Abstract
Background
Mental stress-induced myocardial ischemia (MSIMI) is a frequent phenomenon in patients with coronary artery disease. Women with coronary artery disease tend to have more MSIMI and more chest pain/anginal symptoms than men, but whether the association between MSIMI and angina burden differs in women and men, is unknown.
Methods
This was a cross-sectional study with experimental manipulation of 950 individuals with stable coronary artery disease. Chest pain/angina frequency in the previous 4 weeks was assessed with the Seattle Angina Questionnaire’s angina-frequency subscale. MSIMI was assessed with myocardial perfusion imaging during mental stress (standardized public speaking task). Presence of MSIMI was based on expert readers and established criteria. A conventional (exercise or pharmacological) stress test was used as a control condition.
Results
Overall, 338 individuals (37%) reported angina; 112 (12%) developed MSIMI, and 256 (29%) developed conventional stress ischemia. Women who reported angina had almost double the probability to develop MSIMI (19% vs. 10%), adjusted prevalence rate ratio (PRR)= 1.90, 95% CI: 1.04-3.46), while there was no such difference in men (11% vs. 11%, adjusted PRR=1.09, 95% CI: 0.66-1.82). No association was found between angina symptoms and conventional stress ischemia for either women or men. Results for ischemia as a continuous variable were similar.
Conclusions
In women, but not in men, anginal symptoms may be a marker of vulnerability towards ischemia induced by psychological stress. These results highlight the psychosocial origins of angina in women, and may have important implications for the management and prognosis of women with angina.
Keywords: Cardiovascular disease, angina, ischemia, sex differences
Introduction
Mental stress-induced myocardial ischemia (MSIMI) is a transient myocardial ischemic response to mental stress,1 which can be induced in patients with coronary artery disease during a standardized mental stress challenge.1 MSIMI has a similar prognostic value compared to conventional stress ischemia (evaluated during standard cardiac testing) with a twofold increased risk of future cardiac events,2 but it occurs at lower levels of oxygen demand and is usually not related to severity of coronary artery disease.1, 3 MSIMI has been shown to correlate with myocardial ischemia measured in daily life ambulatory monitoring.3,4
Stable angina pectoris is an important determinant of adverse outcomes, quality of life and healthcare costs in coronary artery disease patients.5, 6 Psychosocial factors like depression are important correlates of anginal symptoms,7 and therefore myocardial ischemia triggered by emotional stress could be an underlying cause of daily life angina. This is particularly relevant for women, as women with coronary artery disease have a higher age-adjusted prevalence of reported angina,6 and also a higher prevalence of MSIMI,8 compared to men.
In a previous study of 98 coronary artery disease patients, we found a positive association between reported angina and MSIMI,9 but were not able to test an effect modification by sex due to the small sample size. In the current, larger study of 950 stable coronary artery disease patients, we sought to confirm this association, and examine whether it is more pronounced in women than in men.
Methods
Study Sample
Between June 2011 and March 2016, we enrolled 950 individuals (627 men, 323 women) with stable coronary artery disease in two parallel studies with similar protocols: the Mental Stress Ischemia: Prognosis and Genetic Influences Study (MIPS) (N=636) and the Myocardial Infarction and Mental Stress Study (MIMS) (N=314). Both studies shared testing and data collection protocols, as well as study staff, investigators, facilities and equipment, but there were some differences in the inclusion criteria (table 1). Since results were similar, we combined the data from these two studies. The MIMS study also recruited 112 community controls without coronary artery disease between the ages of 18 and 60 years, who were recruited from a community-based study of individuals without established coronary artery disease in the Atlanta area.10 This research was approved by the Emory University Institutional Review Board, and all participants provided informed consent.
Table 1.
