Abstract
Background
Patients are frequently discharged from the hospital before all test results have been finalized. Thirty to 40% of tests pending at discharge (TPADs) return potentially actionable results that could necessitate change in the patients’ management, often unbeknownst to their physicians. Delayed follow-up of TPADs can lead to patient harm. We sought to synthesize the existing literature on interventions intended to improve the management of TPADs, including interventions designed to enhance documentation of TPADs, increase physician awareness when TPAD results finalize post-discharge, decrease adverse events related to missed TPADs, and increase physician satisfaction with TPAD management.
Methods
We searched Medline, EMBASE, CINAHL, Cochrane Database of Systematic Reviews, Cochrane Database of Controlled Clinical Trials and Medline (January 1, 2000–November 10, 2016) for randomized controlled trials and prospective, controlled observational studies that evaluated interventions to improve follow-up of TPADs for adult patients discharged from acute care hospitals or emergency department settings. From each study we extracted characteristics of the intervention being evaluated and its impact on TPAD management.
Results
Nine studies met the criteria for inclusion. Six studies evaluated electronic discharge summary templates with a designated field for documenting TPADs, and three of six of these studies reported a significant improvement in documentation of TPADs in discharge summaries in pre- and post-intervention analysis. One study reported that auditing discharge summaries and providing feedback to physicians were associated with improved TPAD documentation in discharge summaries. Two studies found that email alerts when TPADs were finalized improved physicians' awareness of the results and documentation of their follow-up actions. Of the four studies that assessed patient morbidity, two showed a positive effect; however, none specifically measured the impact of their interventions on downstream patient harm due to delayed follow-up of TPADs. Three studies surveyed physicians’ attitudes towards the interventions, of which two studies reported improved physician satisfaction with TPAD management with the implementation of an enhanced discharge template and a notification system when TPADs finalize.
Discussion
Discharge summary templates, educational interventions for discharging physicians, and email alerts when TPAD results are finalized show promise in improving management of TPADs. Given the complexity of the processes necessary to ensure follow-up of TPADs, rigorous evaluations of multifaceted interventions (e.g., improved discharge documentation of TPADs combined with email alerts when results become available) is needed.
Electronic supplementary material
The online version of this article (10.1007/s11606-017-4290-9) contains supplementary material, which is available to authorized users.
KEY WORDS: patient discharge, communication, hospital medicine
Background
Tests pending at discharge (TPADs) are investigations that are collected during a patient’s hospitalization, but the final results of which are incomplete at the time of discharge.1 Between 41% and 100% of patients leave hospital with at least one TPAD, influenced in part by pressure on inpatient physicians to reduce length of stay.1,2,8 Approximately 30% to 40% of finalized TPAD results are likely to change patients’ management,1 so timely follow-up is vital to ensure diagnosis and treatment are not delayed.4–7
To avoid discontinuity when patient care is transferred from inpatient physicians in the hospital setting to primary care providers (PCPs) in the community,9 a plan to follow-up any TPADs must be created as part of the discharge process, documented in the discharge summary, and shared with the patient’s outpatient physicians. Unfortunately, studies show that discharge summaries often fail to include TPADs requiring follow-up.9
After patients are discharged, their physicians must be notified when TPAD results become available so appropriate follow-up actions can be taken.1 Surveys of inpatient physicians have shown that they are often unaware of the majority of the results of their discharged patients’ finalized TPAD results,1–3 and PCPs face barriers in accessing patients’ test results from their hospitalization.10 Thus, many physicians are dissatisfied with current models for managing TPADs.2
We sought to synthesize the existing literature on interventions intended to improve the management of TPADs, including interventions designed to document TPADs, increase physician awareness when TPAD results finalize post-discharge, decrease adverse events related to missed TPADs, and increase physician satisfaction with TPAD management.
Methods
Identification and Selection of Studies
We searched Medline, EMBASE (excluding book and conference materials), CINAHL, Cochrane Database of Systematic Reviews, Cochrane Database of Controlled Clinical Trials, and PubMed (for publisher-supplied citations) for studies on diagnostic tests, continuity of patient care or tests pending, and patient discharged from any clinical setting, published from January 1, 2000, to November 10, 2016 (Appendix A). No language limits were applied. We set the year 2000 as a lower limit, as few relevant articles exist prior to this time, and modern EHRs render older studies obsolete.
We selected studies for inclusion if they met the following criteria: (1) the intervention related to improving management of TPADs in a medicine inpatient ward or Emergency Department (ED) setting; (2) the study analyzed original data and was a random control trial (RCT) or prospective observational study with comparator; (3) the study involved adult patients; (4) the study measured an outcome related to patient mortality, morbidity, or impact on the process of healthcare delivery (Appendix B). This process was conducted by two reviewers, with any disagreements resolved by a senior reviewer.
Data Extraction
Using a structured data extraction instrument (Appendix C) modeled after previous work by Haynes,11 we collected basic identifying information [authorship, full manuscript publication (yes/no), publication date, funding source], study design (RCT or prospective observation study with pre/post analysis), setting (inpatient medicine ward or ED), and details of the intervention. As per Haynes’ methodology, a study was deemed effective if the intervention resulted in a positive effect in ≥ 50% of the study’s primary outcomes, and ineffective otherwise.11
Study Appraisal
Recognizing that no single validated appraisal instrument fit our needs because of the heterogeneity of eligible articles, we developed a structured study quality tool derived from existing instruments with guidance from a senior co-author who is a recognized expert in systematic reviews.22 In particular, we determined that a high-quality study of a TPAD intervention would include the following: (1) the demographics and comorbidities of enrolled patients (‘Patient Data’); (2) the level of training (e.g., clerk, nurse, medical resident) of the discharging staff member; (3) a definition of the particular TPADs of interest (‘TPAD Definition’); (4) a definition of the clinical significance of the TPAD (‘Actionable TPAD Definition’); (5) an outcome measure directly related to TPADs (e.g., physician awareness of TPAD result) (‘TPAD Outcome’); (6) discussion of the cost of implementation and maintenance of the intervention (‘Cost’); (7) an outcome measure related to the satisfaction of staff members using the intervention (‘Intervention Usability’). Thus, each study was judged as meeting or not meeting each of these criteria and assigned a score ranging from zero to seven.
Results
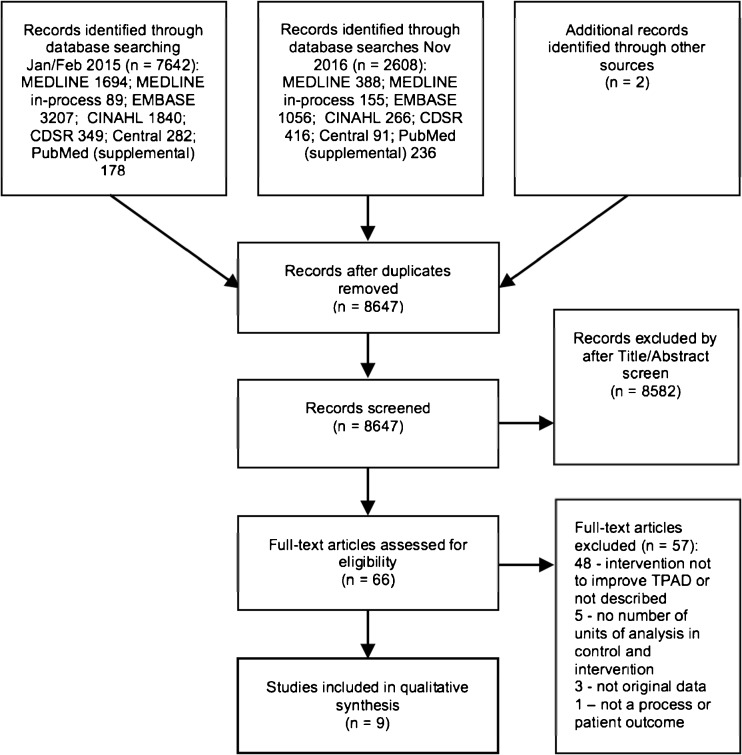
Our literature search (Fig. 1) identified 10,252 citations (8647 excluding duplicates). After brief screening by title and abstract, we reviewed the full text of 66 manuscripts and identified 9 studies that met all inclusion criteria (Fig. 1).12–20 As evident in our findings from the study quality appraisal and overview of the intervention characteristics, the nine included studies were heterogeneous with respect to design and outcomes (Table 1). In subsequent sections we appraise the studies’ designs; general categories of interventions that have been tested and their characteristics; and the efficacy of these interventions to improve documentation of TPADs, increase physician awareness when TPAD results finalize post-discharge, decrease adverse events related to missed TPADs, and improve physician satisfaction with TPAD management.
Figure 1.
PRISMA flow diagram of included and excluded studies for January 1, 2000, to November 10, 2016
Table 1.
