Abstract
Exposure to household air pollution (HAP) from cooking and heating with solid fuels is major risk factor for morbidity and mortality in sub-Saharan Africa. Children under five are particularly at risk for acute lower respiratory infection. We use baseline data from randomized controlled trial evaluating a household energy intervention in Gisenyi, Rwanda to investigate the role of the microenvironment as a determinant of children’s HAP-related health symptoms. Our sample includes 529 households, with 694 children under five. We examine the association between likelihood of HAP-related health symptom prevalence and characteristics of the microenvironment including: dwelling and cooking area structure; distance to nearest road; and tree cover. We find that children residing in groups of enclosed dwellings, in households that cook indoors, and in households proximate to tree cover, are significantly more likely to experience symptoms of respiratory infection, illness with cough and difficulty breathing. On the other hand, children in households with cemented floors and ventilation holes in the cooking area, are significantly less likely to experience the same symptoms. Our findings suggest that in addition to promoting increased access to clean cooking technologies, there are important infrastructure and micro-environment related interventions that mitigate HAP exposure.
Keywords: Household air pollution, Africa, microenvironment, ventilation, biomass fuels, children, health
Introduction
Approximately 3 billion people, mostly in low-income countries, use solid fuels (wood, agricultural residue, dung, charcoal and coal) for cooking and heating (WHO 2016). Though there has been a decline in the relative share of the global population using solid fuels (dropping from 62% to 41% between 1980 and 2010), owing to population growth and thin or missing markets for improved cooking fuels and technologies (GACC 2017), the absolute number of solid fuel users has remained high. Close to 646 million people using solid fuels reside in sub-Saharan Africa (SSA), and the absolute number of users is expected to continue to increase through 2030 (Bonjour et al 2015). Burning solid fuels in three-stone fires or other traditional stoves exposes households to health-damaging pollutants, namely fine particulate matter (PM2.5), carbon monoxide (CO), and polycyclic aromatic hydrocarbons (Bruce et al 2000). The resulting household air pollution (HAP) accounts for 3.7–4.8 million deaths, as per WHO 2012 estimates, while the Global Burden of Disease (GBD) Study estimates between 2.2 million to 3.6 million deaths (Landrigan et al. 2017) from HAP. HAP-related illnesses responsible for millions of these deaths include stroke (34%), ischemic heart disease (26%), chronic obstructive pulmonary disease (22%), pneumonia (12%), and lung cancer (6%) (WHO 2016).
Acute lower respiratory infections (ALRI) are the major cause of death among under 5 years children (under-fives) in less developed countries (Smith et al 2014), and lower respiratory infection (LRI) the leading cause of death in 2016 across all age groups (GBD 2017). Pneumonia, a type of acute respiratory infection (ARI), is one of the leading causes of death among under-fives (15%), and in 2015 accounted for approximately 920,000 deaths in this age group (WHO 2016). Over half of the premature deaths from pneumonia among under-fives were caused by HAP (WHO 2016). As children typically spend a large amount of time with mothers and caregivers who also have cooking responsibilities, under-fives experience relatively high levels of HAP exposure (Gordon et al 2014). Infants and young children are particularly susceptible to severe respiratory infections (e.g. inflamed lung airways and alveoli) from HAP pollutants due to their undeveloped respiratory defense mechanisms and airways (Smith et al 2014). Biomass fuel use is also associated with prevalence of anemia (Mishra and Retherford 2006) and stunting in under-fives (Mishra and Retherford 2006; Kyu et al 2009). In more recent evidence, solid fuel use leads to lower height-forage, and increases probability of stunting and severe stunting in Indian children under 3 years (Balietti and Datta 2017).
Since 2010, 80.9 million clean or efficient stoves and fuels, that emit lower indoor emissions and use less fuel, respectively, have been distributed (GACC 2017). However, their sustained and exclusive adoption remains a challenge. Addressing market barriers to encourage production, distribution and use of clean cooking technologies is an ongoing, long-term goal for all stakeholders and partners in the clean cooking and energy sector. In the interim, changes to house construction (Bruce et al 2004) and modifications to cooking area ventilation (Yadama et al 2012) are alternative or additive solutions. Balakrishnan et al (2002) find type of fuel (fuelwood vs. kerosene or LPG) to be the most important determinant of HAP in rural southern India, in addition to cooking area location (indoor vs. outdoor) and kitchen ventilation. In Malawi, use of firewood or crop residue for cooking, compared to charcoal use, is associated with higher odds of primary cooks experiencing cardiopulmonary and neurologic symptoms (Das et al 2016). While type of fuel/stove is the most important determinant of kitchen CO in Bruce et al’s (2004) study in rural Guatemala, they also find significant positive associations between eave space size, kitchen volume and kitchen CO, but no independent relationship between kitchen volume and young (under 18 months) children’s CO exposure.
Cooking location can have a large observed effect on exposure and health (Langbien 2017). Median exposure reductions of 57–73% have been observed when comparing indoor and outdoor kitchens (Albalak et al 2001; Rosa et al 2014). Others find 93–98% reductions in PM2.5 1-hour concentrations and 83–95% reductions in CO concentrations when comparing open versus closed kitchens, through increased air exchange rates in open kitchens (Grabow et al 2013). Land-use regression studies examining spatial differences in outdoor air pollution find population density to be one of the significant predictors of PM and other pollutants (Hoek et al 2008). Laboratory-based investigations suggest that improvements in ventilation (e.g. building design, wind speed and direction) may lead to reductions in exposure equivalent to those estimated for improved cookstoves (ICS) intervention studies (Ruth et al 2014). Studies examining this relationship have found no significant effect of increasing permeability of roof or walls on human health (Pitt et al 2006), while others find that additional ventilation is associated with a 12% reduction in tracheobronchial particle index in the household, after controlling for modified stove (Yadama et al 2012).
The only structural factors included in Dheerani et al’s (2008) meta-analyses on HAP and underfives’s risk of pneumonia, were stove type (improved vs. traditional) and cooking or heating location (inside vs. outside house). Jagger and Shively (2014) find a higher ARI incidence among under-fives in Ugandan households using fuelwood from non-forest areas, but the opposite correlation in households using crop residues for cooking. Under-five children in Malawi residing in improved homes (fired mud brick walls, tile roofing and concrete foundation) have significantly lower odds of experiencing respiratory, gastrointestinal or malaria-related illnesses, compared to those in traditional houses with mud brick walls, thatch roofing and hard packed mud floors (Wolff et al 2001). Cattaneo et al (2008) , find that Mexico’s Piso Firme program (that offered households with dirt floors a maximum of 538 square feet of concrete cement floors) significantly decreased incidence of parasitic infestations and diarrhea, prevalence of anemia, and significantly improved cognitive development among children aged 0–5 years. Northridge et al’s (2008) study in New York City finds that children residing in private (vs. public) housing have significantly lower odds of asthma. Household crowding may predispose children to viral respiratory illnesses, and housing construction changes have increased indoor allergen exposure (Wright and Fisher 2003). Globally, solid fuel combustion from household cooking accounts for 12% of ambient fine particulate air pollution, the highest (37%) being in SSA (Chafe et al 2014). In a densely populated slum community in Bangladesh, Chowdhury et al (2012) find reductions in personal exposures from ICS, but high neighborhood PM2.5 concentrations, suggesting a need for community-wide improved energy solutions. Researchers have argued for the need to study the effects of exchange between outdoor and indoor microenvironments on area concentrations and personal exposures (Clark et al 2013).
