Abstract
Background: Alexithymia and emotional awareness may be considered overlapping constructs and both have been shown to be related to psychological and emotional well-being. However, it is not clear how the constructs relate to each other empirically or if they may overlap more or less in different populations. The aim of this review was therefore to conduct a meta-analysis of correlations between the most commonly used measures of alexithymia (i.e., the self-report instrument Toronto Alexithymia Scale; TAS-20) and emotional awareness (i.e., the observer-rated instrument Level of Emotional Awareness Scale; LEAS) and to explore potential moderators of their relationship.
Methods: Electronic databases were searched for studies published until the end of February 2018. Study samples were coded as medical conditions, psychiatric disorders and/or healthy controls and sample mean age and gender distribution were extracted. Correlations between the TAS-20 and the LEAS were subjected to a random effect of meta-analysis and moderators were explored in subgroup analyses and meta-regressions. Publication bias was considered.
Results: 21 studies reporting on 28 independent samples on correlation analysis were included, encompassing a total of 2857 subjects (57% women). The aggregated correlation between TAS-20 and LEAS was r = −0.122 (95% CI [−0.180, −0.064]; Z = −4.092; p < 0.001), indicating a significant, but weak, negative relationship between the measures. Heterogeneity was moderate, but we found no indication of significant differences between patients with medical conditions, psychiatric disorders or healthy controls, nor that mean age or percentage of female subjects moderated the relationship. The overall estimate became somewhat weaker after adjusting for possible publication bias.
Conclusions: Our results indicate that TAS-20 and LEAS measure different aspects of emotional functioning. The small overlap suggests that alexithymia and emotional awareness are distinct constructs of emotional well-being. Clinicians need to assess both aspects when considering treatment options for individual patients. Moreover, from the clinical standpoint, an easy reliable and valid way of measuring emotional awareness is still needed. More research should be focus on the differences between alexithymia and emotional awareness in specific conditions, but also how to integrate self-report instrument and observed based measures in a clinical situation.
Keywords: alexithymia, level of emotional awareness, LEAS, toronto alexithymia scale, TAS-20, meta-analysis
Introduction
Alexithymia, which literally means “lack of words for emotion,” is conceptualized as a general impairment in the capacity for processing emotional information, relating to both verbal and non-verbal stimuli (Lane et al., 1996). Individuals who are high in alexithymia have difficulties identifying their own or others' feelings (Lane and Schwartz, 1987) and show an externally-oriented thinking style and a scarcity of fantasy life (Taylor et al., 1997). An externally-oriented thinking style refers to a person's tendency to be concrete, stimulus-bound and oriented to practical aspects of a situation.
Several concepts partly overlap with alexithymia, such as emotion suppression, isolation, denial, and repression. However, while these concepts refer to active, defensive processes that reduce the experience or expression of emotion, alexithymia is generally considered to be a deficit rather than a defense (Lumley et al., 2010). The question of what type of deficit constitutes alexithymia, have not been settled. According to Lane et al. (2015a), an important question is whether the difficulty in putting emotions into words is observed because alexithymic individuals know what they feel but have difficulty describing it, or that simply are unaware of what they feel.
Another construct closely related to alexithymia is emotional awareness (Lane and Schwartz, 1987). Both concepts encompass potential difficulties in identifying one's own and others' feelings and having difficulties putting emotions into words. Emotional awareness can be said to be a facet of alexithymia, but is narrower in scope since its definition does not entail limited imaginal ability and externally-oriented thinking (Lumley et al., 2010).
Several self-report instruments to capture alexithymia are available (see for example the Bermond-Vorst Alexithymia Questionnaire, the Schalling-Sifneos Personality Scale and the MMPI alexithymia scale), but since its revision, the Toronto Alexithymia Scale-20 (TAS-20) has more or less become a standard in the field (Lumley et al., 2010). The TAS-20 is a 20 item self-report questionnaire measuring alexithymic traits using a five-point Likert scale (Bagby R. M. et al., 1994). The instrument includes three subscales: (1) Difficulty Identifying Feelings (DIF), (2) Difficulty Describing Feelings (DDF) and (3) Externally Oriented Thinking (EOT). The TAS-20 has been translated into 18 different languages and has shown rather robust reliability data (Taylor et al., 2003; albeit see also Kooiman et al., 2002). Studies have supported the construct validity by showing that high scores on TAS-20 are correlated with lower levels of psychological mindedness, need-for-cognition and openness to feelings and fantasy (Bagby M. et al., 1994) as well as affective orientation and emotional intelligence (Taylor et al., 2016), providing support that the TAS-20 captures an impairment in experiencing and describing emotions and is a valid measure of the alexithymia construct (Taylor et al., 2016).
Despite TAS-20 being in common use, it has been argued that what can be reported in self-report instruments such as the TAS-20 is actually a respondent's belief about her or his own ability to be emotionally aware and not actual emotional awareness capacity (Lundh et al., 2002). Observer-rated instruments may address this caveat and have been recommended to be used simultaneously with self-report instruments (Waller and Scheidt, 2006). Such instruments may include performance tests, where emotional capacity is directly assessed, or observer-based ratings, where emotional awareness capacity is judged by an external observer. A few performance tests (see for example the Level of Emotional Awareness Scale, the Rorschach Inkblot Test and the Scored Archetypal Test) and several observer ratings (see for example the Affect Consciousness Interview, the Beth Israel Hospital Questionnaire, the 24-item Toronto Structured Interview for Alexithymia and the 33-item Observer Alexithymia Scale) exist.
Since its conception, the Level of Emotional Awareness Scale (LEAS; Lane et al., 1990), with its straightforward administration and interpretive procedure, has become an increasingly used observer-rated test to capture facets of alexithymia and emotional awareness. The test consists of 20 vignettes that describe emotion-provoking interactions between two persons. Scores from 0 to 5 are assigned for the categories “self,” “other,” and “total,” with lower scores reflecting a lower level of emotional awareness. The inter-rater reliability of LEAS is typically high, with several studies having a Cronbach alpha of 0.90 and over. The LEAS has also met certain demands for criterion validity since it correlates with for example empathy and psychological maturity (Lane et al., 1990; Bydlowski et al., 2002; Igarashi et al., 2011). The instrument has been found to predict emotion-related criteria, such as the ability to identify emotions and physiological brain activation in response to emotional stimuli (Lane et al., 1995, 1996).
