Abstract
[Purpose] The objective of this study was to determine the effect of pulsed high intensity laser therapy on delayed caesarean section healing in diabetic women. [Subjects and Methods] This study was conducted on forty diabetic women with delayed caesarean wound healing, ranging in age from 28 to 38 years. They were randomly assigned into two groups; the group I (n=20) received pulsed high intensity laser therapy for 6-weeks, 3 times per week plus standard medical treatment for treatment of diabetes and caesarean wound patients, the group II (n=20) received sham laser treatment for 6 weeks, 3 times per week plus standard medical treatment for treatment of diabetes and caesarean wound patients. The wound size and appearance in all participants were measured by the tracing method and pressure sore status tool before and after the 6-week treatment. [Results] Pulsed high intensity laser therapy produced a significant difference in wound size and appearance in comparison to the sham laser treatment in diabetic women with delayed caesarean wound healing. [Conclusion] Pulsed high intensity laser therapy is effective in the treatment of delayed caesarean section healing in diabetic women.
Key words: Pulsed high intensity laser therapy, Caesarean section, Diabetic women
INTRODUCTION
Caesarean section is a common delivery procedure in obstetric practice which can be performed as emergency or elective. In addition to the successful delivery of the baby, good wound care is a priority for the mother1). Furthermore, whenever a woman has a caesarean section, there is a five to 20-fold greater risk for infection compared with a vaginal delivery and a three-fold higher incidence of surgical site infections in diabetic patients undergoing a caesarean section when compared to non-diabetic women2). The most common type of wound healing problem is separation, opening of the skin and fatty tissue just beneath the skin3).
Wound care is an expensive area of treatment for health care services4), with caesarean section wound infections representing a substantial burden to the health system. The prevention of such infections should be a healthcare priority in developing countries, and the global estimates of surgical site infections (SSI) range from 0.5–15%5, 6). Moreover, diabetes affects about 2–4% of the general population and it is expected that the number of patients with diabetes in the Middle East and North Africa (MENA) region will grow by 96% from 2013 to 2035 or from 34.6 million to 67.9 million. In Egypt, the prevalence of diabetes is around 15.56% among adults and its incidence is increasing7).
Diabetic wounds present a major health problem as they have complex multiple pathophysiological processes characterised by polymicrobial infection, altered immune function or increased susceptibility to infection, decreased wound nitric oxide (NO) production, and often hypoxia/ischemia8, 9). The course of diabetic wound healing appears to be hindered by many factors, including specific metabolic deficiencies and impaired physiological responses, for example, the altered metabolism of carbohydrates, fats and proteins resulting from the absence or deficiency of insulin, hyperglycaemia leading to non-enzymatic glycosylation, osmotic diuresis resulting in decreased perfusion, low oxygen tensions, low pH, and high lactate concentrations, altered collagen metabolism with a significant reduction in the number of fibroblasts and free radical production10).
Wounds that are difficult to heal represent a serious public health problem as the lesions may severely affect the quality of life of individuals due to decreased mobility and substantial loss of productivity. They can also cause emotional damage and contribute to increased burden of public expenditure in healthcare11). Changes in wound size during the initial phase of treatment have been shown to be a potential indicator of the subsequent response to treatment and ultimately healing12). Wound healing acceleration in women who have undergone caesarean surgery could help them to return to their normal function, especially to begin breastfeeding their newborn, one of the most important aspects of newborns’ care13,14,15).
The need to care for a population with poorly healing wounds is a growing challenge that requires innovative strategies. Such an approach in the treatment of these lesions is low-power light therapy, such as laser therapy16,17,18). Low level lasers have been introduced as one treatment modality for wound healing and several indications have been described for their use in wound healing processes. However, the effect in a healthy individual is limited and the prime indication for laser therapy in wound healing is for individuals or tissues with a compromised state16, 19,20,21). Laser therapy is an effective therapeutic modality to promote healing of skin wounds. The biological effects promoted by these therapeutic resources are similar and are related to the decrease in inflammatory cells, increased fibroblast proliferation, angiogenesis stimulation, formation of granulation tissue and increased collagen synthesis18, 22,23,24). When laser energy penetrates deep into the skin it has several effects, such as increased ATP production and microcirculation, stimulation of the immune system, anti-inflammatory effects, and improved metabolism due to photostimulated products that circulate in the blood25). The aim of this study was to determine the effect of pulsed high intensity laser therapy (HILT) on delayed caesarean section healing in diabetic women.