Study Design Similarities and Differences between the Mental Stress Ischemia: Prognosis and Genetic Influences Study, or MIPS and Myocardial Infarction and Mental Stress Study, or MIMS
| Characteristics | MIPS Study | MIMS Study |
|---|---|---|
| Sample size | 636 | 314 |
| Age range | 30 to 80 years | 18 to 60 years |
| Sex ratio (M/F) | 70:30 | 50:50 |
| Inclusion criteria | Significant history of coronary artery disease during their lifetime:
|
Documented history of myocardial infarction within the previous 8 months |
| Common exclusion criteria |
|
|
| Study-specific exclusion criteria | Individuals with inflammatory diseases (like rheumatoid arthritis, lupus), on dialysis, or having any organ transplant excluded | No such exclusion criteria |
Stress Testing Procedures
Mental stress was induced by a standardized social stressor using a public speaking task, as previously described.11, 12 Briefly, each individual was asked to imagine a real-life stressful situation, and to make up a realistic story around this scenario. They were given two minutes to plan the story and three minutes to present it in front of a video camera and a small audience wearing white coats. Individuals were told that their speech would be evaluated by the laboratory staff for content, quality and duration. For physical stress, subjects underwent a Bruce protocol by walking on a treadmill, with exercise target set at 85% of maximum predicted heart rate based on the patient’s sex and age. For individuals who were unable to reach the heart rate target, we performed a pharmacological stress test with Regadenoson (Astellas, Northbrook, IL), an adenosine receptor agonist. We conducted continuous blood pressure and heart rate monitoring during both stresses.12
Myocardial Perfusion Imaging
Study participants with stable coronary artery disease underwent three single-photon emission tomography (SPECT) imaging studies at rest, with mental stress, and with conventional stress (treadmill or pharmacological stress), with 99mTc-Sestamibi, at the dose of 10-14 mCi for rest imaging and 30-40 mCi for stress imaging, based on weight. Stress scans were conducted on two separate days, one week apart, and the rest scan was obtained on the first visit. Community controls underwent a standardized mental stress challenge using the same protocol as the coronary artery disease patients, but they were not subjected to SPECT imaging or conventional stress testing.
SPECT images were interpreted using accepted methodology by two experienced readers blind to patients’ data using a 17-segment model. Each myocardial segment was scored from 0 (no abnormality) to 4 (absent perfusion), and summed scores were calculated in a conventional fashion by adding the individual segment scores, yielding two summed stress scores (SSS) for mental and conventional stress, respectively, and a summed rest score (SRS), each with a theoretical range of 0 to 68. A summed difference score (SDS) was calculated for each stress condition by subtracting SRS from SSS. The SDS is a semi-quantitative measure of the number and severity of reversible (ischemic) myocardial perfusion defects. Myocardial ischemia for both stress conditions was defined as an SDS ≥ 3.13 We also calculated the percent ischemic myocardium on a continuous scale as (SDS/68) × 100.14
Angina Assessment
Chest pain/angina during daily life was assessed with the Seattle Angina Questionnaire (SAQ)’s angina-frequency subscale, which measures frequency of angina and use of nitroglycerin for chest pain over the previous 4-weeks.15, 16 The SAQ angina questionnaire was validated in a variety of populations,15, 16 and was found to be correlated with electronic daily diary entries for angina and nitroglycerin use, both cross-sectionally and longitudinally.17 We categorized the SAQ angina frequency score as no chest pain/angina (score=100) or any chest pain/angina (score < 100).
Other Study Measures
Age was calculated by subtracting date of birth from date of enrollment, and then rounding to the nearest digit. We used validated instruments to collect demographic, behavioral, social and health status data for both coronary artery disease patients and community controls. Depressive symptoms were assessed using the Beck Depression Inventory (BDI-II), a 21-item self-administered scale;18 posttraumatic stress disorder (PTSD) symptoms were assessed using the PTSD Symptom Checklist (PCL: civilian version), a 17-item scale,19 and trait anxiety was measured with the State-Trait Anxiety Inventory (STAI).20 We also measured anger symptoms using the Spielberger’s State-Trait Anger Expression Inventory (STAXI);21 and general perceived stress using the Perceived Stress Scale.22
Statistical Analysis
We compared subject characteristics according to presence or absence of chest pain/angina in the previous 4-weeks using either the two-sample t-test for continuous, normally distributed variables or the chi-square test for categorical variables. For our main analyses, we performed multivariable linear and log-binomial regression models with percent ischemic myocardium and presence/absence of ischemia as outcomes, respectively, and presence of angina as the main predictor variable. Log-binomial models allowed calculation of prevalence risk ratios (PRR) adjusted for other factors. We adjusted for a priori chosen covariates, including sociodemographic characteristics (age, sex, race, poverty status), coronary artery disease risk factors (smoking status, hypertension, dyslipidemia, diabetes, BMI) and coronary artery disease severity indicators (history of myocardial infarction, heart failure and revascularization). In a separate model, we considered sex as effect modifier for the association between angina and ischemia. We used SAS version 9.3 (Cary, NC) for the analysis, with 95% significance threshold for confidence intervals (CI).
