Abstract
Objective
To examine how Transtheoretical Model (TTM)’s processes of change and mHealth literacy strategies are employed in mobile smoking cessation apps.
Methods
A purposive sample of 100 iTunes apps were coded to assess descriptive (price, type, developer, user-rating) and engagement metrics, including processes of change and mHealth literacy strategies (plain language, usability, interactivity). One-way ANOVAs and independent samples t-tests examined associations between descriptive and engagement metrics.
Results
Over half of the apps included 7 (78%) processes of change. Fewer included self-liberation (36%) and reinforcement management (34%). Most apps incorporated plain language, but few integrated usability and interactivity strategies. Hypnotherapy and informational apps included more behavioral processes of change than apps incorporating a combination of features, including gaming, cigarette trackers, and motivational coaching (p<.01).
Conclusion
Apps included behavior change processes but rarely incorporated usability and interactivity features to promote patient engagement. Engagement metrics did not vary by app user-ratings, price-to-download, or developer, including for-profit organizations or government and educational institutions.
Practice Implications
Providers should acknowledge the popularity of smoking cessation apps as potential cessation aids and communicate their benefits and drawbacks to patients. Future efforts to improve smoking cessation apps should focus on enhancing the quality of tailored and interactive content.
Keywords: smoking cessation, mobile health apps, behavior change theory, health literacy
1. Introduction
Health care providers refer patients struggling with smoking cessation to telephone quit lines, national health care organization websites supporting tobacco-free initiatives, and, more recently, text-based message cessation programs [1]. Smoking cessation mobile health (mHealth) apps are interactive tools synced to mobile devices and provide real-time feedback to support quit attempts. Smoking cessation apps are more popular than mainstream support, including telephone quit-lines [2]. One study found that nearly 800,000 smoking cessation apps are downloaded per month from popular systems, including iTunes [2]. Evidence-based smoking cessation apps are not readily available [2–5], which may be why health care providers are not recommending them to patients. However, mHealth technologies hold great promise in tobacco control [6]. Health care providers who recommend interactive, easy-to-use [4] and theory-based [7–8] smoking cessation apps may put smokers in control of their quit attempts and ultimately alleviate the burden of tobacco-related morbidity and mortality.
Smoking cessation is a process-oriented behavior. Cessation occurs as people who smoke tobacco transition through a variety of stages using cognitive/affective and behavioral processes of change. The Transtheoretical Model (TTM) provides a framework for understanding these stages of behavior change and the processes that explain how change occurs [9]. Smoking cessation interventions that use cessation aids and TTM processes of change can help people successfully quit smoking [10–11]. In addition to incorporating behavior change processes, smoking cessation apps should include features that promote patient acceptability [12] so that all users can benefit, regardless of their health literacy and previous mHealth app experiences. In 2014, the Institute of Medicine Roundtable Session on Health Literacy’s Collaborative on New Technologies proposed “mHealth literacy” strategies to support the use of plain language, usability principles, and interactive features in apps [13]. These strategies serve as universal precautions to increase the likelihood of app uptake and behavior change [13]. Table 1 presents these engagement metrics, TTM processes of change and mHealth literacy strategies, as they are relevant to smoking cessation apps.
Table 1.
