Abstract
Pediatric proximal femur fractures are rare injuries resulting from high-energy trauma. The Delbet classification is used when describing these injuries, and associates fracture type to the development of avascular necrosis. Historically, casting was utilized in the treatment of these injuries, but high complication rates following this approach have changed the treatment modality to early and anatomic fixation. Complications associated with these injuries including avascular necrosis, non-union, coxa-vara, and premature physeal fusion. Achieving anatomic reduction and performing internal fixation within 24 h from time of injury has become the standard of care in the treatment of pediatric proximal femur fractures.
Keywords: Pediatric proximal femur fracture, Pediatric hip fracture, Children hip fracture, Pediatric femoral neck fracture, Delbet classification
1. Introduction
Proximal femur fractures in the pediatric patient are rare, accounting for less than one percent of all pediatric fractures.1 In contrast to the elderly patient with osteoporotic bone who sustains a hip fracture from a minor fall, the high bone mineral density in the pediatric patient requires significant trauma to fracture. Historically, the treatment of these rare injuries was incompletely understood, and resulted in poor outcomes with high complication rates. As the volume of literature on this topic has expanded, the treatment methods have become more standardized, and outcomes have improved.
Pediatric hip fractures result from significant trauma with 90% of fractures occurring from motor vehicle collisions and high-energy falls.1, 2, 3, 4 The 10% of hip fractures that occur from low energy mechanisms such as a fall from standing or a twisting mechanism require investigation into underlying metabolic bone diseases, pathologic lesions, and for the possibility of child abuse.
Understanding the management of pediatric hip fractures is necessary to prevent and adequately educate the patient and the patient’s family about the serious complications with these injuries. The most serious complication is osteonecrosis of the femoral head. The vascular supply to the femoral head in the child varies from the vascular supply in the skeletally mature patient, and this vascular variation places the child at greater risk of developing AVN. Scientific investigation of these injuries, since the late 19th century has been to identify precipitating factors leading to poor outcomes, and to standardize the management of theses fractures to reduce the inherent complications of the injury.
2. Vascular anatomy of the proximal femur
An understanding of the vascular anatomy of the proximal femur in children, specifically the transitioning vasculature of the femoral head, is essential to understanding many disease processes of the pediatric hip. Trueta’s research in the 1950s laid the foundation for investigating the dynamic nature of the femoral head’s vascular supply.5 The vascular supply to the pediatric proximal femur will be discussed in terms of three stages (1) birth till formation of the subcapital physis, (2) during ossification of the femoral epiphysis, and (3) following ossification of the physis (Fig. 1, Fig. 2).
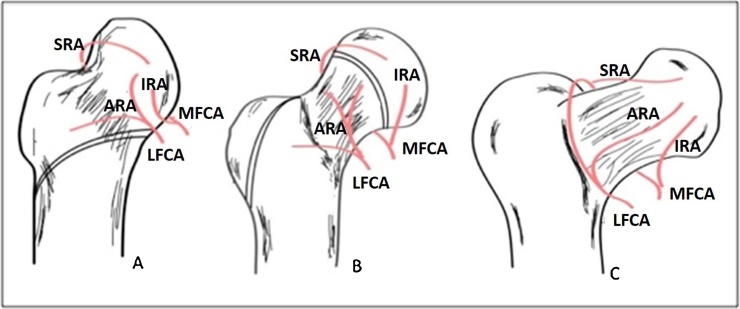
Fig. 1.
Vascular anatomy of the pediatric proximal femur. The image also depicts the progressive femoral neck-shaft angle from 150° in the newborn to 130° in the skeletally maturity. A, Stage 1 with tri-vessel supply. B, Stage 2, the ARA no longer supplies the femoral head due to the physis. C, Stage 3 the skeletally mature vascular supply. MFCA – medial femoral circumflex artery, LFCA – lateral femoral circumflex artery, SRA – superior retinacular artery, IRA – inferior retinacular artery, ARA – anterior retinacular artery.
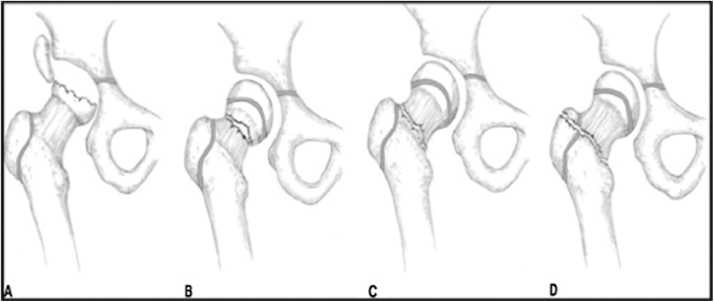
Fig. 2.
