Abstract
Objectives
Enhanced/disturbed activities of monocytes are crucial for perpetuation and for development of rheumatoid arthritis (RA). Therefore, knowledge about monocyte activities and regulation of molecular pathways operating within monocytes early in the course of RA development may help to predict the progression to the full-blown disease. We aimed to investigate the profile of miRNAs expression in circulating monocytes and monocyte-related cytokines in sera of individuals at undifferentiated arthritis (UA) stage, wich could serve as new biomarkers for RA development.
Material and methods
Magnetically sorted monocytes from peripheral blood of 20 UA patients served for total RNA isolation. RNA samples were used for microRNA profiling. Concentrations of CCL3/MIP-1α, M-CSF, CCL2/MCP-1, IL-6, TNF-α and IL-15 in sera of UA patients were measured using ELISA assays. Verification of diagnosis after 4 years of follow-up led to the identification of patients who developed RA (UA→RA patients) and patients who remained still in UA phase (UA → UA patients). Comparisons between patients groups were performed using two-tailed Mann-Whitney U test.
Results
We identified 50 miRNAs in monocytes with the largest variation of expression across all patients samples. From these selected miRNAs, expression of miR-642b-5p, miR-483-3p, miR-371b-5p were significantly up-regulated and miR-25-3p and miR-378d were significantly down-regulated in UA → RA vs. UA → UA patients. This specific pattern of miRNAs expression in circulating monocytes paralleled elevated IL-15 and M-CSF concentrations in sera of UA patients who progressed to RA.
Conclusions
Results of our pilot study indicate that altered activity of monocytes can be detected at early stages of RA. We found new miRNA candidates differentially expressed in peripheral blood monocytes and elevated concentrations of IL-15 and M-CSF involved in monocyte activity and differentiation in patients with UA who subsequently developed RA, in comparison to UA patients who did not progress to RA after 4 years follow-up.
Keywords: undifferentiated arthritis, rheumatoid arthritis, microRNA, cytokines
Introduction
Rheumatoid arthritis (RA) is characterised by immunologic disturbances that can result in autotolerance breakdown and ultimately autoimmunization. The early biological events triggering RA are not well understood. The cellular mechanisms that drive progression of the disease from its early stage – undifferentiated arthritis (UA), to full-blown RA remain also undefined. In this situation identification of key biomarkers that may help to identify UA patients who will develop RA or other diseases in the near future, may create the window of opportunity for more disease-oriented, aggressive treatment that could change the course of disease development or even reverse pathological processes and led to the full remission. Thus, several studies have sought measurable parameters e.g. microRNA (miRNA) or pro-inflammatory cytokines to predict outcomes (and therapeutic strategy) on an individual basis.
miRNAs are non-coding small RNAs molecules that function as post-transcriptional regulators of gene expression [1]. Primary RNA molecule is cleavaged into 19–22 bp mature miRNA that is incorporated into RNA-indicated silencing complex (RISC). miRNAs binds to the target sites in 3′ untranslated regions of target messenger RNA while the protein RISC complex inhibits translation of the mRNA leading to gene silencing [2, 3]. miRNAs participate in the regulation of a wide range of cellular processes and altered expression of specific miRNAs was found to be associated with development of several disorders. Furthermore, in some human conditions miRNAs can be used as diagnostic and prognostic biomarkers [4]. There are also evidences showing dysregulation of miRNAs in RA [5]. The changes of miRNAs expression in RA can contribute to altered function of synovial fibroblasts [6−8], PBMC [8, 9], T cells [10], B cells [11] as well as monocytes [12−14].
Monocytes are central to the initiation of inflammation and bone erosion in RA [15]. Presence of high numbers of macrophages in the synovium is related to clinical manifestation of the disease and effective therapy [16]. In addition, activation and migration of monocytes from peripheral blood into the joints are considered as early events in the development of RA [17] and circulating monocytes were already found to be increased in early RA patients [18]. Interestingly, it was recently shown that disturbed expression of miRNAs is associated with production of pro-inflammatory cytokines, migratory potential and prolonged survival of RA monocytes [12−14]. Therefore, understanding the molecular pathways regulation in monocytes and the activity of these cells, especially at early stages of RA development, is of crucial importance as it may help to predict the progression to the full-blown disease. To date however, there are scarce data available regarding monocytes disturbances at early stages of RA.