Operational Definitions of Patient Engagement Metrics with Relevant Examples
| TTM Processes of Change9,17 | Operational Definition |
|
| |
| Cognitive/Affective Processes | |
| Consciousness Raising | Finding and learning new facts, ideas, and tips that support smoking cessation |
| • Presents statistics about annual smoking rates and deaths; | |
| • Provides general information about the dangers of smoking and benefits of quitting | |
| Self-Reevaluation | Identifying smoking as part of one’s identity |
| • Asks user to image him or herself as a smoker or non-smoker | |
| Dramatic Relief | Experiencing the negative emotions that go along with smoking tobacco |
| • Tracks cigarette cravings | |
| • Discusses how emotions are altered by smoking tobacco and/or quitting | |
| Environmental Reevaluation | Realizing the negative impact of smoking on the social and physical environment. |
| • Describes how smoking tobacco has an effect on other people | |
| • Reminds users about the social benefits of quitting smoking | |
| Behavioral Processes | |
| Self-Liberation | Making a firm commitment to quit smoking |
| • Establish a quit date, with the possibility to share it with online friends/community | |
| Counterconditioning | Substituting smoking tobacco with an alternative healthy behavior |
| • Instructs user to press “smoke” or “crave” options on the app, play a game provided by the app, or talk with someone or exercise when they crave cigarettes | |
| Helping Relationship | Using social support to quit smoking |
| • Provides users the opportunity to exchange information on social media or email; | |
| • Allows users to communicate through an online community | |
| Reinforcement Management | Increasing the rewards for quitting and decreasing awards for smoking |
| • Receives awards, badges, or updates on a daily, weekly, or monthly basis | |
| • Receives push-button notifications to messages or alert users of their progress | |
| Stimulus Control | Removing cues to smoke and adding cues to resist the temptation to smoke |
| • Shows user the time/date/mood where they are most likely to smoke/crave | |
| • Instructs users to avoid locations and people where cigarette cravings occur | |
|
| |
| mHealth Literacy Strategies13,18 | Operational Definitions |
|
| |
| Plain Language Dimension | |
| Paragraph Length | • Paragraphs are less than 8 sentences or 250 words |
| Meaningful Headings | • Headings are shown and they are descriptive or accurate to the page |
| Non-Technical Language | • Simple, non-scientific or technical jargon |
| Sentence Length | • Sentences are less than 20 words |
| Personal Pronouns | • User is referred to as “you” or the app system as “we” |
| Present Tense | • Present or future tense is used; past tense is avoided |
| Active Voice | • Sentences are formatted in the active voice, not the passive voice |
| Usability Dimension | |
| Search/Browse Bar | • In-app search functionality is available |
| Screen Control Options | • The font and its size can be adjusted in the app settings |
| Homepage Accessibility | • Top/bottom menu always provides a “home” or “dashboard” option |
| Linear Navigation Path | • App is navigated in a linear fashion (e.g., pg 1 to pg 2 to pg 3; not pg 1 to pg 3) |
| Navigation Menu | • App pages are easily accessible (e.g., has page/function icons at the bottom/top) |
| Images for Learning | • Images (e.g., charts, graphs, photos) are displayed and supplement page content |
| Color Scheme | • Dark fonts and light backgrounds are used, not dark background and light font |
| Interactivity Dimension | |
| Online Community | • App integrates with an online community/discussion forum unique to the app |
| Email Integration | • App integrates with a user’s email address for easy sharing and contact |
| Social Media Integration | • App integrates with social media (e.g., Facebook, Twitter) for sharing and contact |
| Audio/Visual Multimedia | • Videos or audio are used to supplement and navigate the content on the app |
| Tailored Content | • Demographic information, number of cigarettes/cravings, and money spent per cigarette pack is monitored and used to guide tracking features and education. |
mHealth smoking cessation apps have enormous potential to facilitate patient engagement and activation in promoting smoking cessation and tobacco control in the general population [6]. However, before health care providers recommend smoking cessation apps to patients, they must be certain that apps incorporate effective behavior change strategies within user-friendly platforms to facilitate user interest and retention [14–15]. Currently, the degree to which smoking cessation apps incorporate theory-based behavioral support and strategies to facilitate interactive, easy-to-understand and -use content is unknown. This lack of knowledge poses significant barriers to understanding the quality of existing smoking cessation apps, and raises questions regarding patient use of these apps as smoking cessation aids. To fill this fundamental gap in the literature, this study explored how TTM processes of change and mHealth literacy strategies are programmed into smoking cessation apps.