Research using both measures of alexithymia (TAS-20) and emotional awareness (LEAS) is still not that common. Studies although exist for different populations, including psychiatric, medical and healthy participants. Regarding psychiatric populations, somatoform/functional disorders and eating disorders have been more prominent studied. Correlations between TAS-20 and LEAS have consistently been negative, albeit not significant (Simson et al., 2002; Bydlowski et al., 2005; Subic-Wrana et al., 2005; Parling et al., 2010; Baker et al., 2014; Lane et al., 2015a). For healthy participants (including healthy controls) the results have been mixed, with a few studies showing positive correlations (Lundh et al., 2002; Waller and Scheidt, 2004; Bydlowski et al., 2005) although most studies show a negative association (Lane et al., 1998b; Subic-Wrana et al., 2001; Lumley et al., 2005; Parling et al., 2010; Igarashi et al., 2011; Baeza-Velasco et al., 2012; Baker et al., 2014; Lichev et al., 2014; Maroti et al., 2017). In the few studies including medical conditions (or medical controls), the results have also been mixed, with some studies showing positive associations (Baeza-Velasco et al., 2012; Maroti et al., 2017), while others do not (Consoli et al., 2009; Lane et al., 2015a; Burger et al., 2016; Neumann et al., 2017).
Despite the fact that the concepts of alexithymia and emotional awareness overlap theoretically, and that instruments such as the TAS-20 and LEAS have co-existed for more than 20 years, it is not quite clear how the constructs relate to each other empirically. Further, we do not know if alexithymia and emotional awareness may be more or less closely related in different patient populations. Therefore, the primary aim of this study was to perform a meta-analysis on the correlations between TAS-20 and LEAS. Given the construction of TAS and LEAS, a significant negative correlation was a primary hypothesis (i.e., higher self-reports of alexithymia would correlate with a lower level of emotional awareness). We further aim to explore potential moderators (age, gender, medical conditions) of the relationship. Since the relationship between these commonly used measures has not been investigated thoroughly before, our findings may yield important implications for theory, as well as for the measurement of alexithymia and emotional awareness in research and clinical practice.
Methods
Information sources and literature search
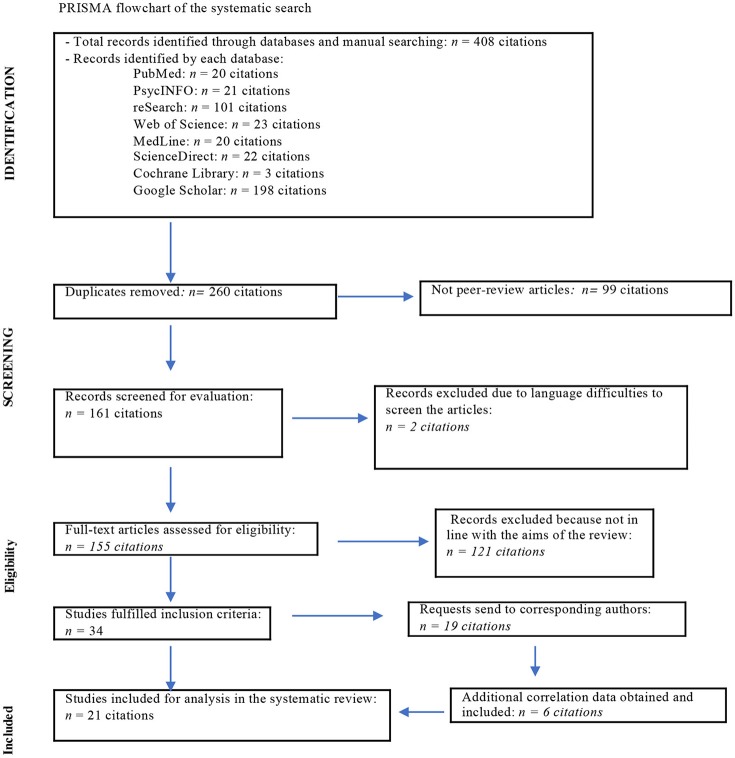
The International Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009) were used during the systematic search procedure. Searched databases included Pubmed, PsychInfo, MedLine, Web of Science, Cochrane, and ScienceDirect. We also searched through Karolinska Institutet's own search database called reSearch, an alternative to Scopus database, as well as an Internet search through Google Scholar. Each database was searched from its inception until the end of February 2018. The following terms were applied for the search strategy: “TAS-20 and LEAS” and “Toronto Alexithymia Scale and Level of Emotional Awareness,” excluding for Google Scholar. For Google Scholar the search term “TAS-20 and Level of emotional awareness” resulted into 198 items, which was more relevant to handle as compare to several thousands of hits when applying the terms “Toronto alexithymia scale” and “LEAS.” Furthermore, Google Scholar interpreted the “LEAS” as “Less.”
Usually the first combination (“TAS-20 and LEAS”) resulted in a larger number of articles than comparing with the other one (“Toronto Alexithymia Scale and Level of Emotional Awareness”). For calculation of the total amount of records in Figure 1, the results only of one combination (the large one) were included. This yielded 260 potentially relevant articles.
Figure 1.
PRISMA flowchart of the systematic search.
Eligibility criteria
Eligible articles included only original research studies published in peer-reviewed journals. We screened articles written in English, Germany, French, Italian, Spanish, Turkish and Persian if they have had English-written abstract and readable report data on TAS-20 and LEAS in the result section. In some articles, the correlations were mentioned as non-significant but not presented in detail. Therefore, we contacted 19 authors of those articles and asked for correlation data. In six cases, further data was obtained and included into the analysis. A total of 21 studies could finally be included in the meta-analysis.
Review articles, dissertations, books, publications related to scientific meetings, case reports and those articles having—for the authors of this article—unreadable languages in the abstract and/or result section (Turkish and Persian) were excluded. We also excluded 3 studies publishing data from the same cohort. Additionally, 121 articles were excluded because of inclusion/exclusions criteria and/or using the same cohort (3 articles). Almost all of the included studies were cross-sectional. In a few studies interventions were made and in that case the initial data of TAS-20 and LEAS was used.
Selection of articles and data extraction
Two authors (D.M. and I.B-L.) completed data extraction from the databases, according to the search terminology and eligibility criteria. They also read the abstracts and result section in order to identify the scales used for measurements. If necessary, they contacted corresponding authors for further details. Finally, if articles met the inclusion criteria, the full-text articles were extracted from databases or by ordering them from Karolinska Institutet's Library. All authors reached a consensus regarding eligibility criteria and inclusion of the article into the meta-analysis.
The following data was extracted for analysis: the size and characteristics of sub- and total groups, the main pathology studied, the values of TAS-20 and LEAS presented in mean and standard deviation, the coefficients and p-values of correlations between total TAS-20 and total LEAS.
Meta-analytic procedures
The correlations between TAS-20 and LEAS and their corresponding sample sizes were entered into the software program Comprehensive Meta-Analysis (CMA; version 2.2.064; Biostat, Englewood, NJ, USA). Procedures within CMA were then used to calculate study weights and the aggregated mean correlation, including its 95% confidence interval. The random-effects model (REM) was applied since we a priori assumed that the true correlation would differ between samples considering the broad inclusion criteria in terms of study populations (Borenstein et al., 2009).
When interpreting the aggregated mean correlation, we followed established conventions in the field and considered a correlation of ≥0.10 as weak, ≥0.30 as moderate, and ≥0.50 as strong (Cohen, 1992). We inspected forest plots for potential outliers and performed sensitivity analyses (using the “one study removed” and “cumulative analysis” features in CMA) to inspect the impact of single studies or samples.
We calculated the Q statistic to test for between-sample heterogeneity and we also estimated the I2 statistic, which expresses the degree of heterogeneity in terms of percentages: an I2 value of 0% indicates no heterogeneity, ≥25% low, ≥50% moderate, and ≥75% indicates substantial heterogeneity (Higgins et al., 2003). A higher I2 value suggests a greater potential for explaining any observed heterogeneity by exploring subgroups and covariates.
Moderators
Subgroup analyses within CMA were used to test if the association between TAS-20 and LEAS differed in different samples. Due to the low number of studies for specific conditions, we decided to group the study samples in three main categories: “Healthy Controls” (e.g., university students, stratified community samples), “Psychiatric Conditions” (e.g., eating disorders, substance disorders, mixed psychiatric disorders, somatoform disorders) or “Medical Conditions” (e.g., hypertension, traumatic brain injury, rheumatoid arthritis, fibromyalgia, chronic fatigue syndrome). Two studies were excluded from subgroup analyses since the samples could not be coded; Suslow et al. (2000) used a mixed sample of psychiatric patients and healthy controls and Pietri and Bonett (2016) studied women with or without a history of domestic violence with no data on diagnoses. The mixed effects method for subgroup analysis was used and since there were few studies in each group we pooled the estimate of Tau-Square across the subgroups as recommended by Borenstein et al. (2009).
Further, we also extracted continuous sample data for mean age and the percentage of females and applied random effects (method of moments) meta-regression models (Borenstein et al., 2009) in order to test for these as possible covariates of the main effect. Two studies (Lane et al., 1998b; Subic-Wrana et al., 2001) did not include data for sample mean age and were thus excluded from that specific analysis.
Publication bias
Lastly, we examined the possible presence of publication bias by inspecting funnel plots and applying (Duval and Tweedie, 2000) a trim-and-fill procedure (as implemented in Comprehensive Meta-Analysis version 2.2.064 package). The random effects model was applied in this procedure as well.
Results
Study characteristics
Study characteristics are presented in Table 1 (Lane et al., 1998b, 2015a; Suslow et al., 2000; Lundh et al., 2002; Simson et al., 2002; Waller and Scheidt, 2004; Bydlowski et al., 2005; Lumley et al., 2005; Consoli et al., 2009; Parling et al., 2010; Subic-Wrana et al., 2010; Igarashi et al., 2011; Baeza-Velasco et al., 2012; Lichev et al., 2014; Maroti et al., 2017; Neumann et al., 2017). In summary, the 21 studies included a total of 2,857 subjects and were conducted in six different countries (France, k = 5; Germany, k = 6; Japan, k = 1; Sweden, k = 3; USA, k = 5 and Australia, k = 1). The 21 studies investigated TAS-20 and LEAS in a total of 28 independent samples: twelve samples of healthy controls (total n = 1561), six samples of patients with medical conditions (n = 328), eight samples of patients with psychiatric conditions (n = 820) and two studies with a mixed sample of psychiatric patients and healthy controls (n = 148). The mean age across all samples was 37 year and on average 57% of sample subjects were female.
Table 1.
Study characteristics and descriptive statistics.
| Study | Country | Sample | Coded as | n | % female | Mean age | TAS-20 total (SD) | LEAS-20 total (SD) |
|---|---|---|---|---|---|---|---|---|
| *Baker et al., 2014 | Australia | Functional voice disorder HC |
Psychiatric | 20 20 |
100 | 39 | X | 76.2 (9.8) 80.8 (7.7) |
| *Baeza-Velasco et al., 2012 | France | Musculoskeletal disorders HC |
Medical | 39 22 |
100 | 53 | 48.7 (11.5) 39.7 (12.7) |
53.4 (7.1) 54.8 (6.2) |
| Burger et al., 2016+ | USA | Chronic musculoskeletal pain | Medical | 72 | 79 | 49 | 50.8 (12.3) | 31.3 (5.2) |
| Bydlowski et al., 2005 | France | Eating disorders HC |
Psychiatric | 70 70 |
100 | 19 | 75.9 (11.3) 66.9 (10.9) |
61.0 (8.8) 66.4 (6.0) |
| *Carton et al., 2010 | France | Substance disorders | Psychiatric | 64 | 22 | 38 | 56.2 (11.7) | 50.0 (8.33) |
| Consoli et al., 2009 | France | Essential hypertension secondary hypertension | Medical | 73 25 |
55 48 |
53 52 |
52.4 (11.6) 48.4 (12.1) |
46.2 (11.5) 52.8 (8.4) |
| Igarashi et al., 2011 | Japan | University students | Healthy | 344 | 65 | 20 | 44.1 (9.4) | 50.0 (9.38) |
| Lane et al., 1998b | USA | Healthy participants | Healthy | 380 | 52 | X | X | X |
| *Lane et al., 2015a+ | USA | Somatic symptom disorders Mixed medical conditions |
Psychiatric Medical |
59 30 |
85 67 |
43 45 |
51.81 (13.1) 44.45 (12.7) |
32.8 (4.28) 32.3 (4.85) |
| Lichev et al., 2014+ | Germany | Healthy participants | Healthy | 84 | 46 | 24 | 46.7 (10.1) | 36.1 (5.1) |
| Lundh et al., 2002 | Sweden | Healthy participants | Healthy | 78 | 83 | 28 | 42.0 (9.1) | 68.3 (8.9) |
| Lumley et al., 2005 | USA | Healthy participants | Healthy | 140 | 75 | 20 | 44.10 (10.3) | 62.70 (8.43) |
| Maroti et al., 2017+ | Sweden | Chronic fatigue HC |
Medical | 65 30 | 81 | 43 | 45.5 (11.4) 33.5 (6.4) |
29.5 (5.4) 34.7 (6.9) |
| *Neumann et al., 2017+ | USA | Traumatic brain injury | Medical | 24 | 24 | 46 | 61.54 (7.26) | 36.9 (7.9) |
| Parling et al., 2010 | Sweden | Anorexia Nervosa HC |
Psychiatric | 35 35 |
100 | 22 | 55.8 (12.2) 43.3 (10.1) |
62.8 (6.3) 62.4 (8.1) |
| *Pietri and Bonett, 2016 | France | Mixed (Victims of domestic violence+HC) |
Not included in sub-group analysis | 80 | 100 | 35 | X | X |
| Simson et al., 2002+ | Germany | Mixed psychiatric | Psychiatric | 146 | 73 | 31 | 55.2 (10.5) | 24.4 (5.2) |
| Subic-Wrana et al., 2001+ | Germany | University students | Healthy | 338 | 52 | X | X | 30.4 (6.0) |
| Subic-Wrana et al., 2005+ | Germany | Mixed psychiatric | Psychiatric | 386 | 72 | 41 | X | X |
| Suslow et al., 2000 | Germany | Mixed (Psychiatric+HC) | Not included in sub-group analysis | 68 | 56 | 28 | 45.9 (13.6) | 62.2 (10.4) |
| Waller and Scheidt, 2004++ | Germany | Somatoform disorder HC |
Psychiatric | 40 20 |
50 | 43 | 46.6 (8.9) 35.6 (8.9) |
2.7 (0.5) 2.7 (0.4) |
, Used LEAS-10 (instead of LEAS-20).
In this study the authors seem to have divided the total score of LEAS-10 with 10. X, missing data.
indicates articles those corresponding authors send additional data for correlations analysis.
Meta-analytic results
The aggregated mean correlation across all 28 samples was r = −0.122 (95% CI [−0.180, −0.064]; Z = −4.092; p < 0.001), suggesting a significant, but small, correspondence between the measures. We found no indication of outliers in sensitivity analyses and confidence intervals largely overlapped across samples (see forest plot in Table 2). Still, heterogeneity was significant (Q = 52.32; p = 0.002) and low to moderate (I2 = 48.39), indicating that the aggregated mean correlation may differ among subgroups of samples and/or may be moderated by covariates.
Table 2.
Forest plot of correlations between the TAS-20 and the LEAS of included studies.
| Study name | Subgroup within study | Statistics for each study | Correlation and 95% Cl | |||
|---|---|---|---|---|---|---|
| Correlation | Lower limit | Upper limit | p-value | |||
| Baker et al., 2014 | Healthy | −0.080 | −0.505 | 0.376 | 0.741 | 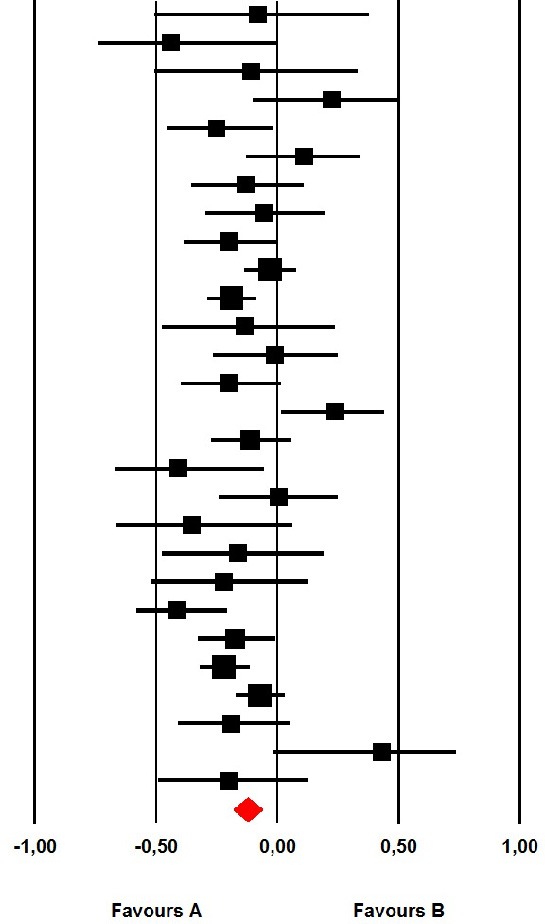 |
| Baker et al., 2014 | Psychiatric | −0.440 | −0.739 | 0.003 | 0.052 | |
| Baeza-Velasco et al., 2012 | Healthy | −0.108 | −0.507 | 0.329 | 0.636 | |
| Baeza-Velasco et al., 2012 | Medical | 0.224 | −0.098 | 0.504 | 0.172 | |
| Burger et al., 2016 | Medical | −0.249 | −0.454 | −0.018 | 0.035 | |
| Bydlowski et al., 2005 | Healthy | 0.110 | −0.128 | 0.336 | 0.366 | |
| Bydlowski et al., 2005 | Psychiatric | −0.130 | −0.354 | 0.108 | 0.285 | |
| Carton et al., 2010 | Psychiatric | −0.055 | −0.297 | 0.193 | 0.667 | |
| Consoli et al., 2009 | Medical | −0.200 | −0.383 | −0.002 | 0.048 | |
| Igarashi et al., 2011 | Healthy | −0.030 | −0.135 | 0.076 | 0.579 | |
| Lane et al., 1998b | Healthy | −0.190 | −0.285 | −0.091 | 0.000 | |
| Lane et al., 2015a | Medical | −0.136 | −0.473 | 0.236 | 0.477 | |
| Lane et al., 2015a | Psychiatric | −0.009 | −0.264 | 0.248 | 0.946 | |
| Lichev et al., 2014 | Healthy | −0.200 | −0.397 | 0.015 | 0.068 | |
| Lundh et al., 2002 | Healthy | 0.240 | 0.018 | 0.439 | 0.034 | |
| Lumley et al., 2005 | Healthy | −0.110 | −0.271 | 0.057 | 0.196 | |
| Maroti et al., 2017 | Healthy | −0.409 | −0.670 | −0.057 | 0.024 | |
| Maroti et al., 2017 | Medical | 0.006 | −0.238 | 0.250 | 0.962 | |
| Neumann et al., 2017 | Medical | −0.353 | −0.662 | 0.059 | 0.091 | |
| Parling et al., 2010 | Healthy | −0.160 | −0.473 | 0.188 | 0.369 | |
| Parling et al., 2010 | Psychiatric | −0.220 | −0.515 | 0.122 | 0.206 | |
| Pietri and Bonett, 2016 | Mixed | −0.410 | −0.578 | −0.209 | 0.000 | |
| Simson et al., 2002 | Psychiatric | −0.173 | −0.326 | −0.011 | 0.037 | |
| Subic-Wrana et al., 2001 | Healthy | −0.220 | −0.319 | −0.116 | 0.000 | |
| Subic-Wrana et al., 2005 | Psychiatric | −0.072 | −0.171 | 0.028 | 0.158 | |
| Suslow et al., 2000 | Mixed | −0.190 | −0.410 | 0.051 | 0.121 | |
| Waller and Scheidt, 2004 | Healthy | 0.430 | −0.015 | 0.733 | 0.058 | |
| Waller and Scheidt, 2004 | Psychiatric | −0.200 | −0.488 | 0.128 | 0.230 | |
| Total | −0.122 | −0.180 | −0.064 | 0.000 | ||
Moderators
In our moderator analyses, we found no significant difference (total between Q = 0.595; p = 0.743) between samples of Healthy Controls (r = −0.087, 95% CI [−0.173, 0.000], Z = −1.951; p = 0.051; k = 12), Psychiatric Conditions (r = −0.130, 95% CI [−0.237, 0.019], Z = −2.303; p = 0.021; k = 8) or Medical Conditions (r = −0.120, 95% CI [−0.257, 0.021], Z = −1.668; p = 0.095; k = 6), suggesting that the small, negative correlation between TAS and LEAS is quite robust across our coded subgroups. Further, in our meta-regression analyses, we found no indication that the correlation varied as a function of sample mean age (intercept = −0.063; β < 0.001; p = 0.648), nor the percentage of female subjects in the sample (intercept = −0.230; β = 0.002; p = 0.145), suggesting stability across age and gender.
Publication bias
Duval and Tweedie (2000) trim-and-fill procedure suggested possible presence of some publication bias and trimmed four studies to the right of the main aggregated effect, adjusting the overall estimate to r = −0.092.
Discussion
In this study, we performed a meta-analysis of the correlation between two commonly used measures of alexithymia and emotional awareness, i.e. the TAS-20 and the LEAS. Through our search strategy, we were able to include 21 studies, reporting on the correlation in 28 different samples. In line with our expectations, we found a significant negative correlation between the instruments; however, the relationship was weak (r = −0.122). Moderator analyses indicated that this small overlap was robust across subgroups of healthy subjects and patients with psychiatric or medical conditions and was unaffected by sample age or gender. The weak overall correlation suggests that TAS-20 and LEAS captures distinct facets of alexithymia and/or measure different constructs. The instruments should therefore be regarded as complimentary and be used according to specific research or clinical questions targeted.
Given that alexithymia and emotional awareness are closely related conceptually, the negligible overlap between TAS-20 and LEAS may seem puzzling. One explanation can simply be that although the instruments are related conceptually they are not related empirically. Studies have found that different areas and activations of brain networks might be involved in alexithymia and emotional awareness (Lane et al., 2015b). For example, functional neuroimaging studies have reported decreased activation of the dorsomedial prefrontal cortex when negative emotional stimuli were being processed for subjects reporting high alexithymia in TAS-20 (van der Velde et al., 2013). In contrast, increased activation of the dorsal anterior cingulate cortex has been associated with processing of emotions in subjects with a high emotional awareness capacity (Lane et al., 1998a; McRae et al., 2008).
Albeit puzzling from a conceptual standpoint, the small correlation between TAS-20 and LEAS is not unexpected from an empirical point of view. Several studies have shown that associations of self-report and observed based measures usually are low, whereas different self-reports and observed based measurement tend to correlate higher with each other (Lumley et al., 2005). For example, in a study evaluating the reliability and validity of the Dutch version of the OAS, the OAS correlation with TAS-20 was low, while a strong correlation was found for Toronto Structured Interview for Alexithymia and OAS (Meganck et al., 2010).
Another possible interpretation of the negligible overlap between the instruments is that it simply may be difficult to infer one's own emotional awareness capacity using a self-report measure like TAS-20, otherwise a stronger negative correlation would be expected. This idea parallels research into subjective memory and objective memory where only a negligible or small correlation is typically found (Burmester et al., 2016).
In line with this, Lundh et al. (2002) found that almost 20% of the individuals reported low levels of alexithymia but performed worse than others on the LEAS. In addition, 15% of patients with high levels of alexithymia performed better than others on the LEAS. Thus, the relationship between alexithymia and emotional awareness may be non-linear, which could also explain the low aggregated correlation found in this review. If not non-linear, at least different depending on patient characteristic studied. In Lundh et al.'s (2002) study, TAS-20 was found to correlate highly with perfectionism. This result can be said to corroborated by a study in which raters, who were blind to patient TAS-20 scores, coded videotaped interviews for the number of emotions expressed by psychiatric patients. Those patients who rated themselves as having more difficulty describing their emotions were actually better able to express their emotions than others, not worse (Leising et al., 2009). Future research should therefore investigate if perfectionistic tendencies contributes to the correlation between TAS-20 and LEAS. Moreover, given that almost 20% of the individuals reported low levels of alexithymia but performed worse than others on the LEAS in Lundh et al.'s (2002) study, the contribution of somatization may be important in future research. One hallmark of somatization is the tendency to report few emotional problems (i.e., pensée opératoire) but actually have internal emotional conflicts (Taylor et al., 1997).
The weak relationship between alexithymia and emotional awareness also seem to contradict theories of emotion that suggest that a persons ability to use words and concepts to label emotional experience is related to their ability to experience and differentiate emotions (e.g., Barrett, 2006; Kashdan et al., 2015). Our results indicate that some people who report a lack of words for emotions on the TAS-20 are clearly quite able to use emotional words when describing motions in an observer-rated procedure such as LEAS. Conversely, some people with low alexithymia may show limited emotional awareness on the LEAS. While, again, this may indicate that it is difficult to infer one's own emotional awareness capacity using self-report measures, it could also indicate that the ability to perceive and experience emotions is not simply a matter of conceptual capacity but other mechanisms may also be involved.
Our results may also have clinical implications since an overestimation or underestimation of patients' particular emotional capacities could affect the outcome of therapeutic interventions. Clinicians may need to consider both alexithymia and emotional awareness and adjust therapeutic interventions to address the patients' particular beliefs and deficits. For example, having lower emotional awareness capacity, as measured with the LEAS, has been shown to moderate treatment effectiveness in both cognitive behavioral therapy (CBT) and psychodynamic psychotherapy (PDT) for patients with a comorbid psychiatric diagnosis (Beutel et al., 2013). Reporting higher levels of alexithymia on TAS-20 has also been found to be a negative prognostic indicator for psychodynamic-oriented treatments (McCallum et al., 2003; Leweke et al., 2009; Ogrodniczuk et al., 2011). Alexithymia may not affect more structured cognitive-behavioral treatments, and certain results do indicate that alexithymia may even be associated with better outcomes of such treatments (Rufer et al., 2004; Spek et al., 2008; de Haan et al., 2011). In other words, and as stated above, TAS-20 and LEAS should not be used interchangeably, but could be informative when used simultaneously in order to find the most suitable treatment options for a particular patient. In somatic diseases, alexithymia also predicted or moderated treatment outcomes (Porcelli et al., 2003). Thus, reducing alexithymia contribute to ameliorate symptoms in patients with functional gastrointestinal disorders (Porcelli et al., 2017) and cancer-related pain (Porcelli et al., 2007). Recent study on antidepressants indicates that pharmacological treatment per see with known side effects such as emotional blunting contributes to at least of some aspects of alexithymia (DIF) (Kajanoja et al., 2018).