Among school children in Nottingham, UK living within 150 meters of a main road, wheezing risk significantly increased with increasing main road proximity (Venn et al 2001). Gehring et al (2010) find significant positive correlations between traffic-linked air pollution (PM2.5, NO2, soot) at birth address and asthma-related symptoms among Dutch children observed from birth till 8 years. In Southern California, USA, McConnell et al (2010) find kindergarten and first-grade children with high asthma risk from modeled road traffic-related pollutants. Computer modeling studies show that trees and shrubs remove vast proportions of air pollutants (O3, PM10, NO2, SO2 and CO) that in turn improve urban air quality. Gaseous air pollutants are eliminated mainly through leaf stomata or plant surface, and absorption by trees (Nowak et al 2006). Using an atmospheric transport model, McDonald et al (2007) find that increasing tree cover in two UK conurbations reduces PM10 air concentrations. Nowak et al (2014) in their simulation study find that trees and forests in USA removed 17.4 million tons of air pollution in 2010, and 670,000 incidences of ARI symptoms were avoided, primarily in urban areas.
While previous studies have considered some housing structure factors (cooking location, building design, roof/wall permeability, stove type) in areas of high HAP exposure, not all studies consider health end-points as the main outcomes of interest. Second, no study has considered the interplay of all the aforementioned factors; and third, none has been conducted in SSA. As the empirical evidence on the role of household structural factors and the neighborhood environment on human health, in areas of high HAP exposure, is limited and inconclusive, this paper estimates the association between microenvironment and young children’s health in urban Rwandan households that primarily use biomass cooking fuel. Rwanda is the most densely populated country in SSA, with a population density of 481.7 per square kilometer (United Nations Statistics Division 2017); lower respiratory infection is the leading cause of years of life lost (GBD 2016 Causes of Death Collaborators 2017) and over 95% of the population uses biomass for cooking (GACC 2016). Though Rwanda made significant progress in achieving an under-five mortality rate of 54/1000 live births in 2013, stunting in under-fives is still high at 44% (WHO 2015). The Government of Rwanda has made strides in improving access to clean water and sanitation, and rural roads, and is now prioritizing increasing geographical access to health facilities (WHO 2015).
In addition to examining the association between the microenvironment and prevalence of child health symptoms, we will test the hypothesis that in households where the primary caregiver of a young child is also the household primary cook, there is likely to be a stronger association between caregiver’s CO exposure (as a proxy for child’s exposure) and children’s HAP-related health symptoms. In defining the household microenvironment, we consider crowding in the immediate vicinity of the household, cooking location, indicators of cooking area ventilation, distance to any road-paved or unpaved (as a proxy for dust and motor vehicle emissions) and percentage tree cover around households. We hypothesize positive associations between agglomerated dwellings, unventilated cooking areas, low quality kitchen structure, and proxies for environmental exposures, and HAP-specific measures of health.
Methodology
Data
We use baseline data from an ongoing randomized controlled trial of an improved household energy initiative in Gisenyi Sector, Rubavu District in Rwanda’s Western Province. We collected data in June 2015 for 1,462 urban households across 22 purposively selected Umudugudus (neighborhoods/sub-divisions) in 2 cells1 (Bugoyi and Kivumu) of Gisenyi town. The sample for this paper includes 694 under-fives residing in 529 households.
At baseline, an extensive survey was administered, with 17 modules including household demographics; physical characteristics of housing and kitchen structure, and cooking technology; health of children and primary cooks; cooking history of primary cooks; time use and preferences; and household expenditure. For each household, we also collected GPS coordinates and objectively measured 24-hour CO exposure of the primary cook. The CO data logger2 (EL-USB-CO, Lascar Electronics) was secured to the cook by use of a lanyard or a clip that the cook wore continuously for 24 hours, except while bathing and sleeping. Of the full sample of 1,462 households, 28 households refused to participate in the CO monitoring. Valid CO exposure information was collected from 78.7% of the study households (N=1,150). The remaining CO data files downloaded from the CO data loggers were unusable owing to batteries of data loggers dying prior to the end of the 24-hour monitoring periods and inability to match CO data loggers’ files with the database. The data loggers recorded CO concentrations once per minute. From each of the data files, a 24-hour average and hourly averages were calculated for each household with children under five (N=529).
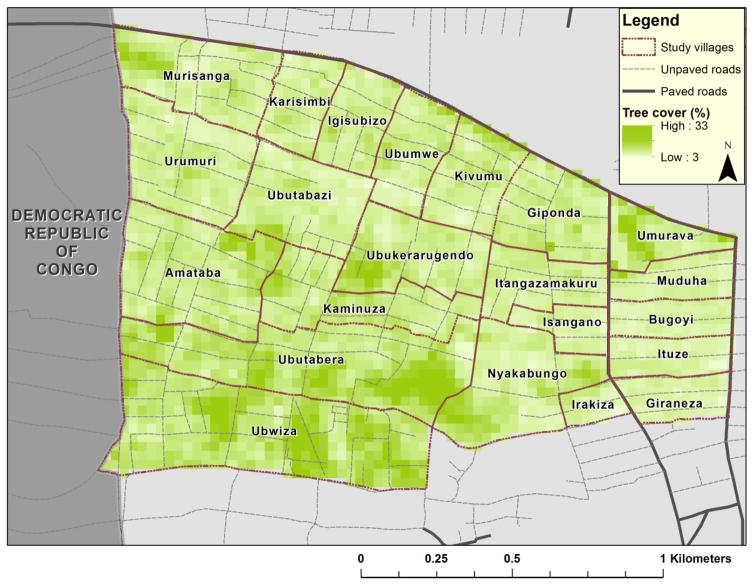
Geospatial information about paved and unpaved roads for the study area was obtained from open access OpenStreetMap (OSM) data. OSM is a volunteered geographic information containing extensive vector data for many African countries. The validity and completeness of the data were assessed using a map compare tool (http://tools.geofabrik.de/mc) and by overlaying the extracted vector information on the available Google satellite imagery. The paved and unpaved roads were differentiated using attribute information stored in the feature tags as 'surface'='paved' or 'surface'='unpaved'. The distance to the nearest paved, unpaved and any road for each household was calculated using the 'Near' tool in the ArcGIS toolbox (ArcGIS version 10.3). The tree cover data were extracted from the freely available LandSat WRS2 30m percentage tree cover data for 2015 (ftp://ftp.glcf.umd.edu/glcf/LandsatTreecover/WRS2). The percentage of tree cover around each household (30-meter resolution) was calculated using the 'Extract values to point' tool in the ArcGIS toolbox (ArcGIS version 10.3) by assigning the pixel value to the household point located in the corresponding pixel. Figure 1 shows our sampled villages, their proximity to roads and tree cover in the study area.
