Abstract
Paget's disease of the breast is a rare type of cancer of the nipple–areola complex and that is often associated with an underlying in situ or invasive carcinoma. Diagnosis and treatment of Paget's disease is controversial. Expert oncologists discuss on the update on the approaches of Paget's disease diagnosis and its treatment options. This expert group used data from published literature, practical experience and opinion of a large group of academic oncologists to arrive at this practical consensus recommendations for the benefit of community oncologists.
Keywords: Biomarkers, magnetic resonance mammography, radiation therapy, SLNB, wedge biopsy, wide local excision
Introduction
Paget's disease is a rare form of breast neoplasm that is associated with approximately 3% of all breast cancers.[1] It is much more frequently found in females than males, though it can be found in men, with some series suggesting worse prognosis in men.[2] In 1856 Velpeau described the eczematous lesions of Paget's disease,[3] but Sir James Paget first described the association with underlying breast cancer in 1874.[4] In his paper, Paget described 15 women between 40 to 60 years old, who first presented with the skin changes involving nipple-areolar complex, and subsequently progressed to development of breast cancer. He noted that all fifteen patients initially presented with an itching eczema-like rash and discharge from the nipple, which were refractory to common remedies, and within the following year progressed to cancer.
The vast majority of patients diagnosed with Paget's disease have an associated underlying neoplasm in the breast. In several series, the percentage of patients diagnosed with Paget's disease of the nipple found to have invasive or non-invasive carcinoma is upwards of 90%.[1,5,6,7,8] Up to 50% of the patients with Paget's disease present with a palpable mass in their breast.[1,6]
On the microscopic level, Paget's disease is characterized by epidermal invasion by malignant glandular cells, which are large, foamy cells that may contain mucin.[9,10] These cells when stained with hematoxylin and eosin have pale cytoplasm and hyperchromatic nuclei.[11] In more advanced disease keratinocytes with atypia and epidermal hyperplasia are not uncommon. Some cells might also contain melanin in their cytoplasm.[12]
Expert group of oncologist meet in the update in oncology-X-2017 to discuss on recent updates in diagnosis tools and treatment option for Paget's disease in Breast cancer.
The update in oncology-X-2017 was organized by Sir Ganga Ram Hospital group met to discuss and arrive at a consensus statement to provide community oncologists practical guidelines for challenging common case scenarios in Breast Cancer out of these we are discus about Paget's disease in Breast cancer in this chapter. While the discussions will take the scenario as exists in India as a representative country with limited resources, the final manuscript is applicable globally.[13,14] The discussion was based on domain expertise of the National as well as international faculty, published evidence and practical experience in real life management of breast cancer patients. Opinion of the 250 oncologist including medical oncologist, radiation oncologist, surgical oncologist, molecular oncologist and radiologist are present in the update in oncology-X-2017 was taken into consideration by the expert panel. The expert group was chaired by Dr. Vijay Arora whereas the discussions were moderated by Dr. Gaurav Agarwal.
The core expert group consists Dr. Vivek Gupta, Dr. Rakesh Koul, Dr. S. Dabas, Dr. Ramesh Sareen, and Dr. K Geeta. Consensus answers were used as the basis of formulating the consensus statement providing community oncologists with ready-to-use practical recommendations. The survey answers were used as the basis for formulating the consensus statement so that community oncologists have a ready-to-use Paget's disease in Breast cancer.
As part of the background work, the best existing evidence was compiled and provided to the expert group panel members for review in preparation of the expert group meeting.[15,16,17] The national and international experts invited to this meeting were also provided the data on the voting by the audience delegates from the update in oncology-X-2017. Members of the panel were also allowed to share their ersonal experiences, make comments and record dissent while voting for the consensus statements. Total of Six broad question categories were part of the expert group discussions [Tables 1–9].
Table 1.