Results
Of the 950 coronary artery disease patients included, 913 had complete data on angina and myocardial perfusion imaging with mental stress. The mean age of these subjects was 60 years (standard deviation, 10), 309 (34%) were women and 370 (41%) were African-American. Overall, 338 (37%) reported having chest pain/angina symptoms over the previous four weeks (table 2), and women reported more angina than men (50% vs 30%). Participants reporting angina were also younger and more likely to be African-American, smokers and with income below the poverty line compared with those without angina. As expected, coronary artery disease risk factors were highly prevalent in this sample, with 77% having hypertension, 82% with dyslipidemia, 33% with diabetes, and 77% with history of previous revascularizations. Of the coronary artery disease risk factors and severity indicators, only history of myocardial infarction was significantly associated with angina: 65% of patients reporting angina had a history of myocardial infarction vs. 46% of those not reporting angina. In contrast, all measures of psychological distress were significantly higher in subjects with angina as compared to subjects without angina. For example, the level of depressive symptoms was approximately twice as high, and the levels of PTSD symptoms and of perceived stress were approximately 50% as high in those reporting angina compared with those not reporting angina (table 2).
Table 2.
Descriptive characteristics of the coronary artery disease patients in the study according to angina frequency score categories
| Variables | No angina in past 4 weeks (N= 575) | Angina in past 4 weeks (N= 338) | Total population (N= 913) |
|---|---|---|---|
| Demographic factors | |||
| Age, Mean (SD)a | 62 (10) | 56 (10) | 60 (10) |
| Women, N (%)a | 154 (27%) | 155 (46%) | 309 (34%) |
| African-American, N (%)a | 190 (33%) | 180 (53%) | 370 (41%) |
| Below poverty line, N (%)a | 74 (13%) | 110 (34%) | 184 (21%) |
| Current smokers, N (%)a | 65 (11%) | 80 (24%) | 145 (16%) |
|
| |||
| Medical factors | |||
| Hypertension, N (%) | 437 (76%) | 267 (79%) | 704 (77%) |
| Dyslipidemia, N (%) | 494 (86%) | 255 (75%) | 749 (82%) |
| Diabetes, N (%) | 184 (32%) | 114 (34%) | 298 (33%) |
| BMI, Mean (SD) | 30 (5) | 31 (7) | 30 (6) |
| Previous MI, N (%)a | 269 (47%) | 220 (65%) | 489 (54%) |
| History of Heart failure, N (%) | 72 (13%) | 46 (14%) | 118 (13%) |
| Previous Revascularization, N (%) | 440 (77%) | 264 (78%) | 704 (77%) |
| Ejection fraction in %, Mean (SD) | 68 (13) | 69 (13) | 69 (14) |
| coronary artery disease ≥ 70% stenosis, N (%)b,c | 430 (85%) | 242 (80%) | 672 (84%) |
| Resting perfusion defects, % myocardium, Mean (SD) | 7 (13) | 7 (11) | 7 (12) |
|
| |||
| Psychological factors | |||
| BDI-II score, Mean (SD)a | 7 (7) | 14 (11) | 10 (9) |
| STAI Anxiety-Trait score, Mean (SD)a | 32 (10) | 39 (12) | 35 (11) |
| STAXI Anger-Trait score, Mean (SD)a | 14 (4) | 16 (5) | 15 (4) |
| PCL score, Mean (SD)a | 25 (9) | 34 (15) | 28 (13) |
| Perceived-stress score, Mean (SD)a | 12 (7) | 17 (8) | 14 (8) |
SD: Standard Deviation; MI: Myocardial Infarction; BMI: Body Mass Index; coronary artery disease: Coronary Artery Disease; BDI: Beck Depression Inventory; STAI: State- Trait Anxiety Inventory; STAXI: State-Trait Anger Expression Inventory; PCL: PTSD Symptom Checklist (Civilian)
P value < 0.05
108 observations missing
coronary artery disease severity based on coronary angiography results prior to revascularization procedures (if any)
Of the 112 community controls, two were excluded because of missing angina data. The mean age of the remaining 110 control subjects was 50 years (standard deviation, 9), 57 (52%) were women and 46 (42%) were African-American. Overall, 11 (10%) of the controls reported angina in the past 4 weeks even though none of them had a previous history of coronary artery disease. In contrast to the coronary artery disease patients, this proportion was only slightly elevated in women (12%) compared with men (8%), p=0.53. Similar to the coronary artery disease patients, community controls who reported angina showed significantly higher symptoms of depression, anxiety, PTSD and perceived stress compared to controls who did not report angina (supplementary table 1).
