Abstract
Incarcerated populations have relatively high HIV prevalence but little has been reported about their aggregate HIV risk behaviors or perceptions of risk. A random selection of HIV-negative men (n = 855) entering a US state prison system were surveyed to assess five risk behaviors and his self-perceived HIV risk. Using multivariate logistic regression, we identified factors associated with having elevated actual but low perceived risk (EALPR). Of the 826 men with complete data, 88% were at elevated risk. While 64% of the sample had risk perceptions concordant with their actual risk, 14% had EALPR (with the remainder at low actual but high perceived risk). EALPR rates were lower in those with a pre-incarceration HIV test but higher for those with a negative prison entry HIV test. HIV testing counseling should assess for discordance between actual and perceived risk and communicate the continued risk of HIV despite a negative result.
Keywords: HIV, Risk behavior, Risk perceptions, Incarcerated populations
Introduction
Incarcerated populations are known to have a several-fold elevated HIV prevalence compared with the general population [1, 2] and, consequently, are recognized as a key population to target for HIV screening and risk reduction interventions [3–7]. Even within incarcerated groups, however, as with other populations with elevated rates of HIV, risks vary among individuals due to variation in their specific behaviors and their degree of exposure to others infected with HIV [8–11]. Moreover, while incarcerated populations are known to be a group with higher HIV prevalence overall [1, 2, 7, 12], less is known about prisoners’ HIV risk behaviors [9, 10, 13, 14] and little has been reported regarding how they perceive their own risk [12].
Although, on average, individuals who engage in riskier behaviors of any kind perceive themselves to be at greater risk than those who do not engage in such behaviors [15–21], perceptions vary among individuals carrying out risky behaviors, and some may be unaware of or underestimate their risk [16, 18–27]. A few studies have assessed discrepancies between perceived and actual risks specifically for HIV [16, 24, 25]. In one study [16] assessing perceived and actual lifetime HIV risk among men who have sex with men (MSM) in six major U.S. cities, while perceiving oneself to be at elevated/moderate risk was associated with actual increased risk behavior, most men perceived themselves to be at low risk of acquiring HIV. Many, however, reported engaging in behaviors that put them at risk of HIV/STIs in the previous 6 months. In another U.S. study of nearly 6000 individuals undergoing rapid HIV testing in Philadelphia, two-thirds of those testing HIV-positive assessed their HIV risk as low or none [25].
How much an individual perceives him or herself to be at risk of acquiring HIV can drive the desire both to be tested for HIV [16, 28, 29] and to engage in risk-reducing behaviors [30, 31], making it an important construct to understand. The potential benefit of identifying individuals with elevated actual yet low perceived risk (EALPR) is supported by recent meta-analyses showing that one can modestly enhance risk-reducing behavior, particularly sexual behavior, by enhancing individuals’ perceptions that they are at greater risk [30, 32, 33]. The significant role of risk perception in driving risk-reduction behaviors suggests that identifying EALPR individuals, and potentially targeting interventions to improve their risk perceptions, could be an effective means to reducing risky behavior in a population at elevated HIV risk. Among incarcerated individuals, there are limited data delineating both the extent to which this population engages in an aggregate of various HIV risk behaviors and their risk perceptions.
To explore factors associated with being an EALPR individual among a key population, HIV-uninfected men entering a statewide prison system, we sought to identify: (1) their self-reported HIV risk behaviors; (2) their perceived risk of HIV infection; (3) the intersection between their actual and perceived risk; and (4) factors associated with being an individual classified as EALPR. To further understand this phenomenon, we also explored factors associated with being in the elevated actual risk group and factors associated with being in the low perceived risk group, independent of one another.
Methods
Study Setting and Population
To examine male prison inmates’ HIV risk behavior and perceptions of their risk of HIV, we analyzed data from a parent study conducted primarily to understand prisoners’ views of the prison HIV screening testing policy. In the study, conducted between April 2010 and April 2011, inmates entering one of the NC state prison system’s seven adult intake centers were surveyed at the time of initial NC Department of Public Safety (NCDPS) processing, shortly after they had entered prison and their medical screening had been initiated. Approximately 24,500 inmates were admitted to the NC prison system during the study period. Further details about the HIV screening study procedures are reported elsewhere [34].
For recruitment into the parent study, potential participants were randomly selected from a roster of inmates at each of the seven adult intake prisons. Sampling was designed so that the distribution of intake prisons among the study population reflected the distribution of prisoners found at intake prisons among all newly incarcerated inmates. Inmates were eligible for inclusion in the parent study if they were: (1) age 18 years or older; (2) English-speaking; (3) not housed in solitary confinement or disciplinary segregation; (4) finished with all prison health processing activities; (5) offered the opportunity to test for HIV in the last 2 weeks; and (6) able to provide informed consent to participate. Participants were demographically similar to the general prison population, as described elsewhere [34].
After inmates provided informed consent, they completed the parent study survey in a private room at the prison. To minimize social desirability bias in inmates’ responses, we administered the surveys using audio computer-assisted self-interviews (ACASI) with touch screen computers, whereby inmates could navigate the survey on their own unless they required assistance by a research assistant. The approximately 30 minute survey contained questions about demographics, incarceration and HIV testing history, substance use, mental health, sexual and drug HIV risk behaviors, attendance at an HIV course, levels of HIV knowledge and HIV-associated stigma, experiences with and perceptions of HIV testing in the prison and perceptions of individual HIV risk, among others.
To be included in the analyses presented here, participants also had to be male and HIV-negative, as determined by self-report. The study protocol was approved by the North Carolina Department of Public Safety, the Institutional Review Board of the University of North Carolina at Chapel Hill, and the Office for Human Research Protection at the U.S. Department of Health and Human Services.
Study Measures
Outcome Variables
Elevated-Risk Behavior
To assess pre-incarceration HIV risk behavior, we asked a series of five questions from the Behavioral Risk Factor Surveillance Survey [35]. Four of the five questions assessed each participant’s risk based on the inmate’s self-reported engagement in the following acts in the 3 months before incarceration: the number of unprotected sex acts; whether or not he traded sex for money/gifts; whether or not he bought sex for money/gifts, and injection drug use. The fifth question asked the participant to indicate whether or not he had engaged in at least one of the following four specified HIV-associated risk behaviors within the past year without identifying which specific behavior(s) he had engaged in: (1) used needles to inject drugs; (2) received treatment for a sexually transmitted disease; (3) gave or received “money, drugs, food, shelter gifts or other things you needed” in exchange for sex; and (4) had anal sex without a condom. Because each of the behaviors assessed by these five items has been well established to increase an individual’s risk of HIV [36–41], participants who reported engaging in an HIV risk behavior on any of the five items were considered to be at elevated risk of contracting HIV, while individuals who reported not engaging in the HIV risk behaviors on all of the five items were not considered to be at elevated risk. Individuals who did not respond to some of the questions and who did not report engaging in an HIV risk behavior on any of the four or fewer items that they did respond to were considered to be at unknown level of risk.