On a clinical note, using both the instrument TAS-20 and LEAS to capture alexithymia and emotional awareness is time consuming. For example, it can take patients up to 1.5 h to complete even the 10-vignettes version of LEAS (Maroti et al., 2017) and even a skilled rater needs at least 15–20 min to score the answers. Although computerized versions of rating LEAS have been developed (Barchard et al., 2010) an easy, reliable and valid way of measuring emotional awareness is still needed. If judgements from the clinician are involved, the clinicians own emotional awareness capacity needs to be taken into account, since the clinician's capacity sets the limit of the level of emotional awareness that reasonably can be detected.
Emotional awareness might be influenced by several factors and circumstances, which might be difficult to capture in research situation. Nevertheless, our results increase knowledge and awareness how to interpret the scales in research practice and point out the necessity to develop less time consuming clinically adapted scales or tests.
Limitations
Through our search strategy, we identified 34 studies that were eligible but could include 21 due to missing, incomplete or unclear data. We tried to address this by emailing the first authors. Most of the excluded studies were published in a language other than English (i.e., French); hence, our results may have been systematically skewed due to the selective inclusion of studies. However, an ad hoc subgroup test of the difference between countries proved insignificant (between Q = 0.073; p = 0.787). Also, given that adjustment for publication bias lowered the overall estimate even further, it seems unlikely that additional studies would change our overall result.
This study is focused on the correlation between the total scores of TAS-20 and LEAS. It could be that the instruments overlap more when looking at particular subscales. However, because of reliability issues, using subscales of TAS-20 has not been recommended (Kooiman et al., 2002). Additionally, since the subscales of the instruments focus on quite different aspects (e.g., “difficulty describing feelings” in TAS-20 and “other” in LEAS), we suspect that it will be difficult to interpret the meaning of a possible overlap or a lack thereof. Since the total scores of the instruments aim at assessing each respective “phenomenon” (i.e., alexithymia or emotional awareness), it was determined to be the most suitable level of analysis for this review.
Another limitation of this study was that distress/negative affect (such as anxiety and depression) was not used as a covariate. Typically, TAS-20 but not LEAS (Lane et al., 2015b) have been found to correlate with negative affect. Moreover, several studies have shown that associations between LEAS and the population studied were not altered by removing variance due to negative affect (Bydlowski et al., 2005; Subic-Wrana et al., 2005; Consoli et al., 2009). On the other hand, control for negative affect made associations with the TAS-20 non-significant. Taken together, this implies that negative affects influence the instrument in this study in a different way and might impact the low correlation found between TAS-20 and LEAS.
Interim conclusion
In this review, we tried to answer the question of whether TAS-20 and LEAS correlate in healthy populations and medical and psychiatric conditions. The results indicate that the correlation is small to negligible in all studied groups. These particular instruments should therefore not be used interchangeably and instead be used in order to answer specific research questions.
Author contributions
DM and IB-L performed and compiled the main bibliography work. PL performed the statistical analysis. IB-L coordinated and supervised the process of manuscript writing. All authors wrote the paper and approved the final version for submission.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are thankful to those authors who contributed with additional correlation data when contacted by mail.
References
- Baeza-Velasco C., Carton S., Almohsen C., Blotman F., Gély-Nargeot M. C. (2012). Alexithymia and emotional awareness in females with Painful Rheumatic Conditions. J. Psychosom. Res. 73, 398–400. 10.1016/j.jpsychores.2012.08.008 [DOI] [PubMed] [Google Scholar]
- Bagby M., Parker J. D., Taylor G. J. (1994). The twenty-item Toronto Alexithymia Scale. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 38, 23–32. 10.1016/0022-3999(94)90005-1 [DOI] [PubMed] [Google Scholar]
- Bagby R. M., Taylor G. J., Parkers J. D. (1994). The twenty-item Toronto Alexithymia Scale. Convergent, discriminant and concurrent validity. J. Psychosom. Res. 38, 33–40. 10.1016/0022-3999(94)90006-X [DOI] [PubMed] [Google Scholar]
- Baker J., Oates J., Leeson E., Woodford H., Bond M. (2014). Patterns of emotional expression and responses to health and illness in women with functional voice disorders (MTVD) and a comparison group. J. Voice 28, 762–769. 10.1016/j.jvoice.2014.03.005 [DOI] [PubMed] [Google Scholar]
- Barchard K., Bajgar J., Ermini-Leaf D., Lane R. (2010). Computer scoring of the levels of emotional awareness scale. Behav. Res. Methods 42, 586–595. 10.3758/BRM.42.2.586 [DOI] [PubMed] [Google Scholar]
- Barrett L. F. (2006). Solving the emotion paradox: categorization and the experience of emotion. Pers. Soc. Psychol. Rev. 10, 20–46. 10.1207/s15327957pspr1001_2 [DOI] [PubMed] [Google Scholar]
- Beutel M. E., Scheurich V., Knebel A., Michal M., Wiltink J., Graf-Morgenstern M., et al. (2013). Implementing panic-focused psychodynamic psychotherapy into clinical practice. Can. J. Psychiatry 58, 326–334. 10.1177/070674371305800604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. (2009). Introduction to Meta-analysis. Chichester: JohnWiley & Sons. [Google Scholar]
- Burger A., Lumley M., Carty J., Latsch D., Thakur E., Hyde-Nolan H., et al. (2016). The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: a preliminary, uncontrolled trial. J. Psychosom. Res. 81, 1–8. 10.1016/j.jpsychores.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burmester B., Leathem J., Merrick P. (2016). Subjective cognitive complaints and objective cognitive function in aging: a systematic review and meta-analysis of recent cross-sectional findings. Neuropsychol. Rev. 26, 376–393. 10.1007/s11065-016-9332-2 [DOI] [PubMed] [Google Scholar]
