Abstract
Objective. To assess whether the Jellybean Polypharmacy Simulation Exercise (JPSE) improved empathy in pharmacy students.
Methods. The JPSE was given to all third-professional year pharmacy students in a required Special Populations course with pre- and post-scores on the Kiersma-Chen Empathy Scale (KCES) assessed, and open-ended questions on lessons learned from the exercise.
Results. Pharmacy students showed a statistically significant increase in KCES scores after completing the JPSE. Open-ended question responses reflected personal growth and appreciation for patients managing difficult medication regimens.
Conclusion. This polypharmacy simulation showed the ability to increase empathy in pharmacy students, as well as mimic a realistic experience in managing a multi-drug, multi-dose medication regimen.
Keywords: polypharmacy, simulation, empathy
INTRODUCTION
The ability to empathize is an essential element of the health care provider-patient relationship, yet is difficult to assess formally.1-3 Empathy is a core element of improving patient outcomes and has been shown to decrease the potential for litigation in the medical literature.4-8 Empathy is enhanced through experiences in which an individual has the opportunity to view a situation from the perspective of another. The demographics of the pharmacy student body evaluated was different in average age and in overall health status as compared to those of the patient population represented by this exercise. It is this difference in life experience that offers an opportunity for a simulated activity to have value for inculcating empathy. With the aging of America, and the dependence of our nation’s seniors on complex medication regimens for the care of chronic conditions, it is imperative for health professionals not only to understand what polypharmacy is, but how it feels.9
Given the potential impact of age and health discordance between the pharmacy learner and patient, the use of a simulated polypharmacy exercise could be an important tool for increasing the learner’s empathy for those managing complex medication regimens. The Jellybean Polypharmacy Simulation Exercise (JPSE) was developed as a way to inculcate empathy for those managing multi-drug, multi-dose regimens on a daily basis. The JPSE is an eight-“prescription” regimen students manage for 7 consecutive days. This regimen includes varied dosing schedules, a drug-drug interaction that needs to be mitigated by a 2-hour separation, and meal-time dosing considerations.
While multi-drug simulation exercises are not new to pharmacy education, research has focused on the ability of students to adhere to a complex regimen.10-13 Researchers have also attempted to assess the impact of interventions on empathy within simulation education; however, there is no research to date on the impact of a polypharmacy simulation on empathy using a validated empathy scale.14 The objective of this study was to determine the effectiveness of the JPSE to inculcate student empathy for those managing multi-drug, multi-dose medication regimens.
METHODS
All third-year pharmacy (P3) students (n=152) in the spring 2015 Special Populations therapeutics course were enrolled in the study. This one-credit course provides a general overview of the therapeutic issues in pediatrics, pregnancy/lactation and geriatrics. The geriatrics elements reviewed in this course include medication appropriateness, a regulatory overview, pharmacokinetic and pharmacodynamic changes seen in older adults as well as hospice principles. The JPSE was a required element of the Special Populations course, and 5% credit was assigned to its completion. Students had to successfully complete three elements to get the 5% course credit. Those elements were: taking the pre-exercise questionnaire prior to picking up their prescriptions, picking up the prescriptions at an assigned location (ie, “the pharmacy”) during “pharmacy hours,” and taking the post-exercise questionnaire by a due date. No credit for the exercise was given if one or more elements were missed. Each student took an online questionnaire prior to starting the JPSE, which consisted of basic demographic information (eg, gender, age category), and responses to the Kiersma-Chen Empathy Scale (KCES).15 The KCES is a 15-item empathy assessment that has been validated in both pharmacy and nursing students.16 It uses a Likert-type scale for ranking each of 15 statements ranging from 1=strongly disagree to 7=strongly agree with 4=neutral. Four items on the KCES are negatively worded and are reverse-coded for analysis.
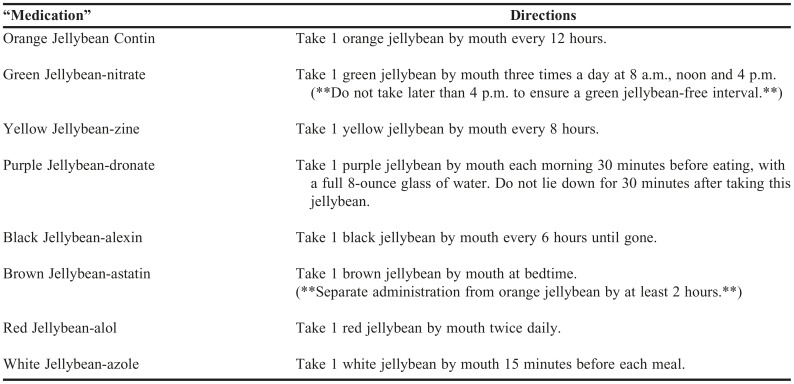
Students were also asked on a 7-point Likert scale how easy/difficult they felt an eight-prescription regimen would be to manage for a week. Each student was then provided with eight distinct jellybean “prescriptions” with a one-week supply of each jellybean with instructions to consume the jellybeans based on the instructions provided (Table 1 for the regimen). Once the one-week exercise was over, the students were again asked to complete an online questionnaire consisting of the KCES, an assessment of their difficulty managing the regimen, a question asking if the student required a medication compliance aid (eg, pill box, phone alerts), and several open-ended questions (Appendix 1). Students were excluded if there was no pre- or post-activity questionnaire recorded. A few questionnaires had a question that was not answered, and those students were excluded from the total KCES and individual item (for that item they left blank) analyses. Students served as their own control and demographic information was analyzed using descriptive statistics. Total test scores between pre- and post-simulation KCES were analyzed by paired t-tests, and individual item differences were analyzed by Wilcoxon matched-pairs signed-rank test.
Table 1.
Jellybean Polypharmacy Simulation Exercise (JPSE) Regimen
Open-ended responses were evaluated for themes of empathy and quality of life impact and were sorted accordingly. One question asked specifically about an increase in the individual student’s perception of their own empathy. However, the authors deemed the question “Were there any ‘medicines’ you opted not to take? Why? How would you feel if a patient told you they weren’t taking that ‘type’ of medicine?” to be a better judge of empathy given its non-leading language, and was therefore used to discern whether empathic language was used in problem solving for future patients with polypharmacy. Each open-ended response was categorized as “empathy” or “no empathy” by each of the four authors. This question also informed the investigators regarding the students’ adherence to the regimen. Each open-ended response was also reviewed for whether their adherence (or lack thereof) was intentional (eg, chose not to take a dose) or unintentional (eg, forgotten dose, missed a reminder). The question “How did this regimen impact your quality of life?” was assessed on how the regimen affected the quality of life of the student, and all open-ended responses were reviewed for the student’s assessment of positive or negative impact. All open-ended responses were categorized as appropriate for that particular question by each author individually. For those categorizations which were discordant, the authors met to discuss each discordant response and came to consensus. When a response to an open-ended question was truly unclear, they were marked as such in the results.
This study was exempt from formal IRB review by the Texas Tech University Health Sciences Center IRB.
