Abstract
[Purpose] The aim of this study was to investigate what outcome measures are reliable in the evaluation of adherence to home exercises among patients with chronic low back pain. [Methods] A systematic review on articles related to adherence to home exercises for patients with chronic low back pain was conducted, and outcome measures and psychometric properties were extracted and evaluated in terms of validity and reliability. [Results] A total of 4,583 articles were identified, and eight articles were finally included after screening. The identified outcome measures were self-reported frequency, duration and intensity of home exercises and Treatment Self-Regulation Questionnaire results. Although the internal consistency and criterion validity of the Treatment Self-Regulation Questionnaire results have been proven in the literature, none of the included articles validated the self-reported frequency, duration, and intensity of the home exercises. [Conclusion] Only the Treatment Self-Regulation Questionnaire results were found to be a reliable measure, and further research to validate self-reported outcome measures is required.
Key words: Patient compliance, Outcome assessment, Low back pain
INTRODUCTION
Chronic low back pain (CLBP) is a significant health problem worldwide. The average prevalence of low back pain (LBP) worldwide is 18.1%1). Further, 32.5% of Japanese patients with LBP have a disability in social activities, such as work and education2). Moreover, the total annual medical cost for occupational LBP in Japan in 2011 was 82.14 billion yen3). Therefore, activity-limiting LBP should be addressed in order to maximize patients’ quality of life (QOL) and to reduce health care costs.
The European guidelines of CLBP4) recommended using exercise therapy because moderate evidence shows that it can alleviate nonspecific CLBP at least in a short duration. Physical therapists prescribe home exercises to their patients to prolong the treatment effects as long as possible5). However, the effectiveness of home exercises has not been proven in the literature, and poor adherence is one of the reasons for such5).
Adherence is defined by the World Health Organization (WHO) as “the extent to which a person’s behavior corresponds with agreed recommendations from a health care provider”6). According to Holden et al.7), patients tend to show poor exercise adherence at a rate of approximately 50%. Patients who did not adhere to exercises showed fewer treatment effects than patients who adhered to such (effect size: 0.16 and 0.42 respectively)8). Moreover, poor adherence caused a higher number of visits to physiotherapy (18.4 times) than good compliance (6.8 times)9). Therefore, adherence could be important to manage patients’ CLBP and to decrease its economic burdens.
There are some interventions provided to improve exercise adherence. For instance, Friedrich et al.10) found that exercise therapy with motivational interventions yielded better adherence to home exercises at a rate of 76.7% than exercise only at a rate of 69.4%. However, the findings of their study were criticized by the WHO6) because Friedrich et al.10) utilized a self-reported diary to measure adherence to home exercises, which is a subjective measure and in which patients may under- or overestimate their frequency of performing home exercises6). Moreover, the outcome measures for adherence to home exercises are not validated in the literature, and invalidated outcome measures may cause measurement bias and reduce the generalizability of the findings of studies7). For these reasons, reliable outcome measures should be first established7). Therefore, the aim of this systematic review is to identify reliable outcome measures for adherence to home exercises among patients with CLBP to conduct more robust research for such.
METHODS
A search was conducted in the databases MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, PsycINFO, PEDro, CINAHL, Web of Science, and AMED. Only English articles were searched, and manual reference searches were not applied. The following key words were utilized: “adherence,’’ “home exercise,’’ and “low back pain,’’ in various combinations.
Study selection was conducted by one author (HU), and articles were evaluated on the basis of the following inclusion criteria: (1) any type of primary research, except for a qualitative study; (2) English language; (3) patients with nonspecific CLBP aged ≥18 years regardless of the presence of sciatica; (4) no history of any operation; (5) any type of interventions and comparisons to enhance adherence to home exercises; and (6) any type of outcomes related to adherence to home exercises, except for the attendance rate. After the selection, the other author (SD) checked the robustness of the selection. Duplicates were eliminated during the evaluations of the articles’ characteristics.
Information on outcome measures for adherence to home exercises was extracted by HU and checked by SD. The name of the measures and how the measures were invented and marked were extracted, and their psychometric properties were evaluated in terms of content validity, internal consistency, criterion validity, construct validity, test-retest reliability, interrater reliability, and responsiveness. The rating was ‘‘yes’’ (if there was discussion on the psychometric properties) or ‘‘no’’ (if there was no discussion on the psychometric properties).