Aim of the study
In this study we aimed to investigate the profile of miRNAs expression in circulating monocytes and monocyte-related cytokines in peripheral blood of individuals at UA stage that could serve as new biomarkers for RA development.
Material and methods
Twenty patients with UA (mean age 55.4 years) who did not meet the criteria for the classification of RA, any other rheumatic disease nor infectious arthritis, crystalopathy or post-traumatic arthritis were enrolled in the study between November 2012 and January 2013. Allowed medication at inclusion included pain killers and/or nonsteroidal anti-inflammatory drugs only. All individuals enrolled in the study gave informed consent and the study was approved by the National Institute of Geriatrics, Rheumatology and Rehabilitation Ethics Committee.
Paired peripheral blood samples were obtained from every patient enrolled in the study for monocytes isolation (using sodium citrate as an anticoagulant) and for serum collection.
Monocytes were isolated by magnetic separation accordingly to CD14 molecule expression (Miltenyi Biotec, Germany). Magnetically sorted CD14+ monocytes served for total RNA isolation (Qiagen, Germany). Fluorescently labelled samples of total RNA (miRCURY LNA microRNA Hi-Power Labelling Kit, Hy3/Hy5; Exiqon, Denmark) were hybridized to miRCURY LNA microRNA Array 7th gen (Exiqon), which contains capture probes targeting all microRNAs for human registered in the miRBASE 18.0., and scanned using Microarray Scanner System (Agilent Technologies, USA). The image analysis was carried out using ImaGene 9 Software (Exiqon). The quantified signals were background corrected (Normexp with offset value 10) and normalized using the global Lowess (Locally Weighted Scatterplot Smoothing) regression algorithm.
The concentrations of chemokine (C-C motif) ligand 3/macrophage inflammatory protein 1 α (CCL3/MIP-1α), macrophage colony-stimulating factor (M-CSF), chemokine C-C motif ligand 2/monocyte chemoattractant protein-1 (CCL2/MCP-1), chemokine (C-Cmotif) ligand 11/edaxin 11 interleukin 6 (IL-6), tumour necrosis factor α (TNF-α) and IL-15 in sera of UA patients were measured using ELISA assays from respectively: R&D Systems (CCL3/MIP-1α, M-CSF, CCL2/MCP-1, IL-6 and CCL11/eotaxin), eBioscience (TNF-α) and RayBiotech (IL-15). The cut-off values for detection of the respective cytokine were as follows: 7.81 pg/ml (CCL3), 15.6 pg/ml (M-CSF and CCL2), 9.38 pg/ml (IL-6), 15 pg/ml (CCL11), 4 pg/ml (TNF-α) and 3.3 pg/ml (IL-15). ELISA assays were performed accordingly to the manufacturer instructions.
Physical examination of the joints and measurement of acute reactants (CRP and ESR) and autoantibodies in peripheral blood samples constituted part of normal clinical diagnostic process. Cut-off values for RF and anti-citrullinated protein antibodies (ACPA) Ab detection were, respectively < 34 IU/ml and < 17 U/ml.
Evaluation of disease progression was carried out after 4 years of follow-up. Patients were treated during follow-up period accordingly to the intensity of signs and symptoms of arthritis using MTX and/or glucocorticosteroids or sulfasalazine, and/or NSAIDs. Comparisons between patients groups were performed using two tailed Mann Whitney U test (Statistica vol. 6.0 software; StatSoft, Poland). P-values less than 0.05 were considered significant.
Results
Out of 20 patients with UA enrolled in the study ten patients were verified for diagnosis after 4 years of follow-up (10 patients did not respond to the call for clinical re-evaluation). Four patients developed full-blown RA (UA → RA patients) and 6 patients remained still in UA phase (UA → UA patients).
Analysis of demographic and immunological data of UA → RA vs. UA → UA patients revealed that at baseline both groups of patients were at the same age (median: 50.5, range 37–59 years, 4 women vs. median: 52.5, range 32–63 years 4 women, 2 men), were characterised by comparable levels of CRP (median: 9.0, range 1–22 mg/l vs. median: 8.0, range 1–21 mg/l), comparable levels of ESR (median: 37.0, range 4–47 mm/h vs. median: 34.0, range 15–44 mm/h) as well as swollen joins count (median: 3.0, range 1–9 vs. median: 2.5, range 1–4). However, the autoantibody status at baseline differed between UA → RA vs. UA → UA patients groups. All UA → RA patients were positive for autoantibodies (patient no 1: 50 IU ACPA Ab; patient no 2: 12 IU ACPA Ab; patient no 3: > 500 IU ACPA Ab and 193 IU RF; patient no 4 > 500 IU ACPA Ab), while none of the UA → UA patient was positive for investigated autoantibodies.