RESULTS
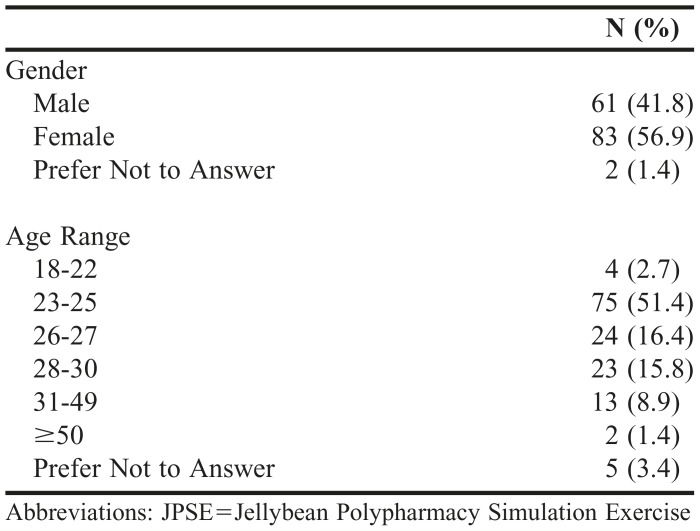
There were 152 P3 students enrolled in the Special Populations course, and 146 completed pre- and post-activity KCES questionnaires, which were used for analysis. The baseline characteristics for these subjects, as obtained via survey at the same time as the initial KCES administration, can be found in Table 2. Six students did not complete one or more of the required elements (ie, picking up “prescriptions,” etc.) and were excluded from the analysis. There were 12 missing values, nine at pre- and three at post-activity, each one belonging to a different student. Since the missing-data pattern was determined at random, there were unbalanced sample sizes in medians and interquartile ranges, but paired tests for each item (data not shown) were conducted.
Table 2.
Baseline Demographics of P3 Students Taking the JPSE
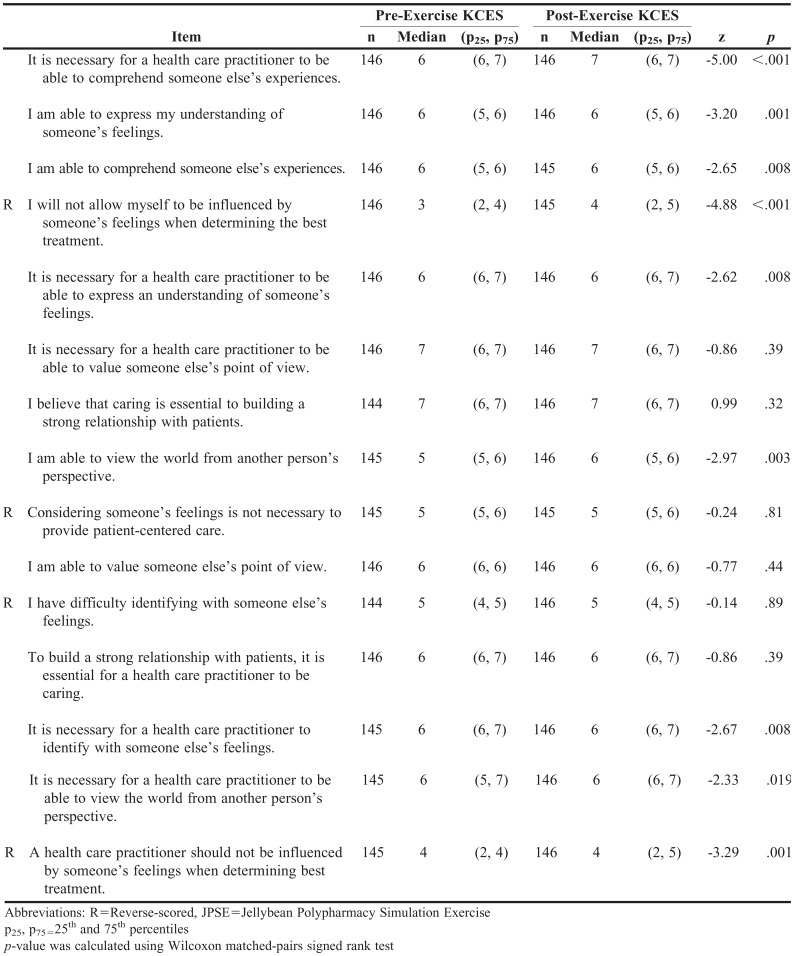
The paired t-test revealed a significant increase in empathy with a low to moderate effect size
(-4.29; p<.001; d=0.35). The open-ended comments supported this conclusion.
Responses to the “difficulty” question showed that students underestimated the difficulty of the regimen, however median scores still denoted the perceived difficulty of the regimen was high. The post-exercise data (median=1, 25th=1, 75=2) was statistically significant compared to the pre-data (median=2, 25th=2, 75th=3), with z=8.45 and p<.001.
The qualitative portion of the JPSE questionnaire consisted of free-text questions focusing on empathy and quality of life. For the prompt “Were there any ‘medicines’ you opted not to take? Why? How would you feel if a patient told you they weren’t taking that ‘type’ of medicine?,” 43 learners (29.4%) expressed language consistent with empathy for patients managing a polypharmacy regimen whereas 55 (37.7%) did not express an element of empathy one way or the other in their response, and 11 learners (7.5%) showed a lack of empathy in their response. Nineteen learners (13%) provided no answer, and 17 (11.6%) provided answers that were inconclusive regarding a change in empathy for the learner. Examples of statements classified as having empathy included: “If I had a patient who [wasn’t] taking the medication because it tastes bad, I would understand what the patient is going through and probably find an alternative or flavoring agent to make it better,” “It was extremely difficult to take the black jellybean, since it had to be administered 4 times a day. If I woke up too late or I went to bed too early, I would miss taking the black jellybean. If a patient told me they weren't taking this type of medicine, I could understand why, and I would try to work with the patient and the patient's health care provider to create a plan, so that the patient is optimizing medication use without compromising the patient's medication regimen.”
Of the 11 responses which were characterized as having no empathy, the responses were frequently noted to be paternalistic in nature: “If a patient told me they weren't taking a particular medication, I would ask why. Depending on the answer, I would suggest an alternate medication, counsel them on the risks, or tell them to have a nice day,”
“I didn't like the black ones because they tasted bad. I would not be okay with my patient doing that.”
Regarding a student’s ability to adhere to the regimen, two students adhered to the entire regimen, while 143 students did not adhere. Intentional non-adherence, seen in 71 students, was often because of unpleasant taste or inconvenient dosing times. Twenty-nine reported unintentional non-adherence primarily due to missing a dose, and for 43 students, the intentionality of the non-adherence was unclear.
Quality of life was stated to have been affected negatively by 112 students, not affected at all in 28 students and no answer was provided by five. No participants reported an improvement in quality of life with the regimen. For those reporting a negative impact, reasons included added stress, inconvenience of rearranging their schedule and feeling tied to the regimen.
DISCUSSION
This study showed that using JPSE was associated with an increase in empathy of pharmacy learners based on a validated empathy instrument. While baseline empathy was high, this simulation activity had a positive effect on overall empathy and open-ended responses reflected personal growth in many respondents.
Medication adherence is fundamentally a patient behavior and not a health professional behavior, yet there is a desire among health professionals to influence medication adherence as health outcomes are directly influenced by this behavior. For this reason, there is, perhaps, the potential for the health professional’s attitudes and behaviors to be paternalistic when approaching this concept. The accepted language may have progressed from the use of the word “compliance” to “adherence” but have attitudes necessarily followed?