RESULTS
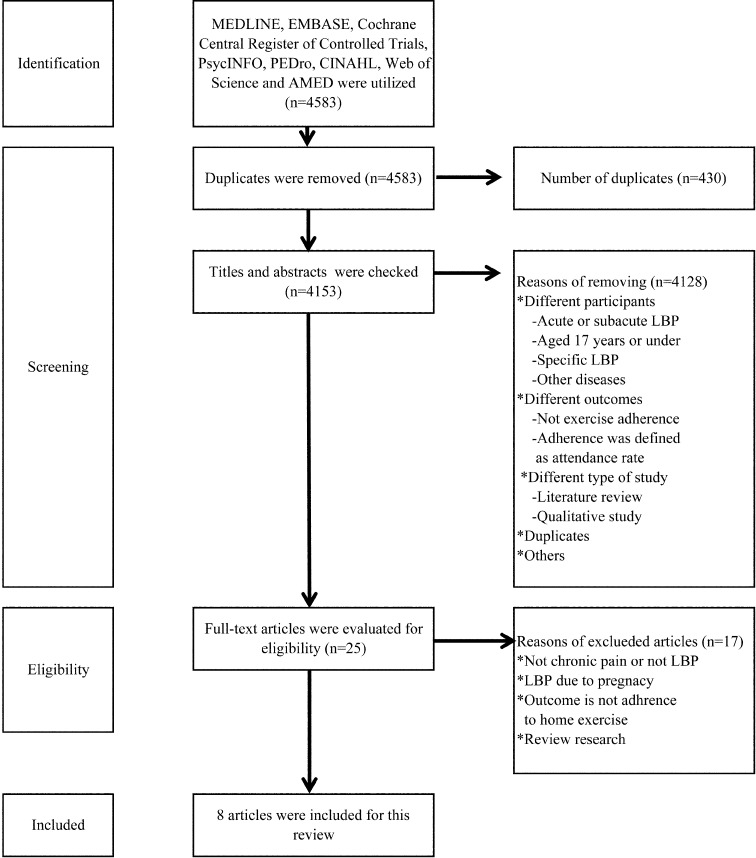
Database searching was conducted on the 20th and 21st of July in 2016. The overview of the study selection is described in Fig. 1 using the PRISMA flow diagram11). A total of 4,583 articles were identified. After screening of the titles and abstracts, full-text reading for 25 studies was conducted to examine their eligibility. Finally, eight articles were included in this review. Four articles10, 12,13,14) were randomized controlled trials, and the other four15,16,17,18) were prospective cohort studies.
Fig. 1.
Flow diagram of study selection.
The main target of this review was the measures for adherence to home exercises; each measure is tabulated in Table 1. Except for the study by Murray et al.14), which used the Treatment Self-Regulation Questionnaire (TSRQ) results, the other included studies utilized frequency as the outcome measure of adherence to home exercises. The frequency of home exercises was measured using a diary10, 12, 15, 17) and a questionnaire16, 18). Ben Salah Frih et al.12) mentioned that the frequency of home exercises was gathered by the researcher; however, there seemed to be no information on the collection of the data. The duration of home exercises was also measured by Linton et al.13) and Medina-Mirapeix et al.18), and both authors used a diary and questionnaire, respectively. Only Linton, Hellsing, and Bergstrom13) evaluated the intensity of home exercises using a diary. Although Medina-Mirapeix et al.18) and Murray et al.14) explained how the outcomes were invented, the other included studies did not mention how they established their outcome measures.
Table 1. Outcome measures for adherence to home exercises.
| Authors | Name of outcome measures | How the measures were invented | How the measures were marked |
|---|---|---|---|
| Alexandre et al.15) | Frequency | No discussion | Diary written by the participants |
| Ben Salah Frih et al.12) | Frequency | No discussion | Assessed by the researchers, but no information on how they collected the participants’ frequency of home exercises |
| Friedrich et al.10) | Frequency | No discussion | Diary written by the participants |
| Hartigan et al.16) | Frequency | No discussion | Questionnaire answered by the participants |
| Linton, Hellsing and Bergstrom.13) | Frequency, duration and intensity | No discussion | Diary written by the participants |
| Mannion et al.17) | Frequency | No discussion | Diary written by the participants |
| Medina-Mirapeix et al.18) | Frequency and duration | Sluijs, Kok, and Zee25) were referred. | Postal questionnaire answered by the participants |
| Murray et al.14) | Autonomous motivation to exercise | Levesque et al.21) were referred. | Treatment Self-Regulation Questionnaire answered by the subjects |
The seven psychometric properties (i.e., content validity, internal consistency, criterion validity, construct validity, test-retest reliability, interrater reliability, and responsiveness) were assessed (Table 2). None of the included articles, except for that by Murray et al.14), discussed any psychometric properties of the measures. Although Murray et al.14) mentioned that the TSRQ results have good validity and reliability, there was no information on which type of properties were validated.