The Delbet classification of pediatric proximal femur fractures. A, type 1 transepiphyseal fracture. B, type II transcervical fracture. C, type III basicervical fracture. D, type IV intertrochanteric fracture.4
In the first stage, typically during the first 4 to 6 months of life, the blood supply to the femoral head comes from three vessels, the medial femoral circumflex artery (MFCA), the lateral femoral circumflex artery (LFCA), and the artery of the ligamentum teres (ALT). The MFCA courses along the posterior head-neck junction to supply the posterior greater trochanter, the subcapital physis, the posteromedial metaphysis, and the capital epiphysis. The LFCA courses anterior at the head-neck junction and supplies areas of the anterior greater trochanter, the subcapital physis, the anteromedial metaphysis, and the capital epiphysis.5,6 Prior to the development of the subcapital physis the retinacular vessels from the MFCA and LFCA traverse along the femoral neck within capsular extensions termed the retinaculum of Weinbreicht. These vessels freely pass from the femoral neck to the femoral head without interference by the growth plate.5,6.
In the second stage, from 4 to 6 months of age until skeletal maturity, the blood supply to the femoral head is derived solely from the MFCA. The presence of the subcapital physis blocks the retinacular vessels of the LFCA from crossing the growth plate, and the terminal branches of the MFCA must course around the growth plate through the perichondrial ring to supply the epiphysis.6 The two terminal branches of the MFCA that supply the femoral head are the superior retinacular artery and the inferior retinacular artery. The superior retinacular artery is the main supply to the femoral head, and historically has been described by varying nomenclature including the lateral epiphyseal artery, the lateral ascending artery, and the posterosuperior artery.5,6 The superior retinacular artery branches from the MFCA at the posterosuperior aspect of the femoral neck, within the piriformis fossa, and travels around the subcapital physis to supply the epiphysis. The anterior retinacular artery, a branch of the LFCA that had previously supplied the femoral head remains distal to the femoral head as the neck elongates and supplies the femoral neck.
In the third stage, the blood supply to the femoral head is primarily derived from the MFCA; however limited contributions from the LFCA and ALT once more contribute. Following ossification of the subcapital physis blood vessels pass from the femoral neck into the femoral head along the entire diameter of the femoral neck. The MFCA and the LFCA form an extracapsular ring at the intertrochanteric line. Retinacular arteries extend from this extracapsular ring to supply the metaphysis and epiphysis. The majority of the femoral head is still supplied by the superior retinacular artery. The anterior retinacular artery branching from the LFCA is responsible for supplying the anterolateral aspect of the femoral head.
Most commonly, disruption of the superior retinacular artery or the MFCA leads to avascular necrosis.7 Hypothetically, the greater degree of AVN in pediatric femoral neck fractures compared to adult femoral neck fractures results from (1) the MFCA being the sole blood supply to the femoral head during the majority of childhood versus the collateral flow from the LFCA and ALT in adults and (2) the high-energy mechanisms of injury required to produce a femoral neck fracture in children resulting in a higher rate of superior retinacular artery injury.
3. Fracture classification
Pediatric hip fractures are classified into transphyseal, transcervical, cervicotrochanteric, and intertrochanteric fractures by the Delbet classification system. The Delbet classification relates the location of fracture to the risk of AVN. In 2007, the Arbeitsgemeinschaft für Osteosynthesefragen (AO) released their classification system for pediatric fractures, and separated pediatric transphyseal fractures (Delbet I) from pediatric femoral neck and intertrochanteric fractures (Delbet II–IV). The Delbet classification remains the most commonly used classification system when discussing these fractures (Fig. 1).
Type I, transphyseal fractures, result from traumatic separation of the femoral head from the femoral neck through the subcapital physis. Type I fractures are the least common hip fractures in children, accounting for only 7%, and carry the worst prognosis for developing AVN, 40%.8 Traumatic transphyseal seperations are further classified into type 1A, without femoral head dislocation, and type 1B, with femoral head dislocation.9 The rate of AVN is worse with type 1B injuries compared to type 1 A, with the largest series demonstrating the rate of AVN being 75% with type 1B.9 These injuries are typically the result of high-energy trauma, traumatic delivery in newborns, and seizures (Fig. 3).