2. Methods
2.1. Sample & procedures
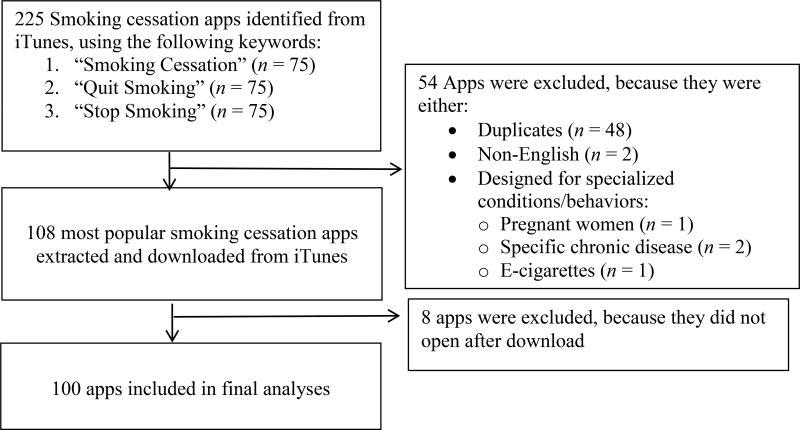
In January 2016, a purposive sample of 100 smoking cessation apps was downloaded from iTunes, a popular system to access these apps [14]. Following search procedures from prior studies [2–3], apps were retrieved through 3 smoking cessation-related search terms (“smoking cessation,” “quit smoking,” “stop smoking”). Figure 1 depicts this process exempt from human subjects review at a local Institutional Review Board. A trained Masters-level researcher coded 100% of the apps and a trained research assistant coded 30% for inter-coder reliability. Krippendorff’s alpha [16] revealed adequate inter-coder reliability for the processes of change (α = .86) and mHealth Literacy strategies (α = .87).
Figure 1.
Flow chart depicting app selection process
2.2. Measures
Table 1 presents operational definitions used to of code variables. The following descriptive metrics were coded: (1) type, (2) developer/source, (3) average user-rating (5-point star-scale), and (4) price-to-download (USD). TTM processes of change and mHealth literacy strategies served as engagement metrics and were also coded within the app user-interface. The presence of nine TTM processes of change [9,17] coded in each app was summed in both cognitive/affective (min = 0; max = 4) and behavioral (min = 0; max = 5) categories. The presence of seventeen mHealth literacy strategies in each app was computed within 3 dimensions [13,18]: plain language (min = 0; max = 7), usability (min = 0; max = 7), and interactivity (min = 0; max = 5).
2.3. Statistical analysis
Mean (± SD) processes of change and mHealth literacy scores were computed. One-way ANOVAs and independent samples t-tests were conducted to determine if the number of mHealth literacy strategies and processes of change significantly differed by descriptive app metrics. Data were analyzed with SPSS v24.
3. Results
Table 2 shows that nearly half of apps were cigarette trackers (45%) and created by independent developers (61%). Apps with a fee (32%) cost $1.08 (SD = $2.37), on average. One-quarter of the apps reported 2.4-to-5-star user-ratings, but nearly 40% were not rated.
Table 2.
Characteristics of Descriptive Metrics in Smoking Cessation Apps (N = 100)
| % | |
|---|---|
| Type of App | |
| Hypnotherapy | 17 |
| Cigarette Rationing | 3 |
| Cigarette Tracker | 45 |
| Informational/Educational | 6 |
| Game/Social | 9 |
| Health/Motivational Coaching | 8 |
| Combination of Features | 12 |
|
| |
| App Source/Developer | |
| Independent Developer | 61 |
| Non-Profit Organization | 7 |
| For-Profit Organization | 32 |
|
| |
| Rating (0–5 Stars) | M = 1.43 (SD = 1.73) |
| 0 Stars | 39 |
| 1 – 2.3 Stars | 36 |
| 2.4 – 5 Stars | 25 |
|
| |
| Price ($) to Download | M = $1.08 (SD = 2.37) |
| Free | 68 |
| Not Free | 32 |
Table 3 shows that over half of the apps included 7 (78%) processes of change. Self-liberation and reinforcement management, two behavioral processes, were used less often (36% and 34%, respectively). Almost all mHealth literacy plain language strategies were included in reviewed apps (M = 5.69; SD = 1.54), yet fewer usability (M = 2.79; SD = .95) and interactivity (M = 1.86; SD = 1.27) strategies were observed. No apps incorporated search/browse bars and few (2%) used screen control features for personalized navigation. Over half (59%) infused tailored interactive content based on user characteristics, including demographics, number of cigarettes smoked/day, and money spent on cigarettes. Interactivity was fostered through social media (i.e., Facebook, Twitter) in almost half of the reviewed apps (48%), while email (28%) and in-app online communities (16%) were used less.
Table 3.
