Abstract
Purpose
Exsanguination is the most common leading cause of death in trauma patients. The massive transfusion (MT) protocol may influence therapeutic strategies and help provide blood components in timely manner. The assessment of blood consumption (ABC) score is a popular MT protocol but has low predictability. The lactate level is a good parameter to reflect poor tissue perfusion or shock states that can guide the management. This study aimed to modify the ABC scoring system by adding the lactate level for better prediction of MT.
Methods
The data were retrospectively collected from 165 trauma patients following the trauma activated criteria at Songklanagarind Hospital from January 2014 to December 2014. The ABC scoring system was applied in all patients. The patients who had an ABC score ≥2 as the cut point for MT were defined as the ABC group. All patients who had a score ≥2 with a lactate level >4 mmol/dL were defined as the ABC plus lactate level (ABC + L) group. The prediction for the requirement of massive blood transfusion was compared between the ABC and ABC + L groups. The ability of ABC and ABC + L groups to predict MT was estimated by the area under the receiver operating characteristic curve (AUROC).
Results
Among 165 patients, 15 patients (9%) required massive blood transfusion. There were no significant differences in age, gender, mechanism of injury or initial vital signs between the MT group and the non-MT group. The group that required MT had a higher Injury Severity Score and mortality. The sensitivity and specificity of the ABC scoring system in our institution were low (81%, 34%, AUC 0.573). The sensitivity and specificity were significantly better in the ABC + L group (92%, 42%, AUC = 0.745).
Conclusion
The ABC scoring system plus lactate increased the sensitivity and specificity compared with the ABC scoring system alone.
Keywords: Assessment of blood consumption scoring system, Blood lactate level, Massive transfusion
Introduction
Exsanguination is the most common leading cause of death in trauma patients.1 Exsanguination represents 50% of deaths from acute blood loss in the first 24 h and half of the patients will have severe coagulopathy.2, 3, 4, 5 Patients who had massive hemorrhage need control of bleeding and resuscitation with massive transfusions (MT).6, 7 The MT protocol may influence therapeutic strategies and help to provide blood components in a timely manner.8, 9 The 3%–5% of all civilian and 10% of all military trauma patients need MT.10 Damage control resuscitation is the main strategy to maintain and resuscitate these patients to decrease morbidity and mortality.11 The MT protocol is an important part of damage control resuscitations.11
Presently, we have many scoring systems to predict the patients who need MT.6, 12 The ideal scoring system must have many properties that include ease of use, fast and good efficacy.13 The assessment of blood consumption (ABC) score is a popular MT protocol which has high sensitivity, specificity, and accuracy to predict blood transfusion.6 But some studies found that it had low predictability.14 Besides the ABC score, we have other scores such as Trauma-Associated Severe Hemorrhage (TASH) or Mc Laughlin Score.12, 15 However, there is no consensus on the best scoring system to predict massive blood transfusion requirement.
The hemorrhage shock patient will have poor tissue perfusion according to the definition of shock.16 From previous literature, the blood lactate level is a good parameter to reflect poor tissue perfusion or shock state that can guide the management. Furthermore, the arterial blood lactate level is easy and quick to interpret and can help to immediately guide the management at the emergency room.10 In the sepsis or septic shock patients, if the blood lactate level is less than 2.5 mmol/L, it demonstrates that a patient has good resuscitation and recovery from the shock state.17 The Broder and Weil study found that a blood lactate level more than 4 mmol/L was related to poor outcomes.18
This study aimed to validate the ABC scoring system in our center and compare combining blood lactate level to the ABC scoring system and the ABC scoring system alone.
Methods
The data of trauma patients who met the trauma team activated criteria (TTAC) from January 2014 to December 2014 were retrospectively collected from a prospectively collected trauma registry. The TTAC consisted of gunshot wound at chest or abdomen, stab wound at chest or abdomen, heart arrest, systolic blood pressure <90 mmHg, respiratory rate <12 or >30/min, pulse rate >120/min (post resuscitation 2 L), Glasgow Coma Scale score ≤8, evidence of pelvic fracture or long bone fracture with SBP <90 mmHg or Focus Assessment of Sonography in Trauma (FAST) positive. The exclusion criteria were younger than 18 years, pregnancy and no data of FAST. The ethics committee of the Prince of Songkla University approved the protocol.
The definition of MT is transfusion of pack red cells of more than 10 units or 3500 mL in first 24 h or an estimated blood loss of more than 4900 mL or 1 blood volume.