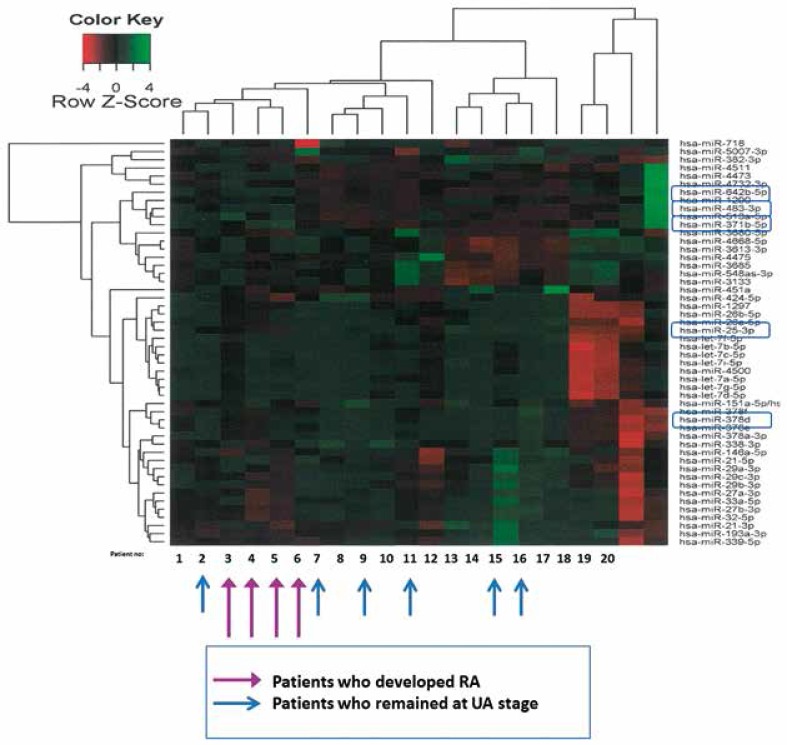
Following computational unsupervised analysis we identified 50 miRNAs in monocytes that had the largest variation across all patients samples (Fig. 1).
Fig. 1.
Heat Map and Unsupervised Hierarchical Clustering of the top 50 microRNAs that have the largest expression differences across all samples. The normalized log ratio values have been used for the analysis. MiRNA candidates of significantly changed expression in monocytes of UA → RA vs. UA → UA patients are indicated in rectangles.
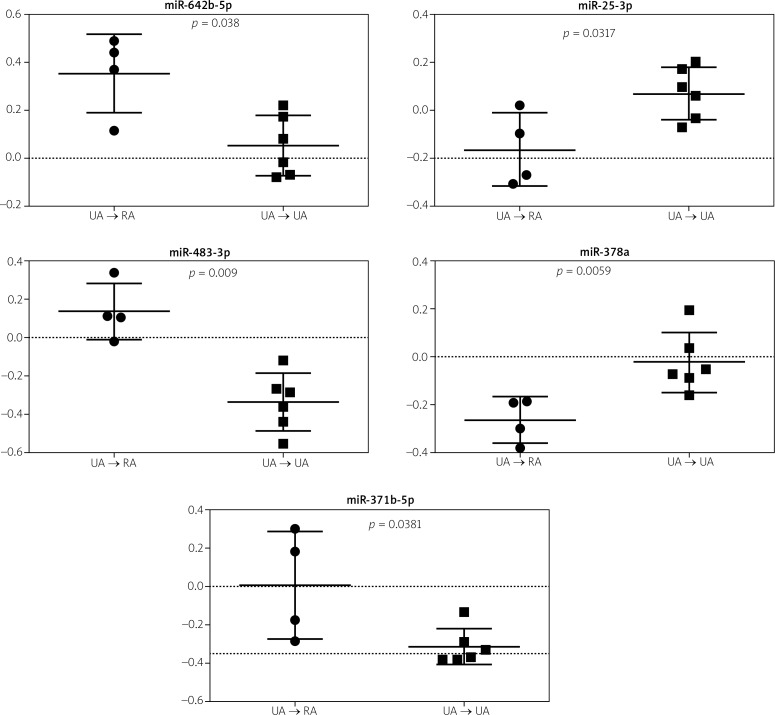
From these 50 miRNAs we selected several specific miRNA candidates based on of significantly changed expression in monocytes of UA → RA vs. UA → UA patients. Predicted specific miRNAs in monocytes of UA → RA patients are: miR-642b-5p (up-regulated, p = 0.0380), miR-483-3p (up-regulated, p = 0.009), miR-371b-5p (up-regulated, p = 0.0381), miR-25-3p (down-regulated, p = 0.0317), and miR-378d (down-regulated, p = 0.0059) (Fig. 2).