Figure 1.
Map of study area in Gisenyi, Rwanda.
Measures
The binary outcomes for analysis, asked to the mother or the person most knowledgeable about an under-five, based on 2-weeks recall include prevalence of the following HAP-related health symptoms: respiratory infection, illness with cough, difficulty breathing and dry eyes. The only non-HAP-related health symptom is fever.
The main explanatory variables indicative of housing structure and cooking location are (a) type of dwelling, (b) cooking location, and (c) kitchen floor material. For households that do not cook fully outdoors, we include specifics on cooking area ventilation, namely, (a) kitchen roof presence, (b) gap between walls and ceiling, (c) number of windows, (d) presence of ventilation holes, and (e) presence of active chimney to remove cooking area smoke. We include the main type of stove used in the past 30 days as a key determinant of HAP exposure, and determinants of other environmental exposures such as distance (in meters) to the nearest road (paved or unpaved road)3 and tree cover. We also control for individual-level characteristics such as age, sex, and health card availability of child; age, sex, and education level of the main respondent (as a proxy for household head). Household characteristics controlled for include log of per capita total expenditure in the past 4 weeks, household size, and weekly charcoal use per capita. For 367 children where the caregiver is the primary cook in the household, caregiver’s CO exposure is the main explanatory variable.
Empirical Strategy
First, we use a logit model to estimate the likelihood of caregiver-reported health symptoms for children using the following equation:
where Yij denotes a health symptom for child ‘i’ in household ‘j’; Ωi represents confounding variables at the individual-level, αj denotes potential household-level confounding variables and εij is the error term.
Second, in the model above, we include a continuous variable for the log of daily average CO concentration of the caregiver as the main explanatory variable. We run both models in the full sample without cooking area specifics, and in the sub-sample of households not cooking fully outdoors, with specific cooking area variables.
Results
Descriptive Statistics
We find high prevalence of illness with cough (36.2%) and illness with fever (29.1%) in our sample of under-fives (Table 1a). The cardiopulmonary symptom of difficulty breathing was prevalent among 20.1% children, and respiratory infection was least prevalent at 14.4%. As there are no
Table 1.
Summary statistics: Baseline results
| a. Dependent Variables: Health symptoms of children under 5 years (N=694) | |||
|
| |||
| HAP-related | % | ||
| Respiratory infection | 12.25 | ||
| Illness with cough | 36.17 | ||
| Difficulty breathing | 20.17 | ||
| Dry eyes | 14.41 | ||
| Other | |||
| Illness with fever | 29.11 | ||
|
| |||
| b. Independent Variables | |||
|
| |||
| Mean | SD | N | |
| Household characteristics | |||
| Per capita monthly total expenditures (in RWF) [1RWF=0.0012 USD] | 56,550.80 | 40,584.28 | 529 |
| Household size (mean) | 5.94 | 2.6 | 529 |
| Most used stove for cooking in the past 30 days (%) | |||
| Traditional 3 stone (open fire) | 2.84 | 529 | |
| Portable charcoal stove | 73.16 | 529 | |
| Fixed charcoal stove | 21.17 | 529 | |
| Improved stove (Electric stove, gas cooker, biogas) | 2.83 | 529 | |
| Per capita weekly charcoal use (in kgs) | 2.97 | 2.39 | 529 |
| Main respondent characteristics | |||
| Age (in years) | 33.56 | 10.57 | 529 |
| Female (%) | 88.66 | 529 | |
| Education level (%) | |||
| No education | 6.05 | 529 | |
| Pre-primary or primary | 19.28 | 529 | |
| Secondary | 42.16 | 529 | |
| University | 32.51 | 529 | |
| Awareness that smoke from burning biomass is harmful to human health (%) | 61.06 | 529 | |
| Child characteristics | |||
| Age (in months) | 27.18 | 16.28 | 694 |
| Female (%) | 49.42 | 694 | |
| Availability of health card for child (%) | 91.93 | 694 | |
| Housing structure | |||
| Dwelling type (%) | |||
| Single house | 15.31 | 529 | |
| Multiple house | 5.67 | 529 | |
| Group of multiple enclosed dwellings | 57.66 | 529 | |
| Group of single enclosed dwellings | 21.36 | 529 | |
| Cooking location (%) | |||
| Fully outdoors | 12.67 | 529 | |
| Partially outdoors | 10.78 | 529 | |
| Kitchen structure outside dwelling | 55.2 | ||
| Cooking inside dwelling | 21.36 | 529 | |
| Cooking area structure | |||
| Main material used in floors of cooking area (%) | |||
| Beaten earth | 17.96 | 529 | |
| Clay tiles, bricks and other materials | 40.45 | 529 | |
| Cement | 41.59 | 529 | |
| Kitchen roof presence (%) | 70.34 | 462 | |
| Gap between walls and ceiling (%) | 18.83 | 462 | |
| Number of windows (mean) | 0.66 | 0.66 | 462 |
| Ventilation holes (%) | 42.6 | 462 | |
| Presence of active chimney to remove smoke (%) | 4.3 | 462 | |
| Household environmental exposure | |||
| Nearest distance to any road (in meters) | 8.83 | 8.09 | 529 |
| Nearest distance to paved road (in meters) | 11.48 | 12.65 | 529 |
| Nearest distance to unpaved road (in meters) | 11.92 | 13.47 | 529 |
| Adjacent tree cover (in %) | 7.33 | 2.23 | 529 |
| Primary caregiver* exposure concentration | |||
| Daily average CO concentration (in ppm) | 6.77 | 9.42 | 282 |
These are unique primary caregivers of children under 5, who are also primary cooks in the household.
The average per capita monthly total expenditure is RWF 56,551 (~$66.9), average household size is 6, 94.3% household use either type of charcoal stove, and on average households use 3 kg of charcoal per capita, on a weekly basis (Table 1b). Majority main respondents are women (88.7%), the average age is 33.6 years, 42.2% have attained secondary education and 61.1% are aware of the negative health consequences from burning biomass fuels in traditional stoves. The average age of under-fives is 27.2 months, 49% are girls and 92% children have a health card. More than half of the households in the sample (57.7%) reside in group of multiple enclosed dwellings5, followed by group of single dwellings (21.4%). Over 55% households primarily cook in a designated kitchen outside their dwelling, close to 21% cook fully inside their dwelling, while 13% cook fully outdoors. An approximately equal share of households has cemented (41.6%) and brick floors (40.5%) in their cooking area. Among households that do not cook fully outdoors, 70% have a kitchen roof; in the cooking area, 19% have a gap between walls and ceilings, 43% have ventilation holes, and only 4% have an active chimney to remove smoke. On average, households have less than one window in their designated kitchen.