Overall, 112 (12%) of the coronary artery disease patients developed ischemia with mental stress, and 256 (29%) developed ischemia with conventional stress. Both forms of ischemia tended to be more common in women than in men (15% vs. 11% for mental stress, 30% vs. 28% for conventional stress). In the full cohort, chest pain/angina in the previous 4 weeks was associated with 37% higher probability of MSIMI (adjusted PRR: 1.37, 95% CI: 0.93 - 2.01), after adjustment by sociodemographic characteristics, coronary artery disease risk factors and coronary artery disease severity indicators; the corresponding association for conventional stress ischemia was 1.17 (95% CI: 0.93 - 1.47) (table 3). However, sex differences were noted. Of the women reporting angina, 19% developed MSIMI, vs. 10% of women not reporting angina (adjusted PRR= 1.90, 95% CI: 1.04 - 3.46), while there were no differences among men (11% vs. 11% respectively, adjusted PRR= 1.09, 95% CI: 0.66 - 1.82), interaction p= 0.16 (table 4). For ischemia as a continuous measure, results were similar. Women who reported angina exhibited over twofold more ischemic myocardium with mental stress as compared to women without angina, although the absolute difference was small, 1.8% of ischemic myocardium vs. 0.8% (table 4), while there was no such difference in men (1.2% of ischemic myocardium vs. 1.0%), interaction p= 0.04. Women with angina also showed a greater percent of ischemic myocardium with mental stress than men with or without angina, while results for conventional stress were comparable across groups of sex and angina status (figure 1). Even when the analysis was restricted to ischemia positive subjects (45 women and 67 men), women reporting angina tended to show greater severity of ischemia than those who did not (8.9% of ischemic myocardium vs 7.5%), which was not the case among men (7.7% vs. 7.4%). Adjustment for depression and anxiety did not change the results (data not shown).
Table 3.
Association between presence of reported angina in past 4 weeks and myocardial perfusion defects with mental or conventional (exercise or pharmacological) stress, in the full sample (N = 913)
| Risks and risk ratios for ischemia (categorical variable), angina vs. no angina
| ||||
|---|---|---|---|---|
| Frequency of Ischemia | ||||
| No angina | Angina | Unadjusted PRR (95% CI) |
Adjusted PRRa (95% CI) |
|
| Mental stress | 11% | 15% | 1.42 (1.01 to 2.01) | 1.37 (0.93 to 2.01) |
| Conventional stressb | 28% | 31% | 1.13 (0.92 to 1.39) | 1.17 (0.93 to 1.47) |
|
| ||||
| Percent of ischemic myocardium (continuous variable), angina vs. no angina | ||||
|
| ||||
| Percent Ischemic Myocardium | ||||
| No angina | Angina | Unadjusted β (95% CI) |
Adjusted βa (95% CI) |
|
|
| ||||
| Mental stress | 0.95% | 1.46% | 0.52 (0.13 to 0.90) | 0.48 (0.05 to 0.90) |
| Conventional stressb | 3.32% | 3.35% | −0.03 (−0.85 to 0.79) | 0.33 (−0.56 to 1.23) |
PRR (prevalence risk ratio): Estimated prevalence of having mental or conventional stress ischemia in subjects with angina in the past 4 weeks, compared with subjects with no angina
β: Estimated difference in mental/conventional stress ischemia percentage score between subjects with angina vs. no angina in the past 4 weeks
Adjusted for demographic factors (age, sex, race, and poverty status), coronary artery disease risk factors (current smoking status, hypertension, dyslipidemia, diabetes, and body mass index), and coronary artery disease severity indicators (previous myocardial infarction, history of heart failure, and history of revascularization)
For conventional stress, 22 observations were missing, with final sample size = 891
Table 4.
