Abstract
Objective. To take a systematic approach to exploring patient safety teaching in health care curricula, particularly in relation to how educators ensure students achieve patient safety competencies.
Findings. There is a lack of formally articulated patient safety curricula, which means that student learning about safety is largely informal and influenced by the quality and culture of the practice environment. Human Factors and Ergonomics appeared largely absent from curricula.
Summary. Despite its absence from health care curricula, Human Factors and Ergonomics approaches offer a vehicle for embedding patient safety teaching. The authors suggest a possible model, with Human Factors and Ergonomics forming the central structure around which the curriculum can be built.
Keywords: patient safety, human factors, ergonomics, pharmacy, hidden curriculum
INTRODUCTION
Growing awareness of health care-related “harm” can be tracked through public responses to landmark events. In 1990, the US Institute of Medicine (IOM) published “To Err is Human,” which estimated that 100,000 deaths per year were a result of preventable medical errors.1 Recent updates suggest this figure is closer to 200,000, making it the third leading cause of death in the US.2 Similar stories are seen worldwide, including the UK, where medical errors at Mid-Staffordshire NHS Foundation Trust led to 1200 unnecessary deaths.3 While these medical errors ultimately resulted in poor care, they were considered to be the result of a wider lack of care and safety management. The personal and financial costs of such events have triggered considerable strategic documentation (including the UK’s “Berwick Report”), committing to “place quality of…care, especially patient safety, above all other aims,” and also influenced the emergence of patient safety as a distinct discipline.4
Cresswell and colleagues described patient safety as “a product…of a highly complex sequence of actions by multiple people and technologies.”5 One challenge is to understand the systems that produce safety-related outcomes and the cultures that influence the behavior of the “actors” within these systems. Recognition of harm as an outcome suggests that the primary goal should be to design and maintain work systems that support good performance.6 There is an increasing realization that Human Factors/Ergonomics (HFE) approaches have much to offer in this regard.7 HFE takes a systems-level approach to optimize system performance and human well-being. HFE approaches are design-based, ensuring that tasks are fitted to workers, rather than the other way round. In the UK, this recognition has resulted in increased interest in this approach. For example the Human Factors Concordat outlines the commitment made by professional, statutory, and regulatory bodies to support front-line staff in realizing the benefits of HFE practices.8 Other UK recommendations are to include HFE in serious incident investigations.9 One of the initiatives to implement the Concordat was a series of HFE taster workshops by the UK professional body for HFE, the Chartered Institute of Ergonomics & Human Factors (CIEHF).10
Changes in professional priorities must be reflected in educational curricula, but development with respect to patient safety has been slow. Regulatory bodies have a growing safety focus, but provide little direction for teaching. In 2011, the World Health Organization (WHO) published a patient safety curriculum for educational staff, but little is known about how education providers ensure learners develop patient safety competencies and even less about teaching HFE principles.5,11-16
In Scotland, 15% of hospital admissions are drug-related and preventable with over half resulting from monitoring and/or prescribing errors.17 While these errors have complex causality, the pharmacist represents a key point in the error chain. It is proposed that developing capacity in pharmacist safety knowledge and skills could contribute to improving work systems to support not only medication safety, but also other aspects of patient safety. Undergraduate pharmacy courses in the UK are regulated by the General Pharmaceutical Council, which provides a framework for guiding course design as Educational Standards for Pharmacists.18 Standard 1 states the importance of patient safety, but there is limited recurrence of the term; where it is mentioned, it is generally negative (“students…must not…jeopardise patient safety”), rather than a positive requirement for developing patient safety skills.
A similar picture is seen across the world. In the US, for example, the Accreditation Council for Pharmacy Education 2016 Standards for PharmD programs describe how output from the IOM report led to recognition of the need to improve safety and outcomes and was a significant driver for the development of the Standards.1,19 However, as in the UK, beyond this introduction, there is limited reiteration of the term, and no guidance on embedding safety teaching within the curriculum. There is no direct mention of HFE, while one outcome includes the “analysis of the systems- and human-associated causes of medication errors [and] exploration of strategies designed to reduce/eliminate them.” It seems that there is a global mismatch between the aspirations of regulatory bodies and the delivery capability of education providers. The aim of this review was to explore patient safety teaching in pharmacy and other health care curricula, particularly in relation to how educators ensure students achieve patient safety competencies.
METHODS
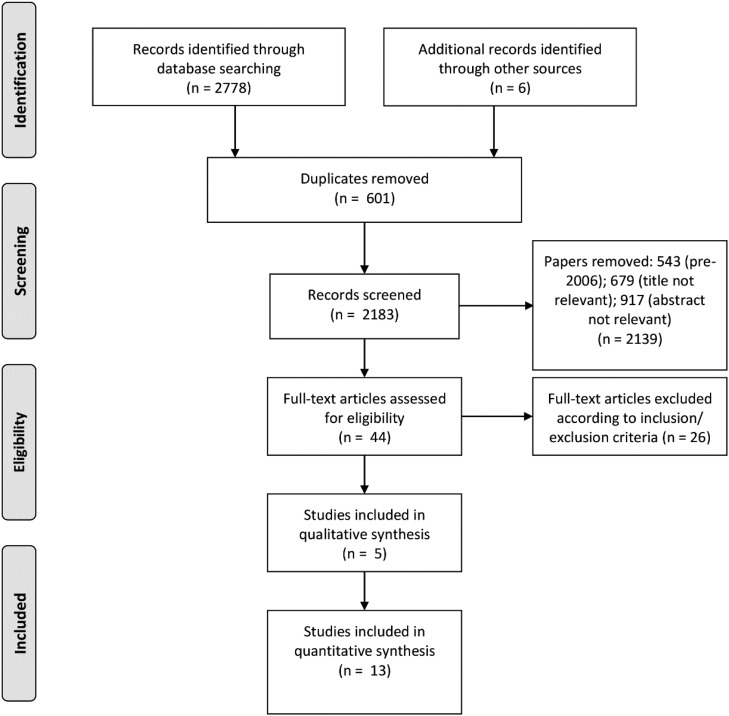
The authors of this review took a systematic approach using selected databases (Scopus, Ergonomics Abstracts, Medline and PubMed) to search for relevant literature. The search terms were: patient safety, ergonomics OR human factors, education OR curriculum, pharmacy, pharmacy education; these terms were used in Boolean combination (AND). The search was restricted to studies reported in academic journals, in English language and published from 2006 to 2017 (as a scoping search revealed very few prior studies). Articles that met the search criteria were included in the study while educational studies not about health care curricula, HFE studies on prevention of staff injuries, reviews, editorials and opinion pieces were excluded. Additional sources of papers included colleagues working in the field (three papers) and “snowballing” references (three papers). These additional papers all met the inclusion criteria. The review was performed by a single researcher. The search strategy is detailed in a PRISMA flowchart (Figure 1).
Figure 1.
PRISMA Flow Diagram Capturing Databases Searched and Retrieval Results.
Data extraction such as study characteristics (aims and design), participant characteristics ethics and governance, setting and intervention, outcome measures, strengths and limitations was followed by critical appraisal using the Critical Appraisal Skills Programme (CASP) checklist.20 Findings were synthesized using NVivo qualitative data analysis software (v10; QSR International, Melbourne, Victoria). NVivo has a “node” feature that allows sources to be thematically analyzed (“coded”). Themes with the highest frequencies (based on number of sources and comments coding at each node) are discussed in this review.
FINDINGS
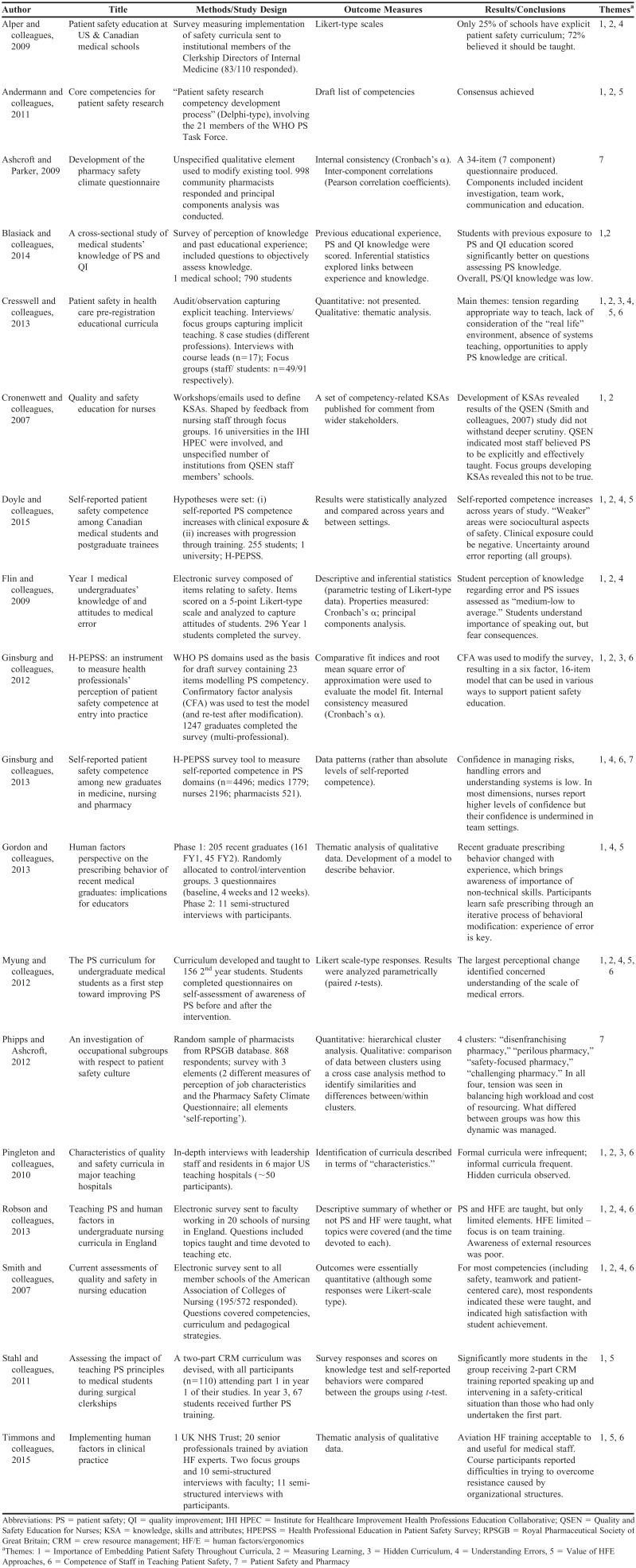
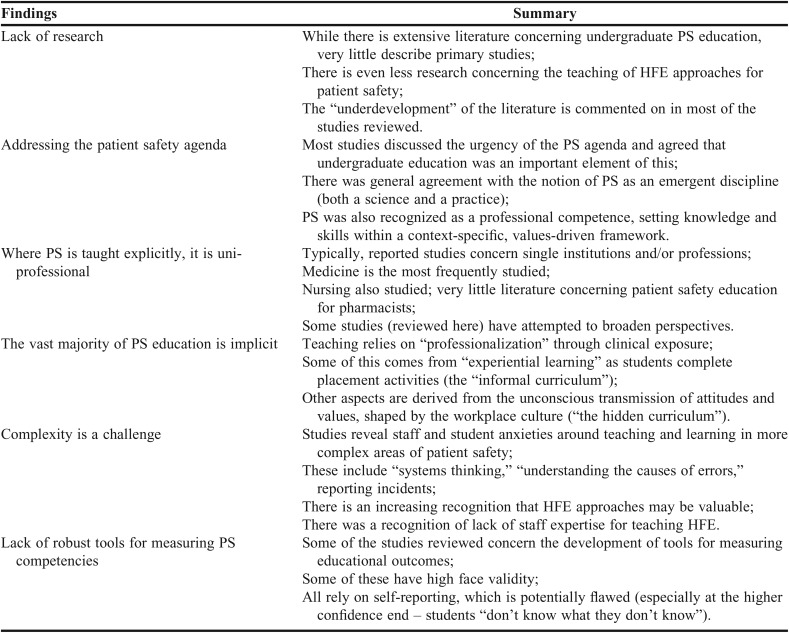
Selected papers are summarized in Table 1. Findings are summarized in Table 2, while noting that research in both patient safety and patient safety education is sparse. Studies indicated that there was very little formal safety teaching, and mostly uni-professional, with patient safety learning largely absorbed from the clinical environment (described as “informal” and “hidden” curricula). While HFE is considered to have much to offer, it is rarely taught in health care curricula (including pharmacy), and there is a lack of faculty expertise in HFE. The themes with the highest coding frequency were importance of embedding patient safety throughout curricula, measuring learning, hidden curriculum, understanding errors, value of HFE approaches, competence of staff in teaching patient safety, and patient safety and pharmacy.
Table 1.
Summary of Papers Selected for Appraisal
Table 2.
Summary of Findings
DISCUSSION
Although all the reviewed papers agreed the patient safety agenda is critical, the same few references were quoted in each. These references described the events that led to the recognition of the importance of patient safety, rather than new research, reflecting that empirical evidence for the value of patient safety programs is limited. Definitions of patient safety were discussed, but most research appeared to have content with domains defined by the WHO.21-24
Importance of Embedding Patient Safety Throughout Curricula
Patient safety was generally agreed to form part of professional identity development.13 Donaldson, introducing the WHO curriculum, states “[undergraduate education] has been under-used and under-valued…for addressing challenges of…improved patient safety.”11 The reviewed studies concurred, indicating that few health care curricula have formal patient safety outcomes and there are very few articulated strategies for supporting students in developing such skills.2,12,13,25 Where formal educational activities were described, they were mostly single modules rather than embedded curricula.26 There was also relatively little information about the content and delivery of patient safety teaching, although some studies reported that there was little in the way of interprofessional patient safety teaching.5 Health professions are at different stages, as evidenced by the disproportionate number of studies involving medicine, but this is further complicated by a teaching “skills-gap.” This was illustrated in the Quality and Safety Education for Nurses (QSEN) project.27 Core quality competencies were derived based on the 2003 IOM report “Health Professions Education, and explored in a survey and focus groups for teaching staff knowledge/ attitudes regarding these competencies. 13,28 The combined data suggested that while staff believed the competencies were being taught, they did not understand key concepts and were unable to articulate pedagogical strategies. There are limitations with this study (primarily sampling), but it raises important issues. The authors conclude that the skills gap needs to be addressed, which a number of the other studies agreed with.5,27,32 However, the observation that perception of competence does not necessarily reflect reality raises the point that accurate measurement of competency is critical.
Measuring Learning
Patient safety, as a professional competence, is the product of knowledge gained and clinical experience, as well as organizational factors shaping these experiences.5 Few validated tools could be applied in this context. Existing tools measure impact of specific interventions and have not been rigorously validity-tested. Ginsburg and colleagues developed the Health Professional Education in Patient Safety Survey (H-PEPSS), to capture self-reported competency in the patient safety domains of the WHO curriculum.23 While confirmatory factor analysis (CFA) supported development of a robust tool and international face validity was reported, it also measured self-reported competence which, as shown by the QSEN study, is flawed.13 Furthermore, to achieve “good fit” with the model proposed in the CFA, several items were removed, affecting the scope of the factor ‘recognize and respond to reduce harm’ limiting validity in this domain. H-PEPSS has been used to explore self-reported competence in medical students in a Canadian university, showing temporal increases in confidence, but also that clinical exposure does not necessarily increase perception of competence.29 The authors suggested that clinical exposure increases students’ awareness of “what they don’t know” as a reason, but it is worth further exploration. Behavioral change models, such as the Geller model, describe the step from “unconscious” to “conscious incompetence” as critical for learning. It is also possible that cultural dimensions of the environment negatively impact confidence.30
One application of H-PEPSS involved new graduates from medicine, nursing and pharmacy.24 This study revealed that common to all was the lack of confidence for managing risk and handling errors, with nurses scoring highest in most safety dimensions. However, self-reported competence with respect to “working in teams,” “communicating effectively” and “culture of safety” declined from classroom to clinic. This reflects findings well-documented elsewhere that “health care hierarchies,” most notably played out in terms of power differentials between doctors and nurses, create tensions undermining safety cultures.31 These cultures will be one of the influences that affect student learning about safety in practice.
The Hidden Curriculum
The complexity of drivers shaping student internalization of standards has led to the coining of terms “informal” and “hidden” curricula.32 Unlike the formal curriculum, they are neither articulated nor associated with defined learning outcomes. “Informal” describes experiential learning, while “hidden” describes unintended transmission of attitudes and values. When the culture of the learning environment is good, these curricula can contribute positively to patient safety education.32
The studies indicated that much of the “hidden curriculum” is delivered implicitly through clinical experiences, usually by non-academic staff during placement, underscoring the importance of how educators work with practice providers to ensure patient safety skills are appropriately developed.5 This is an area of disparity between disciplines. Some, including pharmacy in the UK, have almost no access to the clinical environment and students may seek employment to gain experience, exacerbating the undefined nature of informal curricula.33 Students may also rely on faculty-delivered, explicit patient safety teaching which may focus on “ideal” rather than “real” environments experienced during placement. A critical professional skill is recognizing when deviations from “ideal” may impact safety. Courses with regular clinical exposure have opportunities to discuss with students learning from others’ experience.
Understanding Errors
Teaching more complex patient safety aspects appears to primarily be approached through significant event analysis, with little focus on causal errors, incident reporting and systems thinking.34 Event analysis can suggest adverse events result from exceptional circumstances, rather than arising from convergence of “routine” errors. It appears dealing with errors is not taught and that educational requirements may contribute to this omission. None of the reviewed studies considered the pharmacy education context directly, but there are other information sources that shed light on influences driving error management teaching. There is a UK regulatory expectation from the General Pharmaceutical Council that students making errors should fail assessments if the outcome could cause patient harm.18 This is problematic for a number of reasons. Firstly, “unsafe practice” is a vague concept and making errors is not necessarily “unsafe,” as safety threats actually emerge from the failure to manage error. Secondly, assessment strategies promoting zero tolerance of error miss the value of learning from error. Gordon and colleagues explored prescribing behaviors of medical graduates who reflected on the causes of error and used these experiences to positively shape prescribing.35 There is a strong case for developing learning activities around error, perhaps using simulation, allowing students to err in safety. This also addresses a potential limitation of the work of Gordon and colleagues, as requiring disclosure of “real” error can suffer social acceptability bias where poor behaviors are omitted, or a positive spin (such as claiming errors as learning experiences) makes reporting more palatable. Error management is a cornerstone of HFE practice, and therefore HFE may be useful as a framework to support safety teaching.
The Value of HFE Approaches
Patient safety must consider safety threats but also provide solutions to deal with these. In 2000, the UK Department of Health published “An Organisation with a Memory,” reporting on the findings of an expert group regarding “learning from adverse events.”36 The report defined a number of key observations, including that harms within the NHS are disturbingly repetitive; research into learning from failure in health care is underdeveloped, but much more is available from other organizations; lessons from adverse events rarely become embedded in practice; and analysis of adverse events tends to focus on blaming individuals, which points to a lack of systems understanding among health care practitioners.
The report recognized that culture was a major contributor to safety, but was seen as a “mysterious intangible entity,” rather than as a set of elements that can be captured and measured. It was suggested that health care organizations should aim to become high reliability organizations (HROs) to improve safety with robust safety cultures. The authors also recognized that adverse events arise from interactions between professionals and patients with their environment, highlighting the usefulness of HFE. In response to the report, the UK Patient Safety Research Portfolio (PSRP) was established. Waring and colleagues found the majority had a common theoretical underpinning, namely that HFE approaches of the type adopted by HROs could improve safety, with the limitation that the author panel did not include HFE expertise to assess the HFE approaches.37
Very few of the studies reviewed involved HFE, although Timmons and colleagues reflected on the lack of qualitative research in HFE patient safety in their work that involved a longitudinal qualitative study exploring emergency department and operating theater staff perception of aviation-style HFE training.16 While staff considered the training invaluable, this was expected as participants were “self-selected HFE enthusiasts.” The main findings concerned perceived barriers to implementation including, for example, junior staff struggling with challenging senior colleagues. There were also differences regarding acceptability of change. If change was seen as owned by clinical staff, then it was accepted, but management-imposed change was problematic. Culture is thus critical not just to safety, but to change implementation. This is worth exploring because organizational change is necessary for delivering patient safety teaching agendas. The authors considered this fear of change to manifest itself in institutions hiding behind “excessive pride in professionalism” as alluded to by Robson and colleagues.15 Thirteen English nursing schools all indicated they considered patient safety a priority and that it is featured prominently in their curricula. The majority also stated HFE was taught, but as with the QSEN study, this did not withstand deeper scrutiny. HFE education was sparse; with limited non-technical (non-specialist) skills training rather than HFE.36 The authors also believed that lack of educational corporate responsibility is seen where students are not offered appropriate access to clinical environments or academic-practitioner relationships are insufficiently developed to support effective learning. Institutions may also fail to adequately resource courses, including recruiting and retaining staff with appropriate expertise.
Competence of Staff in Teaching Patient Safety
Cresswell and colleagues offered a robust exploration of patient safety teaching across institutional and professional contexts.5 The study had strong methodological underpinning, based on Eraut’s framework. This framework describes the informal and formal nature of the acquisition of professional knowledge, including the hidden curriculum. A mixed-methods approach developed case studies in medicine, nursing, pharmacy and physiotherapy across eight institutions. The results confirmed the largely implicit nature of patient safety teaching, lack of “formal” curricula and heavy reliance on “hidden” teaching. They suggested that the main challenge was lack of expertise in patient safety science.
These findings echo earlier studies and the challenge is translating patient safety knowledge into curricular change. As discussed, hidden curricula can be valuable and work best when all staff are involved in “teaching” with strong, consistent safety messages transmitted to students.32 A similar cross-sectional staff expertise is required across the whole undergraduate curriculum. This is unlikely to exist at any institution, and anxieties about threats posed by this “identification of ignorance” are possibly behind reluctance of some educators to accept that integrated patient safety teaching is critical.11
One suggestion is increasing expert input.15 Role models are needed, in both clinical practice and academia, and staff may need further training. HFE bridges across engineering, design, architecture, psychology and safety management programs among others and many institutions are likely to have access to such expertise. Pharmacy faculty may be able to make use of this expertise in developing their own safety competence.
Some of the reviewed studies discussed quality improvement (QI) as being an important part of patient safety education, although no case was made for it as an educational strategy, and elsewhere in the literature, there is evidence to suggest it is not always effective in improving safety.38 QI and HFE share similar origins, although QI is more process-focussed compared with HFE, which considers “whole-system optimization.” One weakness of QI is lack of tools for supporting redesign of health care systems, and this systems-level understanding is critical if safety issues are to be successfully addressed. However, the practice of QI is generally well understood within health care and it offers a starting point for change.39 Furthermore, Hignett and colleagues suggest it might be integrated with HFE, yielding a powerful approach to patient safety, building on existing knowledge and training materials.40
Patient Safety and Pharmacy
There were no outputs for literature searches involving HFE and undergraduate pharmacy education, and very little with respect to patient safety and pharmacy undergraduate teaching. Two of the studies did include pharmacy students, but there was little consideration in any of the studies for the specific pharmacy education context.5,24
Lack of clinical experience for pharmacy students is compounded by a lack of good quality placements, which may only comprise short visits and tend to be (i) observational and (ii) lacking in consistency in terms of student experience.33 Placements must be quality assured, and achieved (in the UK) through compliance with the UK Quality Code for Higher Education.41 This indicates that depth of quality assurance should be related to risks posed to the curriculum. One-day placements are unlikely to contribute (directly) to achievement of learning outcomes and quality assurance is therefore often weak.
Given the importance of culture to informal and hidden curricula, a study by Ashcroft and Parker involving the development of a community pharmacy safety climate questionnaire offered insights regarding the congruence between the organization’s official safety stance and actual practice.42 Likert scale-type responses captured participants’ agreement with statements on safety-related themes. Elements were tested using principal components analysis, and some themes merged, resulting in the Pharmacy Safety Climate Questionnaire. This was validated in later studies, including the Phipps and Ashcroft exploration of the concept of subgroups within community pharmacy with respect to their patient safety views, and was based on previous findings regarding the existence of safety culture “archetypes.”43 The questionnaire was sent to a random sample of community pharmacists on the UK national register with cluster analysis of the responses. Four subgroups were described who perceived their workplaces to range from “perilous” to “safety focused.” All clusters showed significant similarities with respect to pressures of work, but differences appeared to derive from how much support pharmacists received to meet these challenges. A potential limitation of this study is the data- (rather than theory) driven analysis. The study raises an interesting question for pharmacy education. Many of these pharmacies provided placement experiences for students and new graduates, and were contributing to informal and hidden curricula. A recent study by the Phipps and Ashcroft group has explored how a combination of incident reporting data and work domain analysis can be used to explore the contextual factors that contribute to degraded safety in community pharmacy environments.44 Such robust approaches to safety will hopefully begin to strengthen the pharmacy hidden curriculum.
