Abstract
Whether to recommend mastectomy in metastatic disease or not has been a matter of debate. Is local therapy, such as mastectomy, of any benefit in advanced breast cancer is the main question. This expert group used data from published literature, practical experience and opinion of a large group of academic oncologists to arrive at these practical consensus recommendations for the benefit of community oncologists.
Keywords: Imaging CR, liver and lung metastasis, response, systemic therapy
Introduction
There is a lack of consensus over the value of surgery as part of the treatment of metastatic breast cancer. The role of removal of the primary tumor in patients with metastatic disease has traditionally been relegated to palliation alone and not expected to have any impact on survival of the patient. However, some recent studies have shown that surgery might have some role in improving the overall survival of stage IV breast cancer patients, thus opening to debate the role of mastectomy in metastatic breast cancer patients.
Expert oncologists from all over India met to discuss and reach a consensus statement to provide community oncologists practical guidelines on whether mastectomy is a possible option in a patient with metastatic disease and if yes, what is its exact role. The discussion was based on published evidence and practical experience in real life management of such patients. The expert group discussions were moderated by Dr Somashekhar S P and Dr K Geeta.
The core expert group consisted of Dr Rajesh Jain, Dr Rakesh Koul and Dr Rohit Nayyar. Members of the panel were also allowed to share their personal experiences and make comments. This manuscript is the outcome of the expert group discussion and consensus arrived at in 2017.
Defining Clinical Cohort and Practice of Expert Group Panel Members
The primary objective was to provide a consensus statement for community oncologists that could be applicable as ready-to-use practical recommendations. Hence, the applicable setting was outlined by defining the clinical cohort and current practice of the participating delegates and expert group panel members – on the basis of which this document was prepared. The experts discussed a case of a 45 year premenopausal lady who was diagnosed with infiltrating duct carcinoma in left breast (5 cm) and multiple bone metastases. Core biopsy showed ER-ve, PR-ve but Her2 neu 3+. The Patient was treated with TCH protocol. After 6 cycles there was complete response in bones on PET CT. However, a 1.5 cm palpable breast lump was still present. Based on this case, a series of questions were put up for poll upon which the expert group discussed and aimed to reach a consensus. Each question had multiple choice options from which participants were to select the one most appropriate for their clinical practice setting. The expert group then formed the practical consensus recommendations for the community oncologists.
Is Mastectomy a Beneficial Option for Stage Iv Patients?
A total of 77.3% of the polled oncologists were in support of recommending mastectomy in stage IV breast cancer patients [Table 1], when the chemotherapy led to complete resolution of the metastatic lesions. Current published recommendations for treatment of such advanced stage IV disease does not include resection, as evidence of a survival benefit from primary resection in such cases is lacking.[1] Also, in an open-label, randomised controlled trial from India, 350 patients with metastatic breast cancer were randomly assigned into two groups: 173 to locoregional treatment and 177 to no locoregional treatment. The median overall survival was similar between the two arms, being 19·2 months in the locoregional treatment group and 20·5 months in the no-locoregional treatment group.[2] The rebuttal for this negative study is that, the patients did not receive recommended standard systemic therapy and anti Her-2-neu therapy, which impacted the OS and also there was no segregation and subset analysis of HR + ve cases and Oligometastases cases. In contrast, a recent Turkish study suggests that primary tumor resection is an independent factor in improving the median overall survival, especially for specific subgroups – bone only metastasis, hormone receptor positive patients, Her2 negative patients and younger patients.[3,4] In fact, because of the finding in metastatic renal cell carcinoma that radical nephrectomy improves survival,[5,6] there has been an increased interest in evaluating the role of removal of the primary tumor in metastatic breast cancer as well. Two older studies analyzing stage IV breast cancer patients had also indicated that the patients who had surgery had a better median Overall Survival than the patients who did not have surgery. The difference in the median Overall Survival was at least 11 months.[7,8] Another potential advantage of resection of the primary tumor in stage IV disease could also be to reduce the number of circulating tumor cells (CTC) shed from the primary cancer.[9]
Table 1.
Question 1 - Will you proceed with mastectomy?