Perceptions of HIV Risk
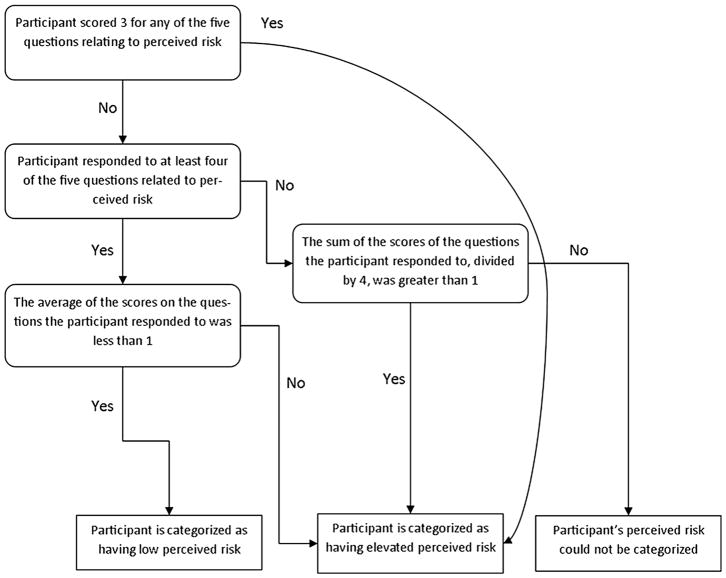
The extent to which participants perceived themselves to be at low risk of HIV was assessed using five questions, each on a four-point response option scale (0 = “agree a lot”, 1 = “agree a little”, 2 = “disagree a little”, 3 = “disagree a lot”), adapted and refined from a previously validated scale [42]. We assessed both the extent to which participants agreed (“a lot” or “a little”) with each of the individual items, and summed the total number of low perceived risk items each participant endorsed. We assessed low perceived risk by averaging participant responses for the five risk perception items, and created a risk perceptions scale from the individuals’ averages ranging from 0 to 3, with “0” representing lowest perceived risk and “3” representing highest perceived risk. We defined individuals with low perceived risk (see Fig. 1 and Table 1), a priori, as those who: (1) responded to at least four of the five risk perception items; (2) scored less than or equal to “1” on the risk perception scale; and (3) did not answer “3” (indicating high perceived risk) in response to any of the five questions. We defined individuals with elevated perceived risk as those who: responded to at least four of the five risk perception items and scored greater than “1” on the risk perception scale. In addition, we categorized as “elevated perceived risk”, those who responded to fewer than four questions but; for whom the sum of their answers to these questions when divided by four was greater than “1”; and those who ever answered a “3” in response to any of the five questions, regardless of the number they answered. Individuals who were neither categorized as elevated perceived risk nor low perceived risk were classified as unknown perceived risk.
Fig. 1.
Diagram describing categorization of “Perceived Risk” from sub-outcomes
Table 1.
Derivation and distribution of EALPR categories
| Risk behavior category | Perceived risk category | Row totals | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| N/A | Low | High | |||||||
| Perceived risk versus risk behavior categories | |||||||||
| N/A | 9 | 1.1% | 16 | 1.9% | 48 | 5.6% | 73 | 8.5% | |
| Low | 2 | 0.2% | 36 | 4.2% | 131 | 15.3% | 169 | 19.8% | |
| Elevated | 4 | 0.5% | 119 | 13.9% | 490 | 57.3% | 613 | 71.7% | |
| Column totals | 15 | 1.8% | 171 | 20.0% | 669 | 78.3% | 855 | 100.0% | |
|
| |||||||||
| N/A | EALPR | Not EALPR | |||||||
|
| |||||||||
| EALPR category | |||||||||
| 29 | 3.4% | 119 | 13.9% | 707 | 82.7% | ||||
Columns give number and percent of individuals in category
N/A indicates individuals were unclassifiable due to missingness pattern
Main Outcome: Individuals at Elevated Risk who Perceive Themselves to Be at Low Risk of HIV
To create the main outcome variable, we first created a variable with nine categories, representing all pairings of the three categories of Risk (Elevated, Low, Unknown) and the three categories of Perceived Risk (Elevated, Low, Unknown). From this multi-categorical variable we then created a dichotomous variable (after removing those who could not be classified as EALPR) for main outcome wherein individuals who were in the Elevated Risk and Low Perceived Risk category were defined to be EALPR individuals, individuals who were in any of the Low Risk or any of the Elevated Perceived Risk categories were defined to not be of EALPR status, and the remaining individuals were defined to have Unknown EALPR status and removed from subsequent analyses. See Table 1 for more information.
Independent Variables
Independent variables of a priori interest include the following factors assessed via ACASI: (1) demographics (i.e., race, age, education level and marital status, using response categories specified in the 2009 Behavioral Risk Factor Surveillance Survey [35]; (2) history of incarceration (the total number of times previously incarcerated in prison); (3) history of HIV testing: (a) whether tested before their current incarceration and (b) having received current in-prison test results back at the time of survey; (4) substance use in the 3 months before incarceration, including: (a) binge alcohol use and (b) the use of one or more illicit drugs (i.e., crack and/or powder cocaine, methamphetamines, heroin, prescription drugs, other), excluding marijuana; (5) self-reported previous sexually transmitted infection (STI) diagnosis; (6) history of having been diagnosed with depression; (7) attendance at an educational HIV course during their current incarceration; (8) level of HIV knowledge score, calculated as the sum of 22 (true–false) items answered correctly as adapted from the Brief HIV Knowledge Questionnaire with skipped questions considered incorrect [43]; (9) endorsement of mandatory HIV testing in prison, (10) sexual history: number of sexual partners in the last 3 months, and direct concurrency in the last 3 months.
Statistical Analyses
In the current study, we focused our analyses on the participants who were able to be classified as EALPR or Not EALPR; those who were unable to be classified were not considered for the main analysis. We first generated descriptive statistics to describe the sample population, including their HIV risk behaviors and risk perceptions.
We conducted logistic regression to investigate the associations between independent variables of interest and whether or not a participant was EALPR. To select the covariates included in the model, we estimated bivariate associations between the independent variables of interest and our main outcome, EALPR, using Mantel–Haenszel Chi square or Fisher’s exact test for categorical variables, and Wilcoxon Rank-Sum test for continuous variables. The final model was fit using variables (race, age, HIV knowledge, and education level) that we considered a priori to be important based on previous studies [24, 26, 27] regardless of the results of the bivariate analyses. While we considered including the variable “having sex with men or with both men and women” due to its importance in previous studies, the extremely small proportion endorsing this (1.5%) would not support its use as a covariate. We also included all independent variables of interest that were associated with the outcome variable in bivariate analyses at a significance level of 0.20 and were not highly collinear. We used a similar approach to assess factors associated with being in the elevated risk group and, separately, those associated with being in the low perceived risk group in two other separate models.
To mitigate the effects of missingness in the independent variables (33 of 826 observations were missing at least one independent variable), we employed multiple imputation with 20 datasets for the models: the missing data, which followed a nonmonotone pattern, was imputed via MCMC sampling using PROC MI in SAS, leaving the binary predictors in each model unrounded to avoid bias [44, 45]. Each of the three models was fit on each of the 20 datasets, and results for each model were combined by the so-called Rubin’s rules [46–48] using PROC MIANA-LYZE in SAS. To evaluate the robustness of the results, we performed sensitivity analysis to assess the effect on findings of changing the cut-off number of risk behaviors (from at least one to more than one) used to define of the EALPR outcome. All data preparation and analyses were completed using SAS 9.3 (SAS Institute, Cary NC).
