Abstract
Background
With the increasing of ageing population, tuberculosis in the elderly brings a challenge for the tuberculosis (TB) control in China. Enough social support can promote the treatment adherence and outcome of the elderly patients with TB. Exploring effective interventions to improve the social support of patients is of great significance for TB management and control.
Methods
A community-based, repeated measurement trial was conducted. Patients with TB >65 years of age were allocated into the intervention or control group. Patients in the intervention group received comprehensive social support interventions, while those in the control group received health education alone. The social support level of patients was measured at baseline and at the first, third and sixth months during the intervention to assess the effectiveness of comprehensive social support interventions.
Results
A total of 201 patients were recruited into the study. Compared with the control group, social support for patients in the intervention group increased significantly over time (βgroup*time=0.61, P<0.01) in the following three dimensions: objective support (βgroup*time=0.15, P<0.05), subjective support (βgroup*time=0.32, P<0.05) and support utilisation (βgroup*time=0.16, P<0.05). The change in the scores in the control group was not statistically significant.
Conclusions
The intervention programme in communities, including health education, psychotherapy and family and community support interventions, can improve the social support for elderly patients with TB compared with single health education.
Trial registration number
ChiCTR-IOR-16009232
Keywords: tuberculosis, the elderly, social support, intervention
Introduction
Although great progress in tuberculosis (TB) control has been made over the last two decades,1 TB remains one of the biggest health problems in China.2 3 Concurrently, WHO reported that the burden of TB disease is shifting to the elderly,4 as the proportion of the older population will increase from 12.4% in 2010 to 28% in 2040 in China.5 According to the fifth national TB survey conducted in China in 2010, the TB prevalence increased with age and peaked in the 75–79 age group.6 TB in the elderly has already become a problem beyond neglect for TB control in China.
Advanced age, concomitant diseases and waning immunity make older people vulnerable to developing TB due to the reactivation of Mycobacterium tuberculosis from infection at a young age.7 8 Compared with other people, elderly individuals with TB need more support because they are more likely to experience negative life events, such as reduced mobility, loss of social status, loneliness after retirement, stigma, social isolation, financial burden and adverse effects of medication.9–11 A qualitative study found that educational, psychological and emotional supports were needed for these patients.12 Evidence has shown that social support is positively associated with health-seeking behaviours, treatment adherence and health outcomes and that it can act as a stress buffer for the psychosocial well-being of patients.13–15 However, a study conducted in Zhejiang Province of China reported that patients with TB had a low level of social support.16 It is meaningful to explore feasible and effective social support interventions in communities for TB management and control.
Social support intervention in patients with TB was recommended by WHO for the programmatic management of drug-resistant TB and the new End TB Strategy.17 Social support via various educational, psychosocial interventions has also been implemented to enhance treatment adherence.14 However, as the types of support, patterns of intervention, target groups and study settings were different, the magnitude of the benefit of these social support interventions should be considered with caution.18 Additionally, most of the studies focused on the effect of social support interventions on treatment adherence or outcomes. Hardly any study assessed the effect of these interventions on the level of social support patients perceived. The social support patients perceived may act as an intermediate variable between the social support intervention and the treatment adherence or outcomes. Exploring the effect of social support interventions on the level of social support of patients can help to understand how social support intervention influences the treatment adherence or treatment outcomes of patients.
To the best of our knowledge, no research has explored interventions to improve the social support of elderly patients with TB in China. Therefore, based on the hypothesis that comprehensive social support interventions might increase the social support of the elderly with TB, we conducted this community-based trial to assess the effects of the comprehensive interventions on the improvement of social support of elderly patients with TB.
Methods
Study settings
This study was conducted in Hubei Province, China, from November 2015 to April 2016. Hubei Province is one of the top 10 high TB-incidence provinces in China and the Directly Observed Treatment, Short-course (DOTS) strategy has been well implemented among its communities.19 After treated in hospitals for the intensive phase, patients with TB are treated as outpatients in communities. Community health centres are responsible for the management of these patients with TB. All patients with TB that are newly diagnosed in all medical institutions must be reported to the local Centers for Disease Control and Prevention through the internet-based National Infectious Diseases Reporting System (NIDRS).20 So information on patients with TB, such as gender, age, occupation before retirement, diagnosis date and sputum smear result, was collected from the NIDRS.