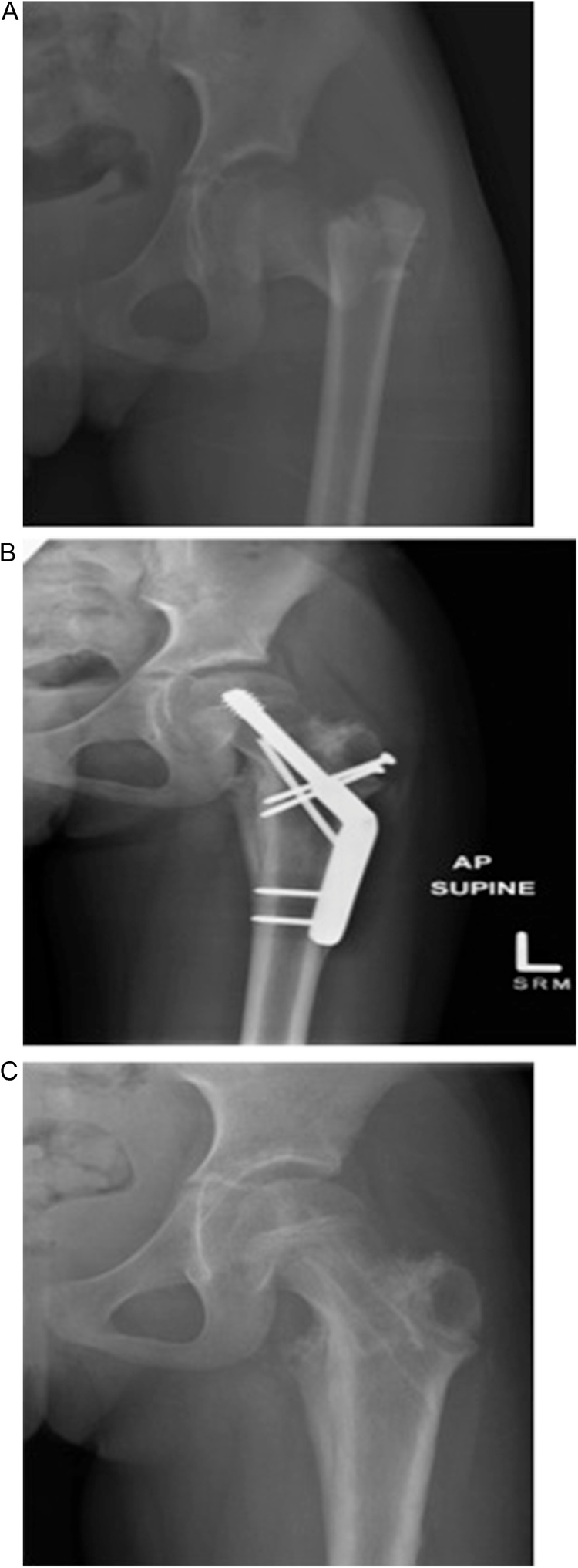
Fig. 3.
A) A 13 year-old boy who sustained a Delbet IA fracture during a snowmobiling accident. B) Two partially threaded screws were used to stabilize the fracture. These screws are inserted through the physis.4 C) For comparison, this is a radiograph of a child who experienced a Delbet IB fracture, the femoral head has dislocated from the acetabulum.
Type II, transcervical fractures occur through the central zone of the femoral neck. This is the most common type of proximal femur fracture accounting for 47% of pediatric hip fractures.8 These fractures are associated with a 27% risk developing AVN.8
Type III, cervicotrochanteric (or basicervical) fractures, occur at the base of the femoral neck. These fractures account for approximately 35% of pediatric hip fractures, and carry a 20% risk of developing AVN.8
Type IV, intertrochanteric (or pertrochanteric) fractures, extend from the greater trochanter to the lesser trochanter. These fractures account for approximately 10% of all proximal pediatric femur fractures, and have the lowest rate of developing AVN, only 5%.8
Pathologic and stress fractures are also seen in the proximal femur. Common etiologies leading to pathologic fractures include bone cysts, fibrous dysplasia, osteogenesis imperfecta, osteomyelitis, myelodysplasia, and metabolic bone diseases. Stress fractures of the femoral neck may occur in an active child, and typically present as progressive vague groin pain.
4. Radiographic evaluation
Initial imaging needs to include an anterior posterior (AP) x-ray of the pelvis and a cross table lateral x-ray of the affected hip, AP and lateral x-rays of the ipsilateral femur, and imaging of the ipsilateral knee. A cross table lateral is recommended over a frog leg lateral to prevent further fracture displacement by manual manipulation.
Assessment of the radiographs should include classification of the fracture, evaluating the degree of displacement, and noting the angle of the fracture line in accordance with the Pauwel’s classification. In addition, the skeletal maturity of the patient and degree of physeal ossification are important for surgical planning. The cross table lateral radiograph needs to be assessed for associated anterior versus posterior femoral head dislocation and for the degree of posterior tilt at the fracture site.