Characteristics of Engagement Metrics in Smoking Cessation Apps (N = 100)
| mHealth Literacy Strategies | % Present in Apps (or otherwise stated) |
| Plain Language | M = 5.69 (SD = 1.54) |
| Paragraph Length | 58 |
| Meaningful Headings | 66 |
| Non-Technical Language | 82 |
| Sentence Length | 89 |
| Personal Pronouns | 89 |
| Present Tense | 91 |
| Active Voice | 94 |
| Usability | M = 2.79 (SD = .95) |
| Search/Browse Bar | 0 |
| Screen Control Options | 2 |
| Homepage Accessibility | 28 |
| Linear Navigation Path | 38 |
| Navigation Menu | 56 |
| Images for Learning | 72 |
| Color Scheme | 83 |
| Interactivity | M = 1.86 (SD = 1.27) |
| Online Community Integration | 16 |
| Email Integration | 28 |
| Social Media Integration | 48 |
| Audio/Visual Multimedia | 35 |
| Tailored Content | 59 |
|
| |
| TTM Processes of Change | % Present in Apps (or otherwise stated) |
| Cognitive/Affective Processes | M = 2.79 (SD = 1.06) |
| Consciousness Raising | 50 |
| Dramatic Relief | 74 |
| Environmental Reevaluation | 79 |
| Self-Reevaluation | 74 |
| Behavioral Processes | M = 2.83 (SD = 1.24) |
| Self-Liberation | 36 |
| Counterconditioning | 63 |
| Helping Relationships | 71 |
| Reinforcement Management | 34 |
| Stimulus Control | 79 |
Note. Range of strategies used for the following mHealth literacy dimensions: plain language (min = 0; max = 7); usability (min = 0; max = 7); interactivity (min = 0; max = 5). Range of TTM processes of change for each category: cognitive/affective processes (min = 0; max = 4); behavioral processes (min = 0; max = 5).
There was no statistically significant relationship between most descriptive app metrics and processes of change or mHealth literacy strategies. However, the number of behavioral processes differed by app type, F(6,92) = 4.41, p < .001. Tukey’s post-hoc analyses indicated that hypnotherapy apps, on average, included 1.16 more behavioral processes than cigarette trackers (p < .01) and 1.85 more behavioral processes than apps integrating a combination of features, including gaming, cigarette trackers, and motivational coaching (p < .01). Finally, informational/educational apps used an average of 1.75 more behavioral processes than apps using a combination of features (p < .05).
4. Discussion and Conclusion
4.1. Discussion
Smoking cessation apps communicated information using theoretical processes of change and plain language, yet few incorporated usability and interactivity strategies to facilitate connectivity with mobile platforms (e.g., progress reports, push-messages) or other users. Previous research suggests that theoretical processes of change are associated with user engagement in smoking-related social media sites [19], and that app engagement features [20] (e.g., text-messaging [21]) are positively associated with quit rates. The static nature of smoking cessation apps may alleviate the potential for cognitive overload among smokers; however, smokers most often access online media to engage and share experiences with other smokers [22]. There is a need to refine smoking cessation apps to simulate a patient-centered platform that promotes user autonomy by not restricting their capacity to interact with others.
The number of mHealth literacy strategies and processes of change were not associated with the developer/source, user-ratings, and price-to-download. Unlike previous research [2], this suggests that user-ratings may not be influenced by the theoretical basis or usability of apps. Also, mHealth users are less likely to download apps requiring payment [23]; therefore, the lack of relationship between app price and the number of mHealth literacy strategies and processes of change suggest that cost may not be a barrier for smokers, who generally have low socioeconomic attainment [24].
This study applied a cross-sectional content analysis methodology. Results are descriptive and do not provide evidence for the effectiveness for processes of behavior change and mHealth literacy strategies to support cessation. Also, the cognitive/affective process of social liberation [9,17] was not coded, because apps do not account for a user’s assessment of social structures and policies to facilitate cessation.
4.2. Conclusion
The future of mHealth smoking cessation support will be dependent on ensuring that apps incorporate effective behavior change strategies through tailored and interactive content with a high degree of usability. Additionally, it will be important to facilitate transparent patient-provider communication regarding the benefits and drawbacks of smoking cessation apps.
4.3. Practice Implications
Smokers contemplating cessation may consider mHealth apps as attractive and feasible tools to facilitate quit attempts. These apps are considerably low-cost and there is zero commitment if the user is not satisfied with the content. Few health care providers believe that evidence-based apps exist, but would be willing to recommend them to their patients [25]. Despite health care providers’ caution toward recommending these apps, smokers continue to download and use them. Although most apps are created by independent developers, some apps are advertised by health care organizations hosting popular quit lines and website resources. Therefore, health care providers should recognize that smoking cessation apps are available to their patients and frequently downloaded, despite evidence of their low usability and interactivity features. These providers should also engage in discussion with their patients about the drawbacks and benefits of existing smoking cessation apps.
Most apps included behavior change processes shown to promote smoking cessation; however, fewer consistently applied usability and interactivity strategies. Apps that included most behavior change processes were hypnotherapy and education apps, which comprised pre-scripted and audio-visual content that fostered information extraction (e.g., listen to recorded message, read informational pages), rather than interactive and active forms of engagement (e.g., co-created quit plans, social environments). mHealth apps are valued because of their capability to deliver content through interactive and tailored content, while facilitating social support, behavior tracking, and health status monitoring [26]. Smokers prefer apps with interactive and tailored features [25], yet smoking cessation apps in this study generally provided static scientific information and fostered superficial and detached connections with its users. Connecting with users in a personally engaging and interactive manner can enhance the quality of communication in delivering health information via technology [27]. Moreover, interactivity helps users overcome feelings of boredom and frustration, which have detrimental effects on technology-based learning [28]. Future research on smoking cessation apps should ensure that behavior change processes are incorporated in a way that reflects the interactive and dynamic features of mHealth apps.
HIGHLIGHTS.
More behavior change processes were included in apps without interactive features
Most of the evaluated smoking cessation apps included behavior change processes
Few smoking cessation apps included usability and interactivity features
Most smoking cessation apps presented information using plain language
Acknowledgments
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health [grant # F31HL132463] and the NIH/NCATS Clinical and Translational Science Award to the University of Florida [grant # ULI TR000064].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Health care professionals: Help your patients quit smoking. [accessed 17.07.27];2017 https://www.cdc.gov/tobacco/campaign/tips/partners/health/hcp/index.html.
- 2.Abroms LC, Westmaas L, Bontemps-Jones J, Ramani R, Mellerson J. A content analysis of popular smartphone apps for smoking cessation. Am. J. Prev. Med. 2013;45:732–6. doi: 10.1016/j.amepre.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abroms LC, Padmanabhan N, Thaweethai L, Phillips T. iPhone apps for smoking cessation: A content analysis. Am. J. Prev. Med. 2011;40:279–85. doi: 10.1016/j.amepre.2010.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferron JC, Brunette MF, Geiger P, Marsch LA, Adachi-Meja AM, Bartels SJ. Mobile phone apps for smoking cessation: Quality and usability among smokers with psychosis. JMIR, Human. Factors. 2017;4:e7. doi: 10.2196/humanfactors.5933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haskins BL, Lesperance D, Gibbons P, Boudreaux ED. A systematic review of smartphone applications for smoking cessation. Transl. Behav. Med. 2017:1–8. doi: 10.1007/s13142-017-0492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman B. New media and tobacco control. Tob. Control. 2012;21:139–44. doi: 10.1136/tobaccocontrol-2011-050193. [DOI] [PubMed] [Google Scholar]
- 7.Bricker JB, Mull K, Kientz JA, Vilardaga RM, Mercer AK, Akioka K, Heffner JL. Randomized, controlled pilot trial of a smartphone app for smoking cessation acceptance and commitment therapy. Drug. Alc. Depend. 2014;1:87–94. doi: 10.1016/j.drugalcdep.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ubhi HK, Michie S, Kotz D, Wong WC, West R. A mobile app to aid smoking cessation: Preliminary revaluation of smokefree28. J. Med. Internet. Res. 2015;17:e17. doi: 10.2196/jmir.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prochaska JO, DiClemente CC, Velicer WF, Ginpil S, Norcross JC. Predicting change in smoking status for self-changers. Addict. Behav. 1985;10:395–406. doi: 10.1016/0306-4603(85)90036-x. [DOI] [PubMed] [Google Scholar]
- 10.Aveyard P, Massey L, Parsons A, Manaseki S, Griffin C. The effect of transtheoretical model based interventions on smoking cessation. Soc. Sci. Med. 2009;68:397–403. doi: 10.1016/j.socscimed.2008.10.036. [DOI] [PubMed] [Google Scholar]
- 11.Ham OK, Lee YJ. Use of the transtheoretical model to predict stages of smoking cessation in Korean adolescents. J. School. Health. 2007;77:319–26. doi: 10.1111/j.1746-1561.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 12.Ghorai K, Akter S, Khatun F, Ray P. mHealth for smoking cessation programs: A systematic review. J. Pers. Med. 2014;4:412–23. doi: 10.3390/jpm4030412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broderick J, Devine T, Langhans E, Lemerise AJ, Lier S, Harris L. Designing health literate mobile apps. Retrieved from. [accessed 17.07.27];2014 http://health.gov/communication/literacy/BPH-HealthLiterateApps.pdf.