The ABC scoring system has 4 dichotomous components which contribute one point to the total score for a range of scores from zero to four. The parameters include penetrating mechanism (0 no, 1 yes), ED SBP (emergency department systolic blood pressure) of 90 mmHg or less (0 no, 1 yes), ED HR (emergency department heart rate) of 120/min or greater (0 no, 1 yes), and positive FAST (0 no, 1 yes).
The patients who had an ABC score ≥2 as the cut point for MTP were defined as the ABC group. All patients who had a score ≥2 with a lactate level (L) > 4 mmol/dL were defined as the ABC + L group. The predictions for the requirement of massive blood transfusion were compared between the ABC and ABC + L groups.
Statistical considerations
Categorical data were compared using Fisher's exact test. Normally distributed data were compared using analysis of variance. Logistic regression was used to measure the relationship between dependent variables and one or more independents variables with a Mann-Whitney U test or Kruskal-Wallis test. Sensitivity, specificity and diagnostic accuracy at the optimal cut-off threshold scores of ABC and ABC + L groups to predict MT was estimated by the area under the receiver operating characteristic curve (AUROC), in which true-positive rates are plotted against the false-positive rates (i.e., sensitivity against 1 – specificity).
Results
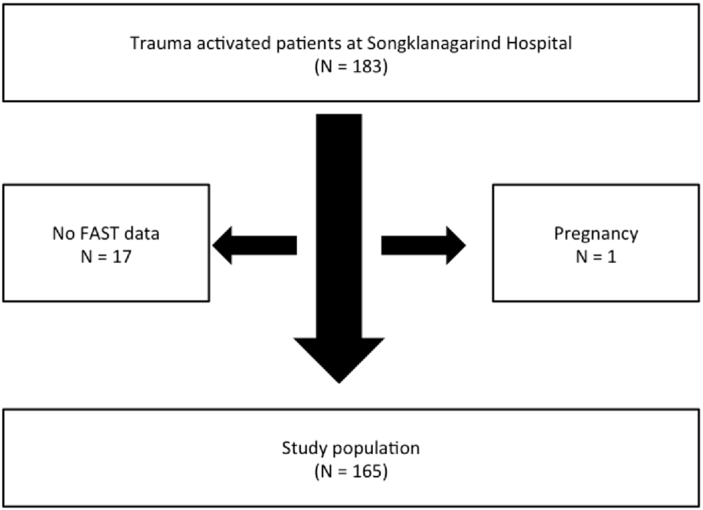
From January to December 2014, 183 patients met the TTAC. Eighteen patients were excluded because 17 patients did not have FAST data and one patient was pregnant (Fig. 1); therefore, 165 patients remained in this study.
Fig. 1.
Flow of patients.
Among 165 patients, 15 patients (9%) required massive blood transfusion. The median age was 35 years old and the majority of the patients were male. A minority of patients had penetrating injuries. There were no significant differences in the initial vital signs between the MT group and the non-MT group. The medians of the injury severity score and lactate level were significantly high in the MT group. The emergency operation requirement, mortality and ICU stay in the MT group were significantly more than the non-MT group. The demographic data are shown in Table 1.
Table 1.
Demographic data divided into MT and non-MT groups (n = 165).
| Variables | MT (n = 15) | Non-MT (n = 150) | p value |
|---|---|---|---|
| Age (year, IQR) | 35 (22, 44.5) | 35 (25, 43) | 0.814 |
| Male (n, %) | 13 (86.7) | 119 (79.3) | 0.738 |
| Penetrating mechanism (n, %) | 3 (20) | 40 (26.7) | 0.761 |
| ED SBP (mmHg, IQR) | 120 (84, 124.5) | 128 (102, 145.8) | 0.110 |
| ED DBP (mmHg, IQR) | 64 (47.5, 72) | 68.5 (54, 78) | 0.309 |
| ED HR (/min, IQR) | 116 (98, 125) | 109 (86.2, 128) | 0.622 |
| ED RR (/min, IQR) | 20 (14, 30) | 24 (18.5, 28) | 0.982 |
| ED SpO2 (%,IQR) | 98 (94, 100) | 98 (95, 100) | 0.822 |
| Positive FAST (n, %) | 6 (40) | 13 (8.7) | 0.003 |
| Injury severity score (IQR) | 38 (29, 40.5) | 17 (9,28.5) | <0.001 |
| Base excess (IQR) | −6.7 (−10.1, −5.8) | −6.1 (−6.9, −5) | 0.088 |
| Lactate (mmol/dL, IQR) | 8.7 (5.1, 11.3) | 3.8 (1.9, 5.4) | 0.006 |
| Emergency operation (n, %) | 15 (100) | 64 (42.7) | <0.001 |
| Amount of blood transfusion (mL, IQR) | 5460 (3966, 6223.5) | 0 (0, 768.5) | <0.001 |
| Mortality in hospital (n, %) | 12 (80) | 22 (14.7) | <0.001 |
| ICU stay (day, IQR) | 3 (1, 5.5) | 0 (0, 1) | <0.001 |
All data are presented as median (IQR) unless indicated otherwise.