Table 2. Psychometric properties of the measures.
| Authors | Content validity | Internal consistency | Criterion validity | Construct validity | Test-retest reliability | Interrater reliability | Responsiveness |
|---|---|---|---|---|---|---|---|
| Alexandre et al.15) | No | No | No | No | No | No | No |
| Ben Salah Frih et al.12) | No | No | No | No | No | No | No |
| Friedrich et al.10) | No | No | No | No | No | No | No |
| Hartigan et al.16) | No | No | No | No | No | No | No |
| Linton, Hellsing and Bergstrom.13) | No | No | No | No | No | No | No |
| Mannion et al.17) | No | No | No | No | No | No | No |
| Medina-Mirapeix et al.18) | No | No | No | No | No | No | No |
| Murray et al.14) | They mentioned that the Treatment Self-Regulation Questionnaire results have good validity and reliability; however, it was unknown which psychometric properties were proven. | ||||||
DISCUSSION
This review identified that adherence to home exercises in patients with CLBP was evaluated as the frequency, duration, and intensity of home exercises collected using a diary or questionnaire and as autonomous motivation to exercises rated by the TSRQ. Seven studies, except for that by Murray et al.14), utilized the frequency of home exercises as the outcome measure of adherence to home exercises. However, the frequency of home exercises seems to be invalidated by the literature as such19). In fact, none of the included articles mentioned that the frequency of home exercises has good validity and reliability. Furthermore, the WHO6) pointed out that self-reported frequency is a subjective measurement and has a possibility to over- or underestimate the patient’s true frequency of performing home exercises. In fact, Yuen et al.20) compared self-reported duration of home exercises and objective assessment (using Wii-Fit), and different averages of duration were found at 29.5 and 33.3 minutes, respectively. Therefore, using only the self-reported frequency may decrease the validity of a study.
The WHO6) recommended simultaneously using some measures for adherence to home exercises to avoid reducing a study’s validity. For instance, the TSRQ used by Murray et al.14) could be useful to improve a study’s validity. The TSRQ includes 15 items and is a seven-Likert scale questionnaire based on the self-determination theory, and the questions of the TSRQ aim to identify the extent to which a respondent is intrinsically or extrinsically motivated to exercise; the internal consistency and criterion validity of the TSRQ results were proven21). Autonomous motivation seems to be consistent with an internal health locus of control, and a higher health locus of control is a positive factor of adherence to home exercises22). Therefore, in addition to the self-reported frequency of home exercises, the TSRQ results may be worth using to evaluate patients’ autonomous attitude towards exercises.
Some differences between this review and a similar report19) were found. One of the differences was the number of identified measures. The similar report19) found other outcome measures, such as the International Physical Activity Questionnaire and the Sport Injury Rehabilitation Adherence Scale results. The reason for this difference may be that this similar report19) had a wider research question. Jordan et al.19) included patients with chronic musculoskeletal pain, while this present systematic review included only patients with CLBP. Moreover, Jordan et al.19) found the outcome measure of accuracy of home exercises, and this aspect seems to be a missing point of this review. The accuracy of home exercises is rated by healthcare professionals depending on how many times a patient incorrectly conducts his/her exercise23). Although this may not be validated in the literature, using the accuracy of home exercises as well as the self-reported frequency and the TSRQ results could evaluate patients’ adherence to home exercises more reliably. Therefore, this review may answer the research question that the TSRQ results were the only one reliable measure: conversely, using three outcome measures simultaneously (frequency and accuracy of home exercises and the TSRQ results) could be a better method to assess adherence to home exercises among patients with CLBP.
One limitation of this review is the methods of study selection and data extraction. These processes were conducted by only one author (HU). Although the methods of selection and extraction were clearly decided before conducting them and approved by the other author (SD), single-individual checking person has a higher possibility of errors than double-checking24). Another limitation is the study selection; this review included English-written articles only. Liberati et al.11) mentioned that any language should be included because language restriction may cause selection bias. This could reduce the robustness of this review’s results. Therefore, no language restriction is required to determine the validated measures of home exercises in patients with CLBP.
In conclusion, only the TSRQ results were found to be a validated measure in evaluating how a patient with CLBP adheres to home exercises, and further research is needed to measure self-reported exercises more accurately.
Funding
None.
Conflict of interest
None.
