |
| Twice | 5 | 14.7 |
| Three times | 2 | 5.9 |
| Four times | 1 | 2.9 |
| Five times or more | 1 | 2.9 |
| Don’t know | 2 | 5.9 |
| Last visit to the ED after a fall | ||
| Less than 1 month ago | 3 | 8.8 |
| 1 month to less than 6 months ago | 1 | 2.9 |
| 6 months to less than 12 months ago | 4 | 11.8 |
| 12 months or more ago | 11 | 32.6 |
| Don’t know | 7 | 20.6 |
| Care provider seen after prior fall | ||
| PCP | 14 | 41.2 |
| Geriatrician | 1 | 2.9 |
| ED provider | 15 | 44.1 |
| Orthopedist | 4 | 11.8 |
| Physical therapist | 3 | 8.8 |
| Occupational therapist | 2 | 5.9 |
| Case manager | 0 | 0.0 |
| Pharmacist | 2 | 5.9 |
| Other | 1 | 2.9 |
| Assessments after prior fall | ||
| Vision | 5 | 14.7 |
| Footwear | 4 | 11.8 |
| Home safety evaluation | 5 | 14.7 |
| Visiting nurse | 3 | 8.8 |
| Don’t know | 3 | 8.8 |
| Preventive changes made after last fall | ||
| No | 23 | 67.6 |
| Yes | 9 | 26.5 |
| Don’t know | 2 | 5.9 |
Suggestions for ED Care Improvement
Table 3 summarizes participants’ free text answers to the following question: “Do you have any suggestions how your care in the Emergency Department could be improved in general?” Most participants reported that they had no suggestions to improve care. Approximately one quarter of participants indicated that the wait time to see a provider and the wait time for tests to return could be improved. Many participants made suggestions about making the ED environment more comfortable for patients like themselves.
Table 3.
ED post-fall care improvement suggestions
| Themes | Quotes |
|---|---|
| Timeliness | ”too long of a wait time”, “faster”, “hurry up and wait, over two hours after tests, still sitting” |
| Environment/Comforts | “mattresses could be better”, “pillows”, “too noisy, hard to get comfortable”, “hard to get good rest”, “if they could make it less cold in the hospital, that would be great”, “shouldn’t have to pay for parking” |
| Communication/Interactions | “communication more frequent what will be done”, “doctors could have better attitude”, “some staff are friendly, some are not”, “more coordinated, they come in and ask the same questions”, “so many people coming in and out and no one knows anything” |
| Medical Care | “came in for heart problem, didn’t put on leads”, “specialist was requested, no one came” |
| None | “No”, “N/A”, “wonderful”, “don’t fix what’s not broke” |
Communication improvements were suggested on multiple levels, including the desire to have more frequent updates on results, minimizing repeated questioning, and wanting a friendlier attitude from ED staff and physicians. Very few were unsatisfied with the medical care provided.
DISCUSSION
In this study of older adults presenting for emergency care, those who self-reported prior falls were more likely to have significant comorbidities that might indicate a predilection to having subsequent falls and performed worse on cognitive testing. Those who self-reported a prior fall also appear to be at risk for multiple subsequent falls, given that approximately one fourth had fallen more than once in the past 12 months. However, despite being at risk for subsequent falls, few patients reported having made preventive changes and few were evaluated by specialists who might offer care to reduce further fall occurrence.
The American College of Emergency Physicians (ACEP) soon will begin accrediting EDs that offer specialized geriatric care.9 Providing a standardized assessment for falls, as well as providing an ED environment that is tailored to older adults, are key criteria for accreditation. Suggested provisions include access to mobility aids, nonslip socks, pressure-reducing mattresses, bedside commodes, transition stools, and large-face analog clocks. Recognizing that ED physicians may lack the training and time to provide geriatric-tailored care, ACEP recommends that hospitals provide geriatric-trained professionals to complement the ED physician assessment, including physical therapists, occupational therapists, social workers, and pharmacists. As indicated by the responses from participants in this study, ED patients are cognizant of improvements that can be made to improve this care.
An interdisciplinary geriatric-focused team could greatly improve on the current status quo. Currently only 3.7% of older adults receive fall-guideline concordant care when they present to the ED after a fall.10 It is uncommon for the ED clinician to ask routinely and systematically about risk factors that frequently precipitate falls, including visual impairment, peripheral neuropathies, alcohol or medication use, appropriate footwear, and the safety of the home environment.11, 12 Prior research of community-dwelling older adults who present to the ED after falls shows that their 6-month fall risk was 29.5% higher than age-matched controls and functional ability, and balance confidence and depression all worsened over six months.10 Our study findings that the majority of ED patients were not evaluated by their primary care provider after their most recent fall and did not make preventive changes, could explain in part why outcomes for this vulnerable population can be dire. An ED-initiated fall prevention protocol, better communication between ED and outpatient providers, and an interdisciplinary approach to falls are necessary to improve post-fall care and help prevent future falls and their sequelae.
Limitations
While this study provides information on older adults lacking in the prior research on this topic, there are several limitations. First, given the convenience sample recruitment, inclusion only of English-speaking patients, and small sample size, it is not possible to generalize these study results to all older adults presenting to the ED, particularly given that those with cognitive impairment were excluded. These patients represent a particularly high-risk group for falls and their care preferences are important and should be queried in future surveys. Additionally, participants were predominantly white and were presenting to a large academic level I trauma center. Adults with different racial/ethnic backgrounds presenting to smaller, community hospitals in other regions of the country may have responded differently. The purpose of the study was to better understand older adults’ perceptions of their medical care; as such we did not collect information that was gathered by the ED provider such as the participant’s neurological exam, musculoskeletal exam, or gait evaluation.
