Abstract
Background
Physician and nurses have worked together for generations; however, their language and training are vastly different; comparing and contrasting their work and their joint impact on patient outcomes is difficult in light of this difference. At the same time, the EHR only includes the physician perspective via the physician-authored discharge summary, but not nurse documentation. Prior research in this area has focused on collaboration and the usage of similar terminology.
Objective
The objective of the study is to gain insight into interprofessional care by developing a computational metric to identify similarities, related concepts and differences in physician and nurse work.
Methods
58 physician discharge summaries and the corresponding nurse plans of care were transformed into Unified Medical Language System (UMLS) Concept Unique Identifiers (CUIs). MedLEE, a Natural Language Processing (NLP) program, extracted “physician terms” from free-text physician summaries. The nursing plans of care were constructed using the HANDS© nursing documentation software. HANDS© utilizes structured terminologies: nursing diagnosis (NANDA-I), outcomes (NOC), and interventions (NIC) to create “nursing terms”. The physician’s and nurse’s terms were compared using the UMLS network for relatedness, overlaying the physician and nurse terms for comparison. Our overarching goal is to provide insight into the care, by innovatively applying graph algorithms to the UMLS network. We reveal the relationships between the care provided by each professional that is specific to the patient level.
Results
We found that only 26% of patients had synonyms (identical UMLS CUIs) between the two professions’ documentation. On average, physicians’ discharge summaries contain 27 terms and nurses’ documentation, 18. Traversing the UMLS network, we found an average of 4 terms related (distance less than 2) between the professions, leaving most concepts as unrelated between nurse and physician care.
Conclusion
Our hypothesis that physician’s and nurse’s practice domains are markedly different is supported by the preliminary, quantitative evidence we found. Leveraging the UMLS network and graph traversal algorithms, allows us to compare and contrast nursing and physician care on a single patient, enabling a more complete picture of patient care. We can differentiate professional contributions to patient outcomes and related and divergent concepts by each profession.
Keywords: UMLS, Physician documentation, Nursing documentation, Professional discontinuity, Health informatics
1. Introduction
Physicians and nurses are an integral care dyad for providing care and treatment to hospitalized patients [1,2]. Their roles are interdependent going back to ancient Hindu scripture [3]. Hospital physicians diagnose and plan medical treatments. Nurses take responsibility for the hands-on-care while exercising independent judgment, intervening, and continuously re-evaluating patients’ health status and response to medical treatments [4]. Given this interdependence, collaboration and synergy (the active assessment or provision of care for a patient health problem by both professions) is clearly important and as nurse–physician communication has been linked to improved patient outcomes [5–7]. Poor MD-RN communication is a common cause of adverse events [8].
1.1. Background
The concept of records for patients’ hospital care as a means of communication was first introduced in 1910 by Dr. Ernest Codman [9]. He noted a poor quality of care and absence of documentation, and asserted that all hospitalized patients have records of their histories, physical exams, medications and laboratory tests [9]. Physician documentations that met this standard, started out as case reports for didactic learning, but evolved to a loose narrative that was further constrained as concern for legal ramifications grew with additional reimbursement requirements [10–12]. Karolinska Hospital was one of the first hospitals to computerize the physician problem-oriented medical record [13,14]. However, physician discharge summaries do not reflect nursing care [15].
Earlier than physician standards, Florence Nightingale asserted the vital role of nurses in “recording” their condition for improving patient health [2]. Despite Nightingale’s assertion, nursing documentation was outside the patient’s medical records and written on a “Kardex” in the 1950s [16]. But its value was recognized around the world [17] as well as its complexities [18]. Nursing documentation has used multiple frameworks including unstructured narratives, structured narratives (e.g. SOAP notes) clinical pathways, and problem-based approaches [18,19]. Beginning in the 1970s, nurse researchers developed standardized terminologies for nursing diagnoses, interventions and outcomes [20,21]. Tastan and colleagues in a review noted that the NANDA-I (nursing diagnosis), NOC (patient outcomes), and NIC (nursing interventions) terminologies have the most empirical support (> 70% of studies) [21]. During this nurse terminology development, an unequivocal definition of nurse sensitive patient outcomes was studied [22]. These terminologies can represent nursing care [4,23].
While physician and nurse documentation have varied historical norms and frameworks, both are included in modern electronic health records. Given the asynchronous work of hospitals’ nurses and physicians [24], the patient’s health record is integral in planning and communicating. There has been long standing research on nurse physician communication and collaboration across the world [25–27], but there are important limitations of this research. Many are qualitative exploration [28–30] or surveys based on perceptions [27,31,32] that are often disparate between physicians and nurses. These studies focus on process and attitudes of providers instead patient outcomes and patient details [25,31]. Prior interprofessional quantitative work focused on higher level physician concepts (Diagnosis Related Groups) of documentation between professions [33]. Here we propose a more detailed method to compute a quantitative measure from clinical care documentation from both nurses and physicians that can link to patient specific outcomes. All of the care in the hospital is not documented in the physician discharge summary nor is all of the care documented in the nursing documentation. By understanding how the terms from the two documentation standards are similar and related, we hypothesize we can obtain a better understanding about where the intersection of care occurs to measure the individual and combined contributions of both professions. The study objective is to gain insight into inter-professional care by developing a computational metric to identify similarities, related concepts and differences in physician and nurse work. The computational metric works by applying a graph traversal algorithms that leverage the existing Unified Medical Language System (UMLS) network to study the synergistic nature of care.
2. Materials and method
2.1. Design
We used a non-experimental correlational design. This research project was approved by the University of Illinois Institutional Review Board as exempt (#2012-0823).
2.2. Setting
Data was collected from existing electronic health record (EHR) (Cerner Millennium) data from a single urban academic hospital.
2.3. Data sources
We used documentation from physicians and nurses for 58 de-identified unique patients discharged with a medical diagnosis of heart failure from a random sample of 8 year of discharges.
2.3.1. Physician discharge summaries
Previously, we processed eight years of physician summaries via the Medical Language Extraction and Encoding System (MedLEE) system [34,35], a Natural Language Processing (NLP) system. The NLP system produces a semi-structured output where concepts are mapped to the corresponding CUI (concept unique identifier) terms from the UMLS metathesaurus, a “common nomenclature” [36–38]. A random sample of 58 de-identified physician discharge summaries was selected. Summaries were created by physicians as free text or smart templates with additional free text. The entire dataset of physician summaries is called, “Physician Discharge Summaries”. The data derived via NLP, is called “Physician terms” (Fig. 1). The physician discharge summary includes several sections: history of present illness, medications list, and follow up appointments. We used the section labeled ‘hospital course’ as it relates most to the hospital care.
Fig. 1.
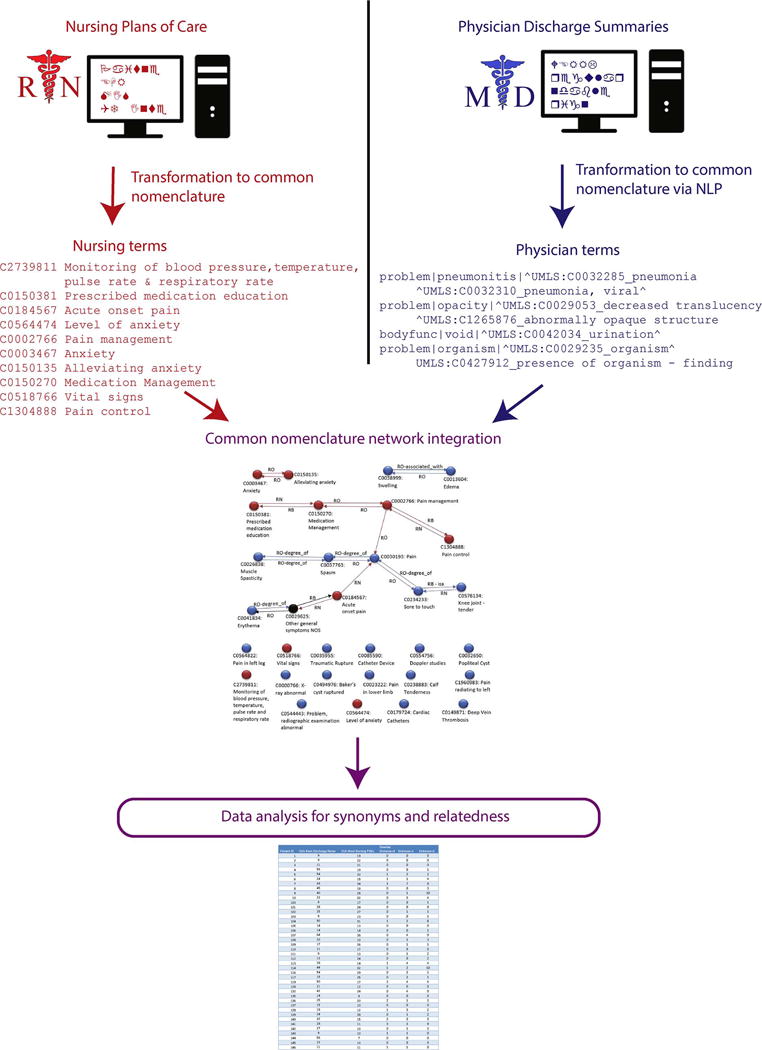
Overview of data analysis steps for the project. Physician and nurse documentation are transformed to compare them for synonymity and relatedness.
2.3.2. Nursing plans-of-care
For this study in a hospital with minimal nursing documentation, two nursing informatics students created rich nursing plans-of-care (POCs), with the HANDS© software, by retrieving cases similar to that described in the physician discharge summary from 40,661 HANDS© POCs from a prior study in four Midwestern hospitals [23]. Also guiding the creation was patient’s numeric data (e.g. Vital signs) and patient’s brief free nursing free text documentation (discharge teaching complete) extracted from the EHR.
HANDS© is a nursing plan-of-care documentation software that represents nursing diagnoses, interventions, and outcomes respectively with NANDA-I, NIC, and NOC [20,39,40]. Nurses update the POCs at each shift change for non-flow sheet information (Fig. 2). A single hospitalization typically results in multiple POCs.
Fig. 2.
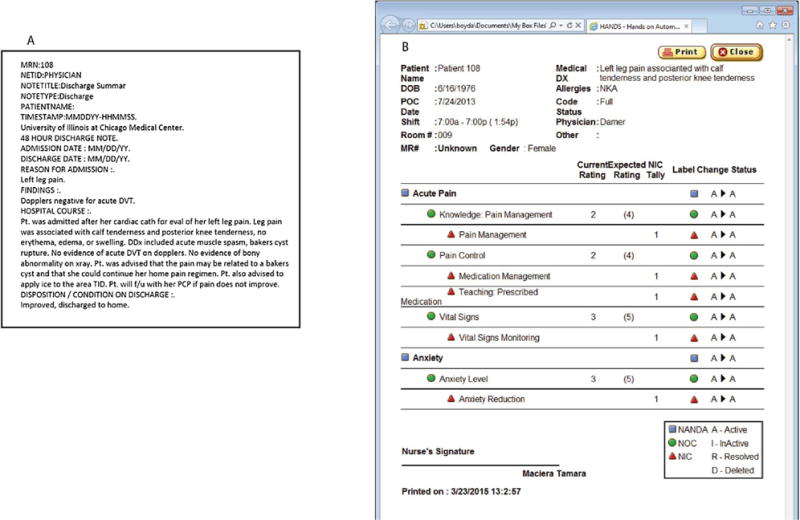
Excerpts from a physician discharge summary and a nurse plan of care.
The student’s POCs were validated by two nurse authors with in depth knowledge of HANDS and nursing terminologies. Since the NANDA-I, NIC, and NOC have been incorporated into UMLS (Fig. 1), we were then able to leverage UMLS’s existing mapping to create a set of “Nursing terms”, identified by their CUIs from UMLS.
2.4. Analysis
The UMLS network enables relationships between the professions to be computed, visualized and analyzed. We compute both “synonymity” and “relatedness” to measure synergy.
2.4.1. Synonyms
Synonyms represent exact matches between the nursing and physician controlled terms. A comparison per patient of the individual terms in the physician and nursing terms are examined for an exact match. For example in subject 7, the physician documented Dehydration, MedLEE mapped the term to UMLS C0011175: Dehydration. The nurse used the nursing terminology “Deficient Fluid Volume”, which is NANDA-I code 00027. The nursing term maps to the same UMLS term C0011175. Since the UMLS terms are identical, the two concepts are labeled synonyms, or atoms in UMLS terminology.
2.4.2. Relatedness
Relatedness examines the non-identical relationship of terms. The common nomenclature (UMLS) links the terms together. A connection between two concepts is called a relationship (see Fig. 3). The relationships come from a variety of validated sources and are bidirectional [41]. If the relationship links between the terms are from a source vocabulary within the UMLS the source is documented [41]. If relationship links are from the UMLS metathesaurus or another service, the origin of the link is documented in the database. For example in Fig. 3, Alleviating anxiety is “otherwise” related to Anxiety (link RO), because it was created by the Metathesaurus at NLM. Other relationship links can be from any of the over 400 taxonomies and ontologies.
Fig. 3.
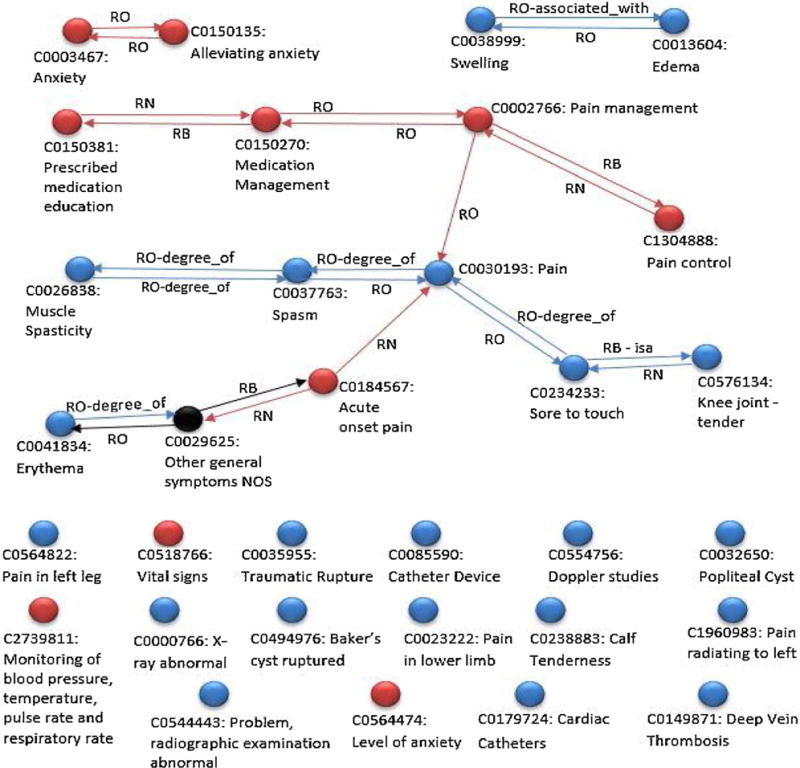
Sample network for research subject 108. Blue circles = MD terms. Red circles = nursing terms. Black circles = intermediate terms that connect the physician and nursing terms. Line = link (relationship) provided by the UMLS network.
To reveal related concepts within a patient record, we construct a concept graph (Fig. 3). The inputs are a patient’s nursing terms and physician terms; we link the two by querying the UMLS Terminology Server. For example, ‘Pain’ (C0030193) was documented by the physician; however, the nurse documents ‘Pain Management’ (NIC 1400). The NIC code maps to the common nomenclature C0002766 ‘Pain Management’. ‘Pain’ (C0030193) and ‘Pain management’ (C0002766) are linked and related. We count distances in terms of relationships traversed; hence, the two terms are at distance 1, since one path links them.
At distance 2, physician terms and nursing terms may be linked through other concepts. For example, ‘Erythema’ (C0041834) was documented by the physician, whereas the nurse documented ‘Acute Pain’ (NANDA-I 00132). The NANDA-I code maps to the UMLS C0184567 ‘Acute Onset Pain’. Both concepts are linked to ‘Other General Symptoms NOS’ (C0029625). While ‘Other General Symptoms NOS’ was not documented, the concept links the two terms.
In UMLS, 50% of terms (more than 1 million) are connected within a distance of 6 [42]. Deciding how many links to traverse in the network, is an empirical question; we have set the threshold to 2 to limit search time on UMLS servers. However, this is an adjustable parameter in the algorithm that traverses the UMLS network (see Fig. 4) We seed (start) the graph with an initial set of nursing terms, because on average there are fewer nursing terms [18] than physician terms [27]. The concept graph contains, for each concept c, a list of concepts related to it, with the distance between each pair of concepts.
Fig. 4.