Fig. 2.
Expression of miRNA candidates in monocytes of UA → RA vs. UA → UA patients. Differences between patients groups were calculated using two tailed Mann Whitney U test. P-values less than 0.05 were considered significant. Data are presented as median values ± SD.
Among investigated peripheral blood cytokines IL-15 and M-CSF were significantly increased at baseline in patients with UA who progressed to RA, in comparison to patients who remained at UA stage. The concentrations of other investigated cytokines were at comparable levels in both patients groups (Table I).
Table I.
Baseline concentrations of cytokines in peripheral blood of UA → RA and UA → UA patients. Statistical significance between UA → RA and UA → UA patients groups is shown
| Patient group | Patient No. | IL-15 [pg/ml] | M-CSF [pg/ml] | CCL3 [pg/ml] | CCL2 [pg/ml] | IL-6 [pg/ml] | TNF-α [pg/ml] | CCL11 [pg/ml] |
| UA → RA | 1 | 5606.7 | 0.0 | 32.0 | 0.0 | 0.0 | 0.0 | 34.9 |
| 2 | 5.0 | 20.7 | 40.6 | 67.5 | 0.0 | 0.0 | 99.0 | |
| 3 | 587.4 | 383.4 | 115.3 | 0 | 0.0 | 0.0 | 31.3 | |
| 4 | 332.2 | 497.0 | 346.3 | 214.7 | 45.6 | 0.0 | 254.2 | |
| Median | 459.8 | 202 | 77.9 | 33.8 | 0.0 | 0.0 | 66.9 | |
| UA → UA | 5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 50.8 |
| 6 | 0.0 | 0.0 | 0.0 | 211.2 | 0.0 | 0.0 | 99.9 | |
| 7 | 0.0 | 0.0 | 45.5 | 0.0 | 0.0 | 0.0 | 109.2 | |
| 8 | 0.0 | 0.0 | 0.0 | 26.0 | 0.0 | 0.0 | 40.8 | |
| 9 | 0.0 | 0.0 | 19.0 | 0.0 | 0.0 | 0.0 | 162.9 | |
| 10 | 0.0 | 0.0 | 122.6 | 144.1 | 0.0 | 0.0 | 46.4 | |
| Median | 0.0 | 0.0 | 9.5 | 13 | 0.0 | 0.0 | 75.4 | |
| Statistical significance | p = 0.003 | p = 0.033 | NS | NS | NS | NS | NS |
NS − not significant
Discussion
The enhanced/disturbed activities of immune system cells are of crucial importance for the pathophysiology of RA. Functional activities of those cells may be identified and detected by changes of specific measurable parameters. The comprehensive analysis of those parameters, especially in early phases of RA development, could help fast, sensitive and specific identification of individuals with UA who will fulfil the criteria of RA in the future.
The essential role of monocytes in RA development is well documented. Therefore, we hypothesised that changes of molecular pathways regulation in monocytes (reflected by changes of specific miRNAs expression) early in the course of RA development could be useful biological marker indicating disease progression. However, the pattern of miRNAs expression in early phases of RA (i.e. UA phase) was not characterized to date. In addition, studies regarding putative miRNA signature in RA are limited by range of miRNAs investigated. To address this issue we investigated the profile of total human miRNAs (registered in miRBASE 18) expression in monocytes isolated from peripheral blood of UA patients by applying miRNA array technology. Simultaneously with analysis of miRNA expression, we investigated the concentrations of circulating cytokines related to monocyte activity in paired peripheral blood samples from patients being at UA stage. After follow-up period of 4 years and clinical re-evaluation we identified individuals who progressed from UA to classified RA and individuals who remained at UA stage (Fig. 1). Then, we performed analysis of selected biological parameters to estimate their value as potential biomarkers for RA development. Although the number of individuals in our preliminary study in both groups of patients was relatively low, we were able to select several specific miRNA candidates on the basis of significantly changed expression in monocytes (Fig. 1).