Sample size
As the social support scores of patients were designed to be measured four times during the study, the sample size was calculated according to the repeated-measures formula: M=2 [1+(k-1)ρ] σ2(Z1-α/2+Z1-β)2/kδ2.21 The following parameters were used in this formula: power of 85% and type I error of 5% (two-sided), number of repeated times K=4, smallest detected meaningful difference δ=4.2, correlation coefficient among measures ρ=0.70 and SE σ=10 based on the results of pilot study. Consequently, 195 patients were needed for this study. To obtain sufficient patients, 12 communities in both cities were estimated to be randomly selected.
Study sample
To perform interventions more easily and avoid information contamination among patients, we used a multistage sampling method. Among the 16 major cities in Hubei Province, Wuhan City and Enshi City were randomly selected and assigned to the intervention and control groups, respectively. Then, 12 communities in each city were randomly selected. The elderly patients with TB in these communities who were registered in the NIDRS were all included in the corresponding group. Because all of the patients in one community were in the same group and because all staff (psychologists, community health workers and administrators) who conducted the intervention could not be blinded to the study group, the patients and staff were not blinded.
Patients in this study met the following inclusion criteria: (a) diagnosed with TB at a local medical institute for TB control according to the WHO guideline,22 (b) >65 years of age, (c) local residents, (d) registered in the NIDRS, (e) normal communication ability and (f) volunteered to participate in this study. Patients were excluded if they (a) were suffering from mental health disorders, (b) had cognitive impairment or (c) were enrolled in other studies.
Interventions
This study lasted for 6 months with an intervention frequency of twice per month. Patients in the control group received the health education intervention alone, and those in the intervention group received psychotherapy and family and community support interventions in addition to health education. Except for the psycho-educational workshops in the family and community support interventions, these interventions were performed in a one-to-one setting rather than a group setting to avoid cross-infection among patients.
Health education
Health education consisted of basic knowledge about TB (including transmission route, treatment policy, therapeutic regimen), psychological coping skills (including treatment side effects, effective communication, confidence enhancement), reasonable diet (including light diet, low salt and fat diet, high protein diet) and healthy lifestyle (including smoking and drinking cessation, regular physical exercise). TB health brochures were also delivered to the patients. It was conducted by community health workers at patients’ homes and lasted approximately 30 min per patient.
Psychotherapy
To eliminate the mental health problems of patients, Morita therapy was delivered to patients at their home by psychologists of the Tongji Research Center of Mental Health at Tongji Medical College, Huazhong University of Science and Technology. A checklist of the key components of Morita therapy was developed according to prior studies23–25 before the intervention and was strictly followed during the intervention. Throughout the study, every patient was asked to complete a diary for psychologists to evaluate the intervention. Every psychotherapy session lasted approximately 30 min per patient.
Family and community support interventions
This part included home visits, psycho-educational workshops and peer support. During the study, one community health worker and one community administrator conducted home visits to communicate and construct a harmonious relationship with the patients. Simultaneously, family members and friends of patients were invited to attend psycho-educational workshops to receive basic knowledge about TB and encourage them to express their emotional pressure. Additionally, recovered patients with TB and their family members were invited to provide peer support. They shared their experiences with patients and their family members about how to solve problems and improve self-care.
Outcome measurement
The primary outcome was the social support level of patients and was evaluated by the Social Support Rating Scale (SSRS). This multidimensional scale consists of three dimensions that measure objective support, subjective support and support utilisation. The total SSRS score ranges from 12 to 66, with a higher score indicating the better availability of support. The reliability and validity of this scale were relatively high when it was applied to measure social support in the Chinese population.16 26 In this sample, Cronbach’s alpha for the total score was 0.91. Details of the SSRS are available in the online supplementary appendix 1.
jech-2017-209458supp001.pdf (10.5KB, pdf)
Data collection
Data were collected at baseline and at the first, third and sixth months after intervention initiation. Each patient was given the scale and asked to complete it alone. Investigators could provide an explanation for any confusion about the scale to avoid any error and ensure the data quality. The investigation was supervised and coordinated by a supervisor. Data were double-entered into the EpiData V.3.1 software. Scales with missing data concerning any items were excluded from the final analysis.