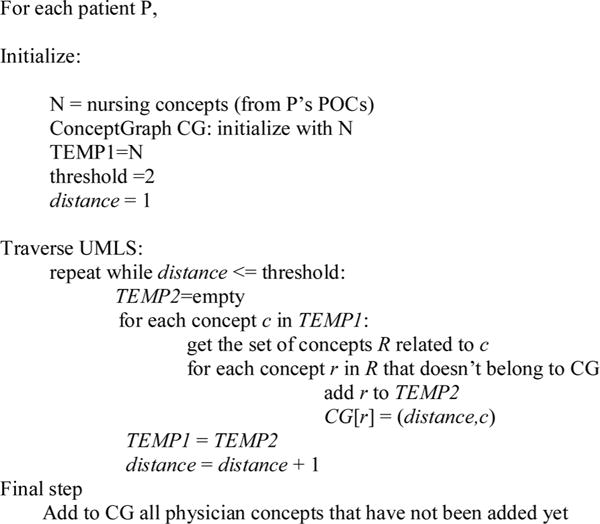
Algorithm to calculate the distance between terms.
At the end, for each concept reachable from the nursing concepts, the ConceptGraph (CG) in Fig. 4, records the shortest distance from a nursing concept, and the predecessor along that shortest path; these may or may not be physician concepts. The physician concepts that were not found by the algorithm are added as separate nodes (see isolated blue nodes in Fig. 3). The unconnected red nodes in Fig. 3 represent nursing concepts; these are the nursing nodes from which no connection has been found. Some physician and nursing terms are seen to be isolated because they either do not have any relation with other terms or are related through intermediate terms at distance greater than 2.
2.4.3. Comparison
After creating the graphs for each hospitalization, the number of terms at a specific distance were compared between patients (see online table 2).
Using a Bayesian Calculator, a confidence interval was calculated for the number of patients with synonyms, where X is the total number of cases and A is the number of cases with synonyms.
2.4.4. Manual inspection
A total of 10 of the patients’ records were selected and the “Hospital Course” section of the physician note and the HANDS notes were compared by one of the authors, to identify any content that this person thought was related (SA). The author who inspected the synonyms was not a health professional, as to limit bias of professional training in the results (see Table 1).
Table 1.
Table of related terms per patient for physician and nursing terms comparing human and UMLS curated lists for 10 patients.
| Patient ID | Human curated | UMLS linked terms | Absolute difference |
|---|---|---|---|
| 100 | 1 | 1 | 0 |
| 101 | 3 | 0 | 3 |
| 102 | 7 | 2 | 5 |
| 103 | 3 | 1 | 2 |
| 105 | 1 | 0 | 1 |
| 106 | 2 | 1 | 1 |
| 108 | 3 | 4 | 1 |
| 109 | 6 | 2 | 4 |
| 112 | 1 | 2 | 1 |
| 113 | 8 | 9 | 1 |
3. Results
The physician discharge summaries processed by NLP generated an average of 87 terms per summary. Of these 87 terms, an average of 27 terms were from the hospital course section, and were used as physician terms. A total of 945 distinct CUIs are in physician terms (see online table 2). The nursing POCs created within HANDS generated 18 terms on average. A total of 304 nursing terms were used. For each individual patient, a concept graph was generated (see Fig. 3).
3.1. Synonyms
The average number of synonyms (terms used in both physician and nurse documentation) between the two professions per patient hospitalization is 0.4 terms. For 26% of patients, synonyms existed between physician and nurse documentation (see online table 2). Using a Bayesian Calculator with a 95% confidence interval the range is 16–38% of patients whose records would include synonyms.
3.2. Relatedness
At a distance 1, an average of 1.2 terms were calculated. A distance of 1 means that each concept is directly linked to a concept derived by the other profession. At a distance 2, the number of terms is 2.6. On average, only 4 terms per patient are linked (at distance 1 or 2) between professions.
3.3. Visual
A visual analysis of the patient level hospital graphs revealed individual physician and nurse terms that do not link via UMLS (namely, the concept graph consists of several components that are not connected one to the other). For example “Deep Vein Thrombosis” (C0149871), from the perspective of a health care professional would consider the concept related to “Swelling” (C0038999) and “Acute onset pain” (C0184567) but they are far enough in the UMLS ontology that the algorithm does not link them.
3.4. Human
Results of the human evaluation of related concepts are in Table 1. The largest difference between the algorithm and the human was Pt 102, with 2 and 7 respectively. The average absolute difference is 1.9.
4. Discussion
We were able to leverage existing knowledge sources (UMLS) to evaluate the differences and similarities between physician and nurse care to create a more unified patient perspective. Taking advantage of the existing UMLS network, we took a knowledge driven approach of the professional differences between nursing and physician care at an individual patient level compared to prior research [33]. The proposed methodology is generalizable to multiple nursing terminologies, physician documentation, and different systems of nomenclature. We have used common elements of an electronic health record to allow others to conduct similar analysis. Unlike previous studies that have relied upon human judgment for relatedness of terms [43], the algorithm we propose measures the differences between physician and nurses using nonhuman links. Prior work also focused on a conceptual definitions of “Nurse-Sensitive” Patient Outcomes [22], however our analysis results in some overlap in terms between physician and nurse documentation (Fig. 3) which causes the evaluation of patient outcomes to be more complex and interdisciplinary sensitive. The prior work by van Beek et al. used Diagnose Behandeling Combinaties (DBC) (Dutch Diagnosis Related Groups DRG variant) and compared to nursing minimum dataset using HOMALs, a principal component analysis for nominal variables [33]. DRGs transform the complete hospital stay to a single disease grouping, with only one term per hospital stay. van Beek used only 23 unique DRG’s across all patients studied as well as 38 unique nursing terms across all patients [33]. In our study, we extracted on 945 unique terms from the hospital course for physicians and 304 unique terms for the nurse documentation, a significant increase in detail with fewer patients. Another difference in the two analyses is van Beek’s use of HOMALS [33] compared to the use of UMLS, an external knowledge domain. Through the use of UMLS, all relationships/linkages can be traced to prior knowledge with UMLS for additional analysis, where HOMALS can reveal relationships but not explain why.
