Introduction
The first description of this condition in 1948 was followed by 17 case reports before Happle delineated the key features and proposed the acronym CHILD syndrome in 1980, which stands for congenital hemidysplasia, ichthyosiform nevus, and limb defects. It is a rare X-linked dominant disorder that is generally lethal in affected male embryos.1
CHILD syndrome is caused by a defect in cholesterol synthesis as a result of mutation in the NSDHL (NAD[P] sterol dehydrogenase–like) gene. This mutation prevents the postlanosterol generation of cholesterol, potentially leading to pathway-product deficiency in addition to metabolite accumulation.2, 3
The characteristic skin changes are unilateral, waxy, scaling, ichthyosiform erythematous plaques with a sharp midline demarcation present at birth or shortly thereafter. The most frequently affected areas are the vulva, axillae, and gluteal folds.4, 5
Treatment until recently has been purely symptomatic using emollients and retinoids to reduce scaling. New therapeutic approaches recently have been developed based on the pathogenesis.6, 7 These studies suggest that topical application of cholesterol in combination with a cholesterol synthesis–inhibiting agent (statin) has the potential to reverse skin symptoms in CHILD syndrome by providing functional cholesterol while inhibiting the accumulation of toxic metabolites.3, 6, 7
We describe a rare case of CHILD syndrome presenting with a rapid onset of skin abnormalities after birth, which was treated successfully with topical 2% simvastatin ointment monotherapy.
Case report
A 1-month-old girl, the first child of a nonconsanguineous marriage, presented with a deformity of the right lower limb and a missing right upper limb, along with redness and scaling over the same side of the body since birth. The delivery was normal, and the child did not show any signs suggestive of systemic involvement. Her birth weight was 2.5 kg. The mother had no history of miscarriage, and there is no family history of same condition.
Cutaneous changes were noted shortly after birth. Cutaneous examination found a strikingly unilateral erythematous dermatosis present over the right shoulder, axilla, and right side of the trunk to the midline anteriorly and posteriorly (Fig 1). Involvement extended to the right leg and was confluent in all areas. The border between the involved and uninvolved skin could be ascertained by palpation. The involved skin was covered with large, thin, yellow-to-brown scales, free at the center, and attached primarily at their edges. The scales did not fall off the skin spontaneously but could be dislodged without any difficulty by an examining finger. Removal of scales did not cause any bleeding. The involved skin was dry and felt somewhat rough to touch. There was no tenderness or sensation of increased or decreased temperature in these areas. Mucosal involvement was absent.
Fig 1.
Cutaneous abnormalities of CHILD syndrome before treatment. A, Ipsilateral ichthyosiform plaques over right pectoralis region, axillae, and shoulder with a sharp midline demarcation and ptychotropism. Note missing right upper limb. B, CHILD nevus following Blaschko lines.
Laboratory investigations found mild anemia. All other testing levels were within normal limits. Further investigations did not find any involvement of other organs, such as the eyes, brain, heart, lungs, or kidneys.
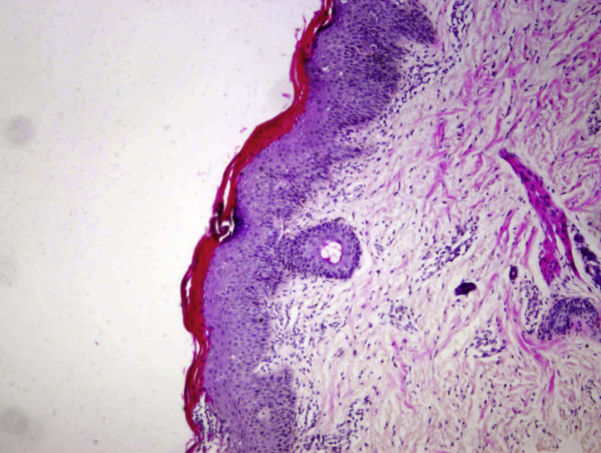
Histologic examination found marked hyperkeratosis and parakeratosis, a reduced to absent stratum granulosum, and a moderate amount of acanthosis of the epidermis (Fig 2).
Fig 2.
Histopathologic examination (hematoxylin-eosin stain) shows psoriasiform dermatitis with acanthosis, zones of parakeratosis, and an exocytosis of neutrophils.
The diagnosis of CHILD syndrome was made based on the clinical, radiologic, and histologic findings. The patient was referred to a pediatric genetic clinic for further evaluation. Genetic analysis revealed a missense mutation of exon 8 of the NSDHL gene, verifying the diagnosis of CHILD syndrome.
After obtaining informed consent from her father, we began treatment with twice-daily topical simvastatin 2% ointment (an ointment was prepared by our pharmacy laboratory by mixing a commercially available 20-mg tablets of simvastatin with ointment base to make a final volume of 2 g simvastatin in 98 g ointment base).
Decreased inflammation, skin thickening, and scaling were noted as early as 3 weeks. By 6 weeks, the treated skin largely and dramatically normalized with a discrete postinflammatory hypopigmentation remaining (Fig 3). Thereafter, the dose decreased to once to twice weekly. No reoccurrence was observed after 10 months of maintenance topical treatment (Fig 3).