For a child with insidious and progressive hip pain, magnetic resonance imaging (MRI) is the study of choice to detect a stress fracture or an occult hip fracture. The T1 weighted coronal MRI scan is the gold standard to assess for occult femoral neck fractures having nearly 100% sensitivity for detection.10
5. Management of the pediatric hip fracture
5.1. Clinical assessment and initial management
The pediatric patient with a proximal femur fracture presents following significant trauma, most commonly a motor vehicle crash or a fall from a height. The injury commonly occurs from a shear force along the femoral neck as an axial load is applied through an abducted knee producing the vertical fracture pattern often seen in children. A trauma evaluation of these patients is indicated due the high-energy nature of the injury. In the medically stable patient, a complete history should be obtained, including mechanism of injury, history of chronic hip pain, history of previous fractures, and family history of genetic bone diseases. If child abuse is suspected, child protective services needs to become involved early in the child’s care. A thorough neurovascular exam needs to be conducted along the effected extremity, and a complete musculoskeletal survey should assess for additional injury.
A pillow should be positioned underneath the effected knee to keep the leg in a slight amount of flexion and external rotation, and to minimize manipulation of the extremity. The position of flexion and external rotation increases the volume of the hip capsule, and theoretically may improve blood flow to the femoral head in the setting of an intracapsular hematoma.11 Traction should not be used in these patients, first in adult studies traction was not shown to decrease pain, and secondly traction forces the leg into extension decreasing the volume of the hip capsule.11
5.2. Timing of reduction
The importance of early reduction, historically, has been a matter of debate. More recently, the literature regarding outcomes with early versus late reduction and fixation favors early reduction.8,12 The theory supporting early reduction is that following injury the vasculature supply to the femoral head “kinks” reducing approximately 60% of the blood flow to the femoral head [25]. Early reduction “unkinks” these vessels reducing ischemic injury to the femoral head. Authors who find no difference with development of AVN and early reduction rely on the theory that the initial injury determines the development of AVN irrespective of how the injury is managed.2 Although authors have debated on the urgency of fracture reduction following a pediatric hip fracture we believe that the literature suggests that an early anatomic reduction reduces the risk of AVN.
5.3. Reduction technique
Anatomic reduction in pediatric hip fractures is mandatory. Closed reduction should be attempted as a primary means of fracture reduction in all hip fractures other than Delbet Type IB. In type 1B fractures the success rate of closed reduction is low, and multiple attempts at closed reduction may increase the rate of AVN.9 The reduction maneuver for a Type IA fracture, similar to the reduction technique for a slipped capital femoral epiphysis (SCFE), is to slowly flex the hip while abducting and internally rotating the leg. For types II, III, and IV fractures the closed reduction maneuver is to first apply longitudinal traction to overcome shortening, second to abduct the leg to correct the varus deformity, and finally to internally rotate the extremity to key in the reduction.
Open reduction of pediatric femoral neck fractures allows for direct visualization of the fracture site and necessitates intracapsular decompression. The surgical approach is primarily dictated by the Delbet classification. Proximal fractures (Delbet IA and II) typically require a direct anterior approach whereas the basicervical and intertrochanteric (Delbet III and IV) can be easily visualized via an anterolateral approach. Patients with a Delbet IB fracture may require a posterior approach to reduce the femoral head. Some authors have found decreased complication rates following open reduction when compared to closed reduction, and recommend open reduction for all pediatric hip fractures.13,14 However, there remains no consensus in the literature as others have shown equivocal results with open and closed methods.2,8,12 Open reduction of the hip fracture is required if an acceptable reduction cannot be achieved by closed means or if the fracture is associated with an underlying vascular injury.
5.4. Capsular decompression
In displaced hip fractures vascular compromise to the femoral head occurs due to vascular kinking, however in non-displaced fractures the mechanism is less clear. One theory is that fracture hematoma forms within the hip capsule resulting in a compartment syndrome like phenomenon of the retinacular vessels. A number of authors have speculated on the utility of capsular decompression, either by anterior hip capsulotomy or needle decompression, however, only a few studies have provided objective evidence towards or against the utility of decompression.14, 15, 16 These studies found statistically significant fewer complications when capsulotomy was performed. One study found increased rates of AVN with capsulotomy, but the study results were likely confounded by all treatments being delayed greater than 24 h following initial injury. Capsular decompression is often debated in the adult hip fracture literature as well, one difference to consider in the pediatric patient is that the consequences AVN are much more devastating, as the adult patient has the option of arthroplasty. Therefore, as hip decompression may decrease the rate of AVN, and have minimal to no additional harmful consequences to the patient, hip decompression should be instituted as part of the surgical treatment in all pediatric patients being treated within 24 h of surgery.