To illustrate the insights from the new method, consider the single patient 108 (see Fig. 3), which is representative of an average patient case. There are no synonyms, there are two terms at distance 1, and one term at distance 2. In Fig. 3, the physician concept Pain (C0030193) is at distance 1 away from the nursing concept of Acute Onset of Pain (C0184567). The terms are related and refer to similar concepts. The nursing concept Acute Onset of Pain (C0184567) is two links away (distance 2) from the physician concept Erythema (C0041434). The concepts are related. By highlighting the differences, a more comprehensive picture of the patient is possible. The related concepts help to highlight the potential synergy between the professionals. The method of searching the UMLS network is not new (UTS Semantic Network Browser is a common example), but highlighting the professional source of the terms and leveraging their relationships is new. The relationships within the UMLS, are generated both through the source terminologies, as well as UMLS and other services. While lack of linkage does not prove that no relationship exists, UMLS provides the largest linkages of diverse health terms open to researchers worldwide to evaluate the interprofessional linkages. This is quantitative evidence for the hypothesis that physicians and nurses focus on different aspects of patient care and need integration for a complete picture.
Future use of this method to measure potential synergist care, as evidenced by use of related terms, could be critical to improving care quality in the temporally demanding hospital. From a patient safety perspective, during a root cause analysis (an in-depth analysis of the factors contributing to an unsafe environment) examining the professions scope and treatment can provide new insight. Additionally, by focusing on aggregate data from the individual wards, floors, and hospitals, treatment patterns could emerge and best practice guidelines could emerge to improve the quality of care. Finally, in this era of evidence based medicine, specific nursing interventions delivered and measured may offer an explanation of why medical treatments are effective in some patients but not others.
4.1. Common nomenclature (UMLS)
While the analysis has revealed similarities and differences between the languages of physician and nurse, the comparison of the terminologies is reliant upon the connections provided by the common nomenclature (UMLS). The common nomenclature is a well-studied clinical terminology relationship generator and health domain taxonomy [36–38]. The common nomenclature would need to create a large number of new concepts to encompass the paradigm of nursing [44]. In the 1990s, the Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT)’s decided to include nursing terms, to account for the differences between the professions [45,46]. Evaluation of the nursing concepts in SNOMED continued for another decade [47,48]. Later research has evaluated the differences between nursing concepts within SNOMED-CT [49,50]. After years of work, nursing terminology was well integrated into the common nomenclature (UMLS).
The selection of the common nomenclature (UMLS) was deliberate. In considering networks, the common nomenclature (UMLS) is a highly connected network ideal for finding relatedness between professions. A different network, Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT) [51,52], has relationships designed as an a-cyclical tree, which would enable easy comparison between two terms but would increase the distance between any two terms. The full network of UMLS is more representative of the complex nature of biomedicine.
4.2. Communication impact
Research examining multi-professional languages is rare. In Sweden, Terner et al. examined the documentation headings of eight professions in an electronic health record [53]. Slightly greater than 50% of the physician report headings (symptoms, medication) were used by nurses, and vice versa [53]. The headings are different than the discrete concepts, limiting comparison between the professions and our work. Another study from Norway shows how the terminologies for the hospital nurse and hospital physician are different but does not try to combine them at the individual patient level [54].
We also found more differences than similarities with on average only 4 related terms per patient. This was quite surprising to us given the high acuity and number of patient problems today’s hospitalized patient is likely to have. One concern that arises with the lack of shared terms is whether physician and nurses understand the subtle differences between the terminologies they use.
One could argue that nurses and physicians should be forced to use a common set of terms. However, each profession has a diversity of concepts and purposes. Asking either profession to only use terms that another profession would need, limits the care and would be a detriment. Each profession needs to reflect their comprehensive contribution to care. In addition, nursing and physician documentation is meant to be a reflection of their clinical assessments and activities. Additional research on the differences and similarities in their documentation should yield important insights about patient outcomes and hospital processes.
4.3. Limitations
One limitation of our study is that the nurses’ terms were not derived from actual nursing documentation, but developed in response to discharge summaries. An initial attempt evaluated the existing nursing documentation in our hospital. Unfortunately, the terms and concepts used in this hospital were very sparse. When narrative free text information was documented, the information was often quite vague (i.e. “Talked to patient about POC”), and did not provide sufficient information to evaluate the nursing care provided. Creating these POCs by hand strengthens the results as the similarity we have found between physician and nursing documentation is likely to be an upper bound, due to the fact the nursing documentation was generated taking into account the physician discharge summary. In practice this would not occur and the similarity between the two documentations would be even lower.
Another limitation of this methodology is the fact it is reliant upon the linkages of UMLS metathesaurus. In the human evaluation, we discovered the largest disagreement between humans and the algorithm in patient 102 were there is a disagreement of 5 terms. However, with an average absolute difference of 1.9 between the algorithm and human evaluators, the algorithm is an approximation of the collaboration between professions.
Another limitation is the number of patients analyzed. The 58 physician discharge summaries were randomly selected before deidentifying so the likelihood is that the discharge summaries reflect a diversity of physicians. The nursing POCs were created by two nursing students, and were then edited and audited by faculty who are experts in nursing terminology. Due to the above variables, the methodology will need to be applied to larger datasets for reproducibility.