REFERENCES
- 1.Hoy D, March L, Brooks P, et al. : Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol, 2010, 24: 155–165. [DOI] [PubMed] [Google Scholar]
- 2.Yamada K, Matsudaira K, Takeshita K, et al. : Prevalence of low back pain as the primary pain site and factors associated with low health-related quality of life in a large Japanese population: a pain-associated cross-sectional epidemiological survey. Mod Rheumatol, 2014, 24: 343–348. [DOI] [PubMed] [Google Scholar]
- 3.Itoh H, Kitamura F, Yokoyama K: Estimates of annual medical costs of work-related low back pain in Japan. Ind Health, 2013, 51: 524–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Airaksinen O, Brox JI, Cedraschi C, et al. COST B13 Working Group on Guidelines for Chronic Low Back Pain: Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J, 2006, 15: S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beattie PF, Silfies SP: Improving long-term outcomes for chronic low back pain: time for a new paradigm? J Orthop Sports Phys Ther, 2015, 45: 236–239. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization: Adherence to long-term therapies: evidence for action. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. (Accessed Jul. 6, 2016)
- 7.Holden MA, Haywood KL, Potia TA, et al. : Recommendations for exercise adherence measures in musculoskeletal settings: a systematic review and consensus meeting (protocol). Syst Rev, 2014, 3: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas KS, Muir KR, Doherty M, et al. : Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ, 2002, 325: 752–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graves JM, Fulton-Kehoe D, Jarvik JG, et al. : Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res, 2014, 49: 645–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedrich M, Gittler G, Halberstadt Y, et al. : Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil, 1998, 79: 475–487. [DOI] [PubMed] [Google Scholar]
- 11.Liberati A, Altman DG, Tetzlaff J, et al. : The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ, 2009, 339: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ben Salah Frih Z, Fendri Y, Jellad A, et al. : Efficacy and treatment compliance of a home-based rehabilitation programme for chronic low back pain: a randomized, controlled study. Ann Phys Rehabil Med, 2009, 52: 485–496. [DOI] [PubMed] [Google Scholar]
- 13.Linton SJ, Hellsing AL, Bergström G: Exercise for workers with musculoskeletal pain: does enhancing compliance decrease pain? J Occup Rehabil, 1996, 6: 177–190. [DOI] [PubMed] [Google Scholar]
- 14.Murray A, Hall AM, Williams GC, et al. : Effect of a self-determination theory-based communication skills training program on physiotherapists’ psychological support for their patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil, 2015, 96: 809–816. [DOI] [PubMed] [Google Scholar]
- 15.Alexandre NM, Nordin M, Hiebert R, et al. : Predictors of compliance with short-term treatment among patients with back pain. Rev Panam Salud Publica, 2002, 12: 86–94. [DOI] [PubMed] [Google Scholar]
- 16.Hartigan C, Rainville J, Sobel JB, et al. : Long-term exercise adherence after intensive rehabilitation for chronic low back pain. Med Sci Sports Exerc, 2000, 32: 551–557. [DOI] [PubMed] [Google Scholar]
- 17.Mannion AF, Helbling D, Pulkovski N, et al. : Spinal segmental stabilisation exercises for chronic low back pain: programme adherence and its influence on clinical outcome. Eur Spine J, 2009, 18: 1881–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medina-Mirapeix F, Escolar-Reina P, Gascón-Cánovas JJ, et al. : Predictive factors of adherence to frequency and duration components in home exercise programs for neck and low back pain: an observational study. BMC Musculoskelet Disord, 2009, 10: 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jordan JL, Holden MA, Mason EE, et al. : Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev, 2010, 20: CD005956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuen HK, Wang E, Holthaus K, et al. : Self-reported versus objectively assessed exercise adherence. Am J Occup Ther, 2013, 67: 484–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levesque CS, Williams GC, Elliot D, et al. : Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res, 2007, 22: 691–702. [DOI] [PubMed] [Google Scholar]
- 22.Beinart NA, Goodchild CE, Weinman JA, et al. : Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J, 2013, 13: 1940–1950. [DOI] [PubMed] [Google Scholar]
- 23.Härkäpää K, Järvikoski A, Mellin G, et al. : Health locus of control beliefs and psychological distress as predictors for treatment outcome in low-back pain patients: results of a 3-month follow-up of a controlled intervention study. Pain, 1991, 46: 35–41. [DOI] [PubMed] [Google Scholar]
- 24.Buscemi N, Hartling L, Vandermeer B, et al. : Single data extraction generated more errors than double data extraction in systematic reviews. J Clin Epidemiol, 2006, 59: 697–703. [DOI] [PubMed] [Google Scholar]
- 25.Sluijs EM, Kok GJ, van der Zee J: Correlates of exercise compliance in physical therapy. Phys Ther, 1993, 73: 771–782, discussion 783–786. [DOI] [PubMed] [Google Scholar]