Association between presence of reported angina in past 4 weeks and myocardial perfusion defects with mental or conventional (exercise or pharmacological) stress, by sex
| Men N = 601) |
Women (N = 306) |
|||||
|---|---|---|---|---|---|---|
| Risks and risk ratios for ischemia (categorical variable), angina vs. no angina | ||||||
|
| ||||||
| Frequency of Ischemia | Frequency of Ischemia | |||||
| No angina | Angina | Adjusted PRRa (95% CI) |
No angina | Angina | Adjusted PRRa (95% CI) |
|
|
| ||||||
| Mental stress | 11% | 11% | 1.09 (0.66 to 1.82) | 10% | 19% | 1.90 (1.04 to 3.46) |
| Conventional stressb | 28% | 29% | 1.09 (0.82 to 1.45) | 27% | 33% | 1.33 (0.92 to 1.90) |
|
| ||||||
| Percent of ischemic myocardium (continuous variable), angina vs. no angina | ||||||
|
| ||||||
| Percent Ischemic Myocardium | Percent Ischemic Myocardium | |||||
| No angina | Angina | Adjusted βa (95% CI) |
No angina | Angina | Adjusted βa (95% CI) |
|
|
| ||||||
| Mental stress | 1.01% | 1.15% | 0.15 (−0.37 to 0.67) | 0.81% | 1.81% | 1.03 (0.36 to 1.70) |
| Conventional stressb | 3.31% | 3.52% | 0.21 (−0.88 to 1.31) | 2.98% | 3.62% | 0.65 (−0.77 to 2.06) |
PRR (prevalence risk ratio): Estimated prevalence of having mental or conventional stress ischemia in subjects with angina in the past 4 weeks, compared with subjects with no angina
β: Estimated difference in mental/conventional stress ischemia percentage score between subjects with angina vs. no angina in the past 4 weeks
Adjusted for demographic factors (age, sex, race, and poverty status), coronary artery disease risk factors (current smoking status, hypertension, dyslipidemia, diabetes, and body mass index), and coronary artery disease severity indicators (previous myocardial infarction, history of heart failure, and history of revascularization).
For conventional stress, 22 observations were missing, with final sample size = 891
Figure 1. Percent of Ischemic Left Ventricular Myocardium with Mental Stress and Conventional Stress, According to Presence or Absence of Reported Angina in Past 4 weeks and Sex.
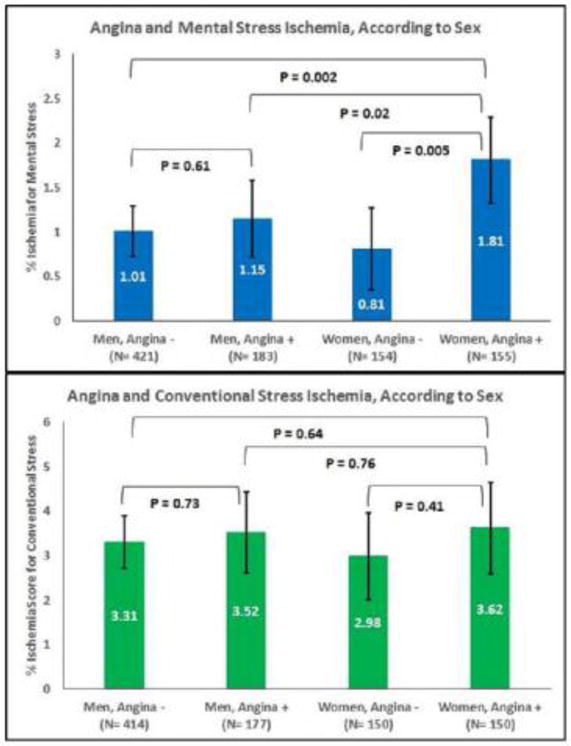
Shown are mental-stress (upper panel) and conventional stress (lower panel) mean percent of ischemic myocardium and 95% confidence intervals according to angina category and sex. Numbers on bars indicate the mean, error bars indicate 95% CI.
Discussion
Among individuals with stable coronary artery disease, reported chest pain/angina in previous 4-weeks was associated with myocardial ischemia due to mental stress measured on the continuous scale, but not with conventional stress. These results are consistent with existing literature,23-25 and replicate our previous findings.9 The association between angina and MSIMI was mainly driven by women, as women with angina showed more ischemic myocardium than any of the other groups. These findings were independent of traditional coronary artery disease risk factors and even psychosocial factors.
As MSIMI is associated with ambulatory ischemia,3, 4 reported chest pain/angina might reflect ischemic episodes triggered by psychological stress in daily life. Based on our results, this phenomenon may be especially important for women, and may potentially be implicated in sex differences in prognosis of coronary artery disease.6
Given our observation that reported chest pain/angina in the previous 4 weeks was related to ischemia provoked by mental stress but not by conventional stress, it is unlikely that our results merely reflect a lower pain threshold, or a higher propensity to report chest pain, in women compared with men.26 Our finding of only a small sex difference in reported chest pain among community controls further corroborates that sex differences in pain perception or in pain reporting should not play an important role in these findings, although the small sample of community controls in our study precludes us from drawing any definitive conclusions.
Several previous studies have found no association between angina reported during daily life and either myocardial ischemia due to exercise stress,25 or measures of coronary artery disease severity like previous myocardial infarction, previous stenting and coronary artery bypass surgery.23 Also, in the Psychophysiological Investigations of Myocardial Ischemia (PIMI) study, exercise stress ischemia was not associated with history of daily life angina.24 These results are also consistent with our previously published data based on a separate sample of coronary artery disease patients.9 While the underlying biological reason for these findings will need further research, it is possible that a predominant mechanism of chest pain in daily life is coronary microvascular dysfunction, which is not detectable with conventional perfusion scans.27 Coronary microvascular dysfunction has been implicated as a mechanism of MSIMI, especially in women.27, 28 Furthermore, coronary microvascular disease has been proposed as the underlying etiology for angina and ischemic heart disease in women in absence of obstructive coronary artery disease.29, 30
Alternatively, reported angina can be a marker of psychological distress. This is suggested by the consistent association we observed between chest pain/angina and symptoms of psychosocial distress such as depression, anxiety and perceived stress, in both patients and controls, consistent with many previous reports,7, 31 including our own previous work.9 However, in this study, the psychosocial profile of coronary artery disease patients did not explain the association between angina and MSIMI, suggesting that other factors may be at play.
Our study has several strengths. This is the largest study to date with measurements of ischemia with both mental stress and conventional stress, and detailed assessments of psychosocial, behavioral and clinical factors. Furthermore, we had a relatively large representation of women and minorities. Main limitations include the cross-sectional study design, and the retrospective assessment of chest pain/angina. However, the SAQ is well validated, and because it was administered prior to stress testing, it is unlikely that responses to the SAQ were biased by the testing itself. Another limitation of our findings is the lack of a significant sex-based interaction when assessing mental stress ischemia as a dichotomous outcome. However, the interaction was significant when ischemia was measured on a continuous scale. A loss of power due to categorizing a continuous variable32 might be implicated.
Our results have important clinical implications for the management of angina and the improvement of quality of life and prognosis of women with coronary artery disease. Specifically, our data points to the importance of assessing psychosocial stress in patients who report angina, especially women. Daily life angina is an important dimension of the quality of life of coronary artery disease patients, and a thorough assessment of the psychosocial sphere may help improve the care of these patients. When indicated, women with angina may benefit from stress-reduction interventions, given that such interventions have shown efficacy in ameliorating depression and anxiety symptoms in coronary artery disease patients, in addition to improving cardiovascular risk factors such as systolic blood pressure.33, 34 However, stress-reduction management strategies need to be specifically investigated in future studies for their efficacy in decreasing angina symptoms.
In conclusion, we found that among women with coronary artery disease, reported chest pain in daily life is positively associated with myocardial ischemia provoked by mental stress, but not by conventional stress. Our results suggest that psychosocial and neurobiological mechanisms may be shared between MSIMI and symptoms of angina in daily life in women, and highlight the importance of psychosocial determinants of chest pain in daily life among women with coronary artery disease.
Supplementary Material
Clinical Significance.
Women with stable coronary artery disease report more chest pain/anginal symptoms than men, but these differences are not well understood.
Women with coronary artery disease who report angina, but not men, are twice more likely to develop ischemia with a laboratory based acute psychological stressor than those without angina.
These results suggest an important psychosocial component for angina in women, which has implications for the management of women with angina.
Acknowledgments
Funding Sources: This work was supported by the National Institutes of Health (P01 HL101398, R01HL109413, R01HL109413-02S1, K24HL077506, K24 MH076955, UL1TR000454, KL2TR000455, and THL130025A). The sponsors of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Access: All the authors had access to the data; and a significant contribution in either data collection and/or design, data analysis, and execution of the manuscript. All authors contributed to the writing of the manuscript.
Conflict of Interest: Dr. Vaccarino and Dr. Quyyumi report research support from NIH. Ernest V. Garcia receives royalties from the sale of the Emory Cardiac Toolbox, used for some analyses in this study. None of the other co-authors report any conflict of interest
References
- 1.Strike PC, Steptoe A. Systematic review of mental stress-induced myocardial ischaemia. European heart journal. 2003;24:690–703. doi: 10.1016/s0195-668x(02)00615-2. [DOI] [PubMed] [Google Scholar]
- 2.Wei J, Rooks C, Ramadan R, et al. Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. Am J Cardiol. 2014;114:187–192. doi: 10.1016/j.amjcard.2014.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blumenthal JA, Jiang W, Waugh RA, et al. Mental stress-induced ischemia in the laboratory and ambulatory ischemia during daily life. Association and hemodynamic features. Circulation. 1995;92:2102–2108. doi: 10.1161/01.cir.92.8.2102. [DOI] [PubMed] [Google Scholar]
- 4.Stone PH, Krantz DS, McMahon RP, et al. Relationship among mental stress-induced ischemia and ischemia during daily life and during exercise: The psychophysiologic investigations of myocardial ischemia (PIMI) Study. Journal of the American College of Cardiology. 1999;33:1477–1484. doi: 10.1016/s0735-1097(99)00075-3. [DOI] [PubMed] [Google Scholar]
- 5.Spertus JA. Evolving applications for patient-centered health status measures. Circulation. 2008;118:2103–2110. doi: 10.1161/CIRCULATIONAHA.107.747568. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayek SS, Ko YA, Awad M, et al. Depression and chest pain in patients with coronary artery disease. International journal of cardiology. 2017;230:420–426. doi: 10.1016/j.ijcard.2016.12.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaccarino V, Wilmot K, Al Mheid I, et al. Sex Differences in Mental Stress-Induced Myocardial Ischemia in Patients With Coronary Heart Disease. Journal of the American Heart Association. 2016;5 doi: 10.1161/JAHA.116.003630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pimple P, Shah AJ, Rooks C, et al. Angina and mental stress-induced myocardial ischemia. Journal of psychosomatic research. 2015;78:433–437. doi: 10.1016/j.jpsychores.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris AA, Zhao L, Ahmed Y, et al. Association between depression and inflammation–differences by race and sex: the META-Health study. Psychosom Med. 2011;73:462–468. doi: 10.1097/PSY.0b013e318222379c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufmann PG, M R, Becker LC, Bertolet B, Bonsall R, Chaitman B, Cohen JD, Forman S, Goldberg AD, Freedland K, Ketterer MW, Krantz DS, Pepine CJ, Raczynski J, Stone PH, Taylor H, Knatterud GL, Sheps DS. The Psychophysiological Investigations of Myocardial Ischemia (PIMI) study: objective, methods, and variability of measures. Psychosom Med. 1998 doi: 10.1097/00006842-199801000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Hammadah M, Al Mheid I, Wilmot K, et al. The Mental Stress Ischemia Prognosis Study: Objectives, Study Design, and Prevalence of Inducible Ischemia. Psychosomatic medicine. 2017;79:311–317. doi: 10.1097/PSY.0000000000000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramachandruni S, Fillingim RB, McGorray SP, et al. Mental stress provokes ischemia in coronary artery disease subjects without exercise- or adenosine-induced ischemia. Journal of the American College of Cardiology. 2006;47:987–991. doi: 10.1016/j.jacc.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 14.Holly TA, Abbott BG, Al-Mallah M, et al. Single photon-emission computed tomography. J Nucl Cardiol. 2010;17:941–973. doi: 10.1007/s12350-010-9246-y. [DOI] [PubMed] [Google Scholar]