Another limitation of this methodology is the potential for gaps in the Natural Language Processing creating false negative due to the limitations of the algorithms or missing concepts within UMLS. However, applying MedLEE to the University of Illinois hospital dataset revealed 24,826 distinct UMLS codes for a single year compared to 3271 distinct ICD-9-CM or CPT codes for the same hospital visits [55]. Potential false negatives due to lack of knowledge of terms or missing concepts will be present in both human and computer evaluation of interprofessional terminology.
The complex relationship between the nursing and physician terms is just beginning to be uncovered in this analysis. We use standard terminologies because they have properties that are stronger than free text: the desired features and defining themes of controlled vocabularies in healthcare called the “desiderata” have been studied and applied for more than 15 years providing strength to this work [56]. Another limitation of our work is that a single site, a single population, and a single country may not be representative of care documentation by all physicians and nurses across the world.
5. Conclusion
Currently, no formal metric exists to compare and contrast work between nurses and physicians. Norma Lang has stated, “If we cannot name it, we cannot control it, practice it, teach it, finance it, or put it into public policy” [57]. The benefit of this analysis is the potential for improving care by highlighting the differences between the two professionals’ care for a complete picture. Additional future analysis will need to compare the results of the qualitative exploration of synergistic care [27–29] to the quantitative metric developed in this study. The future of inter-professional care has a long road to become successful. Future directions include identifying the variability in synonym/relatedness between hospitals and analyzing the impact on patient outcomes such as readmissions to shed light on how potential synergistic care between nurses and physicians can improve outcomes.
Supplementary Material
Summary points.
Prior
Physician nurse communication was previously studied in a qualitative manner.
No prior studies used knowledge based algorithms to compare nurse physicians documentation.
Study added
Unified Medical Language System (UMLS) can be leverage to study professional differences.
Through documentation in the electronic health record better evaluation of physician and nurse collaboration can evaluate systems of care.
Acknowledgments
Carol Friedman provided use of MedLEE for use on this project. Dr. Boyd had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
The development of MedLEE was provided in part by grant R01LM008635 from the National Library of Medicine. Research Open Access Publishing (ROAAP) Fund of the University of Illinois at Chicago provided partial financial support towards the open access publishing fee for this article.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ijmedinf.2018.02.002.
Footnotes
Authors contribution
Drs. Boyd, Dunn Lopez, Sousa, Keenan, Lussier, Di Eugenio and Mr. Lugaresi, Li, Burton, and Ms. Macieira, Balasubramanian, Acharya, Roussi conducted analysis on the data providing domain level expertise and insight.
Conflict of interest
The HANDS software that is discussed in this article is now owned and distributed by HealthTeam IQ, LLC. Dr. Gail Keenan is currently the President and CEO of this company and has a current conflict of interest statement of explanation and management plan in place with the University of Illinois at Chicago.
References
- 1.Reeves S, Nelson S, Zwarenstein M. The doctor–nurse game in the age of inter-professional care: a view from Canada. Nurs Inq. 2008;15(1):1–2. doi: 10.1111/j.1440-1800.2008.00396.x. [DOI] [PubMed] [Google Scholar]
- 2.Nightingale F. Notes on Nursing: What It Is, and What It Is Not. Lippincott Williams & Wilkins; 1992. [Google Scholar]
- 3.Ahad MA. Evolution of nursing sciences: implications for nursing world wide. Image (IN) 1981 Jun;13(2):56–59. doi: 10.1111/j.1547-5069.1981.tb01484.x. [DOI] [PubMed] [Google Scholar]
- 4.Keenan G, Yakel E, Dunn Lopez K, Tschannen D, Ford YB. Challenges to nurses’ efforts of retrieving, documenting, and communicating patient care information. J Am Med Inform Assoc. 2013 Mar-Apr;20(2):245–251. doi: 10.1136/amiajnl-2012-000894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Med Care. 1994:771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Estrabrooks C, Midodi W, Cummings G, Ricker K, Giovannetti P. The impact of hospital nursing characteristics on 30 day mortality. Nurs Res. 2005;2(54):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Mulindwa F, Blitz J. Perceptions of doctors and nurses at a Ugandan hospital regarding the introduction and use of the South African Triage Scale. Afr J Prim Health Care Fam Med. 2016 Mar;8(1):e1–e7. doi: 10.4102/phcfm.v8i1.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003 Jun;133(6):614–621. doi: 10.1067/msy.2003.169. [DOI] [PubMed] [Google Scholar]
- 9.Codman AE. American College of Surgeons Board of Regents. The “1919” Minimum Standard Document. 2006 Available at: https://www.facs.org/about-acs/archives/pasthighlights/minimumhighlight accessed 01/2015.