Summary of Included Studies*
| Study | Study design | Study setting | Targeted TPAD type | Intervention | Unit of analysis | Primary outcome(s) | Outcome type | TPAD outcome |
|---|---|---|---|---|---|---|---|---|
| Balaban12 | RCT | Medicine ward | Not described | Discharge summary template that includes TPADS, electronic transfer of discharge summary to primary care RN, RN discharge facilitator, PCP feedback on post-discharge care plan | Patient | 1. No outpatient appointment within 21 days with either an MD or NP at the patient’s primary care site or with a relevant specialist 2. Readmission, for any reason, within 31 days to any of three study hospitals 3. Emergency department visits within 31 days for a problem related to the original admission in any of the 3 CHA hospitals 4. Failure to complete an outpatient workup recommended by a hospital doctor |
Patient, process | No |
| Dalal13 | RCT | Medicine ward | Microbiology, radiology, biochemistry, hematology | Automated email alerts to discharging physician of finalized test results | Physician | Self-reported awareness of TPAD results by discharging physician | Process | Yes |
| Dinescu14 | POS | Medicine ward | Not described | Audit of discharge summary quality (including TPADs) and feedback loop | Patient | 1. Admission composite score 2. Hospital course composite score 3. Discharge planning composite score 4. Post-discharge care composite score (including test results to follow-up) |
Process | Yes |
| El-Kareh15 | RCT | Medicine ward | Microbiology | Automated email alerts to discharging physician of finalized microbiology test results of possibly inadequately infections | TPAD | Documentation in the patient’s outpatient electronic chart of documentation of follow-up action within 3 days of the post-discharge microbiology result finalizing (note contains acknowledgement of the result, follow-up with the patient, or new antibiotic prescription) | Process | Yes |
| Graumlich16 | RCT | Medicine ward | Not described | Electronic discharge template prompts discharging physician to enter TPADs | Patient | Proportion of patients readmitted at least once within 6 months after the index hospitalization | Patient | No |
| Kantor17 | POS | Medicine ward | Microbiology, hematology, biochemistry, pathology | Electronic discharge application prompts to include TPADs from automatically generated list | TPAD, discharge summary | 1. Proportion of pending studies communicated in discharge summary 2. Proportion of discharge summaries communicated all pending studies |
Process | Yes |
| O’Leary18 | POS | Medicine ward | Not described | Electronic discharge with template (including TPADs), automated distribution to PCP | DSCS, TPAD | 1. Discharge Summary Completeness Score (DSCS) (out of 100) 2. Pending tests documented in discharge summary |
Process | Yes |
| Cadwallader19 | POS | Medicine ward | Not described | Electronic discharge template requires TPADs manual entry | Discharge summary | Percentage of tests with pending results that were documented in the discharge summaries | Process | Yes |
| Jack20 | RCT | Medicine ward | Not described | Discharge template includes TPADs, discharge planner to arrange PCP follow-up | Patient | Total number of emergency department visits and readmissions per participant within 30 days of the index discharge | Patient | No |
*Abbreviations: CHA, Cambridge Health Alliance; DSCS, Discharge Summary Completeness Score; MD, medical doctor; NP, nurse practitioner; PCP, primary care physician; POS, prospective observational study; RCT, randomized controlled trial; RN, registered nurse; TPAD, test pending at discharge
Study Design and Appraisal
Five of the included studies were RCTs,12,13,15,16,20 and the remaining four were prospective observational studies with pre and post comparison (Table 1).14,17–19
Overall, the mean quality score using our structured instrument was 3.4 (with zero being the lowest and seven being the highest possible score) (Table 2). Studies by Dalal and El-Kareh each scored six, while Dinescu, Graumlich, and Kantor each scored two.13–16 Dalal, El-Kareh, and Cadwallader collected demographic data on both patients and staff members involved in the intervention, while Kantor collected neither.13,15,17,19 Dalal, El-Kareh, and Kantor specifically defined the categories of TPADs their interventions targeted (e.g., microbiology), and Dalal, El-Kareh, and Cadwallader defined the conditions under which TPAD results were deemed clinically significant.13,15,17,19 Five of the nine studies assessed some aspect of user satisfaction with the interventions.13,15,18–20 Only Balaban and Jack specifically addressed the implementation cost of the intervention being studied.12,20
Table 2.
Quality Assessment of TPAD Interventions*
| Source | Patient data | User data | TPAD definition | Actionable TPAD definition | TPAD outcome | Cost | Intervention usability | Score (range 0–7) |
|---|---|---|---|---|---|---|---|---|
| Balaban12 | Yes | No | No | No | No | Yes | No | 2 |
| Dalal13 | Yes | Yes | Yes | Yes | Yes | No | Yes | 6 |
| Dinescu14 | No | Yes | No | No | Yes | No | No | 2 |
| El-Kareh15 | Yes | Yes | Yes | Yes | Yes | No | Yes | 6 |
| Graumlich16 | Yes | Yes | No | No | No | No | No | 2 |
| Kantor17 | No | No | Yes | No | Yes | No | No | 2 |
| O’Leary18 | No | Yes | No | No | Yes | No | Yes | 3 |
| Cadwallader19 | Yes | Yes | No | Yes | Yes | No | Yes | 5 |
| Jack20 | Yes | No | No | No | No | Yes | Yes | 3 |
*TPAD, test pending at discharge
Intervention Characteristics
We identified three different types of interventions that were evaluated to enhance TPAD management: six studies focused on enhanced discharge summary templates,12,16–20 one study used an educational intervention,14 and two studies implemented email notifications when TPADs were finalized (Table 3).13,15 Each type of intervention is discussed in detail below.
Table 3.
Detailed Description of TPAD Interventions*
| Study | Intervention design | User interface | Data entry source | Action | Target user |
|---|---|---|---|---|---|
| Balaban12 | • Generation of discharge summary (including TPADs) provided to patients in native language • Telephone contact by a primary care RN to patient • Electronic transfer of discharge summary to the primary care RN(s) • PCP feedback on discharge plan |
Paper, form-based application | Manual | Generation and electronic transmission of discharge documentation, telephone follow-up | Patient, Primary care RN, PCP |
| Dalal13 | • Software that monitors for finalized TPAD results, and sends alerts to attending physician and PCP | Automated from EHR | Email alert | Discharging physician | |
| Dinescu14 | • Audit of discharge summary based on 21-item quality criteria (including documentation of TPADs) • Discharging physicians receive feedback on audit results for their dictated discharge summaries |
Paper, face - to - face | Manual | Audit, feedback loop | Discharging physician |
| El-Kareh15 | • Software that monitors for finalized microbiology TPADs that may be clinically significant, sends alerts to attending physician and PCP | Automated from EHR | Email alert | Discharging physician | |
| Graumlich16 | • Electronic discharge template prompts discharging staff member to document TPADs | Form-based application | Manual | Generation of documentation | Discharging physician |
| Kantor17 | • Electronic discharge template automatically generates a list of pending tests to assist discharging staff member with documenting TPADs | Form-based application | Partially automated | Generation of documentation | Discharging physician |
| O’Leary18 | • Electronic discharge summary template, included field to enter TPADs • Attending physician sent automated reminder if discharge summary not complete after 24 hours • Discharge summary automatically distributed electronically to PCP |
Form-based application | Manual | Generation and electronic dissemination of documentation | Discharging physician, PCP |
| Cadwallader19 | • Discharge summary generation that prompts for TPADs | Form-based application | Manual | Generation of documentation | Discharge physician |
| Jack20 | • Discharging RN generates discharge document (includes TPADs) • Discharging RN arranges follow-up with PCP |
Microsoft Word template | Manual | Generation of documentation, follow-up appointment with PCP | Discharging RN |
*Abbreviations: EHR, Electronic Health Record; PCP, primary care physician; RCT, randomized controlled trial; RN, registered nurse; TPAD, test pending at discharge
Discharge Summary Template Interventions
O’Leary, Graumlich, and Cadwallader studied electronic discharge summary applications that included a field into which the discharging physician could manually enter patients’ TPADs.16,18,19 In O’Leary’s intervention, the automatically generated discharge summary was faxed to the patient’s PCP and submitted to the patient’s EHR; if the discharge summary was not completed within 24 hours of the patient leaving the hospital, then the discharging physician automatically received a reminder.18 Graumlich’s application generated one version of the discharge summary for the patient and one for the patient’s PCP, although it was not clear how the document was transmitted to the PCP.16 Cadwalladers’ application generated a printed copy of the discharge summary, which was mailed to the PCP.19
Jack and Balaban’s studies evaluated multifaceted interventions to improve the discharge process, including components to ensure TPADs were documented in the discharge summary.12,20 In Balaban’s study, a nurse completed an electronic ‘Patient Discharge Form’ that included a field in which to document TPADs, with one version of the form transmitted to the patient’s PCP’s office and a ‘user-friendly’ version provided to the patient.12 In Jack’s study, a nurse manually recorded TPADs in an ‘After-Hospital Care Plan’ (AHCP) template, verbally reviewed all TPADs with the patient, provided a version of the ACHP to the patient, and transmitted another version of the AHCP to the patient’s PCP and other relevant physicians.20
Lastly, Kantor studied an electronic discharge application that automatically compiled a list of laboratory, microbiology, and pathology TPADs, using data drawn from the EHR.17 The discharging physician then indicated which TPADs in the provided list should be included in the discharge summary generated by the application.17
Educational Interventions
Dinescu used an educational intervention in which dictated discharge summaries were audited using a 21-item checklist, including documentation of TPADs. Enrolled discharging physicians were then provided one-on-one feedback on deficiencies detected in their discharge summaries, including whether TPADs were documented.14
Email Notification Interventions
Dalal’s intervention automatically emailed the patients’ discharging physicians and PCPs when chemistry, hematology, radiology, pathology, or microbiology TPAD results were finalized.13 The application attempted to address alert fatigue by grouping results into a single email.13 El-Kareh developed a similar email alert system focusing exclusively on microbiology TPADs.15 To limit alert fatigue, El-Kareh’s application sent messages only for positive cultures that were deemed to be inappropriately treated at discharge.15
Impact on Improving Documentation of TPADs
Four of the nine studies evaluated the impact of their intervention on documentation of TPADs. Implementation of Cadwallader, Kantor, O’Leary, and Dinescu’s interventions was associated with significantly improved documentation of TPADs in discharge summaries.14,17–19 El-Kareh reported email alerts had a positive impact on documentation of physician follow-up actions in response to finalized microbiology TPAD results (Table 4).15
Table 4.
Effectiveness of TPAD Interventions*
| Study | Primary Outcome(s) | Event rate (intervention vs. control) | Impact† |
|---|---|---|---|
| Balaban12 | No outpatient appointment within 21 days with either an MD or NP at the patient’s primary care site or with a relevant specialist | 7/47 (15%) vs. 20/49 (41%) (p 0.005) Historic control 35/100 (35%) |
Negative |
| Readmission, for any reason, within 31 days to any of the 3 CHA hospitals | 4/49 (8%) vs. 4/49 (8%) (p 0.96) Historic control 14/100 (14%) |
||
| Emergency department visits within 31 days for a problem related to the original admission in any of the 3 CHA hospitals | 1/49 (2%) vs. 1/49 (2%) (p 0.97) Historic control 8/100 (8%) |
||
| Failure to complete an outpatient workup recommended by a hospital doctor | 3/26 (12%) vs. 5/16 (31%) (p 0.11) Historic control 13/42 (31%) |
||
| Dalal13 | Self-reported awareness of TPAD results by attending physician | 106/139 (76%) vs. 52/136 (38%) (p < 0.001) | Positive |
| Dinescu14 | Admission composite | 93/100 (93%) vs. 70/100 (70%) (p 0.001) | Positive |
| Hospital course composite | 93/100 (93%) vs. 78/100 (78%) (p 0.001) | ||
| Discharge planning composite | 93/100 (93%) vs. 77/100 (77%) (p 0.02) | ||
| Post-discharge care composite Follow-up results documented |
83/100 (83%) vs. 57/100 (57%) (p < 0.001) 81/100 (81%) vs. 42/100 (42%) (p 0.02) |
||
| El-Kareh15 | Presence in the patient’s outpatient electronic chart of documentation (note describing follow-up with the patient, note with acknowledgement of the result, or new antibiotic prescription) of follow-up action within 3 days of the post-discharge microbiology result | 27/97 (28%) vs. 8/60 (13%) (p 0.01) | Positive |
| Graumlich16 | Proportion of patients readmitted at least once within 6 months after the index hospitalization | 117/316 (37%) vs. 119/314 (38%) (p 0.897) | Negative |
| Kantor17 | Proportion of pending studies communicated in discharge summary | 43% vs. 18% (p 0.001) | Positive |
| Proportion of discharge summaries communicated all pending studies | 26% vs. 8% (p 0.002) | ||
| O’Leary18 | DSCS (out of 100) | 80.3 vs. 74.1 (p 0.007) | Positive |
| Pending tests documented in discharge summary | 44/95 (46%) vs. 14/101 (13%) (p 0.001) | ||
| Cadwallader19 | Frequency of tests with pending results that were documented in the discharge summaries | 178/812 (22%) vs. 87/701 (12%) (p 0.02) | Positive |
| Jack20 | Number of emergency department visits and readmissions per participant within 30 days of the index discharge | 116/370 (31%) vs. 166/368 (45%) (p 0.009) | Positive |
*Abbreviations: CHA, Cambridge Health Alliance; DSCS, Discharge Summary Completeness Score; MD, medical doctor; NP, nurse practitioner; TPAD, test pending at discharge
†Impact is defined as ≥ 50% of primary outcomes positive with p < 0.0511
Cadwallader, Kantor, and O’Leary evaluated whether enhanced discharge summary templates with a field for documenting TPADs would improve the inclusion of TPADs in the discharge summary.17,18,19 Cadwallader reported that 12% (87/701) of TPADs were documented in discharge summaries generated pre-intervention compared to 22% (178/812) of TPADs documented in discharge summaries generated after the intervention was implemented (p = 0.02).19 Kantor showed that the percentage of discharge summaries that communicated all TPADs increased from 8% prior to the intervention to 26% after the intervention had been implemented (p = 0.002).17 As part of a quality score for discharge summaries created before and after the intervention, O’Leary reported an increase in the percentage of discharge summaries that documented TPADs from 13% (14/101) pre-intervention to 46% (44/95) post-intervention (p = 0.001).18
Dinescu evaluated whether their educational intervention improved the percentage of discharge summaries documenting TPADs. The study reported that 42% (42/100) of discharge summaries included TPADs when dictated by physicians during the pre-intervention period, whereas 81% (81/100) of discharge summaries included TPADs when dictated by physicians who had received audit feedback during the intervention period (p = 0.02).14
El-Kareh evaluated the impact of email alerts on physicians’ documentation when microbiology TPADs finalized.15 The percentage of microbiology TPAD results with documentation of follow-up actions taken by the discharging physician within 72 hours of the test being finalized was higher in the intervention group receiving alerts compared to physicians in the control group receiving usual care, from 13% (8/60) in the control group to 28% in the intervention group (27/97) (p < 0.01).15
Impact on Physician Awareness of Finalized TPAD Results
Dalal and El-Kareh evaluated whether email notifications enhanced the awareness of finalized TPAD results by patients’ discharging physicians and outpatient physicians.13,15 Dalal showed that the percentage of discharging physicians’ self-reported awareness of TPAD results 72 hours after finalizing was 38% (52/136) in the control group compared to 76% (106/139) in the intervention group receiving alerts (p < 0.001). The percentage of PCPs’ self-reported awareness of TPAD results 72 hours after finalizing was 33% (27/83) in the control group versus 57% (39/69) (p = 0.004) in the intervention group receiving alerts.13 El-Kareh reported that patients’ inpatient and outpatient physicians were more likely to be aware of finalized microbiology results when receiving email alerts compared to physicians in the control group, but this improvement was not statistically significant.15
Impact on Adverse Events Related to Missed TPADs
Although none of the nine studies specifically measured the effect of their interventions on downstream patient harm due to delayed follow-up of TPADs, four studies did include patient outcomes related to adverse events in the post-discharge period.12,16,18,20 O’Leary surveyed outpatient physicians (PCPs and specialists) receiving discharge summaries to determine whether one or more of their patients in the previous 6 months had experienced an adverse or near-miss event as a result of poor communication at the time of discharge from the hospital.18 Although O’Leary’s study did not capture which qualifying events were due to missed TPADs, the percentage of outpatient physicians who reported preventable errors related to communication at transfer of care decreased from 66% in the pre-intervention period to 53% when the enhanced electronic discharge summary was implemented (p = 0.008).18
Graumlich’s study measured adverse events occurring within one month post-discharge because of delayed follow-up care (which may have indirectly addressed patient harm due to missed TPADs), but did not find a statistically nor clinically significant impact of their intervention on this outcome.16
Jack found that 31% (116/370) of patients in their intervention group had ED visits or hospital readmissions within 30 days of discharge versus 45% (166/368) of patients in the control group (p = 0.009).20 Balaban’s intervention had no effect on ED visits and re-hospitalization rates 31 days post-discharge.12 Unfortunately, neither study measured a TPAD-related process outcome that could have indicated if poor TPAD follow-up was implicated in the post-discharge ED visits or hospitalizations.12,20
Impact on Physician Satisfaction with TPAD Management
Three of the nine studies measured their interventions’ impact on physician satisfaction with TPAD management.13,18,19 O’Leary found that compared to the pre-intervention baseline, outpatient physicians reported significantly greater satisfaction on a 5-point Likert scale (1 being very dissatisfied, 5 very satisfied) with the quality of the discharge summaries they received during the intervention period (mean score of 3.04 versus 3.64, p < 0.001).18 By contrast, Cadawaller found that discharging physicians were divided evenly with respect to whether the intervention positively impacted the overall quality of the discharge summary, the ease of documentation of TPADs, and the quality of transfer of care communication with outpatient physicians.19 While not analyzed for statistical significance, survey results in Dalal’s study indicated that physicians in the intervention arm receiving email alerts reported higher satisfaction with TPAD management compared to physicians in the control group.13
Discussion
We identified nine studies that evaluated three different strategies to enhance TPAD management.12–20 The first approach was to implement a discharge summary template to document patients’ TPADs.12,16–20 The second approach involved an educational intervention to ensure physicians’ dictated discharge summaries included TPADs.14 The third approach was to notify patients’ physicians of finalized TPAD results using email alerts (Table 2).13,15 Available studies suggest that all three approaches could be effective at improving management of TPADs and enhancing patient safety.
This review identified six studies evaluating enhanced discharge templates and one study of a physician educational intervention to ensure TPADs are documented in the discharge summary.12,14,16–20 Four of these seven studies, Cadwallader, Kantor, O’Leary, and Dinescu, measured a process outcome related to TPAD documentation.14,17–19 Although all four studies were associated with a significant improvement in the documentation of TPADs in discharge summaries,14,17–19 none demonstrated that improving TPAD documentation prevented patient harm from missed or delayed follow-up of TPAD results. For example, Cadawaller and O’Leary measured the effect of their interventions on documentation of TPADs in the discharge summary and its transmission to patients' primary care teams, but neither study evaluated whether patients’ outpatient physicians received the discharge summary or followed-up on TPADs. Balaban and Graumlich also studied interventions to improve documentation of TPADs in the discharge summary, but failed to establish any impact on outcomes related to post-discharge patient morbidity, such as hospital readmissions or ED visits.12,16 Including a list of TPADs in a discharge summary can alert the patient’s physicians to tests requiring follow-up, but this approach is limited as outpatient providers may not receive the discharge summary or have access to the patient’s hospital medical record to review finalized TPAD results. Thus, more research is needed to evaluate whether including TPADs in the discharge summary reduces patient harm.
An automated email notification system to alert physicians when TPAD results finalize is a promising approach that was shown to improve both physicians’ awareness13 and documentation of completed test results,15 but this intervention faces barriers to being widely adopted. First of all, there is literature showing that an EHR with a notification system can lead to physician users becoming overwhelmed by too many messages.23 Similarly, in El-Kareh’s study, despite implementing an algorithm to prevent spurious alerts, 85% of emails were generated for untreated urine cultures of unknown clinical significance.15 Second, it is important to note that Dalal and El-Kareh’s interventions used sophisticated computer applications that integrated with their organizations’ extensible EHRs.13,15 Replicating these interventions would require significant institutional investments in IT infrastructure and expertise, a challenging proposition in less resource-rich healthcare settings. While innovative and effective, email alerts for TPADs are limited by the inability of automating heuristics to identify actionable test results and the lack of generalizability. Ultimately, we view the email alerts as a promising intervention, particularly if the notification system integrates with EHR to ensure physician accountability for prompt follow-up of TPADs with high potential for patient harm if missed (e.g., sputum positive for tuberculosis or biopsy positive for malignancy).
Despite the heterogeneity of the designs used by the nine studies in this review, it is clear that both process and patient-related outcomes are necessary to evaluate the ability of an intervention to improve follow-up of TPADs. Balaban, Jack, and Graumlich measured readmission rates and other measures of patient morbidity, but did not include TPAD-related process outcomes that could have established a relationship between follow-up of TPAD results and downstream patient harm.12,16,20 Cadawaller, Kantor, O’Leary, and Dinescu measured documentation of TPADs in the discharge summary, but did not capture other important outcomes, such as receipt of the discharge summary by the patients’ physicians, physicians’ awareness of finalized TPAD results, timeliness and appropriateness of physicians’ follow-up actions in response to the finalized TPAD result, and any patient harm incurred by delays in diagnosis and management as a result of missed TPAD results.14,17,18,19 Notably, Dalal’s primary outcome was physician awareness of TPAD results—an intermediate process measure that may be inaccurate because of reliance on physician self-reporting and may make performance monitoring over time challenging because of survey fatigue.13 El-Kareh’s primary outcome was the existence of documented follow-up action when a TPAD result finalizes, which may over-estimate missed test results because of inadequate or inaccessible documentation.15 Thus, studies should employ not only process outcomes to demonstrate fidelity of the intervention, but also downstream patient outcomes to establish the effectiveness of an intervention in ensuring TPADs are not lost to follow-up.
Lastly, there are several interventions that have not been studied in the context of TPAD management.3,21 While there is a body of literature examining the utility of the test management features of EHRs, such as result inboxes,23 we did not identify any studies that evaluated whether these tools improved TPAD follow-up. Another example is web-based portals that provide patients access to their EHR, yet we did not identify any studies assessing whether use of patient portals in the post-discharge period is effective in reducing the incidence of missed TPADs. Lastly, given the complexity of the process of following up TPADs, an effective solution is likely to consist of a combination of discrete interventions (e.g., improved discharge documentation of TPADs and alerts when results are available), and this approach needs to be studied in future research. The absence of studies evaluating the use of these test management solutions to improve TPAD follow-up presents opportunities for research and quality improvement.
Limitations
Our review has several limitations. First of all, the studies included in our review focused on patients being discharged from medicine inpatient wards. Although we did not limit our search strategy by healthcare setting, we did not find studies of interventions performed in other inpatient or outpatient settings during the screening process. Thus, generalizing our findings to other inpatient services (e.g., surgery) or other ambulatory care settings must be done with caution. Another limitation to generalizing our results is that most included studies were conducted by investigators working in select healthcare systems in the US. Of note, we limited our review to studies undertaken after 2000 and may have missed older studies; however, we believe that studies conducted prior to the widespread implementation of EHRs and electronic communication are unlikely to provide a meaningful contribution to this review. We also did not include information from white papers, blogs, or other “gray literature,” instead choosing to focus on peer-reviewed empirical work. Lastly, the quality assessment tool used in this review was derived from prior work and in consultation with the study’s senior authors, but has not been broadly validated with experts in the field of TPAD management.22
Conclusion
In summary, enhanced discharge summary templates, educational interventions for discharging physicians, and email alerts for finalized TPAD results are promising strategies to improve the follow-up of finalized TPAD results. While there is limited evidence to show that these interventions reduce patient harm from delayed follow-up of TPADs, there are a number of practical interventions that should be considered for healthcare systems seeking to improve TPAD follow-up. Given the complexity of the processes necessary to ensure follow-up of TPADs, future research will need to evaluate multifaceted interventions (e.g., improved discharge documentation of TPADs combined with email alerts when results become available).
Electronic supplementary material
(DOCX 22 kb)
Acknowledgments
Grant Support
Dr. Peter Cram is supported by a K24 award from NIAMS (AR062133) at the US NIH.
Compliance with Ethical Standards
Conflict of Interest
The authors have no conflicts to disclose.
Contributor Information
Patrick J. Darragh, Email: patrick.darragh@gmail.com.
T. Bodley, Email: thomas.bodley@utoronto.ca.
A. Orchanian-Cheff, Email: ani.orchanian-cheff@uhn.ca.
K. G. Shojania, Email: kaveh.shojania@sunnybrook.ca.
J. L. Kwan, Email: janice.kwan@utoronto.ca.
P. Cram, Email: peter.cram@uhn.ca.
References
- 1.Were MC, Li X, Kesterson J, Cadwallader J, Asirwa C, Khan B, Rosenman MB. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24(9):1002–1006. doi: 10.1007/s11606-009-1057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128. doi: 10.7326/0003-4819-143-2-200507190-00011. [DOI] [PubMed] [Google Scholar]
- 3.Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20(2):194–9. doi: 10.1136/bmjqs.2010.044339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hickner J, Graham DG, Elder NC, et al. Testing process errors and their harms and consequences reported from family medicine practices: a study of the American Academy of Family Physicians National Research Network. Qual Saf Health Care. 2008;17(3):194–200. doi: 10.1136/qshc.2006.021915. [DOI] [PubMed] [Google Scholar]
- 5.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from liability insurers. Ann Emerg Med. 2007;49(2):196–205. doi: 10.1016/j.annemergmed.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 6.Tarkan S, Plaisant C, Shneiderman B, Hettinger AZ. Reducing missed laboratory results: defining temporal responsibility, generating user interfaces for test process tracking, and retrospective analyses to identify problems. AMIA Annu Symp Proc. 2011;2011(22):1382–91. [PMC free article] [PubMed] [Google Scholar]
- 7.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–7. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 8.Kosecoff J, Kahn KL, Rogers WH, et al. Prospective payment system and impairment at discharge. The ‘quicker-and-sicker’ story revisited. JAMA. 1990;264(15):1980–3. doi: 10.1001/jama.1990.03450150080035. [DOI] [PubMed] [Google Scholar]
- 9.Kripalani S, LeFevre K, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 10.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is human: building a safer health system. Institute of Medicine (US) Committee on Quality of Health Care in America. Washington (DC): National Academies Press (US); 2000. [PubMed] [Google Scholar]
- 11.Roshanov PS, Misra S, Gerstein HC, et al. Computerized clinical decision support systems for chronic disease management: a decision-maker-researcher partnership systematic review. Implement Sci. 2011;6:92. doi: 10.1186/1748-5908-6-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228–3. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dalal AK, Roy CL, Poon EG, et al. Impact of an automated email notification system for results of tests pending at discharge: a cluster-randomized controlled trial. J Am Med Inform Assoc. 2014;21(3):473–80. doi: 10.1136/amiajnl-2013-002030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dinescu A, Fernandez H, Ross JS, Karani R. Audit and feedback: an intervention to improve discharge summary completion. J Hosp Med. 2011;6(1):28–32. doi: 10.1002/jhm.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Kareh R, Roy C, Williams DH, Poon EG. Impact of automated alerts on follow-up of post-discharge microbiology results: a cluster randomized controlled trial. J Gen Intern Med. 2012;27(10):1243–50. doi: 10.1007/s11606-012-1986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graumlich JF, Novotny NL, Stephen Nace G, et al. Patient readmissions, emergency visits, and adverse events after software-assisted discharge from hospital: cluster randomized trial. J Hosp Med. 2009;4(7):E11–9. doi: 10.1002/jhm.469. [DOI] [PubMed] [Google Scholar]
- 17.Kantor MA, Evans KH, Shieh L. Pending studies at hospital discharge: a pre-post analysis of an electronic medical record tool to improve communication at hospital discharge. J Gen Intern Med. 2015;30(3):312–8. doi: 10.1007/s11606-014-3064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Leary KJ, Liebovitz DM, Feinglass J, et al. Creating a better discharge summary: improvement in quality and timeliness using an electronic discharge summary. J Hosp Med. 2009;4(4):219–25. doi: 10.1002/jhm.425. [DOI] [PubMed] [Google Scholar]
- 19.Cadwallader J, Asirwa C, Li X, Kesterson J, Tierney WM, Were MC. Using computerized provider order entry to enforce documentation of tests with pending results at hospital discharge. Appl Clin Inform. 2012;3(2):154–163. doi: 10.4338/ACI-2012-01-RA-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callen JL, Westbrook JI, Georgiou A, Li J. Failure to follow-up test results for ambulatory patients: a systematic review. J Gen Intern Med. 2012;27(10):1334–48. doi: 10.1007/s11606-011-1949-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haynes RB, Wilczynski NL, Computerized Clinical Decision Support System (CCDSS) Systematic Review Team Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: methods of a decision-maker-research partnership systematic review. Implement Sci. 2010;5:12. doi: 10.1186/1748-5908-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh H, Spitzmueller C, Petersen NJ, et al. Primary care practitioners’ views on test result management in EHR-enabled health systems: a national survey. J Am Med Inform Assoc. 2013;20(4):727–35. doi: 10.1136/amiajnl-2012-001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 22 kb)