Fig 3.
Cutaneous abnormalities of CHILD syndrome after treatment. A, Dramatically responded to topical application of simvastatin with only postinflammatory hypopigmentation after 6 weeks. B, Showing sustained improvement after 10 months of maintenance treatment.
Discussion
Inherited ichthyosiform dermatoses can be provoked by deficiency in intermediate pathway metabolites such as cholesterol, ceramides, and free fatty acids or accumulation of toxic pathway metabolites in syndromic lipid metabolic disorders.3
Cholesterol, 1 of 3 important stratum corneum lipids, is needed to form the normal extracellular lamellar bilayer system that mediates barrier function.8 Lack of cholesterol in cell membranes and the accumulation of toxic sterol precursors disturb the keratinization process.9
Current treatment of the ichthyoses remains symptomatic and largely directed toward reducing the scaling component. This approach often is ineffective, may be accompanied by toxicity (eg, with systemic retinoids), and is intuitively counterproductive because the hyperkeratosis and hyperplasia likely reflect an epidermal homeostatic response to re-establishing a competent barrier.6
Topical application of a lovastatin-cholesterol lotion (but not cholesterol alone) recently was shown to be an effective treatment for the CHILD nevus.3, 7 Similarly, ketoconazole, which influences cholesterol biosynthesis via CYP51 inhibition, has been shown to improve CHILD lesions.10 Encouraged by the previously reported pathogenesis-based therapy,3, 6, 7 we attempted topical simvastatin (cholesterol-synthesis inhibiting agent) monotherapy.
In one study,3 there was no clinical improvement after 3 months of treatment with twice-daily topical 10% cholesterol ointment, but the case reported here confirms a remarkable improvement of the skin lesions in response to treatment with simvastatin 2% ointment. Marked improvement was seen after 1 to 2 weeks. Furthermore, in the case presented here, the patient experienced a reduction of the application frequency from daily to weekly after 6 weeks without negative effects. Sustained improvement was seen after 10 months of maintenance treatment (Fig 3).
This case clearly illustrates that a pathogenesis-based therapy with simvastatin alone can reverse the ichthyosiform skin lesions in CHILD syndrome within a few weeks. To our knowledge, this is the first reported case of CHILD nevus successfully treated with topical statin monotherapy. This brings hope that further research into lipid metabolism of the skin will lead to even more effective treatments of not only CHILD syndrome but also other types of ichthyoses.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Bolognia J.L., Jorizzo J.L., Rapini R.P. 2nd ed. Elsevier Health Sciences; Mosby: 2008. Dermatology. [Google Scholar]
- 2.Porter F.D., Herman G.E. Malformation syndromes caused by disorders of cholesterol synthesis. J Lipid Res. 2011;52:6–34. doi: 10.1194/jlr.R009548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paller A.S., Van Steensel M.A., Rodriguez-Martin M. Pathogenesis-based therapy reverses cutaneous abnormalities in an inherited disorder of distal cholesterol metabolism. J Invest Dermatol. 2011;131:2242–2248. doi: 10.1038/jid.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Happle R., Koch H., Lenz W. The CHILD syndrome. Congenital hemidysplasia with ichthyosiform erythroderma and limb defects. Eur J Pediatr. 1980;134:27–33. doi: 10.1007/BF00442399. [DOI] [PubMed] [Google Scholar]
- 5.Happle R. Ptychotropism as a cutaneous feature of the CHILD syndrome. J Am Acad Dermatol. 1990;23:763–766. doi: 10.1016/0190-9622(90)70285-p. [DOI] [PubMed] [Google Scholar]
- 6.Elias P.M., Williams M.L., Feingold K.R. Abnormal barrier function in the pathogenesis of ichthyosis: therapeutic implications for lipid metabolic disorders. Clin Dermatol. 2012;30:311–322. doi: 10.1016/j.clindermatol.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szabo G.P., Olah A.V., Kozak L. A patient with Smith-Lemli-Opitz syndrome: novel mutation of the DHCR7 gene and effects of therapy with simvastatin and cholesterol supplement. Eur J Pediatr. 2010;169:121–123. doi: 10.1007/s00431-009-0987-z. [DOI] [PubMed] [Google Scholar]
- 8.Feingold K.R. The regulation and role of epidermal lipid synthesis. Adv Lipid Res. 1991;24:57–82. doi: 10.1016/b978-0-12-024924-4.50007-9. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Acebes S., de la Cueva P., Fernandez-Hernando C. Desmosterol can replace cholesterol in sustaining cell proliferation and regulating the SREBP pathway in a sterol-Delta24-reductase-deficient cell line. Biochem J. 2009;420:305–315. doi: 10.1042/BJ20081909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu T., Qian G., Wang X.X., Zhang Y.G. CHILD syndrome: Effective treatment of ichthyosiform naevus with oral and topical ketoconazole. Acta Derm Venereol. 2015;95:91–92. doi: 10.2340/00015555-1859. [DOI] [PubMed] [Google Scholar]