Abstract
As well for optimized emergency management in individual cases as for optimized mass medicine in disaster management, the principle of the medical doctors approaching the patient directly and timely, even close to the site of the incident, is a long-standing marker for quality of care and patient survival in Germany. Professional rescue and emergency forces, including medical services, are the “Golden Standard” of emergency management systems. Regulative laws, proper organization of resources, equipment, training and adequate delivery of medical measures are key factors in systematic approaches to manage emergencies and disasters alike and thus save lives. During disasters command, communication, coordination and cooperation are essential to cope with extreme situations, even more so in a globalized world. In this article, we describe the major historical milestones, the current state of the German system in emergency and disaster management and its integration into the broader European approach.
Keywords: Emergency medical systems, Disaster medicine, Public health, Germany
History of the German emergency and disaster management system
Milestones
The four most important milestones in the developement of the modern day german emergency medical system are:
The Kirschner principle in emergency medicine
The groundbreaking publication and speech of the famous professor for surgery Manfred Kirschner (University of Tübingen and Heidelberg), at the German Annual National Congress of Surgery in 1938,1 offered a completely new perspective of the role of medical doctors in emergency medicine. He recommended the following:
“The ideal of emergency medicine is that a medical doctor approaches the patient at the site of accident and not the patient to approach a medical doctor for the first time after an accident in the hospital” – in other words the doctor has to come to the patient, as early as possible.
The rescue chain by Ahnefeld
The development of the “rescue chain” (Die Rettungskette) by the more than well-known professor for anesthesiology Friedrich Wilhelm Ahnefeld in 1970,2 which was later adopted by the Americans to the so called “chain of survival”, describes each organizational centerpiece of treatment and transport from the site of the accident to the site of definite care in the hospital (Fig. 1). Using Ahnefeld's theorem allows scientists to analyze, understand and improve each single but intermingled aspect of providing emergency assistance.
Fig. 1.
Modern depiction of the original rescue chain by Ahnefeld in German, taken from the Ministry of the Interior of Rhineland-Westphalia. Translation from left to right: secure your own and others safety, life-saving immediate measures, emergency call, first aid, rescue services, hospital admission.
Importance of the response time within the golden hour
The response time - a crucial part of the golden hour, which by itself is an internationally recognized key factor for survival in emergencies3 is one of the most important quality standards in modern emergency medical systems. It describes the time for an emergency assistance team to arrive at the site of incident once the alarm was activated. Only if time management is optimized from the get-go, the golden hour can be respected as what it is: lifesaving. Minutes lost at the beginning are almost impossible to make up while the mission progresses further and more and more variables come into play (Fig. 2).
Fig. 2.
Depiction of crucial times within the rescue chain (Hecker, Domres 2017).
As a method of quality assurance and according to the German National Rescue Law this quality indicator is regularly and obligatory monitored nation-wide and if failed in fixed arranged percentages has severe consequences for providers on a legal basis.
Whole-area provisioning of air-rescue
Especially in high-density urban space and in extreme rural areas the management of the golden hour is severely hampered by existing infrastructure limitations (e.g. traffic jams, road conditions, distances between site of accident and hospital). In Germany, the potential of helicopters to fill these time management gaps has been exploited early on.
Since 1973 helicopter air-rescue is covering all parts of Germany. It was in fact the first time that a nation provided a complete air-based rescue system, in which each helicopter station covers an operative radius of 50 km (Fig. 3).
Fig. 3.
Helicopter bases throughout Germany by the various accredited providers (source ADAC Germany).
History of the German emergency management system
Emergency and disaster medicine are closely related to military medicine. For example, the potentially most important tool of organizing mass casualty incidents, the so called “triage”, was first described by the Russian war surgeon Pirogov in 1864: “In comparison a well-functioning organization of disaster management may save more lives than the knife of the surgeon”.3
Germany's violent military history in the years 1933–1945 however proved to be a major obstacle for the development of modern approaches to emergency and disaster management in the years after World War II.
However, only three decades later by 1973 Germany was the first country to establish a nation-wide air-rescue-system. Looking back a tremendous achievement, that to current day Germans seems like a “natural civil right”.
And in fact, it actually is:
In Germany, the situation after World-War II leads to a complete restructuring of the civil defense approach. In the center of its strategical reorganization is the legal right to live a bodily unharmed life, which is manifested in Germany's Constitution (Grundgesetz Artikel. 2, German Constitution 2nd paragraph).