Statistical analysis
The normality of the data was tested by the Kolmogorov-Smirnov test. Continuous and categorical variables were presented as the means (SD) and frequencies (percentages), respectively, and compared by the t-test and χ2 test, respectively. Considering the structure of repeated-measures data, a multilevel model was performed to assess the changes of social support scores between two groups. These analyses were performed using the Statistical Analysis System V.9.2, and the sample size was calculated using the Power Analysis and Sample Size software V.11.0. A two-sided P value <0.05 was considered statistically significant.
Results
Demographic and TB-related characteristics
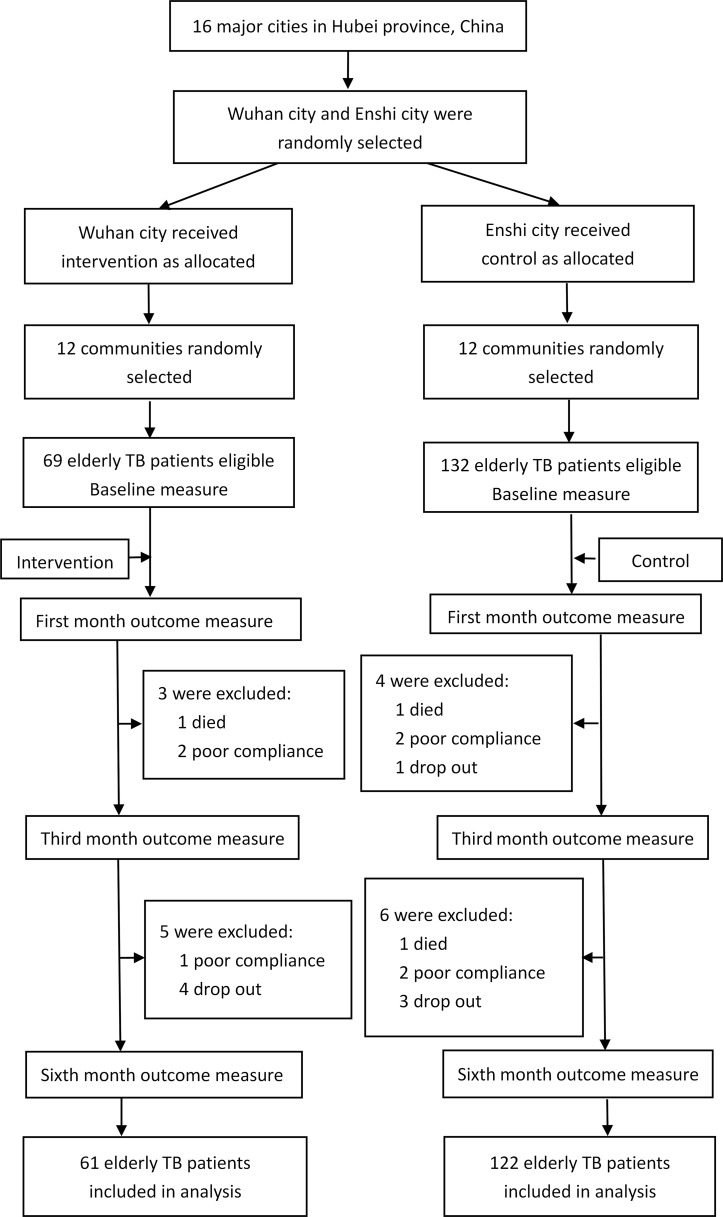
A total of 201 patients were recruited at the beginning of the study (69 in the intervention group and 132 in the control group). During the intervention, 18 patients in two groups were excluded (one died, three showed poor compliance and four dropped out in the intervention group; two died, four showed poor compliance and four dropped out in the control group). Finally, 183 patients were included in the final analysis (61 in the intervention group and 122 in the control group) (see figure 1). Overall, the percentages of men in the two groups were similar and the mean ages of the two groups were both close to 72 years. No significant differences were observed in the baseline characteristics between the groups (see table 1).