Results
Description of Study Sample
Of 1812 inmates invited, 55% (1000/1812) consented to participate in the parent study and 855/1000 met the eligibility criteria for the analyses in this manuscript (were male and by self-report were HIV-uninfected).
There were 29 (3.4%) individuals of unknown EALPR status. These individuals were removed from main analysis, leaving 826 (96.6%) individuals in the sample meeting criteria to be included in the analysis.
Demographic and Other Characteristics (Table 2)
Table 2.
Characteristics of HIV negative male prisoners surveyed from April 2010 to April 2011, North Carolina prison system
| Variable | Total sample size = 826a | |
|---|---|---|
|
| ||
| n | % | |
| Age [Mean (SD)], (NR = 814) | 34.0 | 10.7 |
| Race (NR = 808) | ||
| Black | 401 | 49.6 |
| not black | 407 | 50.4 |
| School completed (NR = 815) | ||
| <HS degree or GED | 303 | 37.2 |
| Completed HS/GED | 310 | 38.0 |
| At least some post-secondary education | 202 | 24.8 |
| Current marital status (NR = 812) | ||
| Single | 470 | 57.9 |
| Married | 129 | 15.9 |
| Separated, divorced, or widowed | 213 | 26.2 |
| MSMb (NR = 821) | 12 | 1.5 |
| Binge drinkingc (NR = 815) | ||
| Never | 221 | 27.1 |
| Sometimes | 282 | 34.6 |
| Often | 312 | 38.3 |
| Hard drug usage (NR = 819) (illicit drugs excluding marijuana) | ||
| Yes, at least 1 hard drug used | 331 | 40.4 |
| Percentage of 22 HIV knowledge questions answered correctlyd | ||
| <69% | 182 | 22.0 |
| 69–82% | 263 | 31.8 |
| 83–99% | 340 | 41.2 |
| 100% | 41 | 5.0 |
| Number of times previously imprisonedd,e (NR = 808) | ||
| 0 | 339 | 42.0 |
| 1 | 155 | 19.2 |
| 2–5 | 274 | 33.9 |
| 6–18 | 40 | 5.0 |
| Endorsed mandatory prison HIV testing (NR = 823) | 696 | 84.6 |
| Underwent HIV class in prison before survey (NR = 823) | 601 | 73.0 |
| Received prison HIV test results before survey (NR = 825) | 354 | 42.9 |
| Diagnosis with an STI (ever)f (NR = 815) | 147 | 18.0 |
| History of depression (ever) (NR = 815) | 192 | 23.6 |
| Had HIV test before this incarceration (NR = 817) | 655 | 80.2 |
| Number of sexual partnersc,d (NR = 809) | ||
| 0 partners | 132 | 16.3 |
| 1 partner | 336 | 41.5 |
| 2+ partners | 341 | 42.2 |
| Concurrent sex with multiple partners (NR = 817) | 297 | 36.4 |
NR indicates number of participants responding to a particular question; Footnotes a–f provide more detailed information about the sample or the individual variables
Less than 2% of data were missing for all variables reported
Due to the lack of information that the data provided for this category, MSM was not considered as a possible independent variable for the model. illicit drugs (i.e., crack and/or powder cocaine, methamphetamines, heroin, prescription drugs, other), excluding marijuana
Reported for the 3 months prior to the survey
Variables presented categorically in Table 2 but analyzed continuously in main analysis
An individual who answered “55” to, “Not counting this incarceration, how many times have you been put in prison?” was counted as missing and not included in the logistic regression model
Chlamydia, gonorrhea, syphilis, and genital herpes included in survey
Of the 826 HIV-negative men in our study sample, 49.6% were Black, 37.2% had no high school degree or GED, 15.9% were married and the mean age was 34.0 years (Table 2). Few (1.5%) reported having sex with men or with both men and women. Fifty-eight percent reported having been previously incarcerated at least once. Other characteristics are summarized in Table 2.
HIV Risk Behaviors in the 3 Months before Incarceration and Risk Perceptions (Table 3)
Table 3.
Risk behaviors and perceptions of risk among a stratified random sample of male prisoners in North Carolina
| Variable | N = 826a | ||
|---|---|---|---|
|
| |||
| N | % | ||
| Risk behaviorsb | |||
| Number of unprotected sex actsc (NR = 762) | |||
| 0 | 226 | 29.7 | |
| 1–5 | 145 | 19.0 | |
| 6–100 | 369 | 48.4 | |
| 101–1000 | 22 | 2.9 | |
| Traded sex for goods (NR = 820) | 47 | 5.7 | |
| Gave goods for sex (NR = 820) | 77 | 9.4 | |
| IV drug users (NR = 824) | 73 | 8.9 | |
| Yes to combined 4-risks item (NR = 819)d | 218 | 26.6 | |
| Perception of own risk | |||
| Agreement with each measure of low risk perception | |||
| ”I don’t do things that put me at risk of HIV” (NR = 822) | 638 | 77.6 | |
| ”I’m not the kind of person who gets HIV” (NR = 808) | 388 | 48.0 | |
| ”I’m perfectly safe from getting HIV” (NR = 818) | 319 | 39.0 | |
| ”HIV is not my problem” (NR = 816) | 243 | 29.8 | |
| ”Getting HIV is not something I really need to worry about” (NR = 220) | 242 | 29.5 | |
|
| |||
| Number of low-perceived risk statements endorsEDe | N endorsing | % Endorsing | |
|
| |||
| 5 (least perceived risk) | 81 | 9.8 | |
| 4 | 109 | 13.2 | |
| 3 | 139 | 16.8 | |
| 2 | 189 | 22.9 | |
| 1 | 194 | 23.5 | |
| 0 (greatest perceived risk) | 114 | 13.8 | |
NR indicates number of participants responding to a particular question; Footnotes a–e provide more detailed information about the sample or the individual variables
All variables here have at least 808 of 826 (97.8%) of responses, except for Number of unprotected sex acts which has 762 (92.3%, or missing 7.75%)
All risk behavior characteristics reported for the 3 months prior to the survey
Variables presented categorically in Table 3 but analyzed continuously in main analysis. P value corresponds to a test of the null hypothesis of no association between the variable and the primary and secondary data sets
4-risk item (at least one of the following in the last 12 months: used intravenous drugs; (2) received treatment for a sexually transmitted or venereal disease; (3) gave or received “money, drugs, food, shelter gifts or other things you needed” in exchange for sex; and (4) had anal sex without a condom
A greater number of items endorsed represents lower perceived risk
More than half of the sample reported six or more unprotected sex acts in the 3 months before incarceration. Regarding transactional sex, 5.7% reported receiving money or gifts for sex and 9.4% reported giving money or gifts for sex. Injection drug use in the 3 months before incarceration was reported by 8.9%. Overall, 26.6% answered “yes” to the combined 4-risks item (at least one of the following in last year: used needles to inject drugs; received treatment for a sexually transmitted disease; gave or received “money, drugs, food, shelter gifts or other things you needed” in exchange for sex; and/or had anal sex without a condom).
Of the 855 individuals, there were 171 (20.0%) individuals with low perceived risk, 669 (78.2%) individuals with elevated perceived risk, and 15 (1.8%) individuals who could not be definitively classified regarding perceived risk due to missing data. The proportion of our sample endorsing each of the individual five risk perception variables ranged from 29.5% (“Getting HIV is not something I really need to worry about”) to 77.6% (“I don’t do things that put me at risk for HIV”). See Table 3 for detailed results.