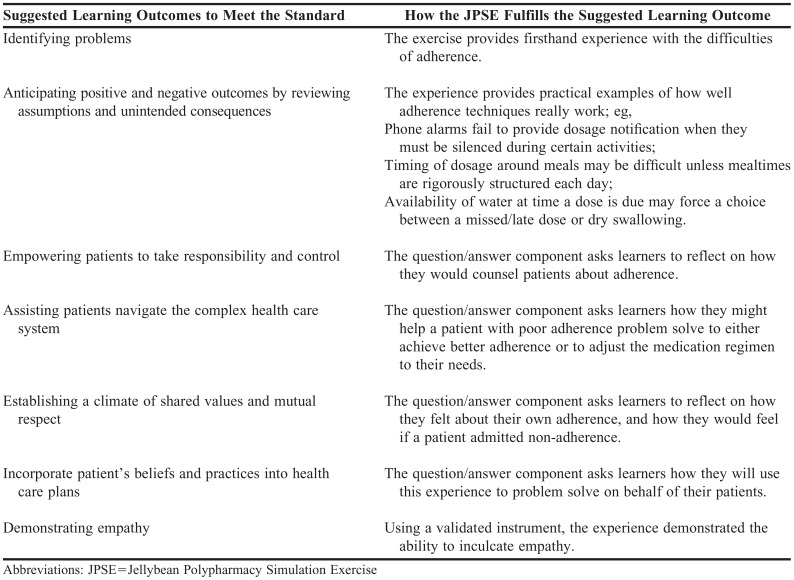
There is increased interest in the ability of pharmacy curricula to evaluate attitudes and behaviors among learners. In Standard 3 of the 2016 ACPE accreditation standards for doctor of pharmacy programs, a part of the focus is the ability of the program to impart attitudes, behaviors, and abilities to recognize social determinants of health, identify problems, and represent the patient’s best interests.17 Some of the language included in the suggested learning outcomes that can demonstrate these abilities include identifying problems, anticipating positive and negative outcomes by reviewing assumptions and unintended consequences, empowering patients to take responsibility for and control of their health, assisting patients navigating the complex health care system, establishing a climate of shared values and mutual respect necessary to meet patient care needs, incorporating patient’s beliefs and practices into health and wellness care plans, and demonstrating empathy (Table 3).
Table 3.
Examples of JPSE Assisting in Meeting Accreditation Council of Pharmacy Education Standard 317
Active learning exercises that simulate the experience of interacting with an aspect of health care delivery in the patient role can be powerful for fulfilling many of the above examples. The simulation experience itself presents learning pearls that might not otherwise be appreciated, and the question/answer or reflection component captures the impact this experience had on the learner.
This research is not without its limitations and lessons learned. This exercise was performed within the confines of a single health profession at a single institution. The increase in empathy was only seen in the pharmacy students who took the JPSE. Baseline empathy was already high in this cohort of pharmacy learners, so one might question the degree to which an educational exercise will significantly alter this. Despite this increased high baseline empathy, the KCES was able to distinguish the extent to which the JPSE was able to increase empathy. The KCES did show a statistically significant difference, and the entirety of the open-ended responses showed personal growth in quite a few participants (data not shown). Given the JPSE only used oral dosage forms, the JPSE may not assist in empathy for those who are struggling with parenteral medication adherence. It was not possible to control for those students who already take medications at baseline. And, the potential exists that students provided answers to the questions they thought were what the instructors wanted to hear, and there were several students whose responses to some of the open-ended questions did not show empathy. However, students were assured their responses wouldn’t be graded – only their participation in all elements (ie, questionnaires, picking up prescriptions) of the exercise. The authors attempted to minimize this by balancing the course credit associated with the activity. However, for future iterations of this activity, the authors will keep each student’s open-ended responses aligned with their KCES responses to discern how frequently a student’s comments are discordant with their KCES responses. Regarding lessons learned, the open-ended reflection brought to light a few items to be mindful of when the exercise is run. First, candy is not medicine. Therefore, students were cautioned within the orientation materials that this could be an issue, especially as it relates to children being present during dosing. A few students with children did note they had a hard time taking doses while in the presence of their children, given they did not want their children to feel that candy was medicine. This was problematic given the “medicine” was dispensed in a prescription vial. For future iterations of the course, zip top bags as replacements for the prescription vials for those students with children or who foresee this being a problem will be used. This activity can be workload-heavy prior to the exercise, depending on the size of the class. The filling of the prescriptions was time- and labor-intensive, filling over 1200 “prescriptions” took about 3 hours with 10 volunteers.
CONCLUSION
Overall, the JPSE was a successful simulation exercise in increasing empathy in pharmacy school students, and the IPE implications of this exercise can be fodder for future research.
ACKNOWLEDGMENTS
The authors wish to acknowledge the Texas Tech University Health Sciences Center Clinical Research Institute, and specifically Eneko Larumbe, PhD, for their assistance in the statistical analysis of this study.
Appendix 1. Jellybean Polypharmacy Simulation Exercise: Short-Answer Questions
Were there any “medicines” you opted not to take? Why? How would you feel if a patient told you they weren’t taking that “type” of medicine?