Question categories addressed by the update in oncology-X-2017
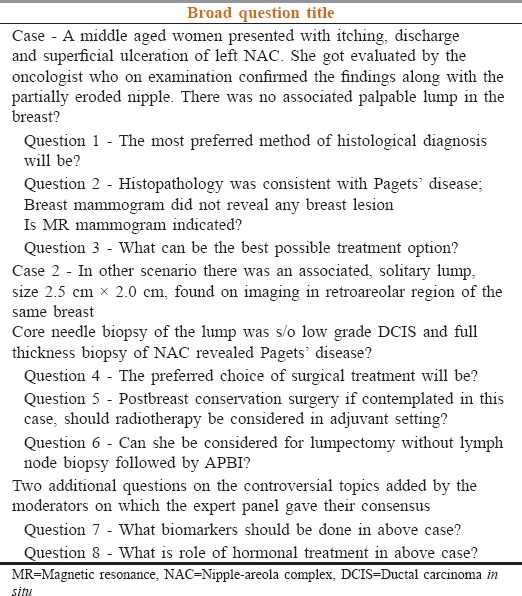
Table 9.
Role of hormonal treatment in above case?
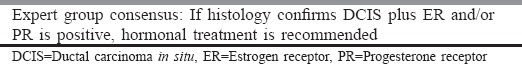
Table 2.
Question 1 - The most preferred method of histological diagnosis will be?
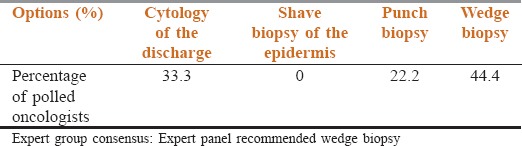
Table 3.
Question 2 - Histopathology was consistent with Pagets’ disease; breast mammogram did not reveal any breast lesion. Is magnetic resonance mammogram indicated?
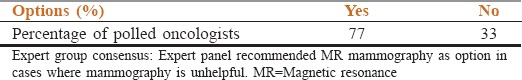
Table 4.
Question 3 - What can be the best possible treatment option?
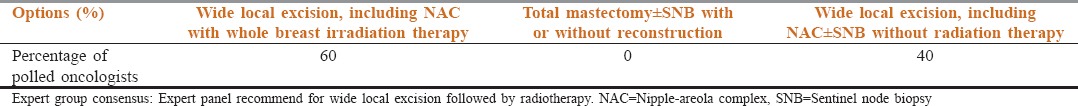
Table 5.
Question 4 - The preferred choice of surgical treatment will be?
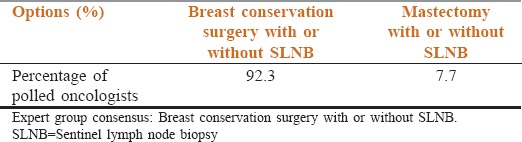
Table 6.
Question 5 - Postbreast conservation surgery if contemplated in this case, should radiotherapy be considered in adjuvant setting?
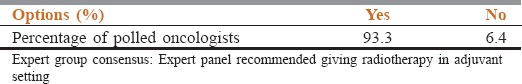
Table 7.
Question 6 - Can she be considered for lumpectomy without lymph node biopsy followed by APBI?
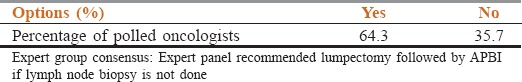
Table 8.
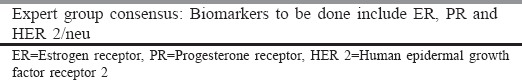
Question 7 - What biomarkers should be done in above case?
Clinical Features
The clinical appearance of the Paget's disease is usually a thickened, sometimes pigmented, eczematoid, erythematous weeping or crusted lesion with irregular borders. The surface of the lesion is occasionally slightly infiltrated. Complaints of pain or itching are frequent. The nipple may be retracted or deformed. Early changes including scaling and redness may be mistaken for eczema or some other inflammatory conditions.[18,19] The inflammatory component may be improved by topical treatment, a result that masks the underlying condition and this may cause delay in diagnosis.[18] These stages of the Paget's disease may result in ulceration, destruction of the nipple–areola complex[9] and bloody discharge. The lesions are almost unilateral and very rarely bilateral.[20] Paget's disease may also develop on ectopic breasts[21] and accessory nipples.[22] No clinical and epidemiologic factors are known to predispose patients to develop Paget's disease.
