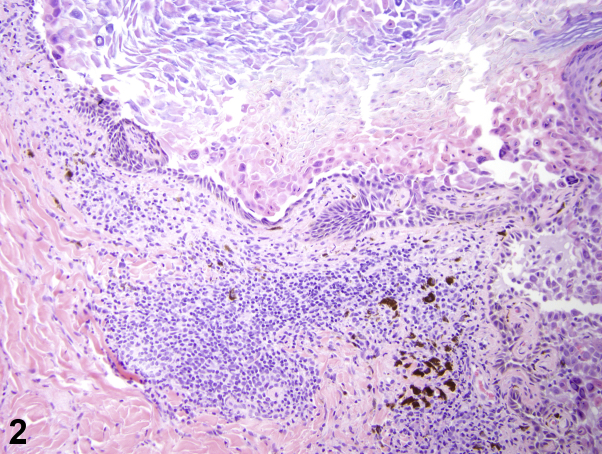
An otherwise healthy 19-year-old African-American man presented with a 6-month history of unremitting scabbed lesions on the scalp. Physical examination found hyperkeratotic plaques with matted, powdery, white crust along the scalp (Fig 1, A and B). He did not respond to antibiotic therapy with cephalexin and doxycycline or topical antifungal therapy with ketoconazole 2% shampoo. A punch biopsy was obtained. On histopathology, suprabasilar acantholysis was seen (Fig 2). Additional studies were subsequently done, including a direct immunofluorescence (DIF), which indicated epidermal IgG and C3 deposition with sparse junctional C3 deposition. Periodic acid–Schiff was suggestive of superficial colonization.
Fig 1.
Fig 2.
Question 1: What is the most likely diagnosis?
-
A.
Seborrheic dermatitis
-
B.
Tinea capitis
-
C.
Pemphigus vulgaris
-
D.
Scalp psoriasis
-
E.
Bullous pemphigoid
Anwers:
-
A.
Seborrheic dermatitis – Incorrect. This diagnosis is not supported given histopathology findings and the positive DIF.
-
B.
Tinea capitis – Incorrect. This diagnosis is not supported given histopathology findings and the positive DIF. Superficial colonization is a nonspecific finding and may represent biocontamination.
-
C.
Pemphigus vