INTRODUCTION
As the health care environment undergoes rapid transformation, increasing costs paired with technological advancements have highlighted the need for value-based health care services and innovative models of delivery. Simultaneously, the role of the pharmacist is undergoing transformation. Pharmacy graduates are now expected to be able to engage in direct patient care roles via collaborative practice, perform comprehensive medication management, and provide preventive care services. Further, the tenets of pharmacy education, while including preparing and dispensing of product, now extend to all-encompassing pharmaceutical care responsibilities. With these transformations, expectations for ensuring competence have grown.1 To meet these and future challenges, pharmacists must be prepared for continuous learning and growth after earning their doctor of pharmacy degree. Unfortunately, the current continuing education (CE) system does not encourage intentional, individualized plans and may need to be reconstructed to meet the needs of today’s practitioners.2,3 Integrating continuing professional development into the current continuing education structure could transform continuing education into a vehicle that advances both the professional’s practice and the greater health care system.
Continuing pharmacy education (CPE) has served as the standard for maintaining professional competence for over 40 years in the United States. Defined by the Accreditation Council for Pharmacy Education (ACPE), CPE is a “structured educational activity designed or intended to support the continuing development of pharmacists and/or pharmacy technicians to maintain and enhance their competence.”4 All 50 state boards of pharmacy, the District of Columbia, Guam, and Puerto Rico require CPE hours as a prerequisite for re-licensure.5 Although specific CPE requirements vary from state to state, the majority of state boards of pharmacy (43 states) require either 15 contact hours [1.5 continuing education units (CEUs)] annually or 30 contact hours (3 CEUs) biennially.5 Twenty-three states specifically require “live” CPE hours, and 17 state boards require specific CPE topics such as law, patient safety, immunizations, HIV, or pain management.5 From a regulatory standpoint, completing the hours-based CPE requirements by definition equals competency.
Researchers have debated the impact of continuing education in the health professions in the literature for decades.6 The debate centers around the question, “Does participation in continuing education enable the learner to enhance their practice and ultimately improve health care outcomes?”7 The prevailing evidence suggests the answer to this question is both “yes” and “it’s complicated.”
Between 1977 and 2014, 39 systematic reviews were published on the impact of continuing medical education (CME).8 These reviews have consistently demonstrated that CME more reliably impacts provider knowledge and performance versus patient outcomes.8 Further, traditional CE activities (conferences, symposia, lectures) improve participant knowledge but generally have a very limited effect on improving clinician practice and patient outcomes.8 Examples of published practice improvements include screening practices, prescribing, and adhering to guideline measurements. Patient outcome measurements include a broad array of clinical endpoints such as smoking cessation, diet, or blood pressure in patients with hypertension, to name a few.8,9 Specific to the pharmacy profession, studies analyzing individual CPE activities have generally, although not exclusively, shown positive effects on behaviors or patient outcomes,10-16 and one systematic review cited the effectiveness of the majority of CPE programs based on their reported outcomes measures, most often knowledge or skill modification.17
Given the frequency of evidence supporting continuing education outcomes, the ultimate CE research question is not “Is CE effective?” but rather “What kinds of CE are effective?”18 Learning activities that are interactive, use multiple delivery methods (case-based learning, demonstrations, feedback, simulations or patient roleplay), involve multiple exposures, and focus on outcomes considered important by the learner lead to more positive outcomes.18 Other factors that affect performance include audience/room size, shorter versus longer sessions, and complexity of intended behavior.8
ACPE classifies accredited CPE activities as one of three types: knowledge-based, application-based, and practice-based.4 In 2015, almost 90% of the 29,661 CPE activities offered by providers were knowledge-based activities or programs designed for participants to acquire factual knowledge as defined by ACPE CPE standards.4,19 Herein lies perhaps one of the major challenges facing continuing education: the overwhelming majority of activities are knowledge-based programs designed to improve a learner’s knowledge of facts when growing expectations from employers, regulators, and payers call for documented improvements in outcomes. Thus, how can one advance one’s practice in a system dominated by activities designed to improve knowledge? One model that has been proposed to aid learners in achieving goals through education is the Continuing Professional Development (CPD) approach.
The CPD Approach
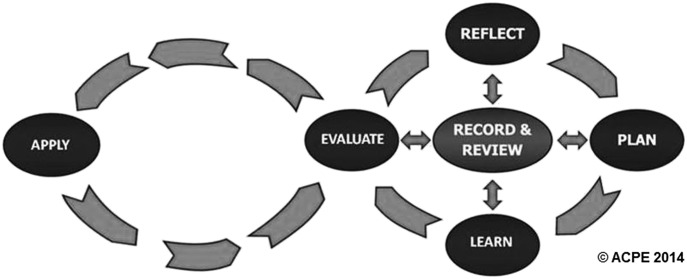
ACPE defines CPD as an ongoing, self-directed, structured, outcomes-focused learning cycle focused on maintaining and improving performance of professional practice.20 CPD does not replace CE, but rather enhances CE in a broader approach ensuring pharmacist competence and performance and patient health outcomes.1 CPD exists as a cyclical learning process (Figure 1) where the learner reflects, plans, learns, evaluates, and applies. The determination of learning experience is based on assessment of needs and goals. Central to each step in the cycle is a personal learning portfolio where learners record self-evaluations.20
Figure 1.
The CPD Cycle
Why CE Needs CPD
In 2009, the Institute of Medicine published a report concerning CE in the health professions. The report noted major flaws in the health care professions’ conduct, finance, regulation, and evaluation of CE.3 Since the report’s publication, accrediting bodies and regulatory boards have addressed many of these issues through revised standards. For example, standards for commercial support and sunshine laws have since further addressed industry influence. Much of the CE system remains in silos, however, even though health care providers are expected to perform as a team in practice. In addition, regulators still mainly base CE requirements on participation and accumulation of credit hours rather than outcomes. Despite some movements toward interprofessional education, CE remains most often associated with didactic learning methods and clinical knowledge, and in most cases, does not measure competence or impact on quality of care.3
Specific to these shortcomings, incorporating the CPD approach into practice can improve the existing composition of continuing education. Given its broader focus, the process capitalizes on intrinsic motivations by allowing health professionals to tailor their learning processes, settings, and curriculum.3,20 Students and professionals alike struggle with accurate self-assessment and identifying gaps in knowledge.21,22 As CPD inherently includes self-assessment, reflection skills can be formally practiced and improved upon, leading to more meaningful learning over time. When identifying practice or educational gaps, learners can specifically target and create plans to improve their practice with measurable results.20
Several countries including Australia, Canada, New Zealand, and the United Kingdom have incorporated the CPD approach as a requirement for pharmacist re-licensure.23 One notable model developed to ensure the competence of pharmacists and technicians is the Ontario College of Pharmacists’ Quality Assurance Program. Developed after passage of competency assessment legislation in 1991, Ontario shifted from an hours-based model to a competence-based model consisting of three components: a learning portfolio, a self-assessment tool, and a peer review process for those who provide patient care.24,25 The learning portfolio’s design puts the practitioner in control of his or her professional development, with learners determining the number of learning activities or contact hours needed to emphasize the focus on the quality of the learning experience vs accumulated hours. Portfolio contents include an education action plan, continuing education log, FAQ log, and professional profile.24 The self-assessment tool assists practitioners with identifying learning needs for both maintaining competency and advancing practice. Although on hold, the peer review process consists of a clinical knowledge and practice-based assessment that includes cases and standardized patient interviews, orientations and feedback sessions.24
As detailed by Austin and colleagues, numerous resources are required for Ontario’s quality assurance program, particularly for the peer review process.25 Volunteers are required for developing and validating cases, and establishing minimum performance levels. In addition, training materials were also developed including a web-based practice examination, and patient interview videos. Costs for the development and implementation of the program are paid for by annual licensure fees.25
The other countries listed each have distinct CPD approaches. The Pharmacy Board of Australia, for instance, requires pharmacists to complete activities that have an aggregate value of 40 or more CPD credits annually, develop a CPD plan, and maintain detailed and verifiable records of learning.26 New Zealand’s pharmacist’s scope of practice system requires participants to earn “points” from activities in three distinct learning groups: activities with limited or no attendee interaction; activities with acquisition of knowledge verified by assessment; and initiatives focused on practice improvements identified by reflection and providing supporting evidence of practice outcomes.27 In another example, the General Pharmaceutical Council of the United Kingdom maintains an online system where online CPD records can be shared with supervisors or other colleagues who support or monitor CPD activities.28
In the medical profession, voluntary board certification largely regulates many elements of CPD beyond required CME hours. Board certification rates among physicians outpace pharmacists. In 2014, the American Board of Medical Specialties had certified 79% of actively licensed physicians in the United States in addition to select osteopathic physicians maintaining osteopathic physician board certifications.29 In contrast, over 25,000 pharmacists maintain Board of Pharmaceutical Specialties (BPS) certifications, comprising approximately 9% of licensed pharmacists in the United States.30-31 The American Board of Internal Medicine (ABIM) and its 24-member organizations regulate a maintenance of certification (MOC) system initiated in 2000. Participants earn “points,” including for participating in CME activities, and in other opportunities that earn credit via demonstrating involvement in the domains of medical knowledge, practice assessment, and patient safety/voice activities.32-36 Activities such as participating in a journal club, precepting trainees, serving as a manuscript reviewer, and attending CME activities, are ways to earn “points.” In addition, physicians must “re-board” by passing a certification exam in one’s specialty every 10 years.32,33
In the US, results of a five state CPD pharmacist pilot project were published in 2010.35 Questions still remain, however, whether CPD adoption into CE should be required or optional for license renewal processes.23 Anecdotal feedback from boards of pharmacy has revealed concerns about capacity to institute and regulate such a system, with specific concerns regarding document review and assessment. An employer-employee partnership is perhaps a more natural home for CPD. Reviewing employees’ CPD goals, for instance, could easily be incorporated into existing annual evaluation processes. Employees wanting to seek opportunities for advancement or to develop local expertise could benefit from a formalized self-directed learning approach such as CPD.
As with all new systems, challenges with the CPD approach exist. Undoubtedly, CPD requires increased efforts on the part of the learner – self-assessing, seeking learning opportunities, and documenting outcomes require energy and support. Critics have noted a variety of barriers to the practice of CPD including lack of time for reflection, funding for learning, defining responsibilities and designating roles of parties involved in CPD, and demonstrating CPD results to stakeholders.36 Not all participants see the need to improve their practice and to support CPD as a lifelong learning model. If adopted, not only would intensive education be needed, but also coaching throughout the learner’s progression through the cycle.37
Implications for CE Providers and the Academy
If one of the ultimate goals of colleges and schools of pharmacy is to produce “CPD ready” self-directed, lifelong learning practitioners, colleges must incorporate the CPD activities throughout the curriculum and co-curriculum. Janke and Tofade published a statement in the American Journal of Pharmaceutical Education in 2014 on incorporating CPD into curriculums.38 Their review noted that self-directed lifelong learning activities should be intentional and coordinated and could begin with developing career goals.38
As a first step toward improving practice behaviors and patient outcomes, colleges and schools of pharmacy who are accredited CPE providers should consider “branching out” beyond knowledge-based programming. Increasing offerings toward application- and practiced-based activities, while aligning offerings with learner interests, will further meet the needs of learners and aid in facilitating change-driven impact in practice. A variety of bodies constitute ACPE CPE providers, including colleges and schools of pharmacy, professional associations, continuing education companies, health systems, and publishers. Arguably, given our mission, academia should drive change in continuing pharmacy education. Additionally, this shift would increase available scholarship and grantmanship opportunities for faculty members who seek to publish outcomes. Further, colleges could support employers wishing to implement the CPD approach to learning in their organizations. For medical center-affiliated CE providers, partnering with the Quality Improvement (QI) departments of partner health systems offers access to data to demonstrate commitment to delivering optimal care. In addition, formation of quality improvement focused education should be interprofessional in connection to the context of new health care delivery systems.2,3
More robust measures for continuing education outcomes must be developed and/or implemented. The academy’s CPD section (formerly known as the CPE section) is the logical place for these models to be developed and tested. Continuing education should be viewed not only as public outreach for colleges, but also as the strategic professional development vehicle that can drive change. Walsh proposed five levels for judging the value of CME: the number of participants; the degree of their satisfaction; the extent to which participants achieve activity objectives or measured increase in competence related to objectives; the degree of translation of new competence into performance of their duties; and the extent to which performance contributes to desired outcomes.39,40 Further efforts should be made toward capitalizing upon levels four and five. Moore’s outcome framework – which outlines seven levels of learner outcomes as participation, satisfaction, learning, competence, performance, patient health, and community health – provides an additional source of measuring the impact of CE programming.41
Given the challenges of adopting the CPD approach into the current CE infrastructure, models must be developed that remove barriers, maximize efficiencies, and decrease burden among all parties. Specific barriers such as funding for travel and time away from work could be mitigated by leveraging technology to facilitate learning. Communities of learners can be created with shared interests that foster innovation and promote sustainable programming that would be efficient in terms of financial resources. Health professionals have historically spent, on average, between 1 and 3 weeks per year at educational meetings.42,43 With the advancement of webinar technology, the industry is seeing significant growth in online learning. In 2015, 7,123 hours of live accredited CME activities were delivered through online means, in addition to the over 74,000 hours of enduring materials available online.44 As we are seeing increased utilization of online learning, careful construction of online communities will supplement live programs and offer new educational models.
