Introduction
Lichen planus (LP) is a common inflammatory dermatosis, which involves the skin, mucosa, and nails. The clinical presentation is highly variable with over 20 distinct morphologic forms described.1 Annular LP, which presents with circinate lesions with elevated borders, is a rare form of LP, comprising 7%-10% of LP cases.2 Annular LP has been reported in association with Sneddon syndrome, Crohn disease, and HIV infection.2, 3 Drug-induced annular LP has not been described. Here, we report the first case of efavirenz-induced giant annular LP in a patient with HIV.
Case report
A 40-year-old black man presented to the dermatology clinic at King Edward Hospital (Durban, South Africa) with an 18-month history of widespread pruritic annular plaques. He was diagnosed with HIV infection 22 months before presentation with a CD4 count of 8 cells/mm3 and viral load of 16,000 copies/mL. He was started on first-line antiretroviral (ARV) therapy with stavudine, lamivudine, and efavirenz as well as Pneumocystis jirovecii and Toxoplasma gondii prophylaxis with trimethoprim-sulfamethoxazole (TMP-SMX). Four months after initiation of drug therapy, he developed mildly pruritic large circinate plaques with raised erythematous scaly borders and hyperpigmented wood-grain centers involving the trunk, extremities, buttocks, and scrotum (Figs 1 and 2). The lesions started as small erythematous to violaceous plaques and spread outwards to attain an annular configuration, ranging from 2-30 cm in width. He had no mucosal, nail, or scalp involvement. He appeared well and denied fevers, chills, night sweats, weight loss, cough, or shortness of breath. He reported daily adherence to stavudine, lamivudine, efavirenz, and TMP-SMX. He took no other prescribed medications, vitamins, herbal supplements, or homeopathic remedies.
Fig 1.

Giant annular lichen planus on trunk. The rash is not photo-distributed.
Fig 2.

Giant annular lichen planus on buttocks and lower extremities.
The patient was treated empirically for syphilis infection with benzathine penicillin G. Laboratory evaluation revealed that he was negative for rapid plasmin reagin, his CD4 count was 310 cells/mm3, and he had an undetectable viral load. A skin biopsy was performed that demonstrated lichenoid interface dermatitis with parakeratosis and dyskeratosis, a mononuclear perivascular infiltrate, and eosinophils consistent with a lichenoid hypersensitivity reaction (Fig 3).
Fig 3.
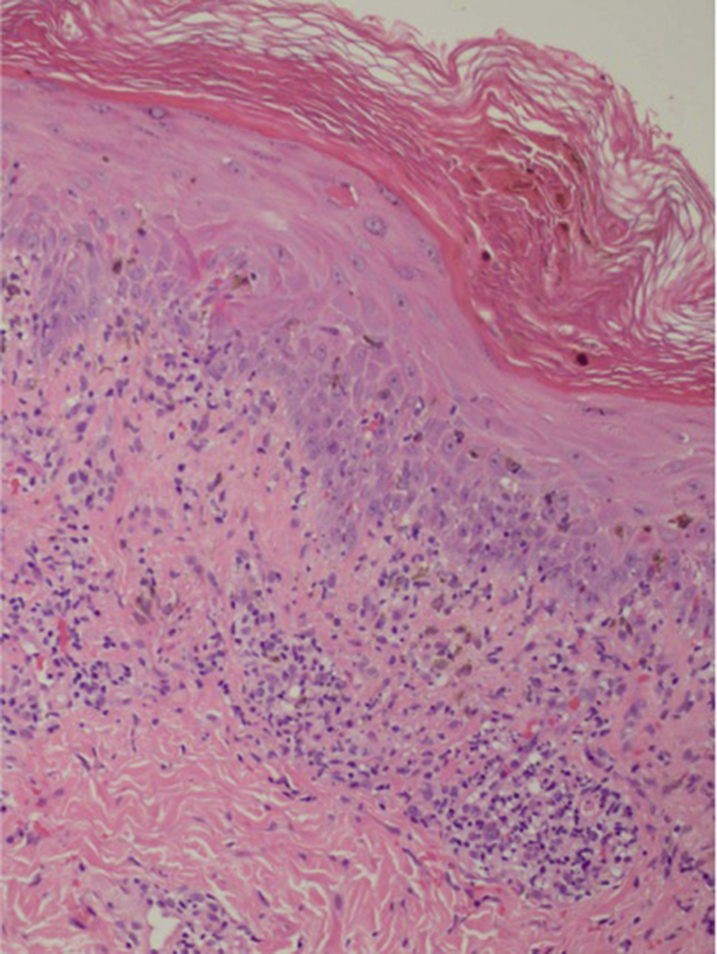
Hematoxylin-eosin stain of punch biopsy.
The patient started topical steroid therapy and subsequently stopped TMP-SMX for 3 months with no effect. ARV-induced hypersensitivity reaction was suspected; however, because of resource limitations for alternative ARV therapy, a treat-through approach was attempted. The patient was started on acitretin 30 mg/day for 3 months followed by prednisone 1 mg/kg for 6 weeks, neither of which resulted in clinical response. Ultimately, stavudine, lamivudine, and efavirenz were discontinued, and the patient had complete resolution of rash 2 weeks later (Fig 4). He was transitioned to stavudine, lamivudine, and lopinavir/ritonavir without recurrence of rash.
Fig 4.