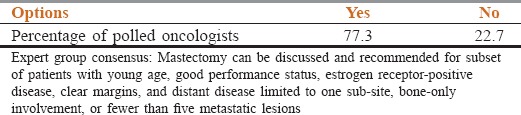
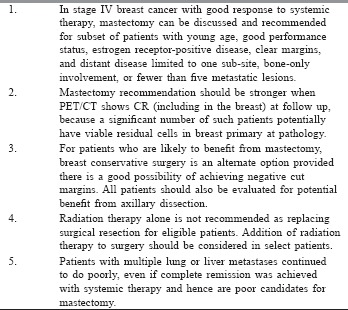
Taking these studies into consideration, the expert panel discussed about the benefits of local surgery on the overall survival of the patient. Newer anti her2 treatments like a combination of pertuzumab, trastuzumab and docetaxel have improved the survival in metastatic setting[10,11] and surgery might further increase the overall survival. Some animal studies have shown that leaving the tumor in situ may increase metastasis by resistant clones. The experts added that having a local surgery has also shown to improve the quality of life and avoids local complications due to progression. The expert group recommended that mastectomy can be recommended and discussed for patients who have the most favorable chance of improved survival viz, subsets with young age, good performance status, estrogen receptor-positive disease, clear margins, and distant disease limited to one sub-site, bone-only involvement, or fewer than five metastatic lesions.[12]
Importance of Positron Emission Tomography Combined with Computed Tomography
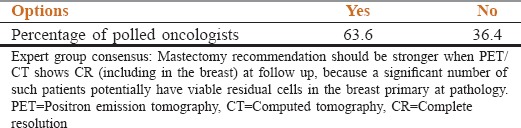
Positron emission tomography combined with computed tomography (PET/CT) has been receiving increasing attention during the recent years for making the diagnosis, for determining the staging and for the follow-up of various malignancies. The ability of PET to detect breast cancer is 92% for 2-5 cm tumors,[13] the size most commonly seen in India. When the baseline PET/CT has demonstrated primary and metastatic disease, it becomes a vital tool in assessing response at follow up. To the question regarding whether to proceed with mastectomy in patients with PET/CT Complete Response at metastatic sites as well as in the breast, the polled oncologists were fairly divided with 63.60% voting for and 36.40 voting against mastectomy for such patients [Table 2]. The expert group discussed about the evidence that PET/CT Complete Response does not always translate to pathological Complete Response. Expert group concluded that the recommendation for mastectomy should be even stronger when imaging CR is identified at follow up.
Table 2.
Question 2 - Will you proceed with mastectomy even if there is positron emission tomography/computed tomography complete resolution in the breast as well?
Breast Conservation Surgery
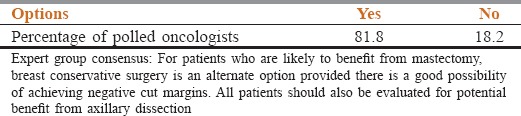
To the question whether Breast Conservation Surgery is a viable option for suitable stage IV breast cancer patients as compared to mastectomy, 82% of the polled oncologists gave an affirmative answer [Table 3]. The expert panel discussed existing published data. A meta-analysis showed that Breast Conservation Surgery (BCS) and Mastectomy had similar results in metastatic patients. The meta-analysis identified 10 studies (9 retrospective cohort studies, 1 retrospective case control study) including 28,693 patients with stage IV disease comparing the outcome between the groups undergoing surgery versus those with no surgery.[14,15,16] A total of 52.8% of the patients underwent excision of the primary carcinoma. Surgical excision of the primary tumor in the setting of stage IV breast cancer was associated with a superior survival at 3 years [40% (surgery) versus 22% (no surgery)] and upon comparing the type of surgical procedures, no difference in outcome could be found between breast-conserving therapy and mastectomy. The expert group therefore recommended that BCS was also feasible in patients with stage IV disease provided adequate surgical margins can be achieved. Surgery with negative margins seems to improve survival compared to positive margins or no surgery.[14] The expert group added that addressing the Axilla was also important based on the study by Rapiti et al.[17] in 2006 that suggests a trend toward a larger benefit for women who had both negative surgical margins and axillary dissection.
Table 3.
Question 3 - Is breast conserving surgery an option?