- 10.Gillum RF. From papyrus to the electronic tablet: a brief history of the clinical medical record with lessons for the digital age. Am J Med. 2013 Oct;126(10):853–857. doi: 10.1016/j.amjmed.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 11.Siegler EL. The evolving medical record. Ann Intern Med. 2010 Nov;153(10):671–677. doi: 10.7326/0003-4819-153-10-201011160-00012. [DOI] [PubMed] [Google Scholar]
- 12.Kesselheim AS, Brennan TA. Overbilling vs. downcoding – the battle between physicians and insurers. N Engl J Med. 2005 Mar;352(9):855–857. doi: 10.1056/NEJMp058011. [DOI] [PubMed] [Google Scholar]
- 13.Mellner C, Selander H, Wolodarski J. The computerized problem-oriented medical record at Karolinska Hospital – format and function, users’ acceptance and patient attitude to questionnaire. Methods Inf Med. 1976 Jan;15(1):11–20. [PubMed] [Google Scholar]
- 14.Chowdhry SM, Mishuris RG, Mann D. Problem-oriented charting: a review. Int J Med Inform. 2017 Jul;103:95–102. doi: 10.1016/j.ijmedinf.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Roussi R, Soussa V, Dunn Lopez K, Balasubramanian A, Keenan GM, Burton M, Bahroos N, Eugenio BDi, Boyd AD. Presented Medinfo 2015. Sao Paulo, Brazil: Aug 19–23, 2015. Are we talking about the same patient? [PubMed] [Google Scholar]
- 16.Steffen L. Ode to the Kardex. Creat Nurs. 2009;15(1):53–54. doi: 10.1891/1078-4535.15.1.53. [DOI] [PubMed] [Google Scholar]
- 17.Ehnfors M. Nursing documentation practice on 153 hospital wards in Sweden as described by nurses. Scand J Caring Sci. 1993;7(4):201–207. doi: 10.1111/j.1471-6712.1993.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 18.Cheevakasemsook A, Chapman Y, Francis K, Davies C. The study of nursing documentation complexities. Int J Nurs Pract. 2006 Dec;12(6):366–374. doi: 10.1111/j.1440-172X.2006.00596.x. [DOI] [PubMed] [Google Scholar]
- 19.Blair W, Smith B. Nursing documentation: frameworks and barriers, Contemp. Nurse. 2012;41(2):160–168. doi: 10.5172/conu.2012.41.2.160. [DOI] [PubMed] [Google Scholar]
- 20.NANDA-I, NANDA-I International Defining the Knowledge of Nursing, History. 2014 Available at: http://www.NANDA-I.org/NANDA-I-international-history. html accessed 13.02.14.
- 21.Tastan S, Linch GC, Keenan GM, Stifter J, McKinney D, Fahey L, et al. Evidence for the existing American Nurses Association-recognized standardized nursing terminologies: a systematic review. Int J Nurs Stud. 2014 Aug;51(8):1160–1170. doi: 10.1016/j.ijnurstu.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van der Bruggen H, Groen M. Toward an unequivocal definition and classification of patient outcomes. Nurs Diagn. 1999 Jul-Sep;10(3):93–102. doi: 10.1111/j.1744-618x.1999.tb00035.x. [DOI] [PubMed] [Google Scholar]
- 23.Keenan GM, Yakel E, Yao Y, Xu D, Szalacha L, Tschannen D, et al. Maintaining a consistent big picture: meaningful use of a Web-based POC EHR system. Int J Nurs Knowl. 2012 Oct;23(3):119–133. doi: 10.1111/j.2047-3095.2012.01215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunn Lopez K. Implications of within profession differences in nurse–physician work relationships on efficiency and care coordination. Int J Qual Methods. 2010;9(4) [Google Scholar]
- 25.Tang CJ, Chan SW, Zhou WT, Liaw SY. Collaboration between hospital physicians and nurses: an integrated literature review. Int Nurs Rev. 2013 Sep;60(3):291–302. doi: 10.1111/inr.12034. [DOI] [PubMed] [Google Scholar]
- 26.Stein LI, Watts DT, Howell T. The doctor-nurse game revisited. N Engl J Med. 1990 Feb;322(8):546–549. doi: 10.1056/NEJM199002223220810. [DOI] [PubMed] [Google Scholar]
- 27.San-Martin M, Delgado-Bolton R, Vivanco L. Professionalism and occupational well-being: similarities and differences among Latin American health professionals. Front Psychol. 2017 Jan;8:63. doi: 10.3389/fpsyg.2017.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lancaster G, Kolakowsky-Hayner S, Kovacich J, Greer-Williams N. Interdisciplinary communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275–284. doi: 10.1111/jnu.12130. [DOI] [PubMed] [Google Scholar]
- 29.Muller-Juge V, Cullati S, Blondon KS, Hudelson P, Maitre F, Vu NV, et al. Interprofessional collaboration on an internal medicine ward: role perceptions and expectations among nurses and residents. PLOS ONE. 2013;8(2):e57570. doi: 10.1371/journal.pone.0057570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manojlovich M, Harrod M, Holtz B, Hofer T, Kuhn L, Krein SL. The use of multiple qualitative methods to characterize communication events between physicians and nurses. Health Commun. 2015;30(1):61–69. doi: 10.1080/10410236.2013.835894. [DOI] [PubMed] [Google Scholar]
- 31.Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003 Mar;31(3):956–959. doi: 10.1097/01.CCM.0000056183.89175.76. [DOI] [PubMed] [Google Scholar]
- 32.Zhang L, Huang L, Liu M, Yan H, Li X. Nurse–physician collaboration impacts job satisfaction and turnover among nurses: a hospital-based cross-sectional study in Beijing. Int J Nurs Pract. 2016 Jun;22(3):284–290. doi: 10.1111/ijn.12424. [DOI] [PubMed] [Google Scholar]
- 33.van Beek L, Goossen WT, van der Kloot WA. Linking nursing care to medical diagnoses: heterogeneity of patient groups. Int J Med Inform. 2005 Dec;74(11–12):926–936. doi: 10.1016/j.ijmedinf.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Clinical research data warehouse enrichment via NLP over discharge summaries. AMIA Clinical Research Informatics Conference. 2014 Apr 10th; [Google Scholar]