CONCLUSIONS
In this study, older adult patients without cognitive impairment who self-reported a prior fall infrequently made changes to prevent future falls and had not been evaluated by professionals who might reduce subsequent fall occurrence. Because these patients are at higher risk for repeat falls, functional decline, and death, efforts aimed at fall prevention both in and outside the ED setting are needed. Future research should evaluate the effectiveness of geriatric-trained professionals in providing standardized fall assessments aimed at prevention in this setting.
Acknowledgments
Dr. Goldberg received research funding for this work from the Center of Gerontology and Healthcare Research, Brown University, AHRQ T32 postdoctoral training grant (Principal Investigator: Mor, Grant No. T32 HS000011).
The authors would like to acknowledge the following people who collected the data for this study: Divya Santhanam, Mitchell Yeary, Tien Hua, Julia Schoenewald, Xiaoshu Zheng, Wendy Gaztanaga.
Contributor Information
Elizabeth M. Goldberg, Department of Emergency Medicine, Alpert Medical School of Brown University; Postdoctoral Research Fellow, Center of Gerontology and Healthcare Research, Brown University School of Public Health, Providence, RI.
Ellen M. Mccreedy, Center of Gerontology and Healthcare Research, Brown University School of Public Health, Providence, RI.
Cameron J. Gettel, Department of Emergency Medicine, Alpert Medical School of Brown University, Providence, RI.
Roland C. Merchant, Departments of Emergency Medicine & Epidemiology, Alpert Medical School of Brown University, Brown University School of Public Health, Providence, RI.
References
- 1.Bergen GSM, Burns ER. [cited 2016 October 1, 2016];Falls and Fall Injuries Among Adults Aged ≥65 Years – United States, 2014. 2016 65 doi: 10.15585/mmwr.mm6537a2. Available from: https://www.cdc.gov/mmwr/volumes/65/wr/mm6537a2.htm?s_cid=mm6537a2_w. [DOI] [PubMed] [Google Scholar]
- 2.Albert M, Rui P, McCaig LF. Emergency Department Visits for Injury and Illness Among Adults Aged 65 and Over: United States, 2012–2013. NCHS data brief. 2017;(272):1–8. Epub 2017/03/04. [PubMed] [Google Scholar]
- 3.Carpenter CR. Deteriorating functional status in older adults after emergency department evaluation of minor trauma--opportunities and pragmatic challenges. Journal of the American Geriatrics Society. 2013;61(10):1806–7. doi: 10.1111/jgs.12478. Epub 2013/10/15. [DOI] [PubMed] [Google Scholar]
- 4.Sirois MJ, Emond M, Ouellet MC, Perry J, Daoust R, Morin J, Dionne C, Camden S, Moore L, Allain-Boule N. Cumulative incidence of functional decline after minor injuries in previously independent older Canadian individuals in the emergency department. Journal of the American Geriatrics Society. 2013;61(10):1661–8. doi: 10.1111/jgs.12482. Epub 2013/10/15. [DOI] [PubMed] [Google Scholar]
- 5.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults – United States. Journal of safety research. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. Epub 2016/09/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Roth EA, Shekelle PG. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. Bmj. 2004;328 doi: 10.1136/bmj328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci. 2011;66(7):775–83. doi: 10.1093/gerona/glr040. Epub 2011/04/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carpenter CR, DesPain B, Keeling TN, Shah M, Rothenberger M. The Six-Item Screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients(1097–6760 (Electronic)) doi: D-NLM: NIHMS334419 D-NLM: PMC3213856 EDAT- 2010/09/22 06:00 MHDA-2011/07/30 06:00 CRDT- 2010/09/22 06:00 PHST-2010/04/21 [received] PHST-2010/05/25 [revised] PHST-2010/06/24 [accepted] AID-S0196-0644(10)01184-4 [pii] AID-10.1016/j.annemergmed. 2010.06.560 [doi] PST-ppublish. [Google Scholar]
- 9.Carpenter CR, Hwang U, Biese K, Carter D, Hogan T, Karounos M, Malone M, Melady D, Rosen A, Rosenberg M, Schneider S, Shah M, Spiegel T, Stern M. [April 19, 2017];ACEP Accredits Geriatric Emergency Care for Emergency Departments ACEPNow. 2017 Available from: http://www.acepnow.com/article/acep-accredits-geriatric-emergency-care-emergency-departments/
- 10.Salter AE, Khan KM, Donaldson MG, Davis JC, Buchanan J, Abu-Laban RB, Cook WL, Lord SR, McKay HA. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2006;17(5):672–83. doi: 10.1007/s00198-005-0032-7. Epub 2006/02/24. [DOI] [PubMed] [Google Scholar]
- 11.Donaldson MG, Khan KM, Davis JC, Salter AE, Buchanan J, McKnight D, Janssen PA, Bell M, McKay HA. Emergency department fall-related presentations do not trigger fall risk assessment: a gap in care of high-risk outpatient fallers. Archives of gerontology and geriatrics. 2005;41(3):311–7. doi: 10.1016/j.archger.2005.04.008. Epub 2005/06/29. [DOI] [PubMed] [Google Scholar]
- 12.Paniagua MA, Malphurs JE, Phelan EA. Older patients presenting to a county hospital ED after a fall: missed opportunities for prevention. The American journal of emergency medicine. 2006;24(4):413–7. doi: 10.1016/j.ajem.2005.12.005. Epub 2006/06/22. [DOI] [PubMed] [Google Scholar]