As a result, Germany's regulative laws regarding emergency and disaster management do not only describe and structure Professional emergency and disaster management systems, but also define the duties of German citizens in emergency situations. Every German is not only granted abovementioned civil right but is also bound by law to provide first-aid to fellow citizens or to alarm professional forces. If the law is not complied, legal punishment is mandatory and often severe.
This public awareness of the need to assist each other in states of emergencies is potentially also the foundation of Germany's highly motivated voluntary basis of civil engagement in emergency and disaster management.
While we will describe the organization of professional forces below, the education of the public is a topic of its own. For example, before being allowed to ride a car, every German has to successfully finish a certified first aid training.
Present state of the German emergency management system
To provide optimized individual care, Germany's emergency medical system is operating a vehicle-based ground and air rescue system. The personnel manning these rescue vehicles are emergency physicians and paramedics, and in the case of air rescue also especially trained pilots. Both air and ground forces operate using specialized equipment and educational routines, which are nation-wide standardized.
Rescue transport vehicle–Rettungswagen (RTW)
Paramedics utilize rescue transport vehicles—RTW. These vehicles offer full high-tech equipment according to nation-wide standards. Training of paramedics is also standardized, but legal barriers regarding medical measures applicable by them may vary between states. At least one patient is able to be transported by one RTW. Modern rescue equipment for difficult and dangerous circumstances is also on board and may supplement the equipment of fire-fighting brigades. Also, personal security equipment against infectious diseases is carried on board. Special variants of these vehicles exist in order to transport intensive care patients during inter-hospital-transfers even over long distances or to treat neonates (Fig. 4).
Fig. 4.
Pictures RTW and equipment (Source: German Red Cross).
Emergency physician mission vehicle—Notarzt-Einsatz-Fahrzeug (NEF)
Emergency physicians are especially trained and qualified medical doctors in rescue, emergency and mass medicine. They have principal training of medical and public health leadership roles during disasters. Together with one paramedic an emergency physician mission vehicle (NEF) is manned by these doctors. This vehicle offers almost all medical equipment to be found on RTW but lacks the ability to transport patients and misses parts of the rescue equipment (Fig. 5).
Fig. 5.
Pictures of NEF and equipment (Source: German Red Cross).
The Rendez–Vous-System
The way these vehicles (RTW and NEF) interact is often called “Rendez-Vous-System” (French for: meeting or come together) which allows for optimal usage of the “Kirschner principle” and management & controlling according to “Ahnefeld's theorem”.
The highly mobile NEF allows emergency physicians to provide individual medical assistance as needed and to accompany the patient up to the hospital by joining the RTW crew or co-operate with multiple RTW by meeting up with them and after stabilizing the patient come to the aid of another RTW. In short it is the current “gold standard” of fulfilling the “Kirschner principle” in Germany and allows medical doctors to approach the patient as early as possible and direct the patient's further treatment form the site of the incident into the emergency room and finally suitable definite care.
On the down-side the Rendez-Vous-System is cost intensive and demands for professionals willing to dedicate their career to EMS. A possible acceptable solution to still offer medicine provided by a medical doctor at the site of incident without a doctor physically being there might be offered by using telemedicine.
Both functional units (RTW and NEF) are tactically led by dispatch centers, which are connected with other adjectant EMS dispatch centers and with those of the police and firefighters.
Trauma centers
An important tool for quality assurance in emergency management is the organization of hospitals according to their expertise in trauma management. Germany defines level 1–3 hospitals. While level 1 hospitals (Fig. 6) hold specialized trained staff and equipment ready to treat even the most severely injured on a 24 h 7 days a week schedule, level 3 hospitals are not suited for those patients and only hold limited capabilities.
Fig. 6.
Shock room level 1 trauma center.
To be certified as level 1, hospitals must hold certain capacities for all sorts of surgery (e.g. trauma, abdominal, vascular, burn surgery) and intensive care plus follow set rules regarding their equipment and organization in the so called Schockraum (engl. shock room).
Trauma-network and trauma registry
One of the most important developments in the treatment of poly-traumatized cases however was not achieved by using special medical equipment, but by making use of big data. The German Soc. for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie) started to make digital data available for the treatment of these cases as early as 1993 by establishing the “Trauma-Netzwerk” (English translation: trauma-network) and “trauma-register” which collects data from more than 700 clinics throughout Germany and is regarded as one of the major sources for quality management and research in the field of treating poly-traumatized cases.
Using these sources medical doctors can compare their treatment and the outcome of patients with each other, thus defining treatment standards, shortages and define future research needs. By 2017 about 280,000 cases have been studied, their data stored and are readily available for national and international comparison.
In order to manage the constant flow of data the German Society for Trauma Surgery demands that standardized documentation of cases is done as early as at the scene of incident and to be followed up during emergency room admission, operation theatre, intensive care unit and final release from hospital. In order to sustain the quality of the system itself, clinics have to be certified and re-evaluate their quality control constantly. Certified clinics then form into networks and exchange and evaluate treatment of other centers, thus forming the trauma-network.
Fig. 7. Exemplarily shows the results of modern emergency management in regards to the death-toll in traffic. While in the year 2014, 301,139 (red-dotted line) people got injured in accidents 3,368 of them died in the process (red line, yellow dots). In 1970 about 21,000 people died to comparable accidents. This is a remarkable decline, even more so since there are currently roughly 62.6 million admissioned cars, trucks and motorbikes in Germany and the country is also one of the most frequented transit countries for European Commerce and Transcontinental Traffic. Of course, the high security standards, public awareness for traffic rules and legal coordination also play a major role.
Fig. 7.
Number of accidents (years 2000–2014) with injured people on German roads (red-dotted line) and fatalities because of accidents directly or in the process (red line with yellow dots). Data are expressed as thousand. Source: German National Statistical Agency.
Present state of the disaster management system
Germany has a decentralized emergency management system, meaning that the state delegates EMS authority to its provinces and the provinces delegate EMS authority to their regions, cities and communes. Regional Emergency Medical Systems, as described above, are the primary tool of medical civil defense during disasters.
In order to cope with mass casualties and disasters, these forces must also have basic abilities to assist the populace beyond regular medical aid.
These capabilities vary in extend from city to city, region to region and state to state. Therefore, the legal demand (German Constitution 2nd paragraph, see above) cannot be fulfilled by local forces alone.
So, in cases that overwhelm local authorities, the organizational structure is reverted, meaning that the bigger the incident is, the command structure shifts from region to province to the federal state. In cases of disasters threatening, the country itself the federal government leads its disaster defense by its centralized command center situated in Berlin, the so called “Gemeinsames Lagezentrum des Bundes und der Länder (GMLZ)”.
Unlike the situation in China, the military in Germany only holds a subsidiary role during disasters. This means that disaster management in Germany is primary a civil task. Germany therefore has defined the standard operating procedures for decision making and political and administrative leadership during disasters in flow charts (Fig. 8).
Fig. 8.
Political and Disaster Management Standard Operating Procedures as defined by the German State (Source German Civil Defense Agency, Bundesamt für Bevölkerungschutz und Katastrophenhilfe).
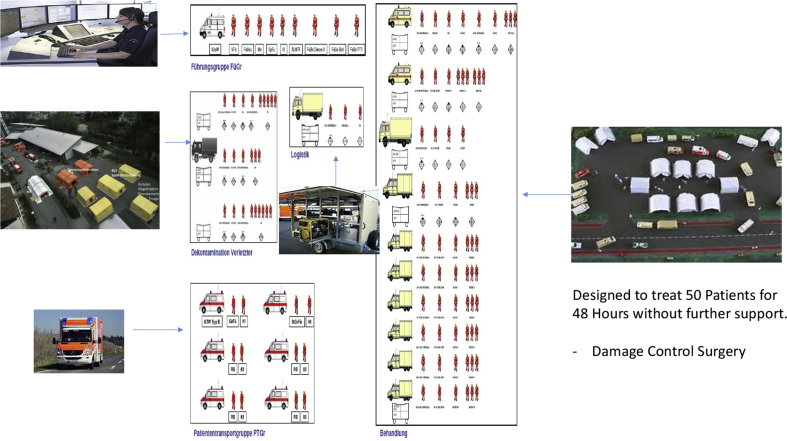
Medical task forces
On the operational level Germany holds special forces to assist regional EMS. These are called medical task forces (MTF). The MTF are functional units that hold components for leadership, treatment, decontamination, transport, logistics and support (Fig. 9, Fig. 10, Fig. 11).
Fig. 9.
Standard operational structure of a MTF (Source: BBK).
Fig. 10.
Standard operational structure of a MTF (2) (Source: BBK).
Fig. 11.
Deployment of MTF across Germany (source: BBK).
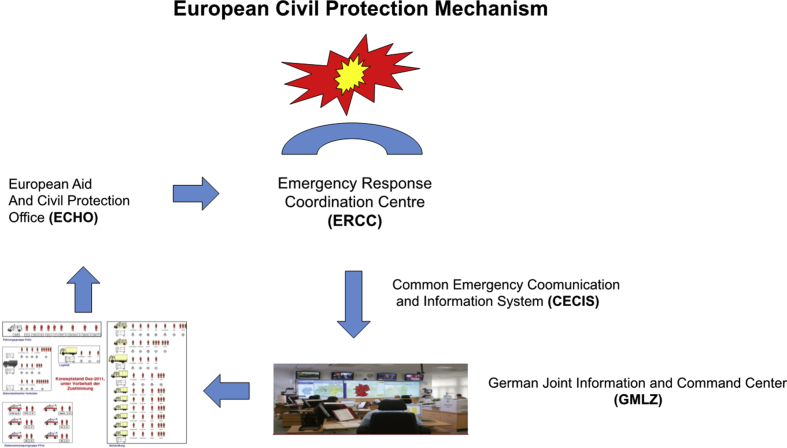
The European civil defense mechanism
The most common definition of a disaster is a long-standing imbalance between need for aid and the ability to provide aid. Therefore, it is only a question of strength of impact before national systems are being overwhelmed. Especially in a globalized world the consequence of one's disaster can easily have a major impact on a global stage. That's why national system should best integrate into international systems. Regarding Germany this means foremost to integrate into a broader European approach, the so called European civil protection mechanism (Fig. 12).
Fig. 12.
European civil protection mechanism.
This mechanism is a routine operational cycle that offers all member states to support other member states by fixed communication and operational structures. For example, Germany's MTF could also be sent to France, or any other member state, to operate under European lead disaster reaction forces. The mechanism is not entirely limited to Europe itself, since the constitution of it also allows for non-member states to appeal for help. As happened during the Ebola crisis in West Africa.
Conclusion
Emergency Medical Systems are an essential part of modern day medical civil defense. During every-day conditions they improve the outcome of even the most severe medical cases as long as quality assurance is enabled and the system constantly evolves.
Quality markers of EMS are the Kirschner principle, the Ahnefeld theorem, whole-area coverage of air-rescue, response time, proper management of the golden hour, standard operating procedures, nation-wide standardized equipment, teaching and training. Usage of digital devices to monitor, analyze and define research and current standards of treatment, especially for severely injured cases is a major factor to further decrease lethality and improve the quality of life. Germany's trauma-network and registry is a milestone in this regard.
EMS has to be organized and structured by national laws in order to have the highest possible impact. In general, they should be operated by especially trained professionals. An asset is, if they also involve the public (e.g. awareness, first aid) and can rely on voluntary forces to assist cost-intensive professional forces.
EMS also forms the first line of defense during mass casualties and disasters. But regional forces will, according to the definition of a disaster, sooner or later be overwhelmed by the effects of the incident. Therefore, each nation needs to organize reserves and follow-up forces. This is a vital task for sovereign societies, since during disasters or in the aftermath of disasters, international aid is often not sufficient to care for a nation in the long-run.
Current disaster zones around the globe (e.g. Sudan, Somalia) show that subsidiary help can only help to ease the situation and prolong the survival. But not solve it. It is therefore necessary for each nation to regulate and structure its own civil defensive capabilities in order to achieve resilience towards disasters. A well-functioning and highly capable nation-wide EMS is the first-line of disaster defense and the primary tool. Even if cost-intensive to be setup, its worth can be proven by the survival of an individual as well by the prolonged resilience towards disasters.
However, disasters don't respect borders and in a globalized world the consequences of another one's disaster can easily affect the whole global system. As a final conclusion Disaster management, even if foremost being a task of national authority, must integrate into international systems. Or as an old Chinese saying states: “一根筷子易折断,十根筷子硬如铁“.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.cjtee.2017.09.003.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Kirschner M. Die Fahrbare chirurgische Klinik. Der Chirurg. 1938;10:713–717. Jahrgang Heft 20. [Google Scholar]
- 2.Ahnefeld F.W., Kilian J. Wiederbelebungsmaßnahmen und Transportprobleme bei Notfallsituationen in der Praxis. Internist. 1970;11:41–46. [PubMed] [Google Scholar]
- 3.Pirogov N.I. Verlag F.W.C; Vogel, Leipzig: 1864. Grundzüge der allgemeinen Kriegschirurgie. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.