Figure 1.
Flow chart of the trial. TB, tuberculosis.
Table 1.
Demographic and tuberculosis (TB)-related characteristics of the elderly patients with TB at baseline (n=183)
| Variable | Intervention group (n=61) |
Control group (n=122) |
P value |
| Male, n (%) | 34 (55.7) | 75 (61.4) | 0.379 |
| Age, mean (SD) | 71.77 (5.49) | 71.88 (5.38) | 0.897 |
| TB initial treatment stage, n (%) | 48 (78.6) | 106 (65.8) | 0.152 |
| TB intensive management, n (%) | 15 (24.6) | 36 (31.2) | 0.356 |
| Education level, n (%) | 0.699 | ||
| Primary school | 9 (14.7) | 17 (13.9) | |
| Junior middle school | 28 (45.9) | 46 (37.7) | |
| Senior high school | 16 (26.2) | 39 (32.0) | |
| College or above | 8 (13.1) | 20 (16.4) | |
| Occupation before diagnosed, n (%) | 0.976 | ||
| Merchant | 8 (13.1) | 15 (12.2) | |
| Factory workers | 38 (62.2) | 74 (60.6) | |
| Civil servant | 7 (11.4) | 14 (11.6) | |
| Farmer | 8 (13.1) | 19 (15.6) | |
| TB knowledge*, n (%) | 17 (27.8) | 37 (30.3) | 0.731 |
| Chronic comorbidity†, n (%) | 26 (42.6) | 55 (45.0) | 0.752 |
*The total awareness rate of the five key messages about TB prevention and treatment proposed in Guidelines for implementation of tuberculosis control program in China (2008 edition).
†Other common chronic diseases coexisting with TB, including hypertension, diabetes mellitus, chronic obstructive pulmonary disease, asthma, coronary heart disease, tumour, arthritis, and so on.
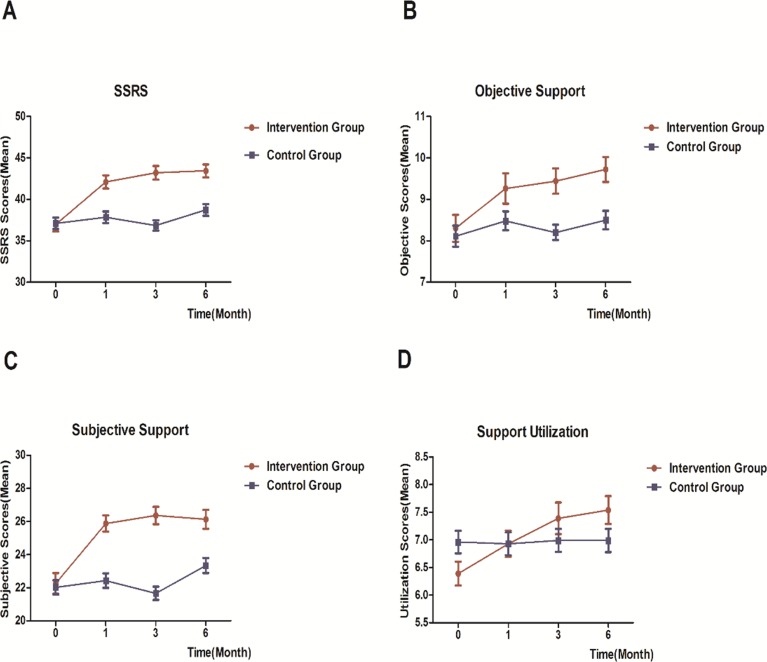
Change in social support scores
At baseline, the average scores of SSRS, objective support, subjective support and support utilisation of 183 patients were 37.04, 8.17, 22.10 and 6.77, respectively. The total SSRS score and scores of its three dimensions (objective support, subjective support and support utilisation) all showed an increasing trend in two groups during the intervention, but this trend was more obvious in the intervention group. At the end of intervention, these four scores in the intervention group were all higher than those in the control group (see figure 2).
Figure 2.
The change in Social Support Rating Scale (SSRS) score and scores for the three dimensions of social support in elderly patients with tuberculosis.
Multilevel model analysis of social support scores
The methods of multilevel analysis are available in the online supplementary appendix 2. After the background variables were controlled, the total SSRS scores and subjective support scores of the two groups were significantly different at baseline (βgroup=2.35, P<0.05 and βgroup=2.00, P<0.001, respectively). Additionally, the score of SSRS and its three dimensions (objective support, subjective support and support utilisation) at four times did not change significantly in the control group (βtime=0.24, P>0.05; βtime=0.04, P>0.05; βtime=0.16, P>0.05; and βtime=0.01, P>0.05, respectively). However, the differences in these four scores between the groups increased with changes in the time (βgroup*time=0.61, P<0.01; βgroup*time=0.15, P<0.05; βgroup*time=0.32, P<0.05; and βgroup*time=0.16, P<0.05, respectively) (see table 2).
Table 2.
Multilevel analysis results of the social support scores
| Parameter | Coefficient (SE) | |||
| SSRS scores | Objective support | Subjective support | Support utilisation | |
| Fixed effect | ||||
| Intercept | 34.15 (2.34)*** | 8.03 (0.82)*** | 19.42 (1.51)*** | 6.90 (0.78)*** |
| Group | 2.35 (0.95)* | 0.56 (0.34) | 2.00 (0.60)*** | −0.31 (0.30) |
| Gender | 0.68 (0.72) | −0.26 (0.25) | 1.15 (0.46)* | −0.22 (0.24) |
| Age | −0.34 (0.38) | −0.13 (0.13) | −0.15 (0.24) | −0.05 (0.12) |
| Treatment | 0.38 (0.92) | −0.57 (0.32) | 1.02 (0.59) | −0.08 (0.30) |
| Management | 0.23 (0.77) | 0.26 (0.27) | −0.13 (0.50) | 0.10 (0.26) |
| Education | 0.57 (0.40) | 0.26 (0.14) | 0.31 (0.26) | −0.02 (0.13) |
| Occupation | 0.03 (0.40) | 0.02 (0.14) | −0.05 (0.25) | 0.05 (0.13) |
| TB knowledge | 0.57 (0.78) | 0.04 (0.27) | 0.09 (0.51) | 0.41 (0.26) |
| Comorbidity | 1.62 (0.73)* | 0.39 (0.26) | 1.12 (0.47)* | 0.15 (0.24) |
| Time | 0.24 (0.13) | 0.04 (0.04) | 0.16 (0.08) | 0.01 (0.03) |
| Group*time | 0.61 (0.23)** | 0.15 (0.07)* | 0.32 (0.14)* | 0.16 (0.06)* |
| Random effects | ||||
| Level 2 (between individuals) | ||||
| τ00 | 16.44 (4.16)*** | 2.14 (0.52)*** | 5.94 (1.64)*** | 2.02 (0.40)*** |
| τ10 | −1.32 (0.85) | −0.12 (0.09) | −0.31 (0.33) | −0.11 (0.07) |
| τ11 | 0.48 (0.26)* | 0.02 (0.02) | 0.16 (0.10) | 0.05 (0.02)* |
| Level 1 (within individuals) | ||||
| σε 2 | 36.24 (2.67)*** | 4.45 (0.32)*** | 15.20 (1.12)*** | 2.82 (0.20)*** |
| 2log*likelihood | 4896.4 | 3361.3 | 4263.4 | 3131.6 |
*P<0.05, **P<0.01, ***P<0.001.
τ00, random intercept variance; τ10, covariance of random intercept and random slope; τ11, random slope variance of time variable; σε 2, residual variance within individuals; SSRS, Social Support Rating Scale; TB, tuberculosis.
Adverse effects
Due to the appropriate guidance, no adverse events associated with comprehensive social support interventions were reported for any patients during the trial.
Discussion
Based on the DOTS strategy, comprehensive social support interventions, including health education, psychotherapy and family and community support interventions, can increase the social support of elderly patients with TB compared with single health education.
Qualitative studies reported that health education was needed by patients with TB.9 12 Receiving more information about the disease might empower the patient to feel more confident and active in his or her treatment.12 However, a Cochrane review found insufficient evidence for the promotion of treatment adherence through health education.27 We found that the social support of patients was not improved obviously through health education. It indicates that TB health education alone is not effective in improving the social support for patients with TB. Effective educational interventions are those that aim to modify patients’ behaviour rather than simply providing information about the disease.28 Considering these, to promote the social support and health behaviour of elderly patients with TB, health education should be provided to those patients combined with other interventions rather than a single one.
Mental disorders, such as depression and anxiety, are often complicated with TB29 due to adverse reactions of drugs, inadequate social support and social stigma.30 Mental health interventions are suggested to provide for patients with TB to tackle their mental issues.9 12 30 Psychotherapies, such as group psychotherapy,31 have been proved to be effective in improving treatment adherence.13 32
In our study, Morita therapy was implemented for elderly patients with TB. Morita therapy is a psychotherapy that was developed in Japan by Dr Shoma Morita in 1919 and is aimed at eliminating the mental health problems of patients through transferring their attention from negative stress.33 This therapy is based on the premise that unpleasant symptoms are a natural part of the human experience.23 We found that most elderly patients with TB often isolated themselves from others because of stigma, but many of them gradually participated in social activities and then sought and used help from others during the intervention. Another significant change was that many patients were willing to disclose their disease to others after the intervention. Some studies pointed out that most of the patients with TB who disclosed their disease status to a wider audience received more positive support.12 34 These suggest that psychotherapy, such as Morita therapy, is effective in improving psychological issues of elderly patients with TB and should be considered as an essential part of the intervention to facilitate the social support of elderly patients with TB.
As the place in which elderly patients with TB lived, communities have great potential to provide valuable social support for patients.12 Involvement of family and community members to support patients with TB was found to be one way to improve treatment outcomes and overcome social issues like stigma.11 Hence, we incorporated the family and community interventions into the comprehensive interventions.
Through home visits, community health workers and administrators knew more about the elderly patients with TB and their families. These patients also expressed that they felt they were cared for and supported. They trusted these health workers and were also willing to ask for help from them. These phenomena indicate that the good patient–health worker relationship, which can be achieved through home visits, is significant for the support patients perceived and for their treatment, as has been found in other studies.12 16
Simultaneously, a study pointed out that caregivers might lose confidence during the treatment of patients with TB, which would result in reduced social support for patients.16 We held psycho-educational workshops for the family members and friends of the elderly patients with TB to lessen their psychological stress and increase their knowledge about TB. Many family members expressed that they experienced isolation by others and lacked knowledge about TB treatment. Through workshops, they gained more confidence and were more active in supporting patients’ treatment. This suggests that not only does the patients need psychological intervention and health education, but also family members and other caregivers need psycho-educational intervention to better support the elderly patients with TB.9 12
Additionally, we invited recovered patients with TB as peer support for the elderly patients with TB. During the intervention, most patients expressed that these former patients with TB understood how they felt. Some elderly patients with TB even developed valuable friendship with the recovered patients with TB. Several studies, which involved other chronic diseases, also proved that peer support was a useful method to support patients.35 36 It is of practical significance to treat recovered patients with TB as peer support to provide emotional support for the elderly with TB.12
Due to the design of the study, several limitations should be acknowledged. First, there might be some bias caused by the differences in the economic and medical level between Wuhan City and Enshi City. Although Wuhan City and Enshi City were selected and allocated into different groups randomly, patients with TB in Wuhan City, which is the biggest city in Hubei Province, might receive better medical services than patients in Enshi City. Second, we did not assess the social support of patients after the end of the study. Therefore, we are uncertain about whether our interventions could consistently influence the social support of patients. Further studies can be done to explore the long-term effects of these interventions on the social support of elderly patients with TB in communities. Third, although the scale used to evaluate the primary outcome in this study was developed based on China’s social conditions and tested with a good reliability and validity in China, it was not widely used to assess social support in foreign studies. This made the results of our study less comparable to foreign studies.
Conclusions
The key aspect of our study was to identify effective comprehensive social support interventions and assess its impact on the social support level of elderly patients with TB in communities. Our results showed that compared with the single health education the interventions, consisting of health education, psychotherapy and family and community support interventions, could effectively promote the social support for the elderly with TB in communities. The comprehensive interventions provide a reference value for the management of elderly patients with TB in China.