- Bydlowski S., Corcos M., Jeammet P., Paterniti S., Berthoz S., Laurier C., et al. (2005). Emotion-processing deficits in eating disorders. Int. J. Eat. Disord. 37, 321–329. 10.1002/eat.20132 [DOI] [PubMed] [Google Scholar]
- Bydlowski S., Corcos M., Paterniti S., Guilbaud O., Jeammet P., Consoli S. M. (2002). [French validation study of the levels of emotional awareness scale]. Encephale 28, 310–320. [PubMed] [Google Scholar]
- Carton S., Bayard S., Paget V., Jouanne C., Varescon I., Edel Y., et al. (2010). Emotional awareness in substance-dependent patients. J. Clin. Psychol. 66, 599–610. 10.1002/jclp.20662 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychol. Bull. 112, 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Consoli S. M., Lemogne C., Roch B., Laurent S., Plouin P., Lane R. D. (2009). Differences in emotion processing in patients with essential and secondary hypertension. Am. J. Hypertens. 23, 515–521. 10.1038/ajh.2010.9 [DOI] [PubMed] [Google Scholar]
- Duval S. J., Tweedie R. L. (2000). A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J. Am. Stat. Assoc. 95, 89–98. 10.1080/01621459.2000.10473905 [DOI] [Google Scholar]
- de Haan H. A., Joosten E. A., Wijdeveld A. G., Boswinkel P. B., van der Palen J., De Jong C. A. (2011). Cognitive behavioural treatment is as effective in high- as in low-scoring alexithymic patients with substance-related disorders. Psychother. Psychosom. 80, 254–255. 10.1159/000322030 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. (2003). Measuring inconsistency in meta-analyses. Br. Med. J. 327, 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igarashi T., Komaki G., Lane R. D., Moriguchi Y., Nishimura H., Arakawa H., et al. (2011). The reliability and validity of the Japanese version of the Levels of Emotional Awareness Scale (LEAS-J). Biopsychosoc. Med. 5:2. 10.1186/1751-0759-5-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajanoja J., Scheinin N. M., Karukivi M., Karlsson L., Karlsson H. (2018). Is antidepressant use associated with difficulty identifying feelings? A brief report. Exp. Clin. Psychopharmacol. 26, 2–5. 10.1037/pha0000165 [DOI] [PubMed] [Google Scholar]
- Kashdan T. B., Barrett L. F., McKnight P. E. (2015). Unpacking emotion differentiation: transforming unpleasant experience by perceiving distinctions in negativity. Curr. Dir. Psychol. Sci. 24, 10–16. 10.1177/0963721414550708 [DOI] [Google Scholar]
- Kooiman C. G., Spinhoven P., Trijsburg R. W. (2002). The assessment of alexithymia: a critical review of the literature and a psychometric study of the Toronto Alexithymia Scale-20. J. Psychosom. Res. 53, 1083–1090. 10.1016/S0022-3999(02)00348-3 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Hsu C., Locke D. E. C., Ritenbaugh C., Stonnington C. M. (2015a). Role of theory of mind in emotional awareness and alexithymia: implications for conceptualization and measurement. Conscious. Cogn. 33, 398–405. 10.1016/j.concog.2015.02.004 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Kivley L. S., Du Bois M. A., Shamasundara P., Schwartz G. E. (1995). Levels of emotional awareness and the degree of right hemispehric dominance in the perception of facial emotion. Neuropsychologia 33, 525–538. 10.1016/0028-3932(94)00131-8 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Quinlan D. M., Schwartz G. E., Walker P. A., Zeitlin S. B. (1990). The Levels of Emotional Awareness Scale: a cognitive-developmental measure of emotion. J. Pers. Assess. 55, 124–134. 10.1080/00223891.1990.9674052 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Reiman E., Axelrod B., Yun L., Holmes A., Schwartz G. (1998a). Neural correlates of emotional awareness. Evidence of an interaction between emotion and attention in the anterior cingulate cortex. J. Cogn. Neurosci. 10, 525–535. 10.1162/089892998562924 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Schwartz G. E. (1987). Levels of emotional awareness: a cognitive-developmental theory and its application to psychopathology. Am. J. Psychiatry 144, 133–143. [DOI] [PubMed] [Google Scholar]
- Lane R. D., Sechrest L., Reidel R., Weldon V., Kaszniak A., Schwartz G. E. (1996). Impaired verbal and nonverbal emotion recognition in alexithymia. Psychosom. Med. 58, 203–210. 10.1097/00006842-199605000-00002 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Sechrest L., Riedel R. (1998b). Sociodemographic correlates of alexithymia. Compr. Psychiatry 39, 377–385. 10.1016/S0010-440X(98)90051-7 [DOI] [PubMed] [Google Scholar]
- Lane R. D., Weihs K. L., Herring A., Hishaw A., Smith R. (2015b). Affective agnosia: expansion of the alexithymia construct and a new opportunity to integrate and extend Freud's legacy. Neurosci. Biobehav. Rev. 55, 594–611. 10.1016/j.neubiorev.2015.06.007 [DOI] [PubMed] [Google Scholar]
- Leising D., Grande T., Faber R. (2009). The Toronto Alexithymia Scale (TAS-20): a measure of general psychological distress. J. Res. Pers. 43, 707–710. 10.1016/j.jrp.2009.03.009 [DOI] [Google Scholar]
- Leweke F., Bausch S., Leichsenring F., Walter B., Stingl M., et al. (2009). Alexithymia as a predictor of outcome of psychodynamically oriented inpatient treatment inpatient treatment. Psychother. Res. 19, 323–331. 10.1080/10503300902870554 [DOI] [PubMed] [Google Scholar]
- Lichev V., Rufer M., Rosenberg N., Ihme K., Grabe H., Kugel H., et al. (2014). Assessing alexithymia and emotional awareness: relations between measures in a German non-clinical sample. Compr. Psychiatry 55, 952–959. 10.1016/j.comppsych.2013.12.013 [DOI] [PubMed] [Google Scholar]
- Lumley M. A., Gustavson B. J., Partridge R. T., Labouvie-Vief G. (2005). Assessing alexithymia and related emotional ability constructs using multiple methods: interrelationships among measures. Emotion 5, 329–342. 10.1037/1528-3542.5.3.329 [DOI] [PubMed] [Google Scholar]
- Lumley M. A., Neely L. C., Burger A. J. (2010). The assessment of alexithymia in medical settings: implications for understanding and treating health problems. J. Pers. Assess. 89, 230–246. 10.1080/00223890701629698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundh L. G., Johnsson A., Sundqvist K., Olsson H. (2002). Alexithymia, memory of emotion, emotional awareness, and perfectionism. Emotion 2, 361–379. 10.1037/1528-3542.2.4.361 [DOI] [PubMed] [Google Scholar]