Diagnosis
The diagnosis of Paget's disease can be made from a wedge biopsy, a superficial “shave” biopsy of epidermis or punch biopsy. The wedge biopsy is the most useful method to make the diagnosis because the epidermis can adequately represent and the biopsy is likely to include a part of lactiferous duct. The shave biopsy is less likely to contain sufficient number of Paget's cells, especially when the surface of the lesion is ulcerated. Although a punch biopsy will include the underlying stroma and possibly part of a duct, there is frequently little epidermis to examine. None of these procedures are always successful; therefore, it is sometimes necessary to take a second biopsy or excise the nipple.[19] When a patient has nipple–areola skin changes, a full thickness biopsy of the nipple and areola is important to establish the diagnosis. The use of immunohistochemical stainings, such as carcinoembryonic antigen (CEA), mucin or Her-2 oncoprotein, has been suggested to enhance the diagnosis;[23] however, a negative result does not exclude a diagnosis of Paget's disease of the breast, and therefore open (surgical) biopsy should be considered as standard for the diagnosis of Paget's disease of the breast.
The diagnosis of Paget's disease is generally made on the basis of clinical findings. However, when the signs are evident and Paget's disease is suspected, imaging should be performed to detect the underlying carcinoma. Radiologic findings are important to assess appropriate further management and the treatment of the disease. Conventional imaging modalities such as mammography (MMG) may depict a mass or calcification representative of invasive cancer or DCIS, respectively. However, MMG is not always a reliable procedure for detecting MPD. It is limited in its depiction of underlying DCIS in women with Paget's disease.[24]
Magnetic resonance imaging (MRI) is known to be highly sensitive for the detection of breast cancer, especially in patients whose mammographic or USG findings are normal or the extent of disease is uncertain.[25,26] MRI may show abnormal nipple enhancement, thickening of the nipple–areola complex, an associated enhancing DCIS or invasive tumor, or a combination of these, even when clinically unsuspected.[27,28]
Because mammography have limitations in the evaluation of patients with Paget's disease, in the setting of clinically and mammographically occult disease, additional evaluation with MRI can help detect underlying invasive cancer and DCIS. Additionally, MRI may have a role in the preoperative evaluation of the patient and might facilitate appropriate further treatment decisions. In fact, if the diagnosis is based solely on radiologic findings without careful clinical examination, it may result in a delay in diagnosis. As a result, both clinical and imaging findings are complementary and should be correlated to confirm or exclude a diagnosis of Paget's disease.
Pathogenesis of Paget's Disease
Two theories have been proposed in regards to pathogenesis of Paget's disease: (I) epidermotropic theory and (II) in situ malignant transformation theory. The first theory claims that changes typical for Paget's disease arise in the ductal cells, and spread along the basement membrane to the nipple.[29] This theory is supported by the fact that most patients with Paget's have underlying breast cancer, and the cells from the nipple are histologically similar to the associated invasive carcinoma.[30] The in situ malignant transformation theory claim holds that Paget's disease originates in the epidermal cells of the nipple by malignant transformation of keratinocytes and is not associated with any coexisting neoplastic process in the affected breast.[8,31]
Treatment
The surgical treatment of Paget's disease is controversial. Mastectomy with or without axillary lymph node dissection has long been regarded as the standard therapy for Paget's disease, even in the absence of other clinical signs of malignancy.[31] The underlying mass is often invasive cancer with a high risk of axillary node metastases. The patients have a poorer prognosis and usually the appropriate therapy is based on the pathologic findings of the mass and axillary staging.[32] In the literature, almost all patients treated with local excision, radiotherapy, or both had the clinical presentation of Paget's disease without a palpable mass. Dixon et al. reported a high recurrence rate of 40% in patients treated with local excision alone, whose mammograms suggested in situ changes confined to the nipple area.[33] Polgár et al. reported a local recurrence rate of 33% with a median follow-up time of 6 years in 33 patients treated with local excision alone with or without underlying ductal carcinoma in situ confined to the nipple–areola complex.[34] They concluded that the local excision alone was not an appropriate treatment for patients with Paget's disease of the nipple.