Clinical improvement after 2 weeks of cessation of antiretroviral therapy.
Discussion
Annular LP is a rare variant of LP that presents as circinate lesions with elevated borders and central clearing. There are 2 proposed mechanisms by which the annular morphology is achieved; coalescing of lichenoid papules into a ring formation4 and central involution of a flat-topped plaque with advancing border.5 Annular LP most commonly presents with few localized lesions with distribution patterns that vary by ethnicity (eg, genitalia in black men, intertriginous sites in whites, and extremities in a Japanese cohort).2, 5, 6 Generalized annular LP, such as that seen in our patient, is rarely described, with one of the few other reported cases presenting in a patient at the time of HIV diagnosis.3
LP is an inflammatory dermatosis that can be either idiopathic or associated with exogenous antigens, such as hepatitis C virus, vaccines, contact allergens, and medications.7 Compared with idiopathic LP, drug-induced LP (lichenoid drug eruption) more commonly presents in photo-distributed areas, sparing the wrists and lower legs and rarely involves the mucosa.7 Eosinophils, parakeratosis, and deep involvement of the lymphocytic infiltrate are characteristic histologic findings of lichenoid drug eruption. However, histologic staining alone cannot be reliably used to distinguish between drug-induced and idiopathic LP.8 Our patient had many clinical and histologic features of drug-induced LP, including sparing of the distal extremities and mucosa as well as presence of eosinophils on pathology. He also scored highly on the Naranjo scale, demonstrating probable causality between efavirenz and the adverse cutaneous reaction.9 His morphologic presentation of generalized giant annular LP is the first described in relation to drug exposure.
HIV infection predisposes to a variety of inflammatory and infectious skin conditions, which often have severe or atypical presentations. Cutaneous adverse drug reactions (CADRs) include drug hypersensitivity syndrome, Stevens-Johnson syndrome, toxic epidermal necrolysis, lichenoid, and fixed drug eruptions and are particularly common in people with HIV infection because of altered drug metabolism due to slow acetylator status, dysregulated immune system, multidrug regimen therapy, and predisposing viral infection.10 Nonnucleoside reverse transcriptase inhibitors are a major cause of CADRs, with cutaneous reactions occurring in 10%-17% of patients.11 Efavirenz, a nonnucleoside reverse transcriptase inhibitor, tends to cause milder forms of CADRs compared with its counterpart nevirapine, with Stevens-Johnson syndrome/toxic epidermal necrolysis occurring in only 0.1% of patients. Although efavirenz-induced eruptions have been poorly defined, a series of 5 photo-distributed, annular erythematous eruptions have been reported with disparate histology results, including spongiotic, vesiculobullous, and perivascular patterns.11
CADRs are common in HIV-infected patients due to a combination of host immunologic factors, as well as the complexity of drug regimens in HIV. In caring for patients with HIV, clinical suspicion of CADRs must remain high because they can present atypically and with novel morphology. In cases of mild CADRs, a treat-through approach is an option in order to continue important systemic medications, particularly in low-resource settings with limited options for alternative therapy. However, our case necessitated cessation of therapy. Our patient represents the first reported case of efavirenz-induced lichenoid drug eruption, which presented as a rare form of generalized annular LP, and thus, efavirenz should be included in the list of drugs that can cause lichenoid eruption.
Acknowledgments
The authors would like to acknowledge Preetha Hariram, MBChB, MMed, FCDerm, and Mahendran Moodley, MBChB, FCDerm, for their efforts in the diagnostic workup and management of this case.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Boyd A., Neldner K. Lichen planus. J Am Acad Dermatol. 1991;25:593–619. doi: 10.1016/0190-9622(91)70241-s. [DOI] [PubMed] [Google Scholar]
- 2.Reich H., Nguyen J., James W. Annular lichen planus: a case series of 20 patients. J Am Acad Dermatol. 2004;50(4):595–599. doi: 10.1016/j.jaad.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Chakraborty S., Chowdhury J., De A., Gharami R. Generalized lichen planus with a unique morphology in a patient seropositive for HIV. JAAD Case Rep. 2015;1:251–253. doi: 10.1016/j.jdcr.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sutton R. The symptomatology and treatment of some variant forms of lichen planus. JAMA. 1914;62:175–183. [Google Scholar]
- 5.Matsunaga T., Tanino C. Case report of lichen planus annularis. Rinsha Dermo. 1990;32:1879–1883. [Google Scholar]
- 6.Popkin D., Greene R., Fung J. Widespread annular eruption in a black man-quiz case. Arch Dermatol. 2005;141(1):93–98. doi: 10.1001/archderm.141.1.93-a. [DOI] [PubMed] [Google Scholar]
- 7.Bolognia J., Jorizzo J., Schaffer J. Elsevier Saunders; Philadelphia, PA: 2012. Dermatology. [Google Scholar]
- 8.Van den Haute V., Antione J., Lachapelle J. Histopathological discriminant criteria between lichenoid drug eruptions and idiopathic lichen planus: retrospective study on selected samples. Dermatologica. 1989;179:10–13. doi: 10.1159/000248091. [DOI] [PubMed] [Google Scholar]
- 9.Naranjo C., Busto U., Sellers E. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 10.Yunihastuti E., Widhani A., Harjono Karjadi T. Drug hypersensitivity in human immunodeficiency virus-infected patient: challenging diagnosis and management. Asia Pac Allergy. 2014;4(1):54–67. doi: 10.5415/apallergy.2014.4.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Isaacs T., Ngwanya M., Dlamini S., Lehloeya R. Annular erythema and photosensitivity as a manifestation of efavirenz-induced cutaneous reactions: a review of five consecutive cases. J Antimicrob Chemother. 2013;68(12):2871–2874. doi: 10.1093/jac/dkt287. [DOI] [PMC free article] [PubMed] [Google Scholar]