- 35.Friedman C, Hripcsak G, Shagina L, Liu H. Representing information in patient reports using natural language processing and the extensible markup language. J Am Med Inform Assoc. 1999 Jan-Feb;6(1):76–87. doi: 10.1136/jamia.1999.0060076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xiang Y, Lu K, James SL, Borlawsky TB, Huang K, Payne PR. k-Neighborhood decentralization: a comprehensive solution to index the UMLS for large scale knowledge discovery. J Biomed Inform. 2012;45(2):323–336. doi: 10.1016/j.jbi.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halper M, Morrey CP, Chen Y, Elhanan G, Hripcsak G, Perl Y. Auditing hierarchical cycles to locate other inconsistencies in the UMLS. AMIA Annu Symp Proc. 2011;2011:529–536. [PMC free article] [PubMed] [Google Scholar]
- 38.Cimino JJ, Clayton PD, Hripcsak G, Johnson SB. Knowledge-based approaches to the maintenance of a large controlled medical terminology. J Am Med Inform Assoc. 1994 Jan-Feb;1(1):35–50. doi: 10.1136/jamia.1994.95236135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butcher HK, Bulechek GM, Dochterman JMM, Wagner C. Nursing Interventions Classification (NIC) Elsevier Health Sciences; 2013. [Google Scholar]
- 40.Moorhead S, Johnson M, Maas M, Swanson E. Nursing Outcomes Classification (NOC) 5th. Elsevier Mosby; St Louis, MO: 2013. [Google Scholar]
- 41.National Library of Medicine (U.S.), 2, Metathesaurus. UMLS® Reference Manual [Internet] National Library of Medicine (U.S.); Bethesda, MD: 2009. http://www.ncbi.nlm.nih.gov/books/NBK9684/ [Google Scholar]
- 42.Patel CO, Cimino JJ. A scale-free network view of the UMLS to learn terminology translations. Stud Health Technol Inform. 2007;129(Pt 1):689–693. [PubMed] [Google Scholar]
- 43.So EY, Park HA. Exploring the possibility of information sharing between the medical and nursing domains by mapping medical records to SNOMED CT and ICNP. Healthc Inform Res. 2011 Sep;17(3):156–161. doi: 10.4258/hir.2011.17.3.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zielstorff RD, Cimino C, Barnett GO, Hassan L, Blewett DR. Representation of nursing terminology in the UMLS Metathesaurus: a pilot study. Proc Annu Symp Comput Appl Med Care. 1992:392–396. [PMC free article] [PubMed] [Google Scholar]
- 45.Campbell JR, Carpenter P, Sneiderman C, Cohn S, Chute CG, Warren J, Phase II. evaluation of clinical coding schemes: completeness, taxonomy, mapping, definitions, and clarity. CPRI Work Group on Codes and Structures. J Am Med Inform Assoc. 1997 May-Jun;4(3):238–251. doi: 10.1136/jamia.1997.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gordon M. Nursing nomenclature and classification system development. Online J Issues Nurs. 1998;3(2) [Google Scholar]
- 47.Bakken S, Warren J, Lundberg C, Casey A, Correia C, Konicek D, et al. An evaluation of the utility of the CEN categorical structure for nursing diagnoses as a terminology model for integrating nursing diagnosis concepts into SNOMED. Stud Health Technol Inform. 2001;84(Pt 1):151–155. [PubMed] [Google Scholar]
- 48.Bakken S, Warren JJ, Lundberg C, Casey A, Correia C, Konicek D, et al. An evaluation of the usefulness of two terminology models for integrating nursing diagnosis concepts into SNOMED Clinical Terms. Int J Med Inform. 2002 Dec;68(1–3):71–77. doi: 10.1016/s1386-5056(02)00066-7. [DOI] [PubMed] [Google Scholar]
- 49.Lu DF, Eichmann D, Konicek D, Park HT, Ucharattana P, Delaney C. Standardized nursing language in the systematized nomenclature of medicine clinical terms: a cross-mapping validation method. Comput Inform Nurs. 2006 Sep-Oct;24(5):288–296. doi: 10.1097/00024665-200609000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Park HT, Lu DF, Konicek D, Delaney C. Nursing interventions classification in systematized nomenclature of medicine clinical terms: a cross-mapping validation. Comput Inform Nurs. 2007 Jul-Aug;25(4):198–208. doi: 10.1097/01.NCN.0000280590.35690.7d. quiz 209–10. [DOI] [PubMed] [Google Scholar]
- 51.Lopez-Garcia P, Boeker M, Illarramendi A, Schulz S. Usability-driven pruning of large ontologies: the case of SNOMED CT. J Am Med Inform Assoc. 2012 Jun;19(1e):e102–e109. doi: 10.1136/amiajnl-2011-000503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.College of American Pathologies, SNOMED Historical Perspectives. 2008 Available at: http://www.cap.org/apps/cap.portal?_nfpb=true&cntvwrPtlt_actionOverride=%2Fportlets%2FcontentViewer%2Fshow&_windowLabel=cntvwrPtlt&cntvwrPtlt{actionForm.contentReference}=snomed%2FhistPersp.html&_state=maximized&_pageLabel=cntvwr. Accessed 3 April 2012.
- 53.Terner A, Lindstedt H, Sonnander K. Predefined headings in a multiprofessional electronic health record system. J Am Med Inform Assoc. 2012 Nov-Dec;19(6):1032–1038. doi: 10.1136/amiajnl-2012-000855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wibe T, Ekstedt M, Helleso R. Information practices of health care professionals related to patient discharge from hospital, Inform. Health Soc Care. 2015;40(3):198–209. doi: 10.3109/17538157.2013.879150. [DOI] [PubMed] [Google Scholar]
- 55.Burton M, Sadhu E, Dong X, Lei Z, Bahroos N. Clinical research data warehouse enrichment via NLP OVer discharge summaires. AMIA Summits on Translational Science Proceedings AMIA Summit on Translational Science. 2014 [Google Scholar]
- 56.Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med. 1998 Nov;37(4–5):394–403. [PMC free article] [PubMed] [Google Scholar]
- 57.Clark J, Lang N. Nursing’s next advance: an internal classification for nursing practice. Int Nurs Rev. 1992 Jul-Aug;39(4):109–111. 128. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