What did you find was the hardest thing about managing your regimen? What was the easiest thing?
How did this regimen impact your quality of life?
Overall, did you find value in your own empathy toward patients with multi-drug, multi-daily dosing medication regimens?
Pre- and Post-JPSE Exercise Kiersma-Chen Empathy Scale Results
REFERENCES
- 1.Hojat M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes. New York, NY: Springer; 2007. [Google Scholar]
- 2.Reiss H. Empathy in medicine: a neurological perspective. JAMA. 2010;304(14):1604–1605. doi: 10.1001/jama.2010.1455. [DOI] [PubMed] [Google Scholar]
- 3.Kestenbaum R, Farber EA, Sroufe LA. In: Individual differences in empathy among preschoolers: relation to attachment history. Empathy and Related Emotional Responses. Eisenberg N, editor. San Francisco, CA: Jossey-Bass; 1989. pp. 51–64. [DOI] [PubMed] [Google Scholar]
- 4.DiMatteo MR, Hays RD, Prince LM. Relationship of physicians’ nonverbal communication skill to patient satisfaction, appointment noncompliance and physician workload. Health Psychol. 1986;5(6):581–594. doi: 10.1037//0278-6133.5.6.581. [DOI] [PubMed] [Google Scholar]
- 5.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’adherence to medical treatment: results from the medical outcomes study. Health Psychol. 1993;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 6.Squier RW. A model of empathetic understanding and adherence results from the medical outcomes study. Soc Sci Med. 1990;30(3):325–339. doi: 10.1016/0277-9536(90)90188-x. [DOI] [PubMed] [Google Scholar]
- 7.Beckham HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice: lessons from plantiff depositions. Arch Intern Med. 1994;154(12):1365–1370. [PubMed] [Google Scholar]
- 8.Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992;267(10):1359–1363. [PubMed] [Google Scholar]
- 9.Gurwitz JH. Polypharmacy: a new paradigm for quality drug therapy in the elderly? Arch Intern Med. 2004;164(18):1957–1959. doi: 10.1001/archinte.164.18.1957. [DOI] [PubMed] [Google Scholar]
- 10.Darbishire PL, Plake KS, Kiersma ME, White JK. An introductory pharmacy practice experience on improving medication adherence. Am J Pharm Educ. 2012;76(3) doi: 10.5688/ajpe76342. Article 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Divine HS, Cain J. Assessing the effect of a polypharmacy medication adherence simulation project in a geriatrics course in a college of pharmacy. J Am Geriatr Soc. 2009;57(8):1487–1491. doi: 10.1111/j.1532-5415.2009.02364.x. [DOI] [PubMed] [Google Scholar]
- 12.Ulbrich T, Hamer D, Lehotsky K. Second-year pharmacy students’ perceptions of adhering to a complex simulation medication regimen. Am J Pharm Educ. 2012;76(1) doi: 10.5688/ajpe76111. Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans S, Lombardo M, Belgeri M, Fontane P. The Geriatric Medication Game in pharmacy education. Am J Pharm Educ. 2005;69(3) Article 46. [Google Scholar]
- 14.Chen JT, LaLopa J, Dang DK. Impact of patient empathy modeling on pharmacy students caring for the underserved. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720240. Article 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiersma ME, Chen AMH, Yehle KS, Plake KS. Validation of an empathy scale in pharmacy and nursing students. Am J Pharm Educ. 2013;77(5) doi: 10.5688/ajpe77594. Article 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zorek J, Raehl C. Interprofessional education accreditation standards in the USA: a comparative analysis. J Interprof Care. 2013;27(2):123–130. doi: 10.3109/13561820.2012.718295. [DOI] [PubMed] [Google Scholar]
- 17.Accreditation Council for Pharmacy Education. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Standards 2016. https://www.acpeaccredit.org/pdf/Standards2016FINAL.pdf. Accessed December 7, 2016.