SUBJECTS AND METHODS
Forty diabetic women from Makkah hospitals diagnosed with delayed caesarean section healing for more than eight weeks participated in this study to investigate the effect of pulsed high intensity laser on delayed caesarean section healing. All participants provided informed consent form, giving agreement to participation and publication of the study results. All patients received the same standard medical care for the treatment of diabetes and caesarean wounds and did not receive any physical therapy modalities before the study. Inclusion criteria: diabetic women categorised as having a delayed caesarean wound for more than eight weeks, ranging in age from 28 to 38 years. Exclusion criteria: any pathological conditions or associated injuries which could affect the results of the study, skin disease or any disease leading to delayed wound healing other than diabetes, such as venous or arterial disease. The study was approved by the research committee of the Physical Therapy Department, Faculty of Applied Medical Sciences in Umm Al-Qura University, Makkah, Saudi Arabia (Approval Number FAMS15022017). Informed consent forms were signed by all participants.
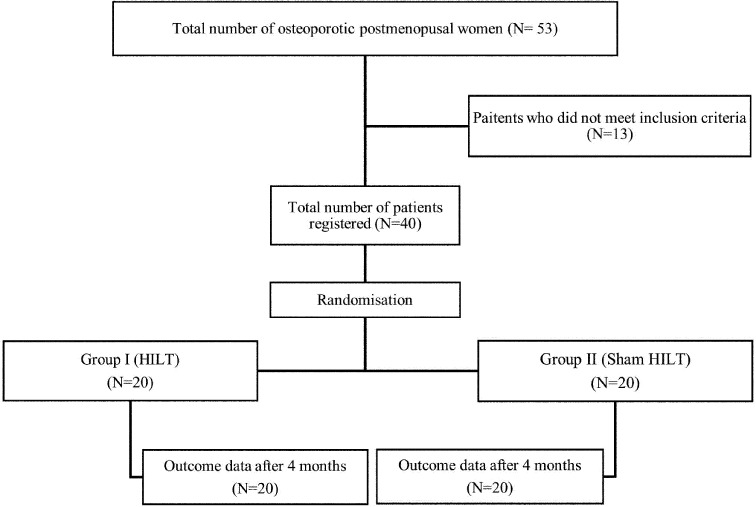
Patients were randomly assigned to one of two groups, the group I (HILT group) and the group II (sham laser group) using systematic sampling. Patients in the laser group received pulsed high intensity laser therapy for 6 weeks, 3 times per week plus standard medical treatment for the treatment of diabetes and caesarean wound patients. Patients in the sham laser group received sham laser for 6-weeks, 3 times per week plus standard medical treatment for treatment of diabetes and caesarean wound patients (Fig. 1).
Fig. 1.
Flowchart of the study.