What is already known on this subject.
Evidence has shown that social support is positively associated with treatment adherence and health outcomes. But no study has explored effective interventions to improve the social support of elderly patients with tuberculosis (TB) in communities of China.
What this study adds.
This community-based trial found that interventions which consisted of health promotion, psychotherapy and family and community support interventions were effective to improve the social support for the elderly with TB. These could provide a reference value for the TB management in communities of China.
Acknowledgments
The authors thank all patients, psychologists, community health workers, community administrators and other participants for their support for this study.
Footnotes
Contributors: XL, BW and YX designed this research. XL wrote the manuscript. BW analysed the data. XL, DT, ML, DZ, CT, XC, YY, SZ and BJ organised the field intervention and collected questionnaires. SY, XL, QC and YX gave instructions on the study.
Funding: This work was supported by National Social Science Fund of China (grant number 15BSH118) and Innovation Research Fund of Huazhong University of Science and Technology (no. 2013TS004).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: This study was approved by the ethics committee of Tongji Medical College, Huazhong University of Science and Technology.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. An J, Gao M, Chu N, et al. Transregional movement of multidrug-resistant tuberculosis in north China: an underlying threat to tuberculosis control. Sci Rep 2016;6:29727 10.1038/srep29727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence in China, 1990-2010; a longitudinal analysis of national survey data. Lancet 2014;383:2057–64. 10.1016/S0140-6736(13)62639-2 [DOI] [PubMed] [Google Scholar]
- 3. Li X, Zhang Y, Shen X, et al. Transmission of drug-resistant tuberculosis among treated patients in Shanghai, China. J Infect Dis 2007;195:864–9. 10.1086/511985 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Global tuberculosis report 2016. Geneva: World Health Organization, 2016. [Google Scholar]
- 5. World Health Organization. China country assessment report on ageing and health. Geneva: World Health Organization, 2015. [Google Scholar]
- 6. Wang LX, Cheng SM, Chen MT, et al. The fifth national tuberculosis epidemiological survey in 2010. Chin J Antituberculosis 2012;34:485–508. Chinese. [Google Scholar]
- 7. Schaaf HS, Collins A, Bekker A, et al. Tuberculosis at extremes of age. Respirology 2010;15:747–63. 10.1111/j.1440-1843.2010.01784.x [DOI] [PubMed] [Google Scholar]
- 8. Tatar D, Senol G, Alptekin S, et al. Tuberculosis in older adults. Eur Geriatr Med 2013;4:15–19. 10.1016/j.eurger.2012.09.005 [DOI] [Google Scholar]
- 9. Morris MD, Quezada L, Bhat P, et al. Social, economic, and psychological impacts of MDR-TB treatment in Tijuana, Mexico: a patient’s perspective. Int J Tuberc Lung Dis 2013;17:954–60. 10.5588/ijtld.12.0480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rajeswari R, Muniyandi M, Balasubramanian R, et al. Perceptions of tuberculosis patients about their physical, mental and social well-being: a field report from south India. Soc Sci Med 2005;60:1845–53. 10.1016/j.socscimed.2004.08.024 [DOI] [PubMed] [Google Scholar]
- 11. Thomas BE, Shanmugam P, Malaisamy M, et al. Psycho-Socio-Economic Issues Challenging Multidrug Resistant Tuberculosis Patients: A Systematic Review. PLoS One 2016;11:e147397 10.1371/journal.pone.0147397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paz-Soldán VA, Alban RE, Jones CD, et al. The provision of and need for social support among adult and pediatric patients with tuberculosis in Lima, Peru: a qualitative study. BMC Health Serv Res 2013;13:1–12. 10.1186/1472-6963-13-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Hoorn R, Jaramillo E, Collins D, et al. The effects of psycho-emotional and socio-economic support for Tuberculosis patients on treatment adherence and treatment outcomes - a systematic review and meta-analysis. PLoS One 2016;11:e154095 10.1371/journal.pone.0154095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Munro SA, Lewin SA, Smith HJ, et al. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med 2007;4:e238 10.1371/journal.pmed.0040238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lönnroth K, Glaziou P, Weil D, et al. Beyond UHC: monitoring health and social protection coverage in the context of tuberculosis care and prevention. PLoS Med 2014;11:e1001693 10.1371/journal.pmed.1001693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen B, Peng Y, Zhou L, et al. Social support received by multidrug-resistant tuberculosis patients and related factors: a cross-sectional study in Zhejiang Province, People’s Republic of China. Patient Prefer Adherence 2016;10:1063–70. 10.2147/PPA.S105655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. Companion Handbook to the WHO Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis. Geneva: WHO Document Production Services, 2014. [PubMed] [Google Scholar]
- 18. Jakubowiak WM, Bogorodskaya EM, Borisov SE, et al. Risk factors associated with default among new pulmonary TB patients and social support in six Russian regions. Int J Tuberc Lung Dis 2007;11:46–53. [PubMed] [Google Scholar]
- 19. Zhang G, Huang S, Duan Q, et al. Application of a hybrid model for predicting the incidence of tuberculosis in Hubei, China. PLoS One 2013;8:e80969 10.1371/journal.pone.0080969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet 2007;369:691–6. 10.1016/S0140-6736(07)60316-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu H, Wu T. Sample size calculation and power analysis of time-averaged difference. J Mod Appl Stat Methods 2005;4:434–45. 10.22237/jmasm/1130803680 [DOI] [Google Scholar]
- 22. World Health Organization. Treatment of tuberculosis: guidelines. 4th edition Geneva: World Health Organization, 2010. [Google Scholar]
- 23. Morita M, Kondō A, LeVine P. Morita therapy and the true nature of anxiety-based disorders. Albany: State University of New York Press, 1998. [Google Scholar]
- 24. Ogawa B. Desire for life: the practitioner’s introduction to morita therapy for the treatment of anxiety disorders. Indiana: XLibris Publ, 2013. [Google Scholar]
- 25. LeVine P. Morita-based therapy and its use across cultures in the treatment of bulimia nervosa. J Couns Dev 1993;72:82–90. 10.1002/j.1556-6676.1993.tb02282.x [DOI] [Google Scholar]
- 26. Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health 2014;128:430–7. 10.1016/j.puhe.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 27. M’imunya JM, Kredo T, Volmink J. Patient education and counselling for promoting adherence to treatment for tuberculosis. Cochrane Database Syst Rev 2012;5:CD006591 10.1002/14651858.CD006591.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Becker MH, et al. Theoretical models of adherence and strategies for improving adherence : Shumaker SA, Schron EB, Ockene JK, Parker CT, Probstfield JL, Handbook of behavior change. New York: Springer, 1990. [Google Scholar]
- 29. Peltzer K, Naidoo P, Matseke G, et al. Prevalence of psychological distress and associated factors in tuberculosis patients in public primary care clinics in South Africa. BMC Psychiatry 2012;12:89 10.1186/1471-244X-12-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pachi A, Bratis D, Moussas G, et al. Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013;2013:1–37. 10.1155/2013/489865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Acha J, Sweetland A, Guerra D, et al. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2007;2:404–17. 10.1080/17441690701191610 [DOI] [PubMed] [Google Scholar]
- 32. Janmeja AK, Das SK, Bhargava R, et al. Psychotherapy improves compliance with tuberculosis treatment. Respiration 2005;72:375–80. 10.1159/000086251 [DOI] [PubMed] [Google Scholar]
- 33. Sugg HV, Richards DA, Frost J. Morita therapy for depression and anxiety (Morita Trial): study protocol for a pilot randomised controlled trial. Trials 2016;17:161 10.1186/s13063-016-1279-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health 2007;7:211–21. 10.1186/1471-2458-7-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Duckworth K, Halpern L. Peer support and peer-led family support for persons living with schizophrenia. Curr Opin Psychiatry 2014;27:216–21. 10.1097/YCO.0000000000000051 [DOI] [PubMed] [Google Scholar]
- 36. Fisher EB, Boothroyd RI, Elstad EA, et al. Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews. Clin Diabetes Endocrinol 2017;3:4 10.1186/s40842-017-0042-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2017-209458supp001.pdf (10.5KB, pdf)