- 14.BinDhim NF, McGeechan K, Trevena L. Who uses smoking cessation apps? A feasibility study across three countries via smartphones. mHealth. uHealth. 2014;2:e4. doi: 10.2196/mhealth.2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boudreaux E, Warring ME, Hayes RB, Sadasivam RS, Mullen S, Pagoto S. Evaluating and selecting mobile health apps: Strategies for healthcare providers and healthcare organizations. Transl. Behav. Med. 2014;4:263–71. doi: 10.1007/s13142-014-0293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hayes AF, Krippendorff K. Answering the call for a standard reliability measure for coding data. Comm. Meth. Meas. 2007;1:77–89. [Google Scholar]
- 17.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrated model of change. J. Consult. Clin. Psych. 1983;51:390–95. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 18.Ginossar T, Shah SFA, West AJ, Bentley JM, Caburnay CA, Kreuter MW, Kinney AY. Content, usability, and utilization of plain language in breast cancer mobile phone apps: A systematic analysis. mHealth. uHealth. 2017;5:e20. doi: 10.2196/mhealth.7073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thrul J, Klein AB, Ramo DE. Smoking cessation intervention on Facebook: Which content generates the best engagement? J. Med. Internet. Res. 2015;17:e244. doi: 10.2196/jmir.4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Regmi K, Kassim N, Ahmad N, Tuah NAA. Effectiveness of mobile apps for smoking cessation: A review. Tob. Prev. Cessation. 2017;3:1–11. doi: 10.18332/tpc/70088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane. Database. Syst. Rev. 2016;4:1–52. doi: 10.1002/14651858.CD006611.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cole-Lewis H, Perotte A, Galica K, et al. Social network behavior and engagement within a smoking cessation Facebook page. J. Med. Internet. Res. 2016;18:e205. doi: 10.2196/jmir.5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krebs P, Duncan DT. Health app use among US mobile phone owners: A national survey. mHealth. Uhealth. 2015;3:e101. doi: 10.2196/mhealth.4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Cigarette smoking and tobacco use among people of low socioeconomic status. [accessed 17.07.10];2017 https://www.cdc.gov/tobacco/disparities/low-ses/index.htm.
- 25.McClure JB, Hartzler AL, Catz SL. Design considerations for smoking cessation apps: Feedback from nicotine dependence treatment providers and smokers. JMIR. Mhealth. Uhealth. 2016;4:e17. doi: 10.2196/mhealth.5181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Food and Drug Administration. Mobile medical applications. [accessed 17.07.05];2015 https://www.fda.gov/MedicalDevices/DigitalHealth/MobileMedicalApplications/ucm255978.htm.
- 27.Baker RSJD, D’Mello SK, Rodrigo MMT, Graesser AC. Better to be frustrated than bored: The incidence, persistence, and impact of learners’ cognitive-affective states during interactions with three different computer-based learning environments. Int. J. Human. Comp. Stud. 2010;68:223–41. [Google Scholar]
- 28.Kreps GL, Neuhauser L. Artificial intelligence and immediacy: Designing health communication to personally engage consumers and providers. Pat. Ed. Couns. 2013;92:205–10. doi: 10.1016/j.pec.2013.04.014. [DOI] [PubMed] [Google Scholar]