Abbreviations: IQR, inter quartile range, median; MT, massive transfusion; Non-MT, non-massive transfusion; ED, Emergency Department; SBP, systolic blood pressure; DBP, diastolic blood pressure; FAST, focused assessment with sonography for trauma; ICU, Intensive Care Unit.
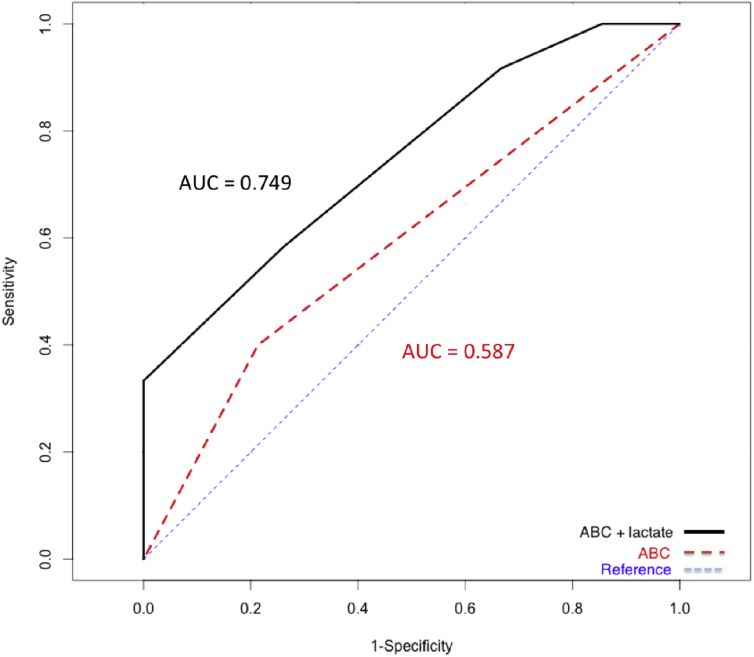
The sensitivity, specificity, and accuracy of the ABC scoring system in our center were 23%, 60%, and 0.587 respectively. The accuracy of ABC + L was 0.749. The accuracy of the ABC scoring system with blood lactate level and ABC scoring system alone is shown in Fig. 2.
Fig. 2.
The area under the curve (AUC) between ABC scoring system with blood lactate level and ABC scoring system alone (N = 165).
Discussion
Hemorrhage is a major factor that determines fate after severe multiple traumas.1 Early and effective therapeutic intervention may reduce mortality and improve outcome.9, 14 In several trauma centers, they usually use the ABC score for early predict massive blood transfusion because of its ease of use and calculation and it has good validity.6 The advantage of ABC scoring system lies in the parameters from history taking, physical examination, and FAST.6 But this study found that the ABC scoring system had low sensitivity (23%) and accuracy (AUC = 0.59) to predict massive transfusion in our center. It means that ABC scoring system is not the best one to predict massive blood transfusion even though it is a good predictor in some trauma centers.6 Many reasons can explain the low sensitivity and accuracy to predict massive blood transfusion in our center. Firstly, most subjects in this study population were younger patients who were able to maintain normal vital signs even though they had ongoing hemorrhage. Secondly, blunt injury was the majority presentation in this study which is a parameter in the ABC scoring system that impacts the interpretation.
We would like to find a parameter to increase sensitivity, specificity, and accuracy to predict massive blood transfusion. The arterial blood lactate level is a parameter that is a sentinel marker of widespread inadequate tissue perfusion and reflects resuscitation adequacy quite well.17, 18 The arterial blood lactate level can be performed easily and is usually done quickly at the emergency room and can be used to predict massive blood transfusion.17 From our study, combining the blood lactate level to the ABC scoring system improved the prediction accuracy of MT requirement (AUC = 0.75) and the accuracy to predict massive blood transfusion was greater than the ABC scoring system alone. Combining the blood lactate level to the ABC scoring system is neither difficult nor complicated. In any case, the blood lactate level is the initial parameter to indicate tissue perfusion which we add to the ABC scoring system in our center to improve the accuracy to predict massive blood transfusion. Although the arterial blood lactate level is a laboratory parameter, it is not a waste of time to perform and interpret the results for emergency situations.