Proportion of Individuals in the Elevated Actual Risk and Low Perceived Risk Groups (Table 1)
As shown in Table 1, of the 855 men in the study sample, 71.7% (613) of the sample was categorized as being at elevated actual risk of HIV as defined above, and 78.2% (669) perceived themselves to be at elevated risk. Overall, in 61.5% (526) there was concordance between reported and perceived risk; among the remainder, 15.3% (131) thought they were at elevated risk but were actually classified as low risk, and 13.9% (119) met criteria for elevated actual risk but perceived their risk to be low (i.e., EALPR). Further, as shown in Table 1, 5.8% [50] were classified as “not EALPR” due to having either unclassified actual risk and high perceived risk or low actual risk and unclassified perceived risk. Lastly, 3.4% [29] were unable to be classified as EALPR or not EALPR due to having either unclassified actual risk and low perceived risk, or high actual risk and unclassified perceived risk, or both actual and perceived risk being unclassified, and were removed from the analysis, leaving N = 826 remaining individuals.
Factors Associated with Categorization in: (1) the Elevated Actual Risk and Low Perceived Risk Group; (2) the Elevated Actual Risk Group; and (3) the Low Perceived Risk Group (Tables 4, 5)
Table 4.
Associations between the independent variables of interest and three outcomes in bivariate analyses
| Variable | EALPR unadjusted model | Perceived risk unadjusted model | Risk behavior unadjusted model | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Statistic | P value | Statistic | P value | Statistic | P value | |
| Age | −0.04 | 0.967 | 1.11 | 0.268 | 3.70 | 0.000 |
| Education | 1.52 | 0.218 | 0.31 | 0.578 | 0.00 | 0.980 |
| Race: African American | 0.26 | 0.610 | 1.02 | 0.312 | 2.02 | 0.155 |
| Incarceration historya | 0.33 | 0.743 | −0.50 | 0.619 | −2.19 | 0.028 |
| Has received HIV test results | 2.82 | 0.093 | 1.96 | 0.162 | 0.00 | 0.970 |
| Binge drinking | 0.16 | 0.693 | 2.12 | 0.145 | 8.09 | 0.004 |
| Hard drug use | 3.37 | 0.066 | 10.03 | 0.002 | 15.16 | 0.000 |
| Previous HIV test | 4.61 | 0.032 | 5.42 | 0.020 | 1.57 | 0.210 |
| Previous STI | 1.32 | 0.250 | 1.95 | 0.162 | 3.36 | 0.067 |
| HIV knowledgea | −0.64 | 0.522 | −1.71 | 0.087 | −3.55 | 0.000 |
| Endorsement of mandatory HIV testing | 0.14 | 0.709 | 1.08 | 0.298 | 3.49 | 0.062 |
| History of depression | 0.50 | 0.478 | 1.39 | 0.239 | 5.10 | 0.024 |
| Number of sexual partnersa | −0.03 | 0.976 | −2.78 | 0.005 | −12.65 | 0.000 |
| Direct concurrent relationships | 1.02 | 0.311 | 5.78 | 0.016 | 35.55 | 0.000 |
| Marital status | 1.10 | 0.295 | 0.89 | 0.345 | 0.08 | 0.775 |
| attended HIV class | 0.18 | 0.671 | 0.67 | 0.412 | 1.13 | 0.288 |
P-values <0.20 bolded
P-values bolded and italicised were not included due to model collinearity
Indicates use of Wilcoxon Rank-Sum Test. All others were conducted using Mantel–Haenszel Chi Square
Table 5.
Associations between participant characteristics and elevated actual/low perceived risk (EALPR) from multiply imputed multivariate logistic regression model
| Independent variablesa | OR (lower CI, upper CI)b P-value | ||
|---|---|---|---|
|
| |||
| EALPR N = 826 |
Low risk perception N = 824 |
Elevated risk behavior N = 778 | |
| Age | 1.00 (0.98, 1.02) 0.772 | 1.00 (0.99, 1.02) 0.692 | 0.98 (0.96, 1.00) 0.017 |
| Education level completedc | |||
| High school | 1.03 (0.64, 1.67) 0.906 | 1.01 (0.66, 1.56) 0.958 | 0.85 (0.54, 1.34) 0.482 |
| Beyond high school | 1.63 (0.96, 2.78) 0.069 | 1.32 (0.81, 2.15) 0.267 | 1.12 (0.65, 1.91) 0.681 |
| Race (African American) | 0.96 (0.64, 1.46) 0.863 | 0.87 (0.59, 1.28) 0.479 | 1.28 (0.84, 1.95) 0.245 |
| Incarceration history | – | – | 1.08 (0.98, 1.20) 0.136 |
| Has received HIV test results | 1.49 (1.00, 2.22) 0.051 | 1.36 (0.94, 1.95) 0.099 | – |
| Binge drinkingd | |||
| Moderate | – | 0.82 (0.52, 1.29) 0.391 | 0.68 (0.43, 1.08) 0.104 |
| High | – | 0.90 (0.57, 1.41) 0.634 | 1.23 (0.75, 2.01) 0.418 |
| Hard drug use | 0.70 (0.46, 1.08) 0.108 | 0.61 (0.41, 0.92) 0.018 | 1.38 (0.89, 2.14) 0.147 |
| Previous HIV test | 0.59 (0.37, 0.94) 0.027 | 0.62 (0.40, 0.95) 0.027 | – |
| Previous STI | – | – | 1.11 (0.64, 1.93) 0.705 |
| HIV knowledge | 0.96 (0.92, 1.01) 0.142 | 0.96 (0.92, 1.01) 0.097 | 1.06 (1.01, 1.11) 0.029 |
| Endorsement of mandatory HIV testing | – | – | 1.11 (0.67, 1.86) 0.678 |
| History of depression | – | – | 1.61 (0.98, 2.64) 0.058 |
| Number of sexual partners | – | 1.02 (0.96, 1.07) 0.602 | 2.20 (1.72, 2.81) 0.000 |
| Direct concurrent relationships | 0.66 (0.42, 1.04) 0.075 | 0.93 (0.53, 1.63) 0.789 | |
Independent variables included in the model if P < 0.20 in bivariate analysis. Race, education, HIV knowledge and age included a priori in all models due to findings from existing literature. MSM left out of all models due to the low percentage in study sample (Table 2). The model for perceived risk included only 824 of the 826 individuals, and the model for risk behavior included only 778 individuals, as 2 and 48 individuals had unclassifiable perceived risk and risk behavior, respectively
Boldface indicates significance at P < 0.05
Odds ratios compared to individuals who did not complete high school or GED
Odds ratios compared to individuals who reported never binge drinking
Table 4 indicates the bivariate associations between independent variables of interest and the three outcome variables. In the multivariate model for the EALPR outcome (Table 5), men who had ever been tested for HIV before this incarceration were less likely to be categorized as EALPR (OR 0.59 for having had a test, 95%CI [0.37, 0.94], P = 0.027). The estimated odds of being in the EALPR group for participants who had never had a previous HIV test were nearly 1.7 times as high as those participants who had been tested prior to this incarceration. In contrast, being tested for and receiving a negative HIV test result upon incarceration (OR 1.49, 95% CI [0.998, 2.22], P = 0.051), and having at least some education beyond high school (OR = 1.63, 95% CI [0.96, 2.78], P = 0.069) were each positively associated with being in the EALPR group; these relationships closely approached but were not statistically significant at the alpha = 0.05 level.