With the increasing diagnosis of the early breast cancers and the findings from multiple randomized, prospective trials demonstrating that breast conserving therapy is a feasible alternative for patients with disease limited to the central segment of the breast,[35,36] the reported techniques for conservative management of Paget's disease vary widely. These include nipple excision alone (partial or complete), central segmentectomy alone, these resections plus radiation and radiation without resection.[33,37,38] Recent reports from several studies with long-term follow-up have shown that breast-conserving surgery is equivalent to mastectomy in terms of overall and disease-free survival in patients with breast cancer.[39,40,41] If conservative therapy is adopted, the patient should be followed up carefully with regular mammography.[42] Mastectomy should be reserved for the few occasions, when relapse occurs.[38]
Use of breast radiation therapy alone for the Paget's disease of the breast has been reported in limited numbers and with varying results.[37,38,43] Current studies suggest that irradiation of the breast tissue to a radical dose may be effective against DCIS.[44] This gives support to the view that selected patients with Paget's disease of the breast can be treated by radiotherapy as an alternative to radical surgery in selected patients with Paget's disease confined to the nipple, without clinical or radiological detectable breast tumor.[43]
Conclusion
Paget's disease of the breast is a relatively uncommon condition affecting the nipple and the surrounding tissue. Almost universally, it is associated with DCIS or invasive cancer in the ipsilateral breast. Because these underlying malignancies tend to be multifocal and multicentric, mammography often is not sufficient and MRI may be necessary to evaluate the true extent of the disease. Both total mastectomy and breast preserving surgery followed by appropriate adjuvant therapy are acceptable treatment options for carefully selected patients with Paget's disease. The output of this discussion is to provide the best and effective method of diagnosis of disease and provide best treatment options for patients with Paget's disease of the breast cancer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ashikari R, Park K, Huvos AG, Urban JA. Paget's disease of the breast. Cancer. 1970;26:680–5. doi: 10.1002/1097-0142(197009)26:3<680::aid-cncr2820260329>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 2.Desai DC, Brennan EJ, Jr, Carp NZ. Paget's disease of the male breast. Am Surg. 1996;62:1068–72. [PubMed] [Google Scholar]
- 3.Velpeau A, editor. On Disease of the Mammary Areola Preceding Cancer of the Mammary Region. London: Sydenham Society; 1856. [Google Scholar]
- 4.Paget J. On disease of the mammary areola preceding cancer of the mammary gland. St Barts Hospital Rep. 1874;10:87–9. [Google Scholar]
- 5.Dominici LS, Lester S, Liao GS, Guo L, Specht M, Smith BL, et al. Current surgical approach to Paget's disease. Am J Surg. 2012;204:18–22. doi: 10.1016/j.amjsurg.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Chaudary MA, Millis RR, Lane EB, Miller NA. Paget's disease of the nipple: A ten year review including clinical, pathological, and immunohistochemical findings. Breast Cancer Res Treat. 1986;8:139–46. doi: 10.1007/BF01807702. [DOI] [PubMed] [Google Scholar]
- 7.Caliskan M, Gatti G, Sosnovskikh I, Rotmensz N, Botteri E, Musmeci S, et al. Paget's disease of the breast: The experience of the European institute of oncology and review of the literature. Breast Cancer Res Treat. 2008;112:513–21. doi: 10.1007/s10549-007-9880-5. [DOI] [PubMed] [Google Scholar]
- 8.Yim JH, Wick MR, Philpott GW, Norton JA, Doherty GM. Underlying pathology in mammary Paget's disease. Ann Surg Oncol. 1997;4:287–92. doi: 10.1007/BF02303576. [DOI] [PubMed] [Google Scholar]