There are some limitations of this study. This study is a single population at a single center and had a small sample size. We plan to collect the data prospectively and increase the study population to show the benefit of this scoring system. If the new scoring system to predict massive blood transfusion has good sensitivity, specificity, and accuracy, multicenter studies should be performed to validate this scoring system.
In conclusion, this study found that combining blood lactate level to the ABC scoring system is a more accurate predictor of MT requirement than the ABC scoring system alone.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.McLeod J.B., Lynn M., Mckenney M.G. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55:39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- 2.Sauaia A., Moore F.A. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–193. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kauvar D.S., Lefering R., Wade C.E. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006;60:S3–S11. doi: 10.1097/01.ta.0000199961.02677.19. [DOI] [PubMed] [Google Scholar]
- 4.Cap A., Hunt B. Acute traumatic coagulopathy. Curr Opin Crit Care. 2014;20:638–645. doi: 10.1097/MCC.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 5.Martinowitz U.M.M. Guidelines for the use of recombinant activated factor VII (rFVIIa) in uncontrolled bleeding: a report by the Israeli Multidisciplinary rVIIa task force. J Thromb Haemost. 2005;3:640–648. doi: 10.1111/j.1538-7836.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- 6.Nunez T.C., Voskresensky I.V., Dossett L.A. Early prediction of massive transfusion in trauma: simple as ABC (assessment of blood consumption)? J Trauma. 2009;66:346–352. doi: 10.1097/TA.0b013e3181961c35. [DOI] [PubMed] [Google Scholar]
- 7.Como J.J., Dutton R.P., Scalea T.M. Blood transfusion rates in the care of acute trauma. Transfusion. 2004;44:809–813. doi: 10.1111/j.1537-2995.2004.03409.x. [DOI] [PubMed] [Google Scholar]
- 8.Cotton B.A., Gunter O.L., Isbell J. Damage control hematology: the impact of a trauma exsanguination protocol on survival and blood product utilization. J Trauma. 2008;64:1177–1182. doi: 10.1097/TA.0b013e31816c5c80. [DOI] [PubMed] [Google Scholar]
- 9.Chidester S.J., Williams N., Wang W. A pediatric massive transfusion protocol. J Trauma Acute Care Surg. 2012;73:1273–1277. doi: 10.1097/TA.0b013e318265d267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holcomb J.B., Jenkins D., Rhee P. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–310. doi: 10.1097/TA.0b013e3180324124. [DOI] [PubMed] [Google Scholar]
- 11.Akaraborworn O. Damage control resuscitation for massive hemorrhage. Chin J Traumatol. 2014;17(2):108–111. [PubMed] [Google Scholar]
- 12.Yücel N., Lefering R., Maegele M. Trauma Associated Severe Hemorrhage (TASH)-Score: probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. J Trauma. 2006;60:1228–1236. doi: 10.1097/01.ta.0000220386.84012.bf. [DOI] [PubMed] [Google Scholar]
- 13.Malone D.L., Hess J.R., Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006;60(6 Suppl):S91–S96. doi: 10.1097/01.ta.0000199549.80731.e6. [DOI] [PubMed] [Google Scholar]
- 14.Dutton R.P., Lefering R., Lynn M. Database predictors of transfusion and mortality. J Trauma. 2006;60:S70–S77. doi: 10.1097/01.ta.0000200856.47545.64. [DOI] [PubMed] [Google Scholar]
- 15.McLaughlin D.F., Niles S.E., Salinas J. A predictive model for massive transfusion in combat casualty patients. J Trauma. 2008;64(2 Suppl):57–63. doi: 10.1097/TA.0b013e318160a566. [DOI] [PubMed] [Google Scholar]
- 16.Kenneth L., Mattox E.E.M., Feliciano David V. 7th, editor. McGraw-Hill Companies; United States: 2013. Trauma; pp. 18–28. [Google Scholar]
- 17.Shapiro N.I., Howell M.D., Talmor D. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005;45:524–528. doi: 10.1016/j.annemergmed.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Broder G.W.M., WEIL M.H. Excess lactate: an index of reversibility of shock in human patients. Science. 1964;143:1457–1459. doi: 10.1126/science.143.3613.1457. [DOI] [PubMed] [Google Scholar]