Participants in HILT group received pulsed Nd:YAG laser produced by a HIRO 3 device (ASA, Arcugnano, Vicenza, Italy) for about 8 minutes during each treatment session. The HILT apparatus used postulates (Nd:YAG), with pulsed emission (1,064 nm), very high peak powers (3 kW), high levels of energy density (fluency from 810–1,780 mJ/cm), very short pulse duration of (120–150 μs), a duty cycle of approximately 0.1%, and frequency (10–40 Hz). The HILT was applied with an average total energy of 360–540 J, which was administered through three phases. The HILT probe was kept perpendicular at a 1 cm distance away from the wound surface. The irradiation was performed in 3 different phases, i.e., the initial, intermediate, and final phase. In the initial phase, fast scanning in the vertical and horizontal directions was applied to the wound area with an energy density of 510 mJ/cm2, a frequency of 25 HZ, energy of 25 J/cm2, and a total energy of 100–150 J. In the intermediate phase, the probe was held at the periphery of the wound on fixed points at a distance of 1 cm away from the wound margin and fixed for 14 seconds at each point providing energy of 20 J/point for 8–12 points (i.e., a total of 160–240 J). In the final phase, the same laser parameters were used as in the initial phase, except that the scanning was done at a slower pace. The laser application was performed after the patient received standard medical treatment at each session. The standard care of diabetes and caesarean wound patients included good glycaemic control, adequate nutrition, local care (moist dressings and topical management), lessening of oedema, surgical debridement of devitalised wound tissue and antibiotic therapy26, 27).
Wound Surface Area (WSA). The wound surface area was measured at two time points, baseline and after 6 weeks, by tracing the wound perimeter as reported by Kloth and Feedar28). In the transparent method, the patient was positioned in a comfortable position with the wound exposed, double sterilised transparent plastic films were placed directly flat and attached to the skin around the wound area by avoiding any movement. The wound margins were traced by the same investigator to ensure reliability of the measurements. The wound perimeter was traced by using the film-tipped transparency marker and each wound was traced three times to establish measurement reliability. After tracing, the side of the transparency film facing the wound was cleaned with a piece of cotton and alcohol. Carbon paper was placed over the 1-mm-squared metric graph paper. The traced transparency film was placed over the carbon paper with white paper in between and the tracing was transcribed onto the metric graph paper. The WSA was calculated by counting the number of square millimetres on the metric graph within the wound tracing. The mean value of the three trials was calculated and taken to be the WSA.
Wound appearance. Changes in wound appearance were evaluated at baseline and after 6 weeks of treatment using a wound assessment tool, the Pressure Sore Status Tool (PSST), also called the Bates-Jensen. It is valid and reliable measurement that characterises changes in the appearance of wound by direct observation29). The PSST is a pen-and-paper tool with 13 domains that use a scale of 1–5 to measure characteristics of wound size and depth, the viability of wound edges, wound exudate, granulation tissue and epithelialization. A total PSST score between 13 and 65 is derived by summing the scores assessed for each of the domains. A lower total PSST scores indicate better wound appearances.
RESULTS
Paired t-tests were performed to examine and compare wound size and appearance within each group. The results revealed that in group I (HILT group), there was highly significant decrease in both wound size and appearance (p<0.0001). Likewise, in group II (sham laser group), there was significant decrease (p<0.0001) in both wound size and appearance (Tables 1 and 3). Unpaired t-tests were performed to examine and compare wound size and appearance between groups, revealing that at pre-study, there was no significant difference in the wound size and appearance mean value between both groups. However, at post-study, there was a significant difference in the wound size and appearance mean value between both groups, in favour of group I (Tables 2 and 4).
Table 1. Wound size mean values prior to and following treatment, Group (I) and Group (II).
| Pre-treatment | Post-treatment | MD | Improvement % | ||
|---|---|---|---|---|---|
| Group I (HILT) | Mean | 5.13 | 0.45 | 4.68* | 91.22 |
| SD | 0.79 | 0.39 | |||
| Group II (Sham) | Mean | 4.98 | 2.90 | 2.08* | 41.77 |
| SD | 0.75 | 0.50 | |||
SD: standard deviation; MD: mean difference; %: percentage; *Significant p<0.05.
Table 3. Wound appearance mean values prior to and following treatment, Group (I) and Group (II).
| Pre-treatment | Post-treatment | MD | Improvement % | ||
|---|---|---|---|---|---|
| Group I (HILT) | Mean | 22.90 | 13.45 | 9.45* | 41 |
| SD | 1.02 | 0.51 | |||
| Group II (Sham) | Mean | 22.75 | 19.15 | 3.6* | 16 |
| SD | 0.97 | 0.88 | |||
SD: standard deviation; MD: mean difference; %: percentage; *Significant p<0.05.