The miRNAs showing the highest expression variation between UA → RA vs. UA → UA patients were as follows: miR-483-3p, miR-378d, miR-371b-5p, miR-642b-5p, and miR-25-3p (Fig. 2). There is little knowledge concerning the biological functions and target genes of these selected miRNAs. Current evidences indicate however involvement at least some of these miRNAs in inflammatory and autoimmune human conditions [19−22]. We found also that specific pattern of selected miRNAs expression in circulating monocytes paralleled several monocyte-related cytokines concentration disturbances in sera of UA → RA vs. UA → UA patients. We noticed increased concentrations of IL-15 and M-CSF in UA patients who progressed to RA (Table I). The essential source of IL-15 are activated monocytes [23]. Interleukin 15 is known to participate in the pathogenesis of RA and can be detected in serum and synovial fluid of inflamed joints in patients with RA but not in patients with osteoarthritis or other inflammatory joint diseases [24].
Relevant functions of this cytokine in established RA covers promotion of TNF-α production, activation of T lymphocytes as well as stimulation of osteoclastogenesis [25]. It was documented that genetic variants in IL-15 associate with progression of joint destruction in RA [26], and neutralization of IL-15 improves arthritis in animal models and patients with RA [27]. Furthermore, the levels of IL-15 has been recently shown to be elevated in patients with early RA, and the concentration of this cytokine was shown to predict severe disease course in patients with early arthritis [28]. Other studies also pointed out that IL-15 is elevated in pre-RA patients [29]. However, the observed by us increased concentrations of circulating M-CSF had not been previously reported in early phases of RA. Elevated concentrations of this monocytes grow factor may result from the increased turnover of monocytes in RA bone marrow tissue, as we reported recently [30]. It is worthy to note herein that bone marrow changes can be detected very early in the course of RA development, and had also been found in UA patients [31].
Interestingly, simultaneous presence of bone marrow edema and ACPA Ab raised the prediction value of developing RA at 1 year up to 100 % in patients with UA [32]. Thus, the elevated concentrations of M-CSF in UA → RA patients may reflect the ongoing pathological processes in bone marrow compartment. Interestingly, concentrations of CCL11, which is not mainly considered as monocyte-associated factor were comparable between UA → RA and UA → UA patients. In our study we could not confirm, reported by others, elevated concentrations of TNF-α, IL-6, MIP-1α nor MCP-1 at pre-clinical stage of RA in comparison to healthy subjects [29]. This discrepancy between our and others findings may be related to application by us different method for detection of single protein and solid phase immobilization instead of multiplexing of freely mobile analyte-reactant in sera [33], sensitivity of our ELISA tests, as well as different disease state of investigated patients. We noted that the increased concentrations of IL-15 and M-CSF in peripheral blood of UA patients are especially prominent in 2 patients with high ACPA Ab levels (patient no 3 and 4).It points out the role for these up-regulated cytokines as relevant biomarkers in improving diagnosis and treatment of patients in early phase of RA development. In order to assess if selected by us biological variables bring new or additive value to the known RA predictive biomarkers like ACPA, the more extensive studies involving larger cohort of UA patients as well as the qPCR and function analyses of miRNA candidates are needed.
It is worthy to note that despite even much aggressive and more frequent treatment of patients from UA→RA group during the follow-up period, these patients had been progressed to full-blown RA, however. This suggests that identified by us variables may help to identify patients requiring more aggressive treatment strategy to impede the progression of disease.
Taken together, results of our pilot study indicate that altered activity of monocytes can be detected at early stages of RA development. Furthermore, measurement of selected specific monocyte-related parameters such as miRNA expression and cytokines concentrations may bring additive value useful to improve diagnostic and prognostic classification of RA.
Conclusions
Our results indicate new miRNA candidates (miR-642b-5p, miR-483-3p, miR-371b-5p, miR-25-3p and miR-378d) differentially expressed in peripheral blood monocytes and elevated concentrations of monocyte-related factors (IL-15 and M-CSF) in patients with UA who subsequently developed RA, in comparison to patients with UA who did not progress to RA after 4 years follow-up.
This work was supported by the Polish National Science Centre (grant no. 2012/06/A/NZ5/00059) and the Polish Ministry of Science and Higher Education (core grant S/17).