Simulation will likely play a larger role in CPD (as seen in PharmD curriculums), particularly if a large number of practicing pharmacists must retool their skillset to assume direct patient care roles. Allowing for practice of skills in a safe environment, simulation can be helpful in achieving goals in CPD and support mastery-based learning.2
CONCLUSION
Societal expectations call for a safe, patient-centered, evidence-based, and efficient health care system. As our profession adapts to meet the needs of a value-based health care system, so, too, must our current continuing education system. Specific improvements for consideration should include a shift beyond an attendance-based credit system; increased focus on interprofessional learning and performance; and linkage of needs-assessment performance gaps with quality improvement. Incorporation of CPD to foster the professional development needs of practitioners can aid in achieving many of these improvements, while ensuring continued competence in practice. A CPD approach that includes CPE will facilitate outcomes-based positive change. Colleges and schools of pharmacy are poised to lead the shift toward self-directed lifelong learning.
ACKNOWLEDGMENTS
Marie Chisholm-Burns serves on the board of directors for ACPE. This paper does not necessarily represent the board’s views and only represents the authors’ views.
Footnotes
Copyright © 2005-2014 Accreditation Council for Pharmacy Education. Used with permission.
CPD Components
Reflect: Self-assessment of personal or organization needs or goals.
Plan: Defining objectives, creating formal and informal learning opportunities, defining measures of success, articulating plan with colleagues.
Learn: Implementing the personalized plan.
Evaluate: Assessing learning effectiveness and impact on performance and relevant outcomes.
Apply: Incorporating learned knowledge, skills, and attitudes into practice.
The following is an example of using the CPD model to facilitate practice change:
Pharmacist Jane Smith reflects on her practice and finds that non-adherence issues with diabetic patients during her MTM consultations are limiting the success of many of her MTM interventions. As a result of her reflection, she would like to incorporate motivational interviewing techniques during her MTM sessions in an attempt to improve patient outcomes. During the CPD planning phase, she develops SMART objectives for this goal (specific, measurable, agreed upon, realistic, and time-related) and develops and documents a plan for implementation. Her SMART goal is to incorporate motivational interviewing techniques for all diabetes-related MTM consultations starting next month. For her documented learning plan, she plans to review articles from the literature on motivational interviewing, participate in an online webinar for which she earns two CPE credit hours, and requests a “sit in” evaluation from the clinical coordinator of her division for verbal feedback. After applying the new interviewing techniques, she assesses whether medication adherence rates have improved in patients who she has provided care for and documents her achievement in her electronic portfolio for annual evaluation purposes.
REFERENCES
- 1.Vlasses PH. Pharmacy continuing education: 40 years ago to now. Ann Pharmacother. 2006;40(10):1854–1856. doi: 10.1345/aph.1H067. [DOI] [PubMed] [Google Scholar]
- 2.Sachdeva AK. Continuing professional development in the twenty-first century. J Contin Educ Health Prof. 2016;36(Suppl1):S8–S13. doi: 10.1097/CEH.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine (US) Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in the Health Professions. Washington, DC: National Academies Press (US); 2010. https://www.ncbi.nlm.nih.gov/books/NBK219811/. Accessed March 20, 2017.
- 4.Accreditation Council for Pharmacy Education. Accreditation standards for continuing pharmacy education. 2014. https://www.acpe-accredit.org/pdf/CPE_Standards_Final.pdf. Accessed March 20, 2017.
- 5.State CE. Requirements for Pharmacists. https://www.medscape.org/public/pharmcestaterequirements. Accessed: March 9, 2018.