Bradley and colleagues explored the nature of the hidden curriculum in graduate pharmacy (master in pharmacy) courses with a purposely selected sample of UK pharmacy schools.45 They suggested that teaching and learning activities based around patient safety were evident in curricula, but confirmed findings that much is implicit.
While patient safety is high on the agenda for all health care disciplines, the need for pharmacy educational reform may be particularly urgent, largely due to the expanding clinical practice element of the role. Across the world, health care reform demands a patient-centered care delivery model, with the pharmacist taking a central role in the management of “pharmaceutical care.”46-48 If pharmacists are to take responsibility for patient outcomes, then they must enter the workplace equipped with the competencies that will allow them to deliver safe care.
As with any systematic review, there are methodological limitations. For example, a pragmatic decision was made to select databases, and there may be others (eg, PsychInfo) which could have identified additional literature sources. Potential bias was managed by offering a transparent process for article selection (PRIMSA), and critical appraisal tool (CASP) with high face validity and application in health care.
CONCLUSION
This review reveals that robust research into patient safety is under-developed with the literature around pedagogical strategies for teaching patient safety even less developed. The literature concerning teaching of patient safety to pharmacy students is limited; a critical concern given the number of preventable errors that are medication-related. The limited patient safety education literature available indicates that formal safety curricula are rare across all health care disciplines, with most teaching implicit, and learning heavily influenced by informal and hidden curricula. Given that pharmacy students have limited access to placement, they may be denied these other sources of learning and rely heavily on other sources such as relevant paid employment and on formally provided, academic scenarios that may not capture real-life work environments.
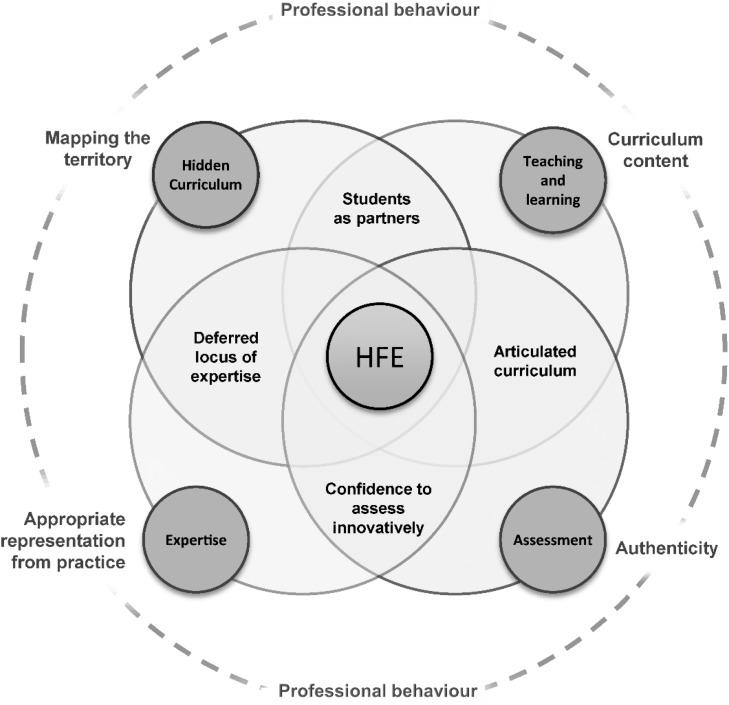
It is certainly timely to consider strategies for formalizing patient safety teaching by clearly articulating safety-related outcomes within course curricula. The findings of this review suggest that one of the major barriers to this is a lack of understanding of safety science, and how practical safety competencies relate to the role of the health care professional. This is exacerbated by the hidden curriculum which means that academic staff members have very little understanding of the factors that influence student learning about safety. The findings also underline the value of HFE in providing systems-based tools for delivering patient safety outcomes, which involves recognizing the need for appropriate staff expertise. Addressing this issue requires the design of a good patient safety curriculum, and the authors propose a model (Figure 2) which reflects these findings with HFE as the central supporting structure around which the curriculum may be designed.
Figure 2.
A Model for Embedding Patient Safety Teaching.
A traditionally constructively aligned health care curriculum reflects professional behavior, articulated in the program outcomes. Assessment is designed to capture these outcomes, and appropriate teaching and learning activities are established to support student success in assessment. Appropriate staff expertise is required to deliver the course. The model proposed above develops this further by:
a. Recognizing the importance of the “hidden curriculum” in driving student learning and behavior. This hidden curriculum must be mapped by working in partnership with students who are the ‘experts’ in this. Space must be provided within the curriculum to allow student-led exploration of all the experiences that contribute to their professional development.
b. Recognizing that curriculum content must be driven by the needs of the practice role and assessment must be authentic, effectively measuring professional competencies. This may require a move away from traditional assessment formats, requiring staff to challenge their existing practice.
c. Proposing that HFE provide the tools to deliver on all of these aspects, and should be central to the curriculum, in both delivery and design.
ACKNOWLEDGMENTS
The authors would like to thank Ed Watson for providing the artwork for Figure 2.
REFERENCES
- 1. Institute of Medicine; Committee on Quality of Healthcare in America. To Err is Human. Building a Safer Health System. Washington, DC: National Academy Press; 1999.