- 15.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 16.Kimble LP, Dunbar SB, Weintraub WS, et al. The Seattle angina questionnaire: reliability and validity in women with chronic stable angina. Heart disease (Hagerstown, Md) 2002;4:206–211. doi: 10.1097/00132580-200207000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold SV, Kosiborod M, Li Y, et al. Comparison of the Seattle Angina Questionnaire With Daily Angina Diary in the TERISA Clinical Trial. Circulation Cardiovascular quality and outcomes. 2014;7:844–850. doi: 10.1161/CIRCOUTCOMES.113.000752. [DOI] [PubMed] [Google Scholar]
- 18.Beck AT, Steer RA, Brown GK. BDI-II Beck Depression Inventory: Second Edition. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 19.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behavioral Research & Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 20.Spielberger CD, Gorsuch RL, Lushene RE. State-Trait Anxiety (STAI) manual. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 21.Spielberger CD. Professional manual for the State-Trait Anger Expression Inventory. Tampa, Fla: University of South Florida; 1988. Research Ed. [Google Scholar]
- 22.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 23.Ketterer MW, Bekkouche NS, Goldberg AD, McMahon RP, Krantz DS. Symptoms of anxiety and depression are correlates of angina pectoris by recent history and an ischemia-positive treadmill test in patients with documented coronary artery disease in the pimi study. Cardiovascular psychiatry and neurology. 2011;2011:134040. doi: 10.1155/2011/134040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheps DS, McMahon RP, Pepine CJ, et al. Heterogeneity among cardiac ischemic and anginal responses to exercise, mental stress, and daily life. The American journal of cardiology. 1998;82:1–6. doi: 10.1016/s0002-9149(98)00228-8. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan MD, Ciechanowski PS, Russo JE, et al. Angina pectoris during daily activities and exercise stress testing: The role of inducible myocardial ischemia and psychological distress. Pain. 2008;139:551–561. doi: 10.1016/j.pain.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 26.Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. British journal of anaesthesia. 2013;111:52–58. doi: 10.1093/bja/aet127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pepine CJ, Petersen JW, Bairey Merz CN. A microvascular-myocardial diastolic dysfunctional state and risk for mental stress ischemia: a revised concept of ischemia during daily life. JACC Cardiovascular imaging. 2014;7:362–365. doi: 10.1016/j.jcmg.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Wokhlu A, Pepine CJ. Mental Stress and Myocardial Ischemia: Young Women at Risk. Journal of the American Heart Association. 2016;5 doi: 10.1161/JAHA.116.004196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reis SE, Holubkov R, Conrad Smith AJ, et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. American heart journal. 2001;141:735–741. doi: 10.1067/mhj.2001.114198. [DOI] [PubMed] [Google Scholar]
- 30.Dean J, Cruz SD, Mehta PK, Merz CN. Coronary microvascular dysfunction: sex-specific risk, diagnosis, and therapy. Nature reviews Cardiology. 2015;12:406–414. doi: 10.1038/nrcardio.2015.72. [DOI] [PubMed] [Google Scholar]
- 31.Jespersen L, Abildstrom SZ, Hvelplund A, Prescott E. Persistent angina: highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life in stable angina pectoris. Clinical research in cardiology : official journal of the German Cardiac Society. 2013;102:571–581. doi: 10.1007/s00392-013-0568-z. [DOI] [PubMed] [Google Scholar]
- 32.Ragland DR. Dichotomizing continuous outcome variables: dependence of the magnitude of association and statistical power on the cutpoint. Epidemiology (Cambridge, Mass) 1992;3:434–440. doi: 10.1097/00001648-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Metin ZG, Ejem D, Dionne-Odom JN, et al. Mind-Body Interventions for Individuals with Heart Failure: a Systematic Review of Randomized Trials. Journal of cardiac failure. 2017 doi: 10.1016/j.cardfail.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Younge JO, Gotink RA, Baena CP, Roos-Hesselink JW, Hunink MG. Mind-body practices for patients with cardiac disease: a systematic review and meta-analysis. European journal of preventive cardiology. 2015;22:1385–1398. doi: 10.1177/2047487314549927. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