- Maroti D., Molander P., Bileviciute-Ljungar I. (2017). Differences in alexithymia and emotional awareness in exhaustion syndrome and chronic fatigue syndrome. Scand. J. Psychol. 58, 52–61. 10.1111/sjop.12332 [DOI] [PubMed] [Google Scholar]
- McCallum M., Piper W. E., Ogrodniczuk J. S., Joyce A. S. (2003). Relationships among psychological mindedness, alexithymia and outcome in four forms of short-term psychotherapy. Psychol. Psychother. 76, 133–144. 10.1348/147608303765951177 [DOI] [PubMed] [Google Scholar]
- McRae K., Reiman E., Fort C., Chen K., Lane R. (2008). Association between trait emotional awareness and dorsal anterior cingulate activity during emotion is arousal-dependent. Neuroimage 41, 648–651. 10.1016/j.neuroimage.2008.02.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meganck R., Vanheule S., Desmet M., Inslegers R. (2010). The Observer Alexithymia Scale: a reliable and valid alternative for alexithymia measurement? J. Pers. Assess. 92, 175–185. 10.1080/00223890903510449 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann D., Malec J. F., Hammond F. M. (2017). Reductions in alexithymia and emotion dysregulation after training emotional self-awareness following traumatic brain injury: a phase I trial. J. Head Trauma Rehabil. 32, 286–295. 10.1097/HTR.0000000000000277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogrodniczuk J. S., Piper W. E., Joyce A. S. (2011). Effect of alexithymia on the process and outcome of psychotherapy: a programmatic review. Psychiatry Res. 190, 43–48. 10.1016/j.psychres.2010.04.026 [DOI] [PubMed] [Google Scholar]
- Parling T., Mortazavi M., Ghaderi A. (2010). Alexithymia and emotional awareness in anorexia nervosa: time for a shift in the measurement of the concept? Eat. Behav. 11, 205–210. 10.1016/j.eatbeh.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Pietri M., Bonett A. (2016). Alexithymia and chronic victimization in partnership. Ann Medicopsychol. 175, 223–228. 10.1016/j.amp.2016.06.004 [DOI] [Google Scholar]
- Porcelli P., Bagby R. M., Taylor G. J., De Carne M., Leandro G., Todarello O. (2003). Alexithymia as predictor of treatment outcome in patients with functional gastrointestinal disorders. Psychosom. Med. 65, 911–918. [DOI] [PubMed] [Google Scholar]
- Porcelli P., De Carne M., Leandro G. (2017). The role of alexithymia and gastrointestinal-specific anxiety as predictors of treatment outcome in irritable bowel syndrome. Compr. Psychiatry 73, 127–135. 10.1016/j.comppsych.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Porcelli P., Tulipani C., Maiello E., Cilenti G., Todarello O. (2007). Alexithymia, coping, and illness behavior correlates of pain experience in cancer patients. Psychooncology 16, 644–650. 10.1002/pon.1115 [DOI] [PubMed] [Google Scholar]
- Rufer M., Hand I., Braatz A., Alsleben H., Fricke S. (2004). A prospective study of alexithymia in obsessive-compulsive patients treated with multimodal cognitive-behavioral therapy. Psychother. Psychosom. 73, 101–106. 10.1159/000075541 [DOI] [PubMed] [Google Scholar]
- Simson U., Martin K., Schäfer R., Franz M., Janssen P. (2002). [Changes in alexithymia and emotional awareness during psychotherapeutic inpatient treatment]. Psychother. Psychosom. Med. Psychol. 52, 454–460. 10.1055/s-2006-940127 [DOI] [PubMed] [Google Scholar]
- Spek V., Nyklíček I., Cuijpers P., Pop V. (2008). Alexithymia and cognitive behaviour therapy outcome for subthreshold depression. Acta Psychiatr. Scand. 118, 164–167. 10.1111/j.1600-0447.2008.01199.x [DOI] [PubMed] [Google Scholar]
- Subic-Wrana C., Beutel M. E., Knebel A., Lane R. D. (2010). Theory of mind and emotional awareness deficits in patients with somatoform disorders. Psychosom. Med. 72, 404–411. 10.1097/PSY.0b013e3181d35e83 [DOI] [PubMed] [Google Scholar]
- Subic-Wrana C., Bruder S., Thomas W., Lane R., Köhle K. (2005). Emotional awareness deficits in inpatients of a psychosomatic ward: a comparison of two different measures of alexithymia. Psychosom. Med. 67, 483–489. 10.1097/01.psy.0000160461.19239.13 [DOI] [PubMed] [Google Scholar]
- Subic-Wrana C., Thomas W., Huber M., Köhl K. (2001). Levels of emotional awareness scale (LEAS) die deutsche version eines neuen alexithymietests. Psychotherapeut 46, 176–181. 10.1007/s002780100157 [DOI] [Google Scholar]
- Suslow T., Donges U., Kersting A., Arolt V. (2000). 20-item toronto alexithymia scale: do difficulties describing feelings assess proneness to shame instead of difficulties symbolizing emotions? Scand. J. Psychol. 41, 329–334. 10.1111/1467-9450.00205 [DOI] [PubMed] [Google Scholar]
- Taylor G., Bagby R., Parker J. (1997). Disorders of Affect Regulation. Alexthymia in Medical and Psychiatric Illness. Cambridge: University Press. [Google Scholar]
- Taylor G. J., Bagby R. M., Parker J. D. A. (2003). The 20-item toronto alexithymia scale IV. Reliability and factorial validity in different languages and cultures. J. Psychosom. Res. 55, 277–283. 10.1016/S0022-3999(02)00601-3 [DOI] [PubMed] [Google Scholar]
- Taylor G. J., Bagby M., Parker J. D. A. (2016). What's in the name ‘alexithymia’? A commentary on “Affective agnosia: expansion of the alexithymia construct and a new opportunity to integrate and extend Freud's legacy.” Neurosci. Biobehav. Rev. 68, 1006–1020. 10.1016/j.neubiorev.2016.05.025 [DOI] [PubMed] [Google Scholar]
- van der Velde J., Servaas M. N., Goerlich K. S., Bruggeman R., Horton P., Costafreda S. G., et al. (2013). Neural correlates of alexithymia: a meta-analysis of emotion processing studies. Neurosci. Biobehav. Rev. 37, 1774–1785. 10.1016/j.neubiorev.2013.07.008 [DOI] [PubMed] [Google Scholar]
- Waller E., Scheidt C. E. (2004). Somatoform disorders as disorders of affect regulation: a study comparing the TAS-20 with non-self-report measures of alexithymia. J. Psychosom. Res. 57, 239–247. 10.1016/S0022-3999(03)00613-5 [DOI] [PubMed] [Google Scholar]
- Waller E., Scheidt C. E. (2006). Somatoform disorders as disorders of affect regulation: a development perspective. Int. Rev. Psychiatry 18, 13–24. 10.1080/09540260500466774 [DOI] [PubMed] [Google Scholar]