- 2.Blasiak RC, Stokes CL, Meyerhoff KL, Hines RE, Wilson LA, Viera AJ. A cross-sectional study of medical students’ knowledge of patient safety and quality improvement. N C Med J. 2014;75(1):15–20. doi: 10.18043/ncm.75.1.15. [DOI] [PubMed] [Google Scholar]
- 3.Francis R. The Mid Staffordshire NHS Foundation Trust public enquiry. 2013. http://www.midstaffspublicinquiry.com/report. Accessed July 10, 2016.
- 4.Berwick D. A promise to learn – a commitment to act: improving the safety of patients in England. 2013. http://www.england.nhs.uk/2013/08/06/pat-safety-berwick-report/ Accessed April 02, 2018.
- 5.Cresswell K, Howe A, Steven A, et al. Patient safety in healthcare preregistration curricula: multiple case study-based investigations of eight medicine, nursing, pharmacy and physiotherapy university courses. BMJ Qual Saf. 2013;22(10):843–854. doi: 10.1136/bmjqs-2013-001905. [DOI] [PubMed] [Google Scholar]
- 6.Buckle P, Clarkson PJ, Coleman R, Ward J, Anderson J. Patient safety, systems design and ergonomics. Appl Ergon. 2006;37(4):491–500. doi: 10.1016/j.apergo.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2014;23(3):196–205. doi: 10.1136/bmjqs-2013-001812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Quality Board. 2013. Human factors in healthcare. A concordat from the National Quality Board. http://www.england.nhs.uk/wp-content/uploads/2013/11/nqb-hum-fact-concord.pdf. Accessed April 02, 2018.
- 9.Care Quality Commission. 2016. Briefing. Learning from serious incidents in NHS acute hospitals. http://www.cqc.org.uk/content/briefing-learning-serious-incidents-nhs-acute-hospitals. Accessed April 02, 2018.
- 10.Hignett S, Lang A, Pickup L, et al. More holes than cheese. What prevents the delivery of effective, high quality, and safe healthcare in England? Ergonomics. 2018;61(1):5–14. doi: 10.1080/00140139.2016.1245446. [DOI] [PubMed] [Google Scholar]
- 11.Walton M, Woodward H, Van Staalduinen S, et al. The WHO patient safety curriculum guide for medical schools. Qual Saf Health Care. 2010;19:542–546. doi: 10.1136/qshc.2009.036970. [DOI] [PubMed] [Google Scholar]
- 12.Alper E, Rosenberg EI, O’Brien KE, Fischer M, Durning SJ. Patient safety education at US and Canadian medical schools: results from the 2006 clerkship directors in internal medicine survey. Acad Med. 2009;84(12):1672–1676. doi: 10.1097/ACM.0b013e3181bf98a4. 2009. [DOI] [PubMed] [Google Scholar]
- 13.Cronenwett L, Sherwood G, Barnsteiner J, et al. Quality and safety education for nurses. Nurs Outlook. 2007;55(3):122–131. doi: 10.1016/j.outlook.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ Qual Saf. 2012;21(4):347–351. doi: 10.1136/bmjqs-2011-000421. [DOI] [PubMed] [Google Scholar]
- 15.Robson W, Clark D, Pinnock D, White N, Baxendale B. Teaching patient safety and human factors in undergraduate nursing curricula in England: a pilot survey. Br J Nurs. 2013;22(17):1001–1005. doi: 10.12968/bjon.2013.22.17.1001. [DOI] [PubMed] [Google Scholar]
- 16.Timmons S, Baxendale B, Buttery A, Miles G, Roe B, Browes S. Implementing human factors in clinical practice. Emerg Med J. 2015;32(5):368–372. doi: 10.1136/emermed-2013-203203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Health Services Scotland: Information Services Division. 2013. Publication report. Prescribing and medicines: prescription cost analysis, financial year 2012/13.
- 18.General Pharmaceutical Council. 2001. Future pharmacists: Standards for the initial education and training of pharmacists. GPhC, London.
- 19.Accreditation Council for Pharmacy Education. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. 2016. https://www.acpe-accredit.org/pharmd-program-accreditation/. Accessed April 02, 2018.
- 20.CASP. 2013. Critical appraisals skills programme. http://www.casp-uk.net/#!checklists/cb36. Accessed July 10, 2016.
- 21.Runciman W, Hibbert P, Thomson R, Van Der Schaaf T, Sherman H, Lewalle P. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health C. 2009;21(1):18–26. doi: 10.1093/intqhc/mzn057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andermann A, Ginsburg L, Norton P, et al. Core competencies for patient safety research: a cornerstone for global capacity strengthening. BMJ Qual Saf. 2011;20:96–101. doi: 10.1136/bmjqs.2010.041814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ginsburg L, Castel E, Tregunno D, Norton PG. The H-PEPSS: an instrument to measure health professionals’ perception of safety competence at entry into practice. BMJ Qual Saf. 2012;21:676–684. doi: 10.1136/bmjqs-2011-000601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ginsburg LR, Tregunno D, Norton PG. Self-reported patient safety competence among new graduates in medicine, nursing and pharmacy. BMJ Qual Saf. 2013;22(2):147–154. doi: 10.1136/bmjqs-2012-001308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nie Y, Li L, Duan Y, et al. Patient safety education for undergraduate medical students: a systematic review. BMC Med Educ. 2011;11:33. doi: 10.1186/1472-6920-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics. 2015;58(1):33–49. doi: 10.1080/00140139.2014.959070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith IL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007;55(3):132–137. doi: 10.1016/j.outlook.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 28. Institute of Medicine. Health Professions Education: A Bridge to Quality. Washington, DC: National Academy Press; 2003.