Table 2. Comparative presentation of wound size mean values prior to and following treatment, Group (I) and Group (II).
| Group I (HILT) | Group II (Sham) | MD | ||
|---|---|---|---|---|
| Pre-treatment | Mean | 5.13 | 4.98 | 0.15 |
| SD | 0.79 | 0.75 | ||
| Post-treatment | Mean | 0.45 | 2.90 | 2.45* |
| SD | 0.39 | 0.50 | ||
SD: standard deviation; MD: mean difference; *Significant p<0.05.
Table 4. Comparative presentation of wound appearance mean values prior to and following treatment, Group (I) and Group (II).
| Group I (HILT) | Group II (Sham) | MD | ||
|---|---|---|---|---|
| Pre-treatment | Mean | 22.90 | 22.75 | 0.15 |
| SD | 1.02 | 0.97 | ||
| Post-treatment | Mean | 13.45 | 19.15 | 5.7* |
| SD | 0.51 | 0.88 | ||
SD: standard deviation; MD: mean difference; *Significant p<0.05.
DISCUSSION
This study was designed to determine the effect of pulsed high intensity laser therapy in delayed caesarean section healing in diabetic women. At the end of the treatment program, the results obtained showed that pulsed high intensity laser therapy produced a significant difference in the wound size and appearance (p<0.0001) in comparison with the control group. The mechanism of light action on the cellular level that supports its biological effects is based on the photobiological reaction involving the absorption of a specific wavelength of light by photoreceptor molecules30). The resulting physiological effects included alterations in cell membrane permeability with changes in intracellular calcium levels, increased cellular metabolism, DNA and RNA synthesis, fibroblast proliferation, activation of T lymphocytes, macrophages and mast cells, increased synthesis of endorphins and decreased bradykinin31, 32).
The observed results are in agreement with a previous study reported that low level laser irradiation can be effective in promoting wound healing, and accelerating the caesarean coetaneous wound healing in normal healthy women. However, larger controlled trials are required to more evaluate this aspect of laser use in the wound healing process in normal healthy people. Low-level laser therapy (LLLT) given post-delivery has no negative effects on lactation, and in fact, helps to modulate metabolic processes and improve wound healing25).
The observed results are in consistence with previous study suggested that semiconductor laser irradiation might have auxiliary effects in the early and middle phases of wound healing in diabetic rats33). It has also been shown that laser therapy given three times per week at 4.71 J/cm2 per dose for diabetic burns, and three times per week at 2.35 J/cm2 per dose for diabetic wound healing are recommended for human clinical trials, especially after major surgery in those with impaired healing, such as diabetics and the elderly34). Furthermore, LLLT has been reported to accelerate the healing process of chronic diabetic foot ulcers, and it can be presumed that LLLT may shorten the time period needed to achieve complete healing35).
LLLT in the immediate postoperative period can enhance the tissue repair process in a diabetes model. Similar effects were achieved with laser therapy applied in a single dose with an energy density of 4 J/cm2 and applied four times with an energy density of 1 J/cm2, as application of laser therapy in the inflammatory phase was the most important factor in the enhancement of the tissue repair process36). Moreover, another study reported that the wounds in subjects treated with LLLT contracted significantly more than the wounds in the non-treated group (40.24% vs. 11.87%, p<0.001), which indicates that LLLT is an effective modality to facilitate wound contraction in patients suffering from diabetes and can be used as an adjunct to conventional modes of treatment (dressings and debridement) for the healing of diabetic wounds37). LLLT has also been shown to alter the expression of MMP-9, as well as accelerate the production of collagen and increase the total percentage of collagen type III in diabetic animals38).
In conclusion, pulsed high intensity laser therapy is effective in the treatment of delayed caesarean section healing in diabetic women and should be considered as a treatment method to be used with other therapeutic modalities.
Conflict of Interests
None.