- 6.Salinas GD. CME effectiveness: utilizing outcomes assessments of 600+ CME programs to evaluate the association between format and effectiveness. J Contin Educ Health Prof. 2015;35(Suppl1):S38–S39. doi: 10.1002/chp.21279. [DOI] [PubMed] [Google Scholar]
- 7.Fjortoft NF, Schwartz AH. Evaluation of a pharmacy continuing education program: long-term learning outcomes and changes in practice behaviors. Am J Pharm Educ. 2003;67(2) Article 35. [Google Scholar]
- 8.Cervero RM, Gaines JK. The impact of CME on physician performance and patient health outcomes: an updated synthesis of systematic reviews. J Contin Educ Health Prof. 2015;35(2):131–138. doi: 10.1002/chp.21290. [DOI] [PubMed] [Google Scholar]
- 9.Mazmanian PE, Davis DA, Galbraith R. Continuing medical education effect on clinical outcomes. Chest. 2009;135(3 Suppl):49S–55S. doi: 10.1378/chest.08-2518. [DOI] [PubMed] [Google Scholar]
- 10.De Almeida Neto AC, Benrimoj SI, Kavanagh DJ, Boakes RA. Novel educational training program for community pharmacists. Am J Pharm Educ. 2000;64(3):302–307. [Google Scholar]
- 11.Kimberlin CL, Berardo DH, Pendergast JF, McKenzie LC. Effects of an education program for community pharmacists on detecting drug-related problems in elderly patients. Med Care. 1993;31(5):451–468. doi: 10.1097/00005650-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Chalker J, Ratanawijitrasin S, Chuc NT, Petzold M, Tomson G. Effectiveness of a multi-component intervention on dispensing practices at private pharmacies in Vietnam and Thailand: a randomized controlled trial. Soc Sci Med. 2005;60(1):131–141. doi: 10.1016/j.socscimed.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Fjortoft N. The effectiveness of commitment to change statements on improving practice behaviors following continuing pharmacy education. Am J Pharm Educ. 2007;71(6) doi: 10.5688/aj7106112. Article 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dopp AL, Moulton JR, Rouse MJ, Trewet CB. A five-state continuing professional development pilot program for practicing pharmacists. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740228. Article 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarayani A, Rashidian A, Gholami K, Torkamandi H, Javadi M. Efficacy of continuing education in improving pharmacists' competencies for providing weight management service: three-arm randomized controlled trial. J Contin Educ Health Prof. 2012;32(3):163–173. doi: 10.1002/chp.21141. [DOI] [PubMed] [Google Scholar]
- 16.Dualde E, Font G, Santonja FJ, Faus MJ. Impact of pharmacists’ participation in a pharmacotherapy follow-up program. Am J Phar Educ. 2012;76(2) doi: 10.5688/ajpe76234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obreli-Neto PR, Marques dos Reis T, Guidoni CM, et al. A systematic review of the effects of continuing education programs on providing clinical community pharmacy services. Am J Pharm Educ. 2016;80(5) doi: 10.5688/ajpe80588. Article 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robertson MK, Umble KE, Cervero RM. Impact studies in continuing education for health professions: update. J Contin Educ Health Prof. 2003;23(3):146–156. doi: 10.1002/chp.1340230305. [DOI] [PubMed] [Google Scholar]
- 19. Travlos D. Baumgartner, J. ACPE Update. Lecture presented at: Alliance for Continuing Education in the Health Professions Annual Meeting. January 15, 2016.
- 20.Accreditation Council for Pharmacy Education. Guidance on continuing professional development (CPD) for the profession of pharmacy. 2015. https://www.acpeaccredit.org/pdf/CPDGuidance%20ProfessionPharmacyJan2015.pdf. Accessed March 20, 2017.
- 21.Norman GR, Shannon SI, Marrin ML. The need for needs assessment in continuing medical education. BMJ. 2004;328(7446):999–1001. doi: 10.1136/bmj.328.7446.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Colthart I, Bagnall G, Evans A, et al. The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME guide no. 10. Med Teach. 2008;30(2):124–145. doi: 10.1080/01421590701881699. [DOI] [PubMed] [Google Scholar]
- 23.Tran D, Tofade T, Thakkar N, Rouse M. US and international health professions’ requirements for continuing professional development. Am J Pharm Educ. 2014;78(6) doi: 10.5688/ajpe786129. Article 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quality assurance program. Ontario College of Pharmacists. http://www.ocpinfo.com/practice-education/qa-program/. Accessed July 10, 2017.