5.5. Fixation technique
The goal of fracture management is anatomic fixation providing the greatest possible functional outcome and to avoid the development of non-union or AVN. Casting, historically, played a prominent role in the treatment of these injuries; however recently the higher reported rates of coxa-vara and nonunion with casting has shifted the trend towards stable fixation.3,17,18
Osteosynthesis can be achieved using cannulated screws, smooth pins, or a pediatric sliding hip screw (SHS). Specific algorithms for hardware selection do not exist for the pediatric hip fracture, and means of fixation are largely dependent on the surgeon’s preferences. In adult hip fractures, biomechanics studies have concluded that three screws in an inverted triangle orientation is the optimal stabilization for non-displaced femoral neck fractures. In pediatric hip fractures biomechanics data does not exist to guide fixation method. Typically, two cannulated screws, two smooth pins, or a combination of a screw and a pin are used to stabilize the fracture site. Utilization of at least two screws or pins prevents rotation at the fracture site, and is recommended. In pediatric hip fractures, despite the theoretical increased stability with additional hardware two aspects need to be considered (1) the smaller diameter of the pediatric femoral neck places the superior and inferior retinacular arteries at increased risk with additional hardware, and (2) increasing the number of pins or screws has been shown to be directly correlated to increased risk of hardware penetration.
Biomechanical data on the fixation method in SCFE patients can provide, albeit with caution, insight into hardware selection for proximal femur fractures. Biomechanics data has shown that a single cannulated screw is 77% as stable as two cannulated screws, compression across the physis with a cannulated screws provides increased stability compared to pinning, and increasing the number of pins or screws increases the risk for hardware penetration.
General considerations for the treatment of these fractures can be organized as follows; (1) attempt to use three screws or pins for fixation, except for type I injuries and in younger patients with smaller diameter femoral necks, (2) Attempt to avoid the femoral epiphysis with fixation, except in the adolescent nearing skeletal maturity, to prevent premature physeal fusion, and if it is necessary to cross the physis do so with smooth pins at the mid-point of the physis, (3) a pediatric SHS should be used for Delbet type IV injuries, and should be considered for type III injuries, and (4) a hip spica cast may be necessary for up to six weeks following surgery.
6. Specific fixation consideration based on type of injury
6.1. Delbet type I fracture
Some experts advocate for hip spica casting for non-displaced transphyseal fractures in children less than 4 years of age.4 Patients older than 4 years of age and all displaced fractures require stable fixation with either smooth pins or cannulated screws. The fracture occurs through the physis, therefore instrumentation must traverse the growth plate. It is recommended to remove the hardware following fracture healing to prevent leg length discrepancy, except in those patients approaching skeletal maturity. Following fixation the patient should remain non-weight bearing in a hip spica cast or abduction orthosis for six weeks (Fig. 3).
6.2. Delbet types II/III fractures
Type II and type III fractures are unstable, and require internal fixation.3,13,14,17,18 Hip spica immobilization as the primary means of treatment is not recommended for any aged child or any degree of displacement; the instability of the fracture pattern results in loss of reduction with casting alone.3,18 In proximal type II fractures transphyseal instrumentation is necessary, and should be removed following fracture healing. In distal type II fractures and type III fractures hardware should remain distal to the physis. Following fixation the patient should remain non-weight bearing in a hip spica cast or abduction orthosis for six weeks (Fig. 4, Fig. 5).
Fig. 4.
A) 12 year-old boy presents with a non-displaced transcervical fracture (Delbet II). B) Three 6.5 m m partially threaded screws were inserted in an inverted triangle configuration. The screws do not cross the physis, and a washer was used for further stabilization with the inferior screw.
Fig. 5.
A) Basicervical fracture (Delbet III) with an associated greater trochanter fracture in a 7 year-old girl following a MVC B) A pediatric sliding hip screw (SHS) was used for primary stabilization, and a second screw was used to control rotation. In addition, two screws were used to stabilize the greater trochanteric fracture. C) Following fracture healing the hardware was removed to prevent physeal arrest.