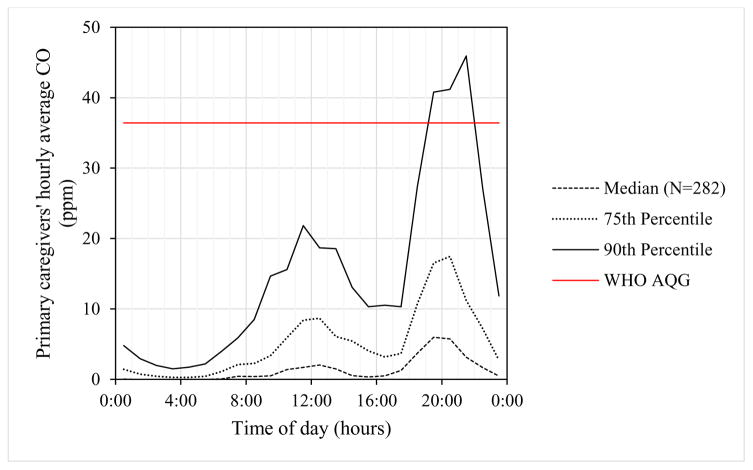
Households, on average, are 9 meters away from the nearest road (either paved or unpaved), and on average have 7.3% tree cover in their surrounding area. Primary caregivers’ daily average CO concentration is 6.8 parts per million (ppm). In addition to 24-hour average CO concentrations, hourly average CO concentrations were calculated for each hour of the day for each caregiver. Community patterns were determined by compiling hourly averages across all caregivers as shown in Figure 2. We find that, on average across the community, the caregivers' CO exposures are low overnight and in the early morning with peaks mid-day and in the early evening. The WHO hourly average air quality guideline (AQG) for CO is 35 mg/m3 (equivalent to 36.4 ppm in Gisenyi). While only 4.1% of all of the caregivers' hourly average concentrations, over the 24-hour monitoring period, exceeded the WHO AQG, 35.8% of the caregivers were exposed to CO concentrations exceeding the WHO AQG for at least one hour during the same period.
Figure 2.
Average hourly CO concentrations of under-fives’ primary caregivers, by time of day.
Regression Results
We find a strong positive association between group of multiple enclosed dwellings, relative to single house, and under-five children’s HAP-related symptoms (respiratory infection, difficulty breathing and dry eyes) and the non-HAP-related fever symptom experienced in the past 2 weeks (Table 2). Multiple house and group of single enclosed dwellings, compared to single house, have strong positive associations with dry eyes only. Relative to cooking fully outdoors, cooking partially outdoors (e.g. in the verandah) has a weak negative association with children experiencing illness with cough. Consistent with the literature, we find that cooking indoors is associated with significantly higher prevalence of most health symptoms. In the truncated sample of households not cooking fully outdoors, cooking either in a designated kitchen outside the main dwelling, or cooking fully inside the main house is associated with significantly higher likelihood of children experiencing illness with cough, difficulty breathing and fever.
Table 2.
Association between microenvironment, environmental exposure & under-fives’ health symptoms
| HAP-related | Other | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Dependent variables | Respiratory infection‡ | Illness with cough‡ | Difficulty breathing‡ | Dry eyes‡ | Fever‡ | |||||
| Explanatory variables | ||||||||||
| Housing structure | ||||||||||
| Dwelling type | ||||||||||
| Multiple house | 0.44 | 0.41 | 0.33 | 0.35 | 0.89* | 0.85 | 1.31** | 1.32** | 0.27 | 0.33 |
| (0.83) | (0.86) | (0.43) | (0.45) | (0.51) | (0.52) | (0.55) | (0.56) | (0.47) | (0.49) | |
| Group of multiple enclosed dwellings | 1.89*** | 1.88*** | 0.57** | 0.56* | 1.05*** | 1.03*** | 0.71* | 0.87** | 0.64** | 0.82** |
| (0.61) | (0.65) | (0.28) | (0.29) | (0.36) | (0.38) | (0.41) | (0.43) | (0.31) | (0.32) | |
| Group of single enclosed dwellings | 0.88 | 0.86 | 0.48* | 0.48 | 0.63* | 0.62 | 0.96** | 1.00** | 0.65** | 0.63* |
| (0.58) | (0.62) | (0.29) | (0.30) | (0.37) | (0.39) | (0.44) | (0.45) | (0.33) | (0.34) | |
| Cooking location | ||||||||||
| Partially outdoors | 0.54 | −0.65* | −0.17 | −0.24 | −0.50 | |||||
| (0.51) | (0.37) | (0.46) | (0.46) | (0.41) | ||||||
| Kitchen structure outside dwellings | 0.81 | 0.72 | 0.44 | 1.12** | 0.72* | 1.47** | −0.43 | 0.09 | 0.50 | 1.59*** |
| (0.50) | (0.79) | (0.33) | (0.47) | (0.42) | (0.58) | (0.42) | (0.75) | (0.37) | (0.54) | |
| Cooking inside dwelling | 0.90** | 0.00 | 0.57* | 1.29*** | 0.53 | 0.99** | 0.27 | 0.40 | 0.55* | 1.37*** |
| (0.45) | (0.48) | (0.30) | (0.37) | (0.37) | (0.43) | (0.38) | (0.47) | (0.32) | (0.40) | |
| Cooking area structure | ||||||||||
| Main floor material | ||||||||||
| Clay tiles, bricks and other materials | 0.66* | 0.06 | 0.30 | 0.32 | 0.17 | −0.10 | 0.50 | −0.52 | 0.21 | 0.48 |
| (0.37) | (0.70) | (0.31) | (0.45) | (0.37) | (0.58) | (0.42) | (0.87) | (0.31) | (0.48) | |
| Cement | −0.51 | −0.78* | 0.11 | 0.21 | 0.06 | 0.08 | 0.30 | 0.15 | −0.03 | 0.12 |
| (0.39) | (0.44) | (0.25) | (0.26) | (0.29) | (0.31) | (0.39) | (0.43) | (0.25) | (0.27) | |
| Kitchen roof | −1.22 | 0.08 | −0.70 | −1.32 | −0.12 | |||||
| (1.00) | (0.52) | (0.71) | (1.05) | (0.62) | ||||||
| Gap between walls and ceiling | 0.46 | 0.44* | 0.64** | 0.35 | 0.45* | |||||
| (0.37) | (0.23) | (0.27) | (0.33) | (0.25) | ||||||
| Number of windows | 0.51** | 0.15 | −0.06 | 0.39* | 0.10 | |||||
| (0.23) | (0.16) | (0.19) | (0.23) | (0.17) | ||||||
| Ventilation holes | −0.16 | −0.64*** | −0.69*** | −0.38 | −0.91*** | |||||
| (0.31) | (0.19) | (0.24) | (0.27) | (0.21) | ||||||
| Presence of active chimney | 0.37 | 0.34 | 0.19 | −0.47 | −0.14 | |||||
| (0.64) | (0.46) | (0.62) | (0.94) | (0.53) | ||||||
| Environmental exposure | ||||||||||
| Distance to nearest road (in meters) | 0.03* | 0.03** | 0.01 | 0.01 | −0.00 | −0.01 | 0.00 | 0.00 | −0.01 | −0.02 |
| (0.02) | (0.02) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Tree cover (%) | 0.14** | 0.17** | 0.06 | 0.02 | 0.18*** | 0.17*** | 0.11** | 0.12* | −0.06 | −0.08 |
| (0.06) | (0.08) | (0.04) | (0.05) | (0.05) | (0.05) | (0.05) | (0.07) | (0.05) | (0.06) | |
| Constant | −3.67 | −1.98 | 1.05 | 1.75 | −0.81 | −0.98 | −5.77** | −5.44* | −1.60 | −1.88 |
| (2.99) | (3.39) | (1.96) | (2.24) | (2.40) | (2.80) | (2.82) | (3.17) | (2.11) | (2.36) | |
|
| ||||||||||
| Observations | 694 | 612 | 694 | 612 | 694 | 612 | 694 | 612 | 694 | 612 |
p<0.01,
p<0.05,
p<0.1;
Column 1 for each health outcome includes fully outdoor cooking, and Column 2 excludes fully outdoor cooking.