- 9.Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol. 2007;21:581–90. doi: 10.1111/j.1468-3083.2007.02154.x. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd J, Flanagan AM. Mammary and extramammary Paget's disease. J Clin Pathol. 2000;53:742–9. doi: 10.1136/jcp.53.10.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalberg K, Hellborg H, Wärnberg F. Paget's disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111:313–9. doi: 10.1007/s10549-007-9783-5. [DOI] [PubMed] [Google Scholar]
- 12.Karakas C. Paget's disease of the breast. J Carcinog. 2011;10:31. doi: 10.4103/1477-3163.90676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Cancer Registry Programme. In: Consolidated Report of Population Based Cancer Registries 20012004, Incidence and Distribution of Cancer. Bangalore: Coordinating Unit, National Cancer Registry Programme (ICMR); 2006. Indian Council of Medical Research. Leading sites of cancer; pp. 8–30. [Google Scholar]
- 14.Badwe RA, Gangawal S, Mittra I, Desai PB. Clinico-pathological features and prognosis of breast cancer in different religious communities in India. Indian J Cancer. 1990;27:220–8. [PubMed] [Google Scholar]
- 15.Altekruse SF, Kosary CL, Krapcho M. SEER Cancer Statistics Review. National Cancer Institute. 19752007. [Google Scholar]
- 16.National Cancer Registry Program. New Delhi: Indian Council of Medical Research; 2001. Ten Year Consolidated Report of the Hospital Based Cancer Registries, 1984–1993, An Assessment of the Burden and Care of Cancer Patients. [Google Scholar]
- 17.Agarwal G, Pradeep PV, Aggarwal V, Yip CH, Cheung PS. Spectrum of breast cancer in Asian women. World J Surg. 2007;31:1031–40. doi: 10.1007/s00268-005-0585-9. [DOI] [PubMed] [Google Scholar]
- 18.Sakorafas GH, Blanchard K, Sarr MG, Farley DR. Paget's disease of the breast. Cancer Treat Rev. 2001;27:9–18. doi: 10.1053/ctrv.2000.0203. [DOI] [PubMed] [Google Scholar]
- 19.Rosen PP. Rosen's Breast Pathology. 2nd ed. Philadelphia: Lippincott-Raven; 2001. Paget's disease of the nipple; pp. 565–80. [Google Scholar]
- 20.Franceschini G, Masetti R, D'Ugo D, Palumbo F, D'Alba P, Mulè A, et al. Synchronous bilateral Paget's disease of the nipple associated with bilateral breast carcinoma. Breast J. 2005;11:355–6. doi: 10.1111/j.1075-122X.2005.21722.x. [DOI] [PubMed] [Google Scholar]
- 21.Kao GF, Graham JH, Helwig EB. Paget's disease of the ectopic breast with an underlying intraductal carcinoma: Report of a case. J Cutan Pathol. 1986;13:59–66. doi: 10.1111/j.1600-0560.1986.tb00461.x. [DOI] [PubMed] [Google Scholar]
- 22.Martin VG, Pellettiere EV, Gress D, Miller AW. Paget's disease in an adolescent arising in a supernumerary nipple. J Cutan Pathol. 1994;21:283–6. doi: 10.1111/j.1600-0560.1994.tb00275.x. [DOI] [PubMed] [Google Scholar]
- 23.Stotter AT, McNeese M, Oswald MJ, Ames FC, Romsdahl MM. The role of limited surgery with irradiation in primary treatment of ductal in situ breast cancer. Int J Radiat Oncol Biol Phys. 1990;18:283–7. doi: 10.1016/0360-3016(90)90090-7. [DOI] [PubMed] [Google Scholar]
- 24.Ikeda DM, Helvie MA, Frank TS, Chapel KL, Andersson IT. Paget disease of the nipple: Radiologic-pathologic correlation. Radiology. 1993;189:89–94. doi: 10.1148/radiology.189.1.8396786. [DOI] [PubMed] [Google Scholar]
- 25.Günhan-Bilgen I, Oktay A. Paget's disease of the breast: Clinical, mammographic, sonographic and pathologic findings in 52 cases. Eur J Radiol. 2006;60:256–63. doi: 10.1016/j.ejrad.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Morrogh M, Morris EA, Liberman L, Borgen PI, King TA. The predictive value of ductography and magnetic resonance imaging in the management of nipple discharge. Ann Surg Oncol. 2007;14:3369–77. doi: 10.1245/s10434-007-9530-5. [DOI] [PubMed] [Google Scholar]