REFERENCES
- 1.Blanc B, Capelle M, Bretelle F, et al. : [The worrying rise in the frequency of cesarean section]. Bull Acad Natl Med, 2006, 190: 905–913, discussion 914 (In French). [PubMed] [Google Scholar]
- 2.Dhar H, Al-Busaidi I, Rathi B, et al. : A study of post-caesarean section wound infections in a regional referral hospital, Oman. Sultan Qaboos Univ Med J, 2014, 14: e211–e217. [PMC free article] [PubMed] [Google Scholar]
- 3.Kwee A, Bots ML, Visser GH, et al. : Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands. Eur J Obstet Gynecol Reprod Biol, 2007, 132: 171–176. [DOI] [PubMed] [Google Scholar]
- 4.Posnett J, Franks PJ: The costs of skin breakdown and ulceration in the UK. In: Pownall M. ed., Skin breakdown: the silent epidemic. Hull, UK: Smith & Nephew Foundation, 2007. [Google Scholar]
- 5.Nwankwo EO, Ibeh I, Enabulele OI: Incidence and risk factors of surgical site infection in a tertiary health institution in Kano, northwestern Nigeria. Int J Infect Control, 2012, 8: 1–6. [Google Scholar]
- 6.Arabshahi KS, Koohpayezade J: Investigation of risk factors for surgical wound infection among teaching hospitals in Tehran. Int Wound J, 2006, 3: 59–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hegazi R, El-Gamal M, Abdel-Hady N, et al. : Epidemiology of and risk factors for type 2 diabetes in Egypt. Ann Glob Health, 2015, 81: 814–820. [DOI] [PubMed] [Google Scholar]
- 8.Mandrup-Poulsen T: Diabetes. BMJ, 1998, 316: 1221–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schäffer MR, Tantry U, van Wesep RA, et al. : Nitric oxide metabolism in wounds. J Surg Res, 1997, 71: 25–31. [DOI] [PubMed] [Google Scholar]
- 10.Reiber GE, Pecoraro RE, Koepsell TD: Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med, 1992, 117: 97–105. [DOI] [PubMed] [Google Scholar]
- 11.Brem H, Kirsner RS, Falanga V: Protocol for the successful treatment of venous ulcers. Am J Surg, 2004, 188: 1–8. [DOI] [PubMed] [Google Scholar]
- 12.European Wound Management Association (EWMA): Position document: hard-to-heal wounds: a holistic approach. London: MEP, 2008. [Google Scholar]
- 13.Conner SN, Verticchio JC, Tuuli MG, et al. : Maternal obesity and risk of postcesarean wound complications. Am J Perinatol, 2014, 31: 299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLean M, Hines R, Polinkovsky M, et al. : Type of skin incision and wound complications in the obese parturient. Am J Perinatol, 2012, 29: 301–306. [DOI] [PubMed] [Google Scholar]
- 15.Subramaniam A, Jauk VC, Figueroa D, et al. : Risk factors for wound disruption following cesarean delivery. J Matern Fetal Neonatal Med, 2014, 27: 1237–1240. [DOI] [PubMed] [Google Scholar]
- 16.Houreld N, Abrahamse H: Low-intensity laser irradiation stimulates wound healing in diabetic wounded fibroblast cells (WS1). Diabetes Technol Ther, 2010, 12: 971–978. [DOI] [PubMed] [Google Scholar]
- 17.Hussein AJ, Alfars AA, Falih MA, et al. : Effects of a low level laser on the acceleration of wound healing in rabbits. N Am J Med Sci, 2011, 3: 193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dawood MS, Salman SD: Low level diode laser accelerates wound healing. Lasers Med Sci, 2013, 28: 941–945. [DOI] [PubMed] [Google Scholar]
- 19.Houreld NN, Abrahamse H: Laser light influences cellular viability and proliferation in diabetic-wounded fibroblast cells in a dose- and wavelength-dependent manner. Lasers Med Sci, 2008, 23: 11–18. [DOI] [PubMed] [Google Scholar]