The referent categories for dwelling type and kitchen floor are: single house and beaten earth, respectively. For cooking location, fully outdoor cooking and partially outdoor cooking are the referent categories in Models 1 and 2 of each symptom, respectively.
Stove type controlled for as a determinant of HAP exposure.
Household-level characteristics controlled for include: log of per capita total expenditure in the past 4 weeks (in RWF), household size, and per capita weekly charcoal use (in kg).
Child characteristics controlled for include: age (in months), sex, and health card availability. Main respondent characteristics controlled for include: age, sex and education level.
Compared to children in households with beaten earth floor in cooking areas, those in households with clay tiled floors have higher likelihood (weak significance) of experiencing respiratory infection. In the sub-sample of households not cooking fully outdoors, cemented cooking area floors have a weak protective effect on children’s respiratory infection symptom, relative to earth floors; there is a significant positive association between gap in walls and ceiling in cooking areas and difficulty breathing. While there is a strong positive association between number of windows and respiratory infection, there is a very strong negative association between cooking area ventilation holes and illness with cough, difficulty breathing and fever.
We find a weak positive association between distance to any road and prevalence of respiratory infection in the full sample of under-fives, but a strong positive association in the truncated sample of under-fives in households that do not cook fully outdoors. In the sub-sample, tree cover has a strong positive association with prevalence of respiratory infection and difficulty breathing but weak positive association with prevalence of dry eyes.
On including an objective measure of HAP exposure (24-hour average CO concentration in ppm) of the primary caregiver, to examine its relationship with child health symptoms (Table 3), we find strong positive associations between log of caregiver’s daily average CO concentration, and difficulty breathing and dry eyes. Contrary to what we would expect, in the sub-sample, presence of an active chimney in the cooking area, significantly increases children’s likelihood of experiencing respiratory infection. Distance to the nearest road significantly increases children’s likelihood of experiencing all HAP-related symptoms except illness with cough. Tree cover has strong positive associations with respiratory infection and difficulty breathing. Similar to the model without average CO concentration, the significance of the associations between child health symptoms, and dwelling type, cooking location, kitchen floor material, gap between walls and ceiling in the cooking area, and presence of ventilation holes persist.
Table 3.
Association between microenvironment, environmental and CO exposures & under-fives’ health symptoms
| HAP-related | Other | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Dependent variables | Respiratory infection‡ | Illness with cough‡ | Difficulty breathing‡ | Dry eyes‡ | Fever‡ | |||||
| Explanatory variables | ||||||||||
| Pollutant exposure | ||||||||||
| Log of daily average CO concentration of caregiver (in ppm) | 0.11 | 0.22 | 0.16 | 0.24 | 0.40*** | 0.48*** | 0.36** | 0.36* | −0.08 | −0.11 |
| (0.19) | (0.25) | (0.13) | (0.15) | (0.15) | (0.18) | (0.17) | (0.19) | (0.15) | (0.17) | |
| Housing structure | ||||||||||
| Dwelling type | ||||||||||
| Multiple house | 1.18 | 1.23 | −0.85 | −0.84 | −0.02 | −0.21 | 1.09 | 1.27 | 0.23 | 0.34 |
| (1.62) | (1.86) | (0.59) | (0.66) | (0.69) | (0.81) | (0.74) | (0.93) | (0.61) | (0.70) | |
| Group of multiple enclosed dwellings | 2.69**r | 2.93** r | −0.20 | −0.28 | 0.68 | 0.62 | 0.47 | 0.85 | 0.47 | 0.67 |
| (1.18) | (1.34) | (0.37) | (0.40) | (0.44) | (0.46) | (0.61) | (0.76) | (0.44) | (0.53) | |
| Group of single enclosed dwellings | 2.32* | 2.43* | −0.47 | −0.27 | −0.31 | −0.32 | 1.10 | 1.51* r | 1.03** r | 1.39** r |
| (1.23) | (1.43) | (0.45) | (0.49) | (0.56) | (0.57) | (0.70) | (0.82) | (0.51) | (0.58) | |
| Cooking location | ||||||||||
| Partially outdoors | 0.35 | −0.73 | −0.18 | −0.35 | −0.58 | |||||
| (0.77) | (0.47) | (0.61) | (0.62) | (0.57) | ||||||
| Kitchen structure outside dwellings | 1.72** | 0.99 | 0.48 | 1.11* r | 0.70 | 1.03 | 0.28 | 1.19 | 1.48*** | 2.66*** r |
| (0.71) | (1.32) | (0.49) | (0.61) | (0.67) | (0.78) | (0.68) | (0.89) | (0.56) | (0.71) | |
| Cooking inside dwelling | 0.84 | 0.12 | 0.35 | 1.43*** r | 0.36 | 0.89 | 0.10 | 0.77 | 0.72 | 2.29*** r |
| (0.67) | (0.82) | (0.40) | (0.50) | (0.52) | (0.60) | (0.52) | (0.61) | (0.45) | (0.56) | |
| Cooking area structure | ||||||||||
| Main floor material | ||||||||||
| Clay tiles, bricks and other materials | 1.07** r | 0.59 | 0.30 | 1.32* | −0.05 | 0.51 | 0.98 | 1.02 | 0.92* | 1.32* |
| (0.53) | (1.64) | (0.45) | (0.71) | (0.58) | (0.93) | (0.63) | (1.15) | (0.51) | (0.77) | |
| Cement | −0.97* | −1.54** r | −0.09 | 0.20 | −0.09 | 0.12 | −0.05 | −0.17 | −0.47 | −0.33 |
| (0.56) | (0.69) | (0.36) | (0.40) | (0.43) | (0.47) | (0.54) | (0.56) | (0.37) | (0.42) | |
| Kitchen roof | −0.38 | 1.36* | 0.53 | −0.27 | 0.54 | |||||
| (2.38) | (0.76) | (1.06) | (1.50) | (0.87) | ||||||
| Gap between walls and ceiling | 1.29** | 0.78** r | 0.77** r | 0.05 | 0.28 | |||||
| (0.54) | (0.35) | (0.38) | (0.48) | (0.44) | ||||||
| Number of windows | 0.53 | −0.23 | −0.14 | −0.03 | −0.47 | |||||
| (0.41) | (0.25) | (0.27) | (0.32) | (0.29) | ||||||
| Ventilation holes | −0.65 | −1.01*** r | −0.79** r | −0.37 | −1.31*** r | |||||
| (0.44) | (0.30) | (0.32) | (0.37) | (0.32) | ||||||
| Presence of active chimney | 1.81** | 0.31 | 1.14 | −0.56 | −0.74 | |||||
| (0.70) | (0.80) | (0.76) | (1.06) | (0.80) | ||||||
| Environmental exposure | ||||||||||
| Distance to nearest road (in meters) | 0.06** r | 0.08*** r | 0.01 | 0.01 | 0.04** | 0.04** | 0.04* | 0.04** | −0.00 | −0.02 |