Modeling individuals’ perceived risk independently from risk behaviors, we found that participants were less likely to be in the low perceived risk group if they had previously undergone HIV testing prior to this incarceration (OR = 0.62, 95% CI [0.40, 0.95], P = 0.027) or if they had used illicit substances other than marijuana (OR = 0.61, 95% CI [0.41, 0.92], P = 0.018). In contrast, factors associated with being classified in the elevated actual risk group included being younger (OR 0.98 for each year of age, 95% CI [0.96, 0.996], P = 0.017), scoring higher on the HIV knowledge test (OR 1.06 for more correct answers, 95% CI [1.01, 1.11], P = 0.029), and having had a greater number of sexual partners in the last 3 months than those with low perceived risk (OR 2.20, 95% CI [1.72, 2.81], P < 0.0001).
Discussion
In this representative large sample of men entering prison, we found that a very high proportion (71.7% of the study sample) had, in the 3 months before incarceration, engaged in drug use and/or sexual behaviors that placed them at risk of HIV infection. Those men more likely to engage in risk behaviors were younger, binge drank, and were more educated. Almost 80% perceived that they were at elevated risk of HIV. However, among the approximately 20% of the study sample who perceived themselves to be at low risk, the vast majority (88%) actually reported HIV risk behaviors and comprised the EALPR group. Overall, 14% of the full study sample met criteria for EALPR.
While most prisoners accurately perceived themselves to be at risk of HIV, we were particularly interested in the substantial minority with elevated actual but low perceived risk, as this group may benefit from targeting of interventions that seek to change behavior by improving perceptions of risk. We found that prisoners who had undergone HIV testing before this incarceration were less likely to be in the EALPR group and were less likely to perceive themselves as low risk. Having had a previous HIV test was not, however, associated with engaging in less HIV risk behavior. These findings suggest that counseling that occurred during community testing improved prisoner’s risk perceptions but not their HIV knowledge or their behavior. In addition, those who had received their test result (all of which were negative in this sample) during this incarceration were more likely to be in the EALPR group. It is likely that, without post-test counseling, which was not provided in this setting, learning that one is not HIV-infected may make some individuals perceive themselves as being at less risk than their actual behaviors indicate.
Our findings also suggest that interventions that provide tailored information during post-test counseling regarding one’s HIV risk may improve the accuracy of individuals’ risk perceptions and potentially thereby reduce risk behavior. HIV testing counseling should also include assessments of discordance between actual and perceived risk and messaging regarding continued risk of HIV acquisition despite a negative result. It is noteworthy that post-test counseling is not a component of Centers for Disease Control and Prevention HIV opt-out testing recommendations. While opt-out testing may offer benefits in reaching more individuals for testing, there are trade-offs, particularly among higher risk populations. These results, combined with the findings in our study that hard drug usage was also associated with perceiving oneself to be at higher HIV risk, suggest that prisoners may need even more counseling regarding their risk from sexual risk behaviors than regarding their drug use and that those who are not involved in illicit substance use should be targeted as individuals who may underestimate their risks. Drug and alcohol use, however, are still important to address among this target population, and warrant efforts to improve understanding not only of risky sexual behavior but also of the link between substance use and risky sexual behavior. In addition, we found a trend, consistent with other studies [30], that older prisoners were less likely to misperceive their risk. Sheeran et al. meta-analysis showed that improving the accuracy of individuals’ perceptions of risk can increase risk-reducing behaviors. However, our finding that HIV knowledge alone was not associated with having better perceptions of risk suggests that multipronged, tailored approaches may be needed to enable an individual to apply general HIV knowledge to their own circumstances in the process of perceiving their own risk. Other investigators, such as Brown et al. [49] as well as van der Plight [50] have indicated that risk perceptions are also influenced by antecedents other than actual behavior or knowledge, including cognitive processes, such as a tendency toward denial, the use of social distancing [49], and optimism bias, which may vary based on perceived personal control, personal experience, and the perceived risk of a peer group to which one compares one’s self [50].
Brewer et al. and others [15, 49, 51] have demonstrated that the causal relationship between risk perceptions and health behavior is complex. While we cannot assume a causal direction for this group in this cross-sectional study, it is possible that, for some participants, their high perceived risk had influenced them to minimize their risk behaviors.
To our knowledge, only two other large studies in the US have sought to characterize the degree to which individuals engaging in HIV risk behaviors are unaware of their risk. In their study of factors influencing MSM to undergo HIV testing, MacKellar et al. [16] assessed perceived and actual lifetime risk among 2788 participants in the second phase of the multicity Young Men’s Survey. Those who perceived themselves to be at elevated or moderate HIV risk engaged in greater risk behaviors than those who did not have these perceptions. The majority (74%) of the full sample, however, perceived themselves to be at low risk of acquiring HIV over their lifetime, although many of the men perceiving low risk reported engaging in behavior that put them at significant risk of HIV/STIs: 46.7% reported ≥20 lifetime male sex partners; in the prior 6 months, 32.1% reported ≥4 male sex partners; 7.6% had unprotected anal intercourse with male partners of unknown HIV status; and 21.3% had been diagnosed with an STI. Further, among the full sample, 267 (~10%) were HIV-infected and were unaware of it: half of these individuals perceived themselves to be at low lifetime risk of HIV acquisition. In another U.S. study of 5871 individuals undergoing rapid HIV testing in Philadelphia, among the 62 (1.1%) who tested HIV-positive, two-thirds assessed their HIV risk as low or none [25], although the vast majority reported using condoms inconsistently and many had multiple sexual partners. Like ours, these studies document that discrepancies exist between actual and perceived risk among some individuals at elevated risk for HIV.
Investigations by Mills, Britain, Reyna, and Estrada indicate another mechanism by which inaccurate risk perceptions may occur. They found that perceived risk can be either positively or negatively associated with actual risk, depending on how an individual processes one’s risk. Individuals with a high perceived risk were more likely to engage in a risky behavior if they processed their risk perception globally or qualitatively (i.e., using what Reyna refers to as a “gist approach” in which they understand the “gist” of their risk but not the exact extent or nature of the risk) and less likely to do so if they processed using quantitative thought processes, such as risk–benefit analysis [52, 53]. These findings suggest that helping individuals assess their risk using quantitative central cognitive processes could reduce discrepancies between perceived and actual risk, thus decreasing participation in risky behaviors among high-risk individuals. Providing HIV knowledge information that is quantitatively based and individually tailored may assist this process. Studies also show that one’s self-efficacy, or confidence, to reduce risk is an important determinant of behavior [30, 54], and interventions aimed at enhancing self-efficacy and skills to reduce risk related to sexual settings may be useful. Moreover, enhancing self-efficacy may act synergistically with improving accuracy of risk perceptions [30, 55] to reduce risky behavior, particularly among the EALPR group.