- 27.Amano G, Yajima M, Moroboshi Y, Kuriya Y, Ohuchi N. MRI accurately depicts underlying DCIS in a patient with Paget's disease of the breast without palpable mass and mammography findings. Jpn J Clin Oncol. 2005;35:149–53. doi: 10.1093/jjco/hyi044. [DOI] [PubMed] [Google Scholar]
- 28.Frei KA, Bonel HM, Pelte MF, Hylton NM, Kinkel K. Paget disease of the breast: Findings at magnetic resonance imaging and histopathologic correlation. Invest Radiol. 2005;40:363–7. doi: 10.1097/01.rli.0000163742.40401.4e. [DOI] [PubMed] [Google Scholar]
- 29.Muir R. The pathogenesis of Paget's disease of the nipple and associated lesions. Br J Surg. 1935;22:728–37. [Google Scholar]
- 30.Inglis K. Paget's disease of the nipple: With special reference to the changes in the ducts. Am J Pathol. 1946;22:1–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Paone JF, Baker RR. Pathogenesis and treatment of Paget's disease of the breast. Cancer. 1981;48:825–9. doi: 10.1002/1097-0142(19810801)48:3<825::aid-cncr2820480326>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 32.Kollmorgen DR, Varanasi JS, Edge SB, Carson WE., 3rd Paget's disease of the breast: A 33-year experience. J Am Coll Surg. 1998;187:171–7. doi: 10.1016/s1072-7515(98)00143-4. [DOI] [PubMed] [Google Scholar]
- 33.Dixon AR, Galea MH, Ellis IO, Elston CW, Blamey RW. Paget's disease of the nipple. Br J Surg. 1991;78:722–3. doi: 10.1002/bjs.1800780627. [DOI] [PubMed] [Google Scholar]
- 34.Polgár C, Orosz Z, Kovács T, Fodor J. Breast-conserving therapy for Paget disease of the nipple: A prospective European Organization for Research and Treatment of Cancer Study of 61 patients. Cancer. 2002;94:1904–5. doi: 10.1002/cncr.10405. [DOI] [PubMed] [Google Scholar]
- 35.Kawase K, Dimaio DJ, Tucker SL, Buchholz TA, Ross MI, Feig BW, et al. Paget's disease of the breast: There is a role for breast-conserving therapy. Ann Surg Oncol. 2005;12:391–7. doi: 10.1245/ASO.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 36.Bijker N, Rutgers EJ, Duchateau L, Peterse JL, Julien JP, Cataliotti L, et al. Breast-conserving therapy for Paget disease of the nipple: A prospective European Organization for Research and Treatment of Cancer Study of 61 patients. Cancer. 2001;91:472–7. doi: 10.1002/1097-0142(20010201)91:3<472::aid-cncr1024>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 37.Bulens P, Vanuytsel L, Rijnders A, van der Schueren E. Breast conserving treatment of Paget's disease. Radiother Oncol. 1990;17:305–9. doi: 10.1016/0167-8140(90)90004-g. [DOI] [PubMed] [Google Scholar]
- 38.Stockdale AD, Brierley JD, White WF, Folkes A, Rostom AY. Radiotherapy for Paget's disease of the nipple: A conservative alternative. Lancet. 1989;2:664–6. doi: 10.1016/s0140-6736(89)90904-5. [DOI] [PubMed] [Google Scholar]
- 39.van Dongen JA, Voogd AC, Fentiman IS, Legrand C, Sylvester RJ, Tong D, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92:1143–50. doi: 10.1093/jnci/92.14.1143. [DOI] [PubMed] [Google Scholar]
- 40.Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 41.Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 42.el-Sharkawi A, Waters JS. The place for conservative treatment in the management of Paget's disease of the nipple. Eur J Surg Oncol. 1992;18:301–3. [PubMed] [Google Scholar]
- 43.Fourquet A, Campana F, Vielh P, Schlienger P, Jullien D, Vilcoq JR, et al. Paget's disease of the nipple without detectable breast tumor: Conservative management with radiation therapy. Int J Radiat Oncol Biol Phys. 1987;13:1463–5. doi: 10.1016/0360-3016(87)90311-7. [DOI] [PubMed] [Google Scholar]
- 44.Stotter AT, McNeese M, Oswald MJ, Ames FC, Romsdahl MM. The role of limited surgery with irradiation in primary treatment of ductal in situ breast cancer. Int J Radiat Oncol Biol Phys. 1990;18:283–7. doi: 10.1016/0360-3016(90)90090-7. [DOI] [PubMed] [Google Scholar]