| (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Tree cover (%) | 0.24*** r | 0.35*** r | 0.12* | 0.11 | 0.30*** r | 0.37*** r | 0.01 | 0.08 | -0.13 | −0.19 |
| (0.09) | (0.11) | (0.06) | (0.08) | (0.07) | (0.09) | (0.07) | (0.10) | (0.10) | (0.13) | |
| Constant | −12.57*** | −11.75** | 2.67 | 2.18 | −2.36 | −1.88 | −6.53* | −9.76*** | 1.49 | −0.95 |
| (4.78) | (5.16) | (2.57) | (3.10) | (3.11) | (3.66) | (3.53) | (3.69) | (2.64) | (3.24) | |
|
| ||||||||||
| Observations | 367 | 321 | 367 | 321 | 367 | 321 | 367 | 321 | 367 | 321 |
p<0.01,
p<0.05,
p<0.1;
Column 1 for each health outcome includes fully outdoor cooking, and Column 2 excludes fully outdoor cooking.
Coefficients marked ‘r’ are robust in the alternate specification without log of daily average CO concentration of the caregiver.
The referent categories for dwelling type and kitchen floor are: single house and beaten earth, respectively. For cooking location, fully outdoor cooking and partially outdoor cooking are the referent categories in Models 1 and 2 of each symptom, respectively.
Stove type controlled for as a determinant of HAP exposure.
Household-level characteristics controlled for include: log of per capita total expenditure in the past 4 weeks (in RWF), household size, and per capita weekly charcoal consumption (in kg).
Child characteristics controlled for include: age (in months) and sex. Caregiver characteristic controlled for: perception about negative health impacts from traditional cooking practices.
Discussion and Conclusion
The importance of studying the association between housing structure and neighborhood environment is two-fold. First, the results have pertinent implications for policy-makers as they consider infrastructure-related interventions to reduce HAP exposure, in conjunction with promoting improved access to modern household energy services. Second, in exploring the role of the neighborhood on human health in the context of HAP, there is potential for community-level interventions.
We find that (a) residing in agglomerated dwelling structures, (b) cooking indoors, (c) presence of a gap between walls and ceiling in the cooking area, and (d) more tree cover significantly increase children under-five’s probability of experiencing health symptoms in the short-term (2 weeks) recall period. On the other hand, children residing in households with (a) cooking area ventilation holes and (b) cemented floors in the cooking area are significantly less likely to experience many health symptoms.
Our finding that cement floors have a protective effect on child health (respiratory infection) is similar to Cattaneo et al’s (2008) finding of reduction in intestinal parasites that are not treatable with common deworming drugs found in developing countries, among low-income urban Mexican households. Consistent with the urban planning and public health literature on housing improvements being critical to health (Northridge et al 2003), housing improvements such as cemented floors to improve child health, is a key policy recommendation. Our finding that cooking indoors, relative to outdoor cooking, significantly increases children’s likelihood of experiencing HAP-related illnesses, is similar to results from Langbien (2017) that outdoor cooking significantly reduces respiratory diseases among children aged 0–4 years, in 30 developing countries. A second policy recommendation would be to promote outdoor (full or partial) cooking, during favorable seasons, in alignment with households’ existing cooking practices.
Contrary to Bruce et al’s (2004) findings, we find that number of windows have a significant positive association with respiratory infection. Our finding that number of windows and ventilation holes have opposing associations with the likelihood of children experiencing health symptoms may be due to differences in size of these structures, and frequency of keeping windows open. It is likely that in some households, though there is an active chimney, owing to poor house construction (lack of concrete material), smoke removed from the chimney may be circulating back into the house owing to porous walls. Echoing Langbien (2017) we argue for the need to study pollutant exposure and its impact on human health under various ventilation conditions and cooking locations.
Our results of a positive relationship between distance to any road and prevalence of health symptoms in most models, is contrary to Venn et al’s (2001) findings that increasing proximity to a main road increases the risk of wheezing. It is likely that proximity to roads may not be a good proxy for traffic-related air pollutants. One explanation for the counter-intuitive strong positive relationship between tree cover in the area surrounding households and prevalence of health symptoms, contrary to Nowak et al’s (2014) findings from the United States, could be insufficient air ventilation and low pollutant dispersal owing to scattered non-dense vegetation (Wang et al 2014). Our results correspond to Musafiri et al’s (2011) finding that allergens (house dust mite and grass pollen mix) are a risk factor for asthma in rural and urban Rwanda. With changing climate and rising CO2 emissions, pollen production and correspondingly allergenicity may increase (Ziska and Beggs 2012). In our geographically small and densely populated study area, it is also likely that tree cover does little to reduce HAP exposure, particularly CO.
Our study is not without its limitations. First, the cross-sectional nature of our analysis does not allow for making causal claims. Relatedly, we are unable to control for children’s poor health endowment. Second, owing to binary caregiver-reported health symptoms, and small number of data points for exposure concentrations, we are unable to analyze the spatial autocorrelation in our sample. Third, though CO concentration coefficients are significant for some health symptoms, it is likely that caregiver’s CO exposure does not fully capture child’s CO exposure. Fourth, though there is no multicollinearity in our regression models, cooking area dimensions would have better characterized well-ventilated structures.