The fact that most prisoners were at elevated risk, were aware of their risk, and yet continued to engage in HIV risk behaviors also suggests that interventions to reduce risk are very much needed among incarcerated men, but that interventions need to be tailored. Interventions that focus on self-efficacy, rather than solely on enhancing risk perceptions, may be more beneficial for these individuals who recognize yet continue to put themselves at risk. In addition, other factors not assessed here, such as a history of trauma, social networks, domestic violence, food insecurity, other stressors, or environmental factors, may hinder an individuals’ motivations or abilities to reduce their risk behaviors, even when they are aware of their risk. As Mills and Reyna’s work suggests, it is also possible that these individuals, while aware of their risk, process their perception more qualitatively and that they could benefit, not from increased knowledge, but rather from assistance learning to process risk information differently. Future studies are needed to tease apart, prospectively, the relative influences of HIV knowledge, risk perceptions, cognitive processes of risk and, other factors, such as self-efficacy, that may change risk behavior among key populations.
Our study has several limitations. First, its cross-sectional design precludes drawing conclusions regarding causal associations due to temporal ambiguity among the variables. Future prospective studies are needed to determine whether tailored post-test counseling can improve the accuracy of risk perceptions among incarcerated individuals. Second, our use of self-reported data to assess risky behavior may be inaccurate; however, our use of ACASI surveys to collect data likely mitigated social desirability bias to some extent. Moreover, 71.7% of the participants in this study reported engaging in HIV risk behaviors, which suggests that participants felt comfortable reporting many risk behaviors. That said, we suspect that the 1.5% who reported engaging in sex with men is an underestimate of actual risk given that general population estimates are 5% or greater [56] and hence our findings may be unable to identify factors most likely to be associated with high risk men who have sex with men (MSM) having a low perceived risk of HIV. Third, because 29 individuals (3.4%) were unable to be classified as EALPR or Not EALPR, some selection bias may have been introduced into our study. This study also has several strengths: As far as we are aware, this is the first study to investigate risk perceptions and the accuracy of such perceptions among a large representative statewide sample of prisoners. Moreover, we used a conservative method, in line with methods of other studies of risk perceptions [16], to identify individuals who engage in at least one HIV risk behavior yet perceived themselves to be at low risk of HIV. Sensitivity analyses (see Appendix) demonstrated the robustness of our findings to changes in the cut-off used to determine risk (at least 1 risk behavior versus more than 1 risk behavior).
The findings reported here provide insight into the HIV risk behaviors and perceptions of HIV-negative men incarcerated in a state prison system. Our findings confirm that most prisoners engaged in behaviors that placed them at risk of HIV infection in the months leading up to incarceration. Most prisoners accurately perceived that they were at risk of contracting HIV. The nearly one in six who were at risk but did not perceive being at risk (EALPR individuals) were less likely than the others to have had an HIV test before this incarceration and did not have greater HIV knowledge, suggesting that tailored post-test counseling to determine and enhance the accuracy of their perceptions could be a first step toward reducing risky behavior.
Acknowledgments
This study was supported by the National Institute of Mental Health (R01 MH079720-01A1). Dr. Golin’s salary for conducting this work was partly supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K24-HD06920 K24-DA037101). Mr. Barkley was partially supported by a T32 training Grant (T32ES007018). Additional support was provided by the University of North Carolina at Chapel Hill Center for AIDS Research (CFAR) (P30 AI-50410). We would like to acknowledge Dr. Michael Hudgens assistance with statistical analytic planning, Dr. Angela Thrasher for editorial assistance, Ms. Jennifer Lawall for data cleaning, Ms. Kelly Green for her assistance with study data collection and management and Monique Williams, Dani Strauss, Makisha Ruffin, and Catherine Grodensky for assistance with data collection. The authors thank the NCDPS, as well as the participants in the study.
Appendix
Table 6.
Sensitivity analysis: associations between the independent variables of interest and three outcomes in unadjusted bivariate analyses
| Variable | EALPR model | Perceived risk model | Risk behavior model | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Statistic | P value | Statistic | P value | Statistic | P value | |
| Age | −1.74 | 0.083 | 1.17 | 0.243 | −2.29 | 0.022 |
| Education | 0.00 | 0.978 | 0.52 | 0.469 | 0.02 | 0.884 |
| Race: African American | 0.11 | 0.745 | 0.76 | 0.384 | 0.08 | 0.771 |
| Incarceration historya | −0.49 | 0.628 | −0.50 | 0.616 | 3.39 | 0.001 |
| Has Received HIV test results | 0.42 | 0.515 | 1.92 | 0.166 | 0.56 | 0.453 |
| Binge drinking | 1.01 | 0.315 | 2.09 | 0.148 | 9.97 | 0.002 |
| Hard drug use | 1.73 | 0.188 | 9.38 | 0.002 | 50.82 | 0.000 |
| Previous HIV test | 0.40 | 0.527 | 4.99 | 0.026 | 0.46 | 0.498 |
| Previous STI | 0.94 | 0.332 | 2.33 | 0.127 | 12.06 | 0.001 |
| HIV knowledgea | −0.95 | 0.340 | −1.51 | 0.131 | 2.42 | 0.016 |
| Endorsement of mandatory HIV testing | 0.30 | 0.581 | 1.23 | 0.268 | 0.84 | 0.358 |
| History of depression | 1.37 | 0.241 | 1.21 | 0.271 | 2.73 | 0.099 |
| Number of sexual partnersa | 0.21 | 0.835 | −2.82 | 0.005 | 8.11 | 0.000 |
| Direct concurrent relationships | 1.28 | 0.258 | 6.05 | 0.014 | 50.35 | 0.000 |
| Marital status | 0.17 | 0.676 | 1.13 | 0.287 | 3.27 | 0.071 |
| Attended HIV class | 1.50 | 0.220 | 0.83 | 0.361 | 1.89 | 0.169 |
P-values < 0.20 bolded
P-value bolded and italicised was not included due to model collinearity
Indicates use of Wilcoxon Rank-Sum Test. All others were conducted using Mantel–Haenszel Chi Square
Table 7.