- 25.Austin Z, Croteau D, Marini A, Violato C. Continuous professional development: the Ontario experience in professional self-regulation through quality assurance and peer review. Am J Pharm Educ. 2003;67(2) Article 56. [Google Scholar]
- 26.Continuing professional development (CPD) FAQ. Pharmacy Board of Australia. http://www.pharmacyboard.gov.au/Codes-Guidelines/FAQ/CPD-FAQ.aspx. Accessed July 10, 2017.
- 27.Recertification Framework. Pharmaceutical Society of New Zealand. https://www.psnz.org.nz/Folder?Action=View%20File&Folder_id=94&File=framework%20with%20PCNZ%20logo.pdf. Accessed: March 9, 2017.
- 28.Authorised viewers. General Pharmaceutical Council. http://www.uptodate.org.uk/access/allowOthersAccess.shtml. Accessed July 10, 2017.
- 29.Young A, Chaudhry HJ, Pei X, Halbesleben K, Polk DH, Dugan M. A census of actively licensed physicians in the United States, 2014. J Med Reg. 2015;101(2):8–22. [Google Scholar]
- 30.Board of Pharmaceutical Specialties announces results of fall 2016 exams. 2017. http://www.bpsweb.org/2017/03/23/. Accessed April 5, 2017.
- 31.Bureau of Labor Statistics. Occupational Outlook Handbook. https://www.bls.gov/ooh/healthcare/pharmacists.htm. Accessed April 11, 2017.
- 32.Balmer JT. The transformation of continuing medical education (CME) in the United States. Adv Educ Pract. 2013;4:171–182. doi: 10.2147/AMEP.S35087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Earning MOC points. American Board of Internal Medicine. https://www.abim.org/maintenance-of-certification/earning-points.aspx. Accessed April 5, 2017.
- 34.Lipner RS, Brossman BG. Characteristics of internal medicine physicians and their practices that have differential impacts on their maintenance of certification. Acad Med. 2015;90(1):82–87. doi: 10.1097/ACM.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 35.Dopp AL, Moulton JR, Rouse MJ, Trewet CB. A five-state continuing professional development pilot program for practicing pharmacists. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740228. Article 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filipe HP, Silva ED, Stulting AA, Golnik KC. Continuing professional development: best practices. Middle East Afr. J. Ophthalmol. 2014;21(2):131–141. doi: 10.4103/0974-9233.129760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meštrović A, Rouse MJ. Pillars and foundations of quality for continuing education in pharmacy. Am J Pharm Educ. 2015;79(3) doi: 10.5688/ajpe79345. Article 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Janke KK, Tofade T. Making a curricular commitment to continuing professional development in doctor of pharmacy programs. Am J Pharm Educ. 2015;79(8) doi: 10.5688/ajpe798112. Article 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Walsh PL. Evaluating educational activities. In: Adelson R, Watkins FS, Caplan RM, eds. Continuing Education for the Health Professional: Educational and Administrative Methods. Rockville, MD: Aspen; 1985:71–100.
- 40.Moore DE, Green JS, Jay SJ, Leist JC, Maitland FM. Creating a new paradigm for CME: seizing opportunities within the health care revolution. J. Contin. Educ. Health Prof. 1994;14(1):1–28. [Google Scholar]
- 41.Moore DE, Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1–15. doi: 10.1002/chp.20001. [DOI] [PubMed] [Google Scholar]
- 42.Mansouri M, Lockyer J. A meta-analysis of continuing medical education effectiveness. J Contin Educ Health Prof. 2007;27(1):6–15. doi: 10.1002/chp.88. [DOI] [PubMed] [Google Scholar]
- 43.Owen PA, Allery LA, Harding KG, Hayes TM. General practitioners’ continuing medical education within and outside their practice. BMJ. 1989;299(6993):238–240. doi: 10.1136/bmj.299.6693.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Accreditation Council for Continuing Medical Education. 2015 Annual Report. http://www.accme.org/sites/default/files/630_20160719_2015_Annual_Report.pdf. Accessed April 5, 2017.