Our analysis highlights the importance of understanding the relationship between structural factors about dwelling and cooking area, and child health. In areas of high HAP exposure as Rwanda, where there is near universal dependence on solid fuels for cooking, and provision of improved energy services is in its nascent stages, improvements in the microenvironment of the vulnerable population of under-fives, is central to reducing HAP-related health symptom prevalence. Housing structure improvements such as cemented kitchen floors and behavioral strategies of encouraging outdoor cooking where possible and favorable, subject to seasonality, are suggestive policy interventions governments could undertake to reduce prevalence of negative health outcomes.
Acknowledgments
This impact evaluation is led and executed by The University of North Carolina at Chapel Hill, United States (UNC-CH). The baseline survey was funded by the National Institutes of Health/National Institute of Environmental Health Sciences (R01ES023861: The Health and Poverty Effects of a Large-scale Cookstove Initiative in Rwanda) and conducted in collaboration with The Access Project, Rwanda. This research has been reviewed and approved by the Institutional Review Board at UNC-CH, the Rwanda National Ethics Committee, and the National Institute of Statistics Rwanda. We are grateful to the Carolina Population Center (P2C HD050924) at UNC-CH for general support. We would also like to acknowledge the excellent geospatial data assistance provided by Varun Goel. Map data copyrighted OpenStreetMap contributors and available from https://www.openstreetmap.org. We thank two anonymous referees for their helpful comments.
Footnotes
Cells are the second-lowest level of administration in Rwanda, above village. The political-administrative units above cell are sector, district and province.
The CO data loggers record readings from 0 to 1000 ppm in 0.5 ppm increments and have a reported accuracy of ±7 ppm. All of these loggers were calibrated before and after the three-month field sampling period. Calibration involved placing the CO data loggers in a sealed chamber that had a small mixing fan, an inlet line for a calibration gas (200 ppm CO in air), and an outlet line to a fume hood. A correction factor was developed for each data logger based on its average maximum readings relative to the calibration gas before and after the field sampling period.
Though we have data on distance to tarmac road and dust road, we use ‘distance to any road’ instead, as majority households (98%) are closer to an unpaved road than a paved road (see Figure 1). As of September 2017, i.e. 2 years after this data were collected, all roads in the study area were tarred. statistically significant differences in symptom prevalence among younger (0–23 months) and older (24–59 months) under-fives4, we do not analyze these age groups separately.
We use the WHO and CDC classification of growth curves for younger and older children, respectively (https://www.cdc.gov/mmWr/preview/mmwrhtml/rr5909a1.htm).
Group of single enclosed dwellings are single households within a shared, walled compound. Group of multiple enclosed dwellings include multiple housing structures within a common, walled compound. These classifications were taken from the Rwanda Integrated Household Living Conditions Survey administered by the National Institute of Statistics of Rwanda.
References
- Albalak R, Bruce N, McCracken JP, Smith KR, De Gallardo T. Indoor respirable particulate matter concentrations from an open fire, improved cookstove, and LPG/open fire combination in a rural Guatemalan community. Environmental Science & Technology. 2001;35(13):2650–2655. doi: 10.1021/es001940m. [DOI] [PubMed] [Google Scholar]
- Balakrishnan K, Parikh J, Sankar S, Padmavathi R, Srividya K, Venugopal V, Prasad S, Pandey VL. Daily average exposures to respirable particulate matter from combustion of biomass fuels in rural households of southern India. Environmental Health Perspectives. 2002;110(11):1069. doi: 10.1289/ehp.021101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balietti A, Datta S. The impact of indoor solid fuel use on the stunting of Indian children. [Accessed on September 28, 2017];Working Paper. 2017 Available at: http://www.ancabalietti.net/wp-content/uploads/2017/04/Datta_Balietti_March2017.pdf.
- Bonjour S, Adair-Rohani H, Wolf J, Bruce NG, Mehta S, Prüss-Ustün A, Lahiff M, Rehfuess EA, Mishra V, Smith KR. Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environmental Health Perspectives (Online) 2015;121(7):784. doi: 10.1289/ehp.1205987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce N, McCracken J, Albalak R, Schei M, Smith KR, Lopez V, West C. Impact of improved stoves, house construction and child location on levels of indoor air pollution exposure in young Guatemalan children. Journal of Exposure Science and Environmental Epidemiology. 2004;14:S26–S33. doi: 10.1038/sj.jea.7500355. [DOI] [PubMed] [Google Scholar]
- Cattaneo MD, Galiani S, Gertler PJ, Martinez S, Titiunik R. Housing, health, and happiness. American Economic Journal: Economic Policy. 2009;1(1):75–105. [Google Scholar]
- Chafe ZA, Brauer M, Klimont Z, Van Dingenen R, Mehta S, Rao S, Riahi K, Dentener F, Smith KR. Household cooking with solid fuels contributes to ambient PM2. 5 air pollution and the burden of disease. Environmental Health Perspectives. 2014;122(12):1314. doi: 10.1289/ehp.1206340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury Z, Le LT, Masud AA, Chang KC, Alauddin M, Hossain M, Zakaria ABM, Hopke PK. Quantification of indoor air pollution from using cookstoves and estimation of its health effects on adult women in northwest Bangladesh. Aerosol Air Qual Res. 2012;12(4):463–475. [Google Scholar]
- Clark ML, Peel JL, Balakrishnan K, Breysse PN, Chillrud SN, Naeher LP, Rodes CE, Vette AF, Balbus JM. Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environmental Health Perspectives. 2013;121(10):1120. doi: 10.1289/ehp.1206429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das I, Jagger P, Yeatts K. Biomass cooking fuels and health outcomes for women in Malawi. Ecohealth. 2017;14(1):7–19. doi: 10.1007/s10393-016-1190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2008;86(5):390–398C. doi: 10.2471/BLT.07.044529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Alliance for Clean Cookstoves. [Accessed on February 7, 2017];Country Profiles. 2016 Available at: http://cleancookstoves.org/country-profiles/32-rwanda.html.
- Global Alliance for Clean Cookstoves. 2017 Progress Report. Driving Demand. [Accessed on December 21, 2017];Delivering Impact. 2017 Available at: http://cleancookstoves.org/binary-data/RESOURCE/file/000/000/536-1.pdf.