6.3. Delbet type IV fractures
Pediatric intertrochanteric fractures are typically stable, and have a low risk of developing AVN. Hip spica casting can be used as the primary treatment method in children less than 8 years of age. Internal fixation with a pediatric SHS is indicated for older children, and in those who fail treatment with external immobilization. Weekly radiographs are recommended for the first two weeks or until fracture callus is visualized for the patient being managed in a hip spica cast. In the patient’s managed with a pediatric SHS he or she may be weight bearing as tolerated following fixation (Fig. 6).
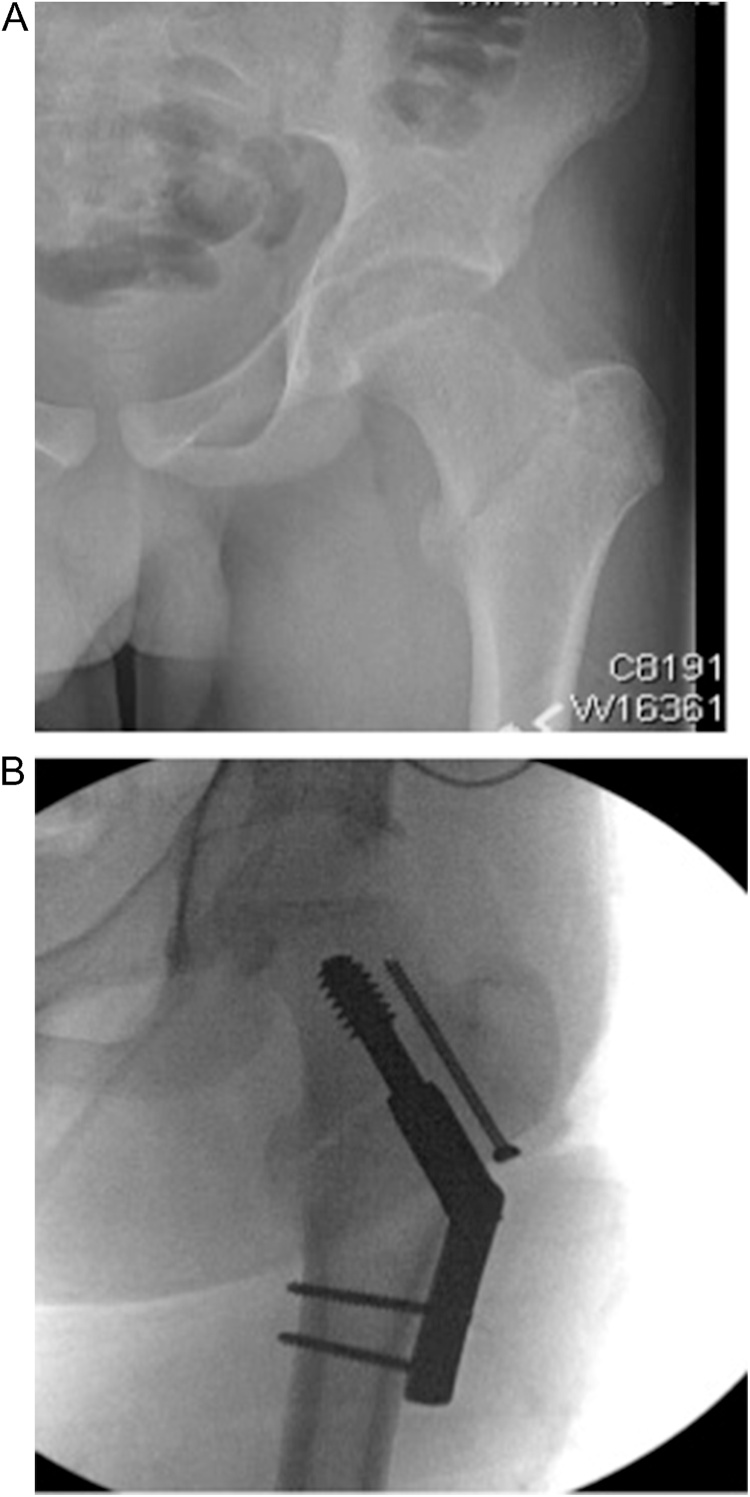
Fig. 6.
A) An intertrochanteric fracture (Delbet IV) in a patient approaching skeletal maturity. B) Intra-operative fluoroscopy showing a standard hip screw (SHS) was used for primary stabilization, and a partially threaded screw was inserted across the fracture site to prevent rotation.
7. Complications
7.1. AVN
AVN of the femoral head is the most devastating complication following a pediatric hip fracture, and its incidence following injury is 40%, 27%, 20%, and 5% for fracture types I through IV respectively.8 These rates are significantly lower than the original rates of AVN published by Delbet and others. The decreased incidence of AVN following hip fracture is likely attributable to advances in management over time.