The authors declare no conflict of interest.
References
- 1.Macfarlane LA, Murphy PR. MicroRNA: Biogenesis, Function and Role in Cancer. Curr Genomics. 2010;11:537–561. doi: 10.2174/138920210793175895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghosh S, Hayden MS. New regulators of NF-kappaB in inflammation. Nat Rev Immunol. 2008;8:837–848. doi: 10.1038/nri2423. [DOI] [PubMed] [Google Scholar]
- 4.Wang J, Chen J, Sen S. MicroRNA as Biomarkers and Diagnostics. J Cell Physiol. 2016;231:25–30. doi: 10.1002/jcp.25056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salehi E, Eftekhari R, Oraei M, et al. MicroRNAs in rheumatoid arthritis. Clin Rheumatol. 2015;34:615–628. doi: 10.1007/s10067-015-2898-x. [DOI] [PubMed] [Google Scholar]
- 6.Akhtar N, Singh AK, Ahmed S. MicroRNA-17 Suppresses TNF-α signaling by interfering with TRAF2 and cIAP2 association in rheumatoid arthritis synovial fibroblasts. J Immunol. 2016;197:2219–2228. doi: 10.4049/jimmunol.1600360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi DL, Shi GR, Xie J, et al. MicroRNA-27a Inhibits Cell Migration and Invasion of Fibroblast-Like Synoviocytes by Targeting Follistatin-Like Protein 1 in Rheumatoid Arthritis. Mol Cells. 2016;39:611–618. doi: 10.14348/molcells.2016.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long L, Yu P, Liu Y, et al. Upregulated microRNA-155 expression in peripheral blood mononuclear cells and fibroblast-like synoviocytes in rheumatoid arthritis. Clin Dev Immunol. 2013;2013:ID 296139. doi: 10.1155/2013/296139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pauley KM, Satoh M, Chan AL, et al. Upregulated miR-146a expression in peripheral blood mononuclear cells from rheumatoid arthritis patients. Arthritis Res Ther. 2008;10:R101. doi: 10.1186/ar2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sebastiani GD, Fulci V, Niccolini S, et al. Over-expression of miR-223 in T-lymphocytes of early rheumatoid arthritis patients. Clin Exp Rheumatol. 2011;29:1058–1059. [PubMed] [Google Scholar]
- 11.Alivernini S, Kurowska-Stolarska M, Tolusso B, et al. MicroRNA-155 influences B-cell function through PU.1 in rheumatoid arthritis. Nat Commun. 2016;7:12970. doi: 10.1038/ncomms12970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurowska-Stolarska M, Alivernini S, Ballantine LE, et al. Micro-RNA-155 as a proinflammatory regulator in clinical and experimental arthritis. Proc Natl Acad Sci U S A. 2011;108:11193–11198. doi: 10.1073/pnas.1019536108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajasekhar M, Olsson AM, Steel KJ, et al. MicroRNA-155 contributes to enhanced resistance to apoptosis in monocytes from patients with rheumatoid arthritis. J Autoimmun. 2017;79:53–62. doi: 10.1016/j.jaut.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elmesmari A, Fraser AR, Wood C, Gilchrist D, et al. MicroRNA-155 regulates monocyte chemokine and chemokine receptor expression in Rheumatoid Arthritis. Rheumatology (Oxford) 2016;55:2056–2065. doi: 10.1093/rheumatology/kew272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davignon JL, Hayder M, Baron M, et al. Targeting monocytes/macrophages in the treatment of rheumatoid arthritis. Rheumatology (Oxford) 2013;52:590–598. doi: 10.1093/rheumatology/kes304. [DOI] [PubMed] [Google Scholar]
- 16.Bresnihan B, Gerlag DM, Rooney T, et al. Synovial macrophages as a biomarker of response to therapeutic intervention in rheumatoid arthritis: standardization and consistency across centers. J Rheumatol. 2007;34:620–622. [PubMed] [Google Scholar]