- 29.Doyle P, VanDenKerkhof EG, Edge DS, Ginsburg L, Goldstein DH. Self-reported patient safety competence among Canadian medical students and postgraduate trainees: a cross-sectional survey. BMJ Qual Saf. 2015;24(2):135–141. doi: 10.1136/bmjqs-2014-003142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Geller ES. The challenge of increasing pro-environment behaviour. In: Handbook of Environmental Psychology. Bechtel RB, Churchman A, eds. New York, NY: Wiley; 2002:525–540.
- 31.Lui JK, Philbin M, Lau S, Philip PA, Yazdani M, Hatem D. Interprofessionalism between physicians and nurses: moving forward. Int J Nurs Stud. 2015;52(2):1785–1788. doi: 10.1016/j.ijnurstu.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Pingleton SK, Davis DA, Dickler RM. Characteristics of quality and patient safety curricula in major teaching hospitals. Am J Med Qual. 2010;25(4):305–311. doi: 10.1177/1062860610367677. [DOI] [PubMed] [Google Scholar]
- 33. Smith A, Darracott R. Modernising Pharmacy Careers Programme. Review of pharmacist undergraduate education and pre-registration training and proposals for reform. Medical Education England; 2011.
- 34.Flin R, Patey R, Jackson J, Mearns K, Dissanayaka U. Year 1 medical undergraduates’ knowledge of and attitudes to medical error. Med Educ. 2009;43(12):1147–1155. doi: 10.1111/j.1365-2923.2009.03499.x. [DOI] [PubMed] [Google Scholar]
- 35.Gordon M, Catchpole K, Baker P. Human factors perspective on the prescribing behaviour of recent medical graduates: implications for educators. Adv Med Educ Pract. 2013;4:1–9. doi: 10.2147/AMEP.S40487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Donaldson L.An organisation with a memory Clin Med (Lond). 200225452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waring J, Rowley E, Dingwall R, Palmer C, Murcott T. Narrative review of the UK patient safety research portfolio. J Health Serv Res Policy. 2010;15(Suppl I):26–32. doi: 10.1258/jhsrp.2009.009042. [DOI] [PubMed] [Google Scholar]
- 38.Pickup L, Atkinson S, Hollnagel E, et al. Blood sampling – two sides to the story. Appl Ergon. 2017;59(A):234–242. doi: 10.1016/j.apergo.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 39.Hignett S, Carayon P, Buckle P, Catchpole K. State of science: human factors and ergonomics in healthcare. Ergonomics. 2013;56(10):1491–1503. doi: 10.1080/00140139.2013.822932. [DOI] [PubMed] [Google Scholar]
- 40.Hignett S, Jones EL, Miller D, et al. Human factors and ergonomics and quality improvement science: integrating approaches for safety in healthcare. BMJ Qual Saf. 2015;24(4):250–254. doi: 10.1136/bmjqs-2014-003623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Quality Assurance Agency. 2015. The UK Quality Code for Higher Education. http://www.qaa.ac.uk/quality-code. Accessed April 02, 2018.
- 42.Ashcroft DM, Parker D. Development of the pharmacy safety climate questionnaire: a principal components analysis. Qual Saf Health Care. 2009;18(1):28–31. doi: 10.1136/qshc.2006.022129. [DOI] [PubMed] [Google Scholar]
- 43.Phipps DL, Ashcroft DM. An investigation of occupational subgroups with respect to patient safety culture. Safety Sci. 2012;50(5):1290–1298. [Google Scholar]
- 44.Phipps DL, Tam WV, Ashcroft DM. Integrating data from the UK national reporting and learning system with work domain analysis to understand patient safety incidents in community pharmacy. J Patient Saf. 2017;13(1):6–13. doi: 10.1097/PTS.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 45.Bradley F, Steven A, Ashcroft DM. The role of hidden curriculum in teaching pharmacy students about patient safety. Am J Pharm Educ. 2011;75(7) doi: 10.5688/ajpe757143. Article 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robinson E, Shcherbakova N, Backer L. Assessment of pharmacy manpower and services in New England. J Pharm Pract. 2016;29(6):549–55. doi: 10.1177/0897190015579449. [DOI] [PubMed] [Google Scholar]
- 47.Rosenthal M, Zubin A, Tsuyuki RT. Are pharmacists the ultimate barrier to pharmacy practice change? Canadian Pharm J. 2010;143(1):37–42. [Google Scholar]
- 48. Scottish Government. Prescription for excellence: A vision and action plan for the right pharmaceutical care through integrated partnerships and innovation. 2013; Scottish Government.