Sensitivity analysis: associations between participant characteristics and elevated actual/low perceived risk (EALPR) from multiply imputed multivariate logistic regression model
| Independent variablesa | OR (lower CI, upper CI)b P-value | ||
|---|---|---|---|
|
| |||
| EALPR N = 827 |
Low risk perception N = 822 |
Elevated risk behavior N = 766 |
|
| Age | – | 1.00 (0.99, 1.02) 0.654 | 0.99 (0.97, 1.01) 0.278 |
| Education level completedc | |||
| High school | 0.86 (0.36, 2.05) 0.737 | 1.04 (0.67, 1.60) 0.874 | 1.08 (0.72, 1.63) 0.696 |
| Beyond high school | 1.35 (0.53, 3.43) 0.528 | 1.33 (0.81, 2.17) 0.257 | 1.04 (0.64, 1.67) 0.886 |
| Race (African American) | 0.86 (0.41, 1.79) 0.680 | 0.89 (0.60, 1.31) 0.555 | 0.91 (0.62, 1.35) 0.647 |
| Incarceration history | – | – | 1.03 (0.95, 1.12) 0.441 |
| Has received HIV test results | – | 1.34 (0.93, 1.93) 0.116 | – |
| Binge drinkingd | |||
| Moderate | – | 0.83 (0.53, 1.31) 0.423 | 0.64 (0.40, 1.02) 0.061 |
| High | – | 0.89 (0.57, 1.41) 0.621 | 1.00 (0.64, 1.56) 0.999 |
| Hard drug use | 1.66 (0.80, 3.43) 0.174 | 0.62 (0.41, 0.94) 0.023 | 2.76 (1.91, 3.99) 0.000 |
| Previous HIV test | – | 0.63 (0.41, 0.97) 0.037 | – |
| Previous STI | – | – | 1.43 (0.93, 2.21) 0.103 |
| HIV knowledge | 0.97 (0.89, 1.06) 0.473 | 0.97 (0.92, 1.01) 0.136 | 1.04 (0.98, 1.09) 0.189 |
| Endorsement of mandatory HIV testing | – | – | – |
| History of depression | – | – | 1.23 (0.82, 1.85) 0.323 |
| Number of sexual partners | – | 1.01 (0.96, 1.07) 0.611 | 1.13 (1.05, 1.21) 0.001 |
| Direct concurrent relationships | – | 0.66 (0.42, 1.04) 0.072 | 1.93 (1.29, 2.88) 0.001 |
| Marital statuse | |||
| Married | – | – | 0.75 (0.44, 1.30) 0.307 |
| Divorced, separated or widowed | – | – | 0.93 (0.58, 1.48) 0.751 |
| Attended HIV class | – | – | 1.41 (0.92, 2.15) 0.116 |
Independent variables included in the model if P < 0.20 in bivariate analysis. Race, education, HIV knowledge and age included a priori in all models due to findings from existing literature. MSM left out of all models due to the low percentage in study sample (Table 2). The model for perceived risk included only 824 of the 827 individuals, and the model for risk behavior included only 766 individuals, as 3 and 66 individuals had unclassifiable perceived risk and risk behavior in the sensitivity analysis, respectively
Boldface indicates significance at P < 0.05
Odds ratios compared to individuals who did not complete high school or GED
Odds ratios compared to individuals who reported never binge drinking
Odds ratios compared to individuals who reported being single
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors have no disclosures to report.
References
- 1.Spaulding A, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4:e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maruschak LM, Bezofsky M, Unangst J. Medical problems of state and federal prisoners and jail inmates, 2011–2012. Bur Justice Stat. 2015:1–23. [Google Scholar]
- 3.Lambert EY, Normand JL, Volkow ND. Prevention and treatment of HIV/AIDS among drug-using populations: a global perspective. J Acquir Immune Defic Syndr. 2010;55:S1–4. doi: 10.1097/QAI.0b013e3181f9c120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rich JD, Wohl D, Beckwith CG, Spaulding AC, Lepp NE, Baillargeon J, Gardner A, Avery A, Altice FL, Springer S On behalf of the CFAR-CHIC Working Group. HIV-related research in correctional populations: now is the time. Curr HIV/AIDS Rep. 2011;8:288–96. doi: 10.1007/s11904-011-0095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55:S49–55. doi: 10.1097/QAI.0b013e3181f9c0f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beckwith C, Bazerman L, Gillani F, Tran L, Larson B, Rivard S, Flanigan T, Rich MD. The feasibility of implementing the HIV seek, test, and treat strategy in jails. AIDS Patient Care STDs. 2014;28(4):183–7. doi: 10.1089/apc.2013.0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen DL, Wohl DA, Golin CE, Rigdon J, May J, White BL, Leone PA, Hudgens MG, Bowling JM. Comparing HIV case detection in prison during opt-in vs. opt-out testing policies: a seroprevalence study. J Acquir Immune Defic Syndr. 2016;71(3):e85–8. doi: 10.1097/QAI.0000000000000889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosen DL, Schoenbach VJ, Wohl DA, White BL, Stewart PW, Golin CE. An evaluation of HIV testing among inmates in the North Carolina prison system. Am J Public Health. 2009;99:S452–9. doi: 10.2105/AJPH.2007.133124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Margolis AD, MacGowan RJ, Grinstead O, Sosman J, Kashif I, Flanigan TP The Project Start Study Group. Unprotected sex with multiple partners: implications for HIV prevention among young men with a history of incarceration. Sex Transm Dis. 2006;33(3):175–80. doi: 10.1097/01.olq.0000187232.49111.48. [DOI] [PubMed] [Google Scholar]
- 10.Morrow K The START Study Group. HIV, STD, and hepatitis risk behaviors of young men before and after incarceration. AIDS Care. 2009;21(2):235–43. doi: 10.1080/09540120802017586. [DOI] [PubMed] [Google Scholar]
- 11.Epperson MW, Khan MR, Miller DP, Perron BE, El-Bassell N, Gilbert L. Assessing criminal justice involvement as an indicator of HIV risk among women in methadone treatment. J Subst Abus Treat. 2010;38(4):375–83. doi: 10.1016/j.jsat.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Begier EM, Bennani Y, Forgione F, Punsalang A, Hanna DB, Herrera J, Torian L, Gbur M, Sepkowitz KA, Parvez F. Undiagnosed HIV infection among New York City jail entrants, 2006: results of a blinded serosurvey. J Acquir Immune Defic Syndr. 2010;54:93–101. doi: 10.1097/QAI.0b013e3181c98fa8. [DOI] [PubMed] [Google Scholar]
- 13.Khan MR, Golin CE, Friedman S, Scheidell JD, Adimora AA, Monk S, Hobbs MM, Dockery G, Brown S, Oza K, Myers D, Hu H, Wohl DA. STI/HIV Sexual risk behavior and prevalent STI among incarcerated African American men in committed partnerships: the significance of poverty, mood disorders, and substance use. AIDS Behav. 2015;19(8):1478–90. doi: 10.1007/s10461-015-1062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grinstead OA, Faigeles B, Comfort M, Seal D, Nealey-Moore J, Belcher L, Morrow K. HIV, STD, and hepatitis risk to primary female partners of men being released from prison. Women Health. 2005;41(2):63–80. doi: 10.1300/J013v41n02_05. [DOI] [PubMed] [Google Scholar]
- 15.Gerrard M, Gibbons FX, Bushman BJ. Relation between perceived vulnerability to HIV and precautionary sexual behavior. Psychol Bull. 1996;119(3):390–409. doi: 10.1037/0033-2909.119.3.390. [DOI] [PubMed] [Google Scholar]
- 16.MacKellar DA, et al. Perceptions of lifetime risk for acquiring HIV among young men who have sex with men. AIDS Behav. 2007;11:263–70. doi: 10.1007/s10461-006-9136-0. [DOI] [PubMed] [Google Scholar]
- 17.Akwara AP, Madise NJ, Hinde A. Perception of risk of HIV/AIDS and sexual behavior in Kenya. J Biosoc Sci. 2003;35:384–411. doi: 10.1017/s0021932003003857. [DOI] [PubMed] [Google Scholar]
- 18.Ladwig KH, Baumert J, Lowel H, Doring A, Wichmann HE. Contemplating to quit current smoking status: differences in behavioural and psychosocial patterns in a population-based cohort of current smokers. Prev Med. 2005;41:134–40. doi: 10.1016/j.ypmed.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Katapodi MC, Lee KA, Facione NC, Dodd MJ. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med. 2004;38:388–402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Katapodi MC, Dodd MJ, Lee KA, Facione NC. Underestimation of breast cancer risk: influence on screening behavior. Oncol Nurs Forum. 2009;36(3):306–14. doi: 10.1188/09.ONF.306-314. [DOI] [PubMed] [Google Scholar]