- 20.Skopin MD, Molitor SC: Effects of near-infrared laser exposure in a cellular model of wound healing. Photodermatol Photoimmunol Photomed, 2009, 25: 75–80. [DOI] [PubMed] [Google Scholar]
- 21.de Oliveira Guirro EC, de Lima Montebelo MI, de Almeida Bortot B, et al. : Effect of laser (670 nm) on healing of wounds covered with occlusive dressing: a histologic and biomechanical analysis. Photomed Laser Surg, 2010, 28: 629–634. [DOI] [PubMed] [Google Scholar]
- 22.Chaves ME, Araújo AR, Piancastelli AC, et al. : Effects of low-power light therapy on wound healing: LASER x LED. An Bras Dermatol, 2014, 89: 616–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basso FG, Pansani TN, Turrioni AP, et al. : In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent, 2012, 2012: 719452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crisan B, Soritau O, Baciut M, et al. : Influence of three laser wavelengths on human fibroblasts cell culture. Lasers Med Sci, 2013, 28: 457–463. [DOI] [PubMed] [Google Scholar]
- 25.Mokmeli S, Khazemikho N, Niromanesh S, et al. : The application of low-level laser therapy after cesarean section does not compromise blood prolactin levels and lactation status. Photomed Laser Surg, 2009, 27: 509–512. [DOI] [PubMed] [Google Scholar]
- 26.Levin ME: Prevention and treatment of diabetic foot wounds. J Wound Ostomy Continence Nurs, 1998, 25: 129–146. [DOI] [PubMed] [Google Scholar]
- 27.Stone JA: Wound healing for foot ulcers. Diabetes Self Manag, 2003, 20: 38–, 40, 42 passim.. [PubMed] [Google Scholar]
- 28.Kloth LC, Feedar JA: Acceleration of wound healing with high voltage, monophasic, pulsed current. Phys Ther, 1988, 68: 503–508. [DOI] [PubMed] [Google Scholar]
- 29.Bates-Jensen BM, Vredevoe DL, Brecht ML: Validity and reliability of the Pressure Sore Status Tool. Decubitus, 1992, 5: 20–28. [PubMed] [Google Scholar]
- 30.Karu T: Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B, 1999, 49: 1–17. [DOI] [PubMed] [Google Scholar]
- 31.Karu TI, Vo-Dinh T: Biomedical photonics handbook, low-power laser therapy. Florida: CRC Press, 2003. [Google Scholar]
- 32.Karu TI, Kolyakov SF: Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg, 2005, 23: 355–361. [DOI] [PubMed] [Google Scholar]
- 33.Hui M, Ying X, Hong C, et al. : Effects of low-intensity laser irradiation on wound healing in diabetic rats. Int J Photoenergy, 2012, 2012: 1–7. [Google Scholar]
- 34.Al-Watban FA: Laser therapy converts diabetic wound healing to normal healing. Photomed Laser Surg, 2009, 27: 127–135. [DOI] [PubMed] [Google Scholar]
- 35.Kaviani A, Djavid GE, Ataie-Fashtami L, et al. : A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg, 2011, 29: 109–114. [DOI] [PubMed] [Google Scholar]
- 36.de Loura Santana C, Silva DF, Deana AM, et al. : Tissue responses to postoperative laser therapy in diabetic rats submitted to excisional wounds. PLoS One, 2015, 10: e0122042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kajagar BM, Godhi AS, Pandit A, et al. : Efficacy of low level laser therapy on wound healing in patients with chronic diabetic foot ulcers-a randomised control trial. Indian J Surg, 2012, 74: 359–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aparecida Da Silva A, Leal-Junior EC, Alves AC, et al. : Wound-healing effects of low-level laser therapy in diabetic rats involve the modulation of MMP-2 and MMP-9 and the redistribution of collagen types I and III. J Cosmet Laser Ther, 2013, 15: 210–216. [DOI] [PubMed] [Google Scholar]