- 17.Lioté F, Boval-Boizard B, Weill D, et al. Blood monocyte activation in rheumatoid arthritis: increased monocyte adhesiveness, integrin expression, and cytokine release. Clin Exp Immunol. 1996;106:13–19. doi: 10.1046/j.1365-2249.1996.d01-820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coulthard LR, Geiler J, Mathews R, et al. Differential effects of infliximab on absolute circulating blood leucocyte counts of innate immune cells in early and late rheumatoid arthritis patients. J Clin Exp Immunol. 2012;170:36–46. doi: 10.1111/j.1365-2249.2012.04626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pacurari M, Tchounwou PB. Role of MicroRNAs in renin-angiotensin-aldosterone system-mediated cardiovascular inflammation and remodeling. Int J Inflam. 2015;2015:101527.. doi: 10.1155/2015/101527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valmiki S, Ahuja V, Paul J, et al. MicroRNA exhibit altered expression in the inflamed colonic mucosa of ulcerative colitis patients. World J Gastroenterol. 2017;23:5324–5332. doi: 10.3748/wjg.v23.i29.5324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lv Z, Shi Q, Huang W at al. MicroRNA expression profiling in Guillain-Barré syndrome. J Neuroimmunol. 2016;301:12–15. doi: 10.1016/j.jneuroim.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Liguori M, Nuzziello N, Licciulli F, et al. Combined microRNAs and mRNAs expression analysis in Pediatric Multiple Sclerosis: an integrated approach to uncover novel pathogenic mechanisms of the disease. Hum Mol Genet. 2017;27:66–79. doi: 10.1093/hmg/ddx385. [DOI] [PubMed] [Google Scholar]
- 23.Grabstein KH, Eisenman J, Shanebeck K, et al. Cloning of a T cell growth factor that interacts with the beta chain of the interleukin-2 receptor. Science. 1994;264:965–968. doi: 10.1126/science.8178155. [DOI] [PubMed] [Google Scholar]
- 24.Ortiz AM, Laffon A, Gonzalez-Alvaro I. CD69 expression on lymphocytes and interleukin-15 levels in synovial fluids from different inflammatory arthropathies. Rheumatol Int. 2002;21:182–188. doi: 10.1007/s00296-001-0161-z. [DOI] [PubMed] [Google Scholar]
- 25.Ogata Y, Kukita A, Kukita T, et al. A novel role of IL-15 in the development of osteoclasts: inability to replace its activity with IL-2. J Immunol. 1999;162:2754–2760. [PubMed] [Google Scholar]
- 26.Knevel R, Krabben A, Brouwer E, et al. Genetic variants in IL15 associate with progression of joint destruction in rheumatoid arthritis: a multicohort study. Ann Rheum Dis. 2012;71:1651–1657. doi: 10.1136/annrheumdis-2011-200724. [DOI] [PubMed] [Google Scholar]
- 27.Xiao-Ke Yang, Wang-Dong Xu, Rui-Xue Leng, et al. Therapeutic potential of IL-15 in rheumatoid arthritis. Human Immunology. 2015;76:812–818. doi: 10.1016/j.humimm.2015.09.041. [DOI] [PubMed] [Google Scholar]
- 28.González-Álvaro I, Ortiz AM, Alvaro-Gracia JM, et al. Interleukin 15 levels in serum may predict a severe disease course in patients with early arthritis. PLoS One. 2011;6:e29492. doi: 10.1371/journal.pone.0029492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deane KD, O’Donnell CI, Hueber W, et al. The number of elevated cytokines and chemokines in preclinical seropositive rheumatoid arthritis predicts time to diagnosis in an age-dependent manner. Arthritis Rheum. 2010;62:3161–3172. doi: 10.1002/art.27638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smiljanovic B, Radzikowska A, Kuca-Warnawin E, et al. Increased turnover of monocytes in patients with rheumatoid arthritis identified by transcriptome and cytometric prifiling. Ann Rheu Dis. 2017;76:A1–A55. [Google Scholar]
- 31.McQueen FM. Bone marrow edema and osteitis in rheumatoid arthritis: the imaging perspective. Arthritis Res Ther. 2012;14:224. doi: 10.1186/ar4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tamai M, Kawakami A, Uetani M, et al. A prediction rule for disease outcome in patients with undifferentiated arthritis using magnetic resonance imaging of the wrists and finger joints and serologic autoantibodies. Arthritis Rheum. 2009;61:772–778. doi: 10.1002/art.24711. [DOI] [PubMed] [Google Scholar]
- 33.Leng SX, McElhaney JE, Walston JD, et al. ELISA and multiplex technologies for cytokine measurement in inflammation and aging research. J Gerontol A Biol Sci Med Sci. 2008;63:879–884. doi: 10.1093/gerona/63.8.879. [DOI] [PMC free article] [PubMed] [Google Scholar]