- GBD 2016 Causes of Death Collaborators. Global, regional and national age-sex specific mortality for 264 causes of death 1980–2016: systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, Oldenwening M, Smit HA, Brunekreef B. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. American Journal of Respiratory and Critical Care Medicine. 2010;181(6):596–603. doi: 10.1164/rccm.200906-0858OC. [DOI] [PubMed] [Google Scholar]
- Gordon SB, et al. Respiratory risks from household air pollution in low and middle income countries. The Lancet Respiratory Medicine. 2014;2(10):823–860. doi: 10.1016/S2213-2600(14)70168-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabow K, Still D, Bentson S. Test kitchen studies of indoor air pollution from biomass cookstoves. Energy for Sustainable Development. 2013;17(5):458–462. [Google Scholar]
- Harkness S, Super CM. The developmental niche: A theoretical framework for analyzing the household production of health. Social Science & Medicine. 1994;38(2):217–226. doi: 10.1016/0277-9536(94)90391-3. [DOI] [PubMed] [Google Scholar]
- Hoek G, Beelen R, De Hoogh K, Vienneau D, Gulliver J, Fischer P, Briggs D. A review of land-use regression models to assess spatial variation of outdoor air pollution. Atmospheric Environment. 2008;42(33):7561–7578. [Google Scholar]
- Jagger P, Shively G. Land use change, fuel use and respiratory health in Uganda. Energy Policy. 2014;67:713–726. doi: 10.1016/j.enpol.2013.11.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyu HH, Georgiades K, Boyle MH. Maternal smoking, biofuel smoke exposure and child height-for-age in seven developing countries. International Journal of Epidemiology. 2009;38(5):1342–1350. doi: 10.1093/ije/dyp253. [DOI] [PubMed] [Google Scholar]
- Langbein J. Firewood, smoke and respiratory diseases in developing countries—The neglected role of outdoor cooking. PloS One. 2017;12(6):e0178631. doi: 10.1371/journal.pone.0178631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan PJ, et al. The Lancet Commission on pollution and health. The Lancet. 2017 doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, Gauderman J. Childhood incident asthma and traffic-related air pollution at home and school. Environmental Health Perspectives. 2010;118(7):1021. doi: 10.1289/ehp.0901232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald AG, Bealey WJ, Fowler D, Dragosits U, Skiba U, Smith RI, Donovan RG, Brett HE, Hewitt CN, Nemitz E. Quantifying the effect of urban tree planting on concentrations and depositions of PM 10 in two UK conurbations. Atmospheric Environment. 2007;41(38):8455–8467. [Google Scholar]
- Mishra V, Retherford RD. Does biofuel smoke contribute to anaemia and stunting in early childhood? International Journal of Epidemiology. 2006;36(1):117–129. doi: 10.1093/ije/dyl234. [DOI] [PubMed] [Google Scholar]
- Musafiri S, Van Meerbeeck J, Musango L, Brusselle G, Joos G, Seminega B, Rutayisire C. Prevalence of atopy, asthma and COPD in an urban and a rural area of an African country. Respiratory Medicine. 2011;105(11):1596–1605. doi: 10.1016/j.rmed.2011.06.013. [DOI] [PubMed] [Google Scholar]
- Northridge ME, Sclar ED, Biswas P. Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. Journal of Urban Health. 2003;80(4):556–568. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. Journal of Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak DJ, Crane DE, Stevens JC. Air pollution removal by urban trees and shrubs in the United States. Urban Forestry & Urban Greening. 2006;4(3):115–123. [Google Scholar]
- Nowak DJ, Hirabayashi S, Bodine A, Greenfield E. Tree and forest effects on air quality and human health in the United States. Environmental Pollution. 2014;193:119–129. doi: 10.1016/j.envpol.2014.05.028. [DOI] [PubMed] [Google Scholar]
- OpenStreetMap contributors. Planet dump [Data file from $date of database dump$] 2015 Retrieved from https://planet.openstreetmap.org.
- Pitt MM, Rosenzweig MR, Hassan MN. Sharing the burden of disease: Gender, the household division of labor and the health effects of indoor air pollution in Bangladesh and India. Stanford Institute for Theoretical Economics Summer Workshop.2006. Jun, [Google Scholar]
- Rosa G, Majorin F, Boisson S, Barstow C, Johnson M, Kirby M, Ngabo F, Thomas E, Clasen T. Assessing the impact of water filters and improved cook stoves on drinking water quality and household air pollution: a randomized controlled trial in Rwanda. PLoS One. 2014;9(3):e91011. doi: 10.1371/journal.pone.0091011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruth M, Maggio J, Whelan K, DeYoung M, May J, Peterson A, Paterson K. Kitchen 2.0: Design guidance for healthier cooking environments. International Journal for Service Learning in Engineering, Humanitarian Engineering and Social Entrepreneurship. 2014:151–169. [Google Scholar]
- Sexton JO, Song X-P, Feng M, Noojipady P, Anand A, Huang C, Kim D-H, Collins KM, Channan S, DiMiceli C, Townshend JRG. Global, 30-m resolution continuous fields of tree cover: Landsat-based rescaling of MODIS Vegetation Continuous Fields with lidar-based estimates of error. International Journal of Digital Earth. 2013 doi: 10.1080/17538947.2013.786146. 130321031236007. [DOI] [Google Scholar]
- Smith KR, et al. Millions dead: how do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annual Review of Public Health. 2014;35:185–206. doi: 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- United Nations Statistics Division. [Accessed on February 7, 2017];2017 Available at: http://data.un.org/CountryProfile.aspx?crName=RWANDA.
- Venn AJ, Lewis SA, Cooper M, Hubbard R, Britton J. Living near a main road and the risk of wheezing illness in children. American Journal of Respiratory and Critical Care Medicine. 2001;164(12):2177–2180. doi: 10.1164/ajrccm.164.12.2106126. [DOI] [PubMed] [Google Scholar]
- Wang Y, Bakker F, De Groot R, Wörtche H. Effect of ecosystem services provided by urban green infrastructure on indoor environment: A literature review. Building and Environment. 2014;77:88–100. [Google Scholar]
- Wolff CG, Schroeder DG, Young MW. Effect of improved housing on illness in children under 5 years old in northern Malawi: cross sectional study. BMJ. 2001;322(7296):1209–1212. doi: 10.1136/bmj.322.7296.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization: Geneva. [Accessed on April 12, 2016];Success factors for women’s and children’s health: Rwanda. 2015 Available from: http://www.who.int/pmnch/knowledge/publications/rwanda_country_report.pdf.
- World Health Organization: Geneva. [Accessed on September 20, 2016];Pneumonia Factsheet. 2016 Available from: http://www.who.int/mediacentre/factsheets/fs331/en/
- Wright RJ, Fisher EB. Putting asthma into context: community influences on risk, behavior, and intervention. Neighborhoods and Health. 2003:233–264. [Google Scholar]
- Yadama GN, Peipert J, Sahu M, Biswas P, Dyda V. Social, economic, and resource predictors of variability in household air pollution from cookstove emissions. PloS One. 2012;7(10):e46381. doi: 10.1371/journal.pone.0046381. [DOI] [PMC free article] [PubMed] [Google Scholar]