Numerous authors have attempted to identify modifiable and non-modifiable risk factors for the development of AVN. Non-modifiable risk factors include patient’s age at time of injury, fracture type, and degree of fracture displacement. Modifiable risk factors include timing to reduction, quality of reduction, capsular decompression, and stability of fixation. Three studies have attempted to identify these risk factors in the setting of current treatment protocols. Moon and colleagues found that the fracture type and age of the patient were significant risk factors for developing AVN. They hypothesized that older children had a decreased ability to revascularize their femoral head.19 Yeransonian et al. found that delay in treatment increased risk of AVN along with fracture type.8 And, Spence et al. published that fracture type and displacement affected AVN rates, but did not find that patient age, type of fixation, mechanism of injury, capsular decompression, and quality of reduction could be used to predict AVN risk.2 Summarizing these three articles, and other smaller series looking at this issue, fracture type, degree of displacement, timing till reduction, and quality of reduction all impact the development of AVN. The data is insufficient to say whether patient’s age, capsular decompression, and type of osteosynthesis impact osteonecrosis (Fig. 5, Fig. 6 ).
Radiographic and clinical evidence of AVN typically presents between two and 12 months of injury.1,4,7 Post operatively, radiographs should be obtained every three to six months for the first year, and then once at two years following injury. The first clinical symptoms of AVN usually are groin, proximal femur, or buttock pain and decreased hip range of motion. Radiographically, the first evidence of AVN presents as osteopenia of the femoral head, this is followed by sclerosis, fragmentation, and ultimately collapse.
7.2. Coxa-Vara
The decreased neck-shaft angle that may complicate pediatric femoral neck fractures is a cause of acquired coxa-vara. Coxa-vara is defined as a decrease in neck shaft angle of the proximal femur when compared to the contralateral hip, or a neck shaft angle <120° in the skeletally mature patient. Post-traumatic coxa-vara may develop following loss of reduction at the fracture site, the development of avascular necrosis, non-union, or premature closure of the epiphysis. Most recently the incidence was reported as 18% when all types of hip fractures were investigated together.8 Historically, the incidence was reported to be as high as 62% with the use of hip spica casting in displaced femoral neck fractures. The transition from external mobilization to internal fixation has reduced the occurrence of coxa vara. Coxa vara results in decreased hip abductor strength and a mild limb length discrepancy that functionally limits the patient. One study demonstrated that a difference of greater 10° in the neck shaft angles between the two hips becomes clinically significant.17
7.3. Non-union
Non-unions result from inadequate fixation at the fracture site, most commonly occurring when casting is used as definitive treatment. The incidence of non-union following pediatric proximal femur fractures is 11%.8 Non-unions need to be addressed surgically when diagnosed to prevent AVN and coxa vara from developing. As discussed throughout this review, vascular injury is common, and likely contributes to the poor healing at the fracture site. Other factors associated with non-unions are non-anatomic reductions and vertical femoral neck fractures.
7.4. Premature physeal arrest
Premature epiphyseal arrest may occur from (1) direct injury to the physis during the trauma, (2) injury to the phseal vascular supply during the initial injury, and/or (3) iatrogenically from hardware crossing the physis. Following arrest of the subcapital physis the patient may developing a limb length discrepancy or angular deformity of the hip. The proximal femur contributes to 13–15% of the entire length of the lower extremity, approximately 3 mm per year, and depending on the expected growth remaining in the child this may or may not become significant. In the pediatric patient approaching skeletal maturity crossing the physis with hardware is acceptable and even recommended for the increased stability of the construct. In younger children, where premature growth plate closure would result in greater than a 2 cm leg length discrepancy avoidance of the physis should be attempted, and if the fracture pattern necessitates crossing of the physis it should be crossed with smooth pins that are removed following fracture healing.
8. Summary
Pediatric hip fractures are rare but potentially devastating injuries. They are most often the result of high energy trauma but can result from pathologic bone. Avascular necrosis of the femoral head carries the worst prognosis as a complication of hip fractures so thorough knowledge of the variable anatomy of the vascular supply to the femoral head in children is mandatory. Early recognition and operative management of pediatric hip fractures has improved outcomes.
Conflict of interest
None.
Funding
No external funding or support was received for the conduct of this research and/or preparation of the article.
References
- 1.Ratliff A.H. Fractures of the neck of the femur in children. J Bone Jt Surg. 1962;44B(3) doi: 10.1302/0301-620X.44B3.528. [DOI] [PubMed] [Google Scholar]
- 2.Spence D., DiMauro J.P., Miller P.E., Glotzbecker M.P., Hedequist D.J., Shore B.J. Osteonecrosis after femoral neck fractures in children and adolescents: analysis of risk factors. J Pediatr Orthop. 2016;36(2):111–116. doi: 10.1097/BPO.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 3.Bali K., Sudesh P., Patel S., Kumar V., Saini U., Dhillon M.S. Pediatric femoral neck fractures: our 10 years of experience. Clin Orthop Surg. 2011;3(4):302–308. doi: 10.4055/cios.2011.3.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boardman M.J., Herman M.J., Buck B., Pizzutillo P. Hip fractures in children. JAAOS. 2009;17(3):162–173. doi: 10.5435/00124635-200903000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Trueta J. The normal vascular anatomy of the human femoral head during growth. J Bone Jt Surg Br. 1957;39-b(2):358–394. doi: 10.1302/0301-620X.39B2.358. [DOI] [PubMed] [Google Scholar]
- 6.Ogden J.A. Changing patterns of proximal femoral vascularity. J Bone Jt Surg Am. 1974;56(5):941–950. [PubMed] [Google Scholar]
- 7.Ehlinger M., Moser T., Adam P. Early prediction of femoral head avascular necrosis following neck fracture. Orthop Traumatol Surg Res. 2011;97(1):79–88. doi: 10.1016/j.otsr.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Yeranosian M., Horneff J.G., Baldwin K., Hosalkar H.S. Factors affecting the outcome of fractures of the femoral neck in children and adolescents: a systematic review. Bone Jt J. 2013;95-b(1):135–142. doi: 10.1302/0301-620X.95B1.30161. [DOI] [PubMed] [Google Scholar]
- 9.Akahane T., Fujioka F., Shiozawa R. A transepiphyseal fracture of the proximal femur combined with a fracture of the mid-shaft of ipsilateral femur in a child: a case report and literature review. Arch Orthop Trauma Surg. 2006;126(5):330–334. doi: 10.1007/s00402-005-0028-y. [DOI] [PubMed] [Google Scholar]
- 10.Iwata T., Nozawa S., Dohjima T. The value of T1-weighted coronal MRI scans in diagnosing occult fracture of the hip. J Bone Jt Surg Br. 2012;94(7):969–973. doi: 10.1302/0301-620X.94B7.28693. [DOI] [PubMed] [Google Scholar]
- 11.Drake J.K., Meyers M.H. Intracapsular pressure and hemarthrosis following femoral neck fracture. Clin Orthop Relat Res. 1984;(182):172–176. [PubMed] [Google Scholar]
- 12.Dendane M.A., Amrani A., El Alami Z.F., El Medhi T., Gourinda H. Displaced femoral neck fractures in children: are complications predictable? Orthop Traumatol Surg Res. 2010;96(2):161–165. doi: 10.1016/j.rcot.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Stone J.D. Open reduction of pediatric femoral neck fractures reduces osteonecrosis risk. Orthopedics. 2015;38(11):e983–e990. doi: 10.3928/01477447-20151020-06. [DOI] [PubMed] [Google Scholar]
- 14.Panigrahi R. Treatment analysis of paediatric femoral neck fractures: a prospective multicenter theraupetic study in Indian scenario. Int Orthop. 2015;39(6):1121–1127. doi: 10.1007/s00264-015-2677-y. [DOI] [PubMed] [Google Scholar]
- 15.Ng G.P., Cole W.G. Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury. 1996;27(6):419–421. doi: 10.1016/0020-1383(96)00025-3. [DOI] [PubMed] [Google Scholar]
- 16.Bukva B., Abramovic D., Vrgoc G. Femoral neck fractures in children and the role of early hip decompression in final outcome. Injury. 2015;46(Suppl. 6):S44–S47. doi: 10.1016/j.injury.2015.10.059. [DOI] [PubMed] [Google Scholar]
- 17.Eberl R., Singer G., Ferlic P., Weinberg A.M., Hoellwarth M.E. Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthop. 2010;81(4):442–445. doi: 10.3109/17453674.2010.501744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forster N.A., Ramseier L.E., Exner G.U. Undisplaced femoral neck fractures in children have a high risk of secondary displacement. J Pediatr Orthop B. 2006;15(2):131–133. doi: 10.1097/01.bpb.0000188249.17148.eb. [DOI] [PubMed] [Google Scholar]
- 19.Moon E.S., Mehlman C.T. Risk factors for avascular necrosis after femoral neck fractures in children: 25 cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma. 2006;20(5):323–329. doi: 10.1097/00005131-200605000-00005. [DOI] [PubMed] [Google Scholar]