Radiation Therapy
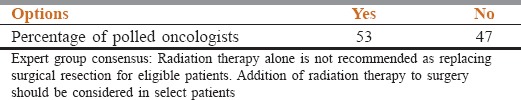
To the question about considering radiation therapy in the breast for residual disease rather than surgery, the polled answers are shown in Table 4. The polled oncologists were almost equally divided in their answers. Whereas 53% preferred Radiation Therapy, 47% were supporting surgery. In a retrospective study by Bourgier et al.,[18] the survival of patients receiving radiation alone was compared with that of patients undergoing surgery of the primary tumor and also receiving radiotherapy. The 3-year metastasis progression-free survival was 20% and 39% respectively and 3-year OS rates were 39% and 57% respectively, however no significant differences were found when adjusted to prognostic factors. Taking these studies into consideration, the expert group was of the opinion that it was best to use Radiation Therapy along with surgery in stage IV breast cancer patients. The expert consensus was that standard treatment guidelines for post operative Radiation Therapy used for non metastatic disease may also be applied in metastatic settings for the select subset mentioned in Table 1.
Table 4.
Question 4 - Will you consider radiation in the breast for residual disease rather than surgery?
An additional question posed by the moderators was whether mastectomy would be recommended even when the patient had liver or lung (visceral) metastasis. Favourable rates of survival were observed in patients who had distant disease at only one sub-site and not multi-organ metastases. A multivariate analysis showed overall survival to be influenced by the number of metastases.[1] The expert group opinion was that the patients with multiple lung or liver metastases continued to do poorly, even if Complete Remission was achieved with systemic therapy. Hence such patients are not good candidates for resection of the primary, usually having short disease free interval. The expert group reiterated that in all patients, careful discussion and counseling are helpful.
Timing of Surgery
Even though there are no studies comparing timing of surgery, sandwich therapy over sequential therapy, it's a broad consensus that, surgery timing is at the end of completion of systemic therapy. Which subserves two aspects: (a) If option of Breast conservation is considered, its chances are best after maximum response at the completion of entire systemic therapy and (b) Response verses progression in other sites is known.
Conclusions
The Update in Oncology-2017 expert group for mastectomy in metastatic breast cancer had the specific aim to develop practical consensus recommendations for easy application by the community oncologists.[19] It took into consideration data as well as the current practices in India, in addition to international data that conventional panels look at. The group also took into consideration the opinion of the participating oncologists with the help of polls.
The expert consensus that was reached was that surgery for primary tumor should be done in patients with oligometastatic breast cancer with good response to chemotherapy in an appropriately selected subgroup of patients- young, hormone positive and good response to systemic treatment. Surgery should be considered in even those patients who have a complete radiological response at the primary site. Regarding Breast conservation surgery, the expert group thought that it may also be feasible, provided adequate surgical margins can be achieved. Post-operative radiation therapy protocol can be followed but the use of radiation therapy as the sole way of treatment was not recommended by the expert group. Surgery in the patients with stage IV breast cancer may be a means of at least improving the quality of life along with the added benefit of avoiding local complications due to progression. Even if surgery is being seen as the way to go, discussion with the patient is of prime importance and the patient has to be counselled properly. Once data from trials such as Eastern Cooperative Oncology Group (ECOG) E2108 becomes available (overall survival as well as quality of life; NCT01242800) we will revisit and modify these practical consensus recommendations if necessary.
Unresolved issues of importance include the need for adjuvant radiotherapy and the timing of the surgery in relation to adjuvant and neo-adjuvant therapies.
Take Home Message
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Babiera GV, Rao R, Feng L, Meric-Bernstam F, Kuerer HM, Singletary SE, et al. Effect of primary tumor extirpation in breast cancer patients who present with stage IV disease and an intact primary tumor. Ann Surg Oncol. 2006;13:776–82. doi: 10.1245/ASO.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 2.Badwe R, Hawaldar R, Nair N, Kaushik R, Parmar V, Siddique S, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: An open-label randomised controlled trial. Lancet Oncol. 2015;16:1380–8. doi: 10.1016/S1470-2045(15)00135-7. [DOI] [PubMed] [Google Scholar]
- 3.Soran A, Ozmen V, Ozbas S. A randomized controlled trial evaluating resection of the primary breast tumor in women presenting with de novo stage IV breast cancer: Turkish Study (Protocol MF07-01) 2016 ASCO Annual Meeting. Abstract 1005. 2016 Jun 04; [Google Scholar]
- 4.Soran A, Ozmen V, Ozbas S, Karanlik H, Muslumanoglu M, Igci A, et al. Abstract S2-03: Early follow up of a randomized trial evaluating resection of the primary breast tumor in women presenting with de novo stage IV breast cancer; Turkish study (protocol MF07-01) Cancer Res. 73:S2–03. [Google Scholar]
- 5.Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, McGrath PC, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med. 2001;345:1655–9. doi: 10.1056/NEJMoa003013. [DOI] [PubMed] [Google Scholar]
- 6.Mickisch GH, Garin A, van Poppel H, de Prijck L, Sylvester R, European Organisation for Research and Treatment of Cancer (EORTC) Genitourinary Group et al. Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: A randomised trial. Lancet. 2001;358:966–70. doi: 10.1016/s0140-6736(01)06103-7. [DOI] [PubMed] [Google Scholar]
- 7.Khan SA. Primary tumor resection in stage IV breast cancer: Consistent benefit, or consistent bias? Ann Surg Oncol. 2007;14:3285–7. doi: 10.1245/s10434-007-9547-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanchard DK, Shetty PB, Hilsenbeck SG, Elledge RM. Association of surgery with improved survival in stage IV breast cancer patients. Ann Surg. 2008;247:732–8. doi: 10.1097/SLA.0b013e3181656d32. [DOI] [PubMed] [Google Scholar]
- 9.Budd GT, Cristofanilli M, Ellis MJ, Stopeck A, Borden E, Miller MC, et al. Circulating tumor cells versus imaging – predicting overall survival in metastatic breast cancer. Clin Cancer Res. 2006;12:6403–9. doi: 10.1158/1078-0432.CCR-05-1769. [DOI] [PubMed] [Google Scholar]
- 10.Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724–34. doi: 10.1056/NEJMoa1413513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baselga J, Cortés J, Kim SB, Im SA, Hegg R, Im YH, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366:109–19. doi: 10.1056/NEJMoa1113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen DH, Truong PT, Alexander C, Walter CV, Hayashi E, Christie J, et al. Can locoregional treatment of the primary tumor improve outcomes for women with stage IV breast cancer at diagnosis? Int J Radiat Oncol Biol Phys. 2012;84:39–45. doi: 10.1016/j.ijrobp.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 13.Avril N, Rosé CA, Schelling M, Dose J, Kuhn W, Bense S, et al. Breast imaging with positron emission tomography and fluorine-18 fluorodeoxyglucose: Use and limitations. J Clin Oncol. 2000;18:3495–502. doi: 10.1200/JCO.2000.18.20.3495. [DOI] [PubMed] [Google Scholar]
- 14.Harris E, Barry M, Kell MR. Meta-analysis to determine if surgical resection of the primary tumour in the setting of stage IV breast cancer impacts on survival. Ann Surg Oncol. 2013;20:2828–34. doi: 10.1245/s10434-013-2998-2. [DOI] [PubMed] [Google Scholar]
- 15.Hartmann S, Reimer T, Gerber B, Stachs A. Primary metastatic breast cancer: The impact of locoregional therapy. Breast Care (Basel) 2014;9:23–8. doi: 10.1159/000360054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruiterkamp J, Ernst MF, van de Poll-Franse LV, Bosscha K, Tjan-Heijnen VC, Voogd AC, et al. Surgical resection of the primary tumour is associated with improved survival in patients with distant metastatic breast cancer at diagnosis. Eur J Surg Oncol. 2009;35:1146–51. doi: 10.1016/j.ejso.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Rapiti E, Verkooijen HM, Vlastos G, Fioretta G, Neyroud-Caspar I, Sappino AP, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006;24:2743–9. doi: 10.1200/JCO.2005.04.2226. [DOI] [PubMed] [Google Scholar]
- 18.Bourgier C, Khodari W, Vataire AL, Pessoa EL, Dunant A, Delaloge S, et al. Breast radiotherapy as part of loco-regional treatments in stage IV breast cancer patients with oligometastatic disease. Radiother Oncol. 2010;96:199–203. doi: 10.1016/j.radonc.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 19.Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, Fan L, Li J, Chavarri-Guerra Y, et al. Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489–538. doi: 10.1016/S1470-2045(14)70029-4. [DOI] [PubMed] [Google Scholar]