- 21.Ko Y, Boo S. Self-perceived health versus actual cardiovascular disease risks. Jpn J Nurs Sci. 2016;13:65–74. doi: 10.1111/jjns.12087. [DOI] [PubMed] [Google Scholar]
- 22.Fontenat HB, Fantasia HC, Charyk A, Sutherland MA. Human papillomavirus (hpv) risk factors, vaccination patterns, and vaccine perceptions among a sample of male college students. J Am Coll Health. 2014;62(3):186–92. doi: 10.1080/07448481.2013.872649. [DOI] [PubMed] [Google Scholar]
- 23.Fan W, et al. HIV risk perception among HIV negative or status-unknown, men who have sex with men in China. BioMed Res Int. 2014;2014:1–9. doi: 10.1155/2014/232451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mgbere O, Monjok E, Abughosh S, Ekong E, Holstad MM, Essien EJ. Modeling covariates of self-perceived and epidemiologic notions of risk for acquiring stis/hiv among military personnel: a comparative analysis. AIDS Behav. 2013;17:1159–75. doi: 10.1007/s10461-011-0126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nunn A, et al. Low perceived risk and high HIV prevalence among a predominantly African American population participating in Philadelphia’s rapid HIV testing program. AIDS Patient Care STDs. 2011;25(4):229–35. doi: 10.1089/apc.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jain AK, et al. Relationship between reported prior condom use and current self-perceived risk of acquiring HIV among mobile female sex workers in southern India. BMC Public Health. 2011;11(S6):S5. doi: 10.1186/1471-2458-11-S6-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ankomah A, et al. HIV-related risk perception among female sex workers in Nigeria. HIV AIDS (Auckl) 2011;3:93–100. doi: 10.2147/HIV.S23081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Earnshaw VA, Smith LR, Chaudoir SR, Lee I-C, Copenhaver MM. Stereotypes about people living with HIV: implications for Perceptions of HIV risk and testing frequency among at-risk populations. AIDS Educ Prev. 2012;24(6):574–81. doi: 10.1521/aeap.2012.24.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kacanek D, et al. Young incarcerated men’s perceptions of and experiences with HIV testing. AJPH. 2007;97(7):1209–15. doi: 10.2105/AJPH.2006.085886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014;140(2):511. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- 31.Reyna VF, Farley F. Risk and rationality in adolescent decision making implications for theory, practice, and public policy. Psychol Sci Public Interest. 2006;7(1):1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [DOI] [PubMed] [Google Scholar]
- 32.Brewer N, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–45. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 33.Brewer NT, Weinstein ND, Cuite CL, Herrington J. Risk perceptions and their relation to risk behavior. Ann Behav Med. 2004;27(2):125–30. doi: 10.1207/s15324796abm2702_7. [DOI] [PubMed] [Google Scholar]
- 34.Rosen D, Golin CE, Grodensky CA, May J, Bowling JM, DeVellis RF, White BL, Wohl D. Opt-out testing in prison: informed and voluntary? AIDS Care. 2015;27(5):545–54. doi: 10.1080/09540121.2014.989486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Survey. 2009 http://www.cdc.gov/brfss/questionnaires/pdf-ques/2009brfss.pdf.
- 36.Centers for Diseaase Control and Prevention (CDC) HIV Transmission Risk. 2012 http://www.cdc.gov/hiv/law/pdf/HIVtranmsmision.pdf.
- 37.Oldenberg CE, Perez-Brumer AG, Reisner SL, Mattie J, Barnighausen T, Mayer K, Mimiage MJ. Global burden of HIV among men who engage in transactional sex: a systematic review and meta-analysis. PLoS ONE. 2014;9(7):e103549. doi: 10.1371/journal.pone.0103549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Astemborski J, Vlahov D, Warren D, Solomon L, Nelson KE. The trading of sex for drugs or money and HIV seropositivity among female intravenous-drug-users. Am J Public Health. 1994;84(3):382–7. doi: 10.2105/ajph.84.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edwards JM, Iritani BJ, Hallfors DD. Prevalence and correlates of exchanging sex for drugs or money among adolescents in the United States. Sex Transm Infect. 2006;82(5):354–8. doi: 10.1136/sti.2006.020693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fishbein M, Coutinho R, Trial NMHP. Demographic and behavioral predictors of sexual risk in the NIMH multisite HIV prevention trial. AIDS. 1997;11:S21–7. [PubMed] [Google Scholar]
- 41.Ross MW, Hwang LY, Zack C, Bull L, Williams ML. Sexual risk behaviours and STIs in drug abuse treatment populations whose drug of choice is crack cocaine. Int J STD AIDS. 2002;13(11):769–74. doi: 10.1258/095646202320753736. [DOI] [PubMed] [Google Scholar]
- 42.Snell WE, Jr, Finney PD, Godwin L. Stereotypes about AIDS. Contemp Soc Psychol. 1991;15:18–38. [Google Scholar]
- 43.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–82. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allison PD. Imputation of categorical variables with PROC MI. SUGI 30 Proceedings. 2005;113(30):1–4. [Google Scholar]
- 45.Horton NJ, Lipsitz SR, Parzen M. A potential for bias when rounding in multiple imputation. Am Stat. 2003;57(4):229–32. [Google Scholar]
- 46.Rubin DB, Schenker N. Multiple imputation for interval estimation from simple random samples with ignorable nonresponse. J Am Stat Assoc. 1986;81(394):366–74. [Google Scholar]
- 47.Rubin DB. Multiple imputation for nonresponse in surveys. Vol. 81. John Wiley & Sons; 2004. [Google Scholar]
- 48.Schafer JL. Multiple imputation in multivariate problems when the imputation and analysis models differ. Stat Neerl. 2003;57(1):19–35. [Google Scholar]
- 49.Brown EJ, Outlaw FH, Simpson EM. Theoretical antecedents to HIV risk perception. JAPNA. 2000;6(6):177–82. [Google Scholar]
- 50.van der Pligt J. Perceived risk and vulnerability as predictors of precautionary behavior. Br J Health Psychol. 1998;3:1–14. [Google Scholar]
- 51.Eiser JR, Bostrom A, Burton I, Johnston DM, McClure J, Paton D, van der Pligt J, White MP. Risk interpretation and action: a conceptual framework for responses to natural hazards. Int J Disaster Risk Reduct. 2012;1:5–16. [Google Scholar]
- 52.Mills B, Reyna VF, Estrada S. Explaining contradictory relations between risk perception and risk taking. Psychol Sci. 2008;19(5):429–33. doi: 10.1111/j.1467-9280.2008.02104.x. [DOI] [PubMed] [Google Scholar]
- 53.Reyna VF. How people make decisions that involve risk: a dual-processes approach. Curr Dir Psychol Sci. 2004;13(2):60–6. [Google Scholar]
- 54.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 55.Kowalewski MR, Henson KD, Longshore D. Rethinking perceived risk and health behavior: a critical review of HIV prevention research. Health Educ Behav. 1997;24(3):313–25. doi: 10.1177/109019819702400305. [DOI] [PubMed] [Google Scholar]
- 56.Centers for Disease Control and Prevention (CDC) Estimated percentages and characteristic of men who have sex with men and use injection drugs, United States 1999–2011. MMWR Morb Mortal Wkly Rep. 2013;62(37):557–62. [PMC free article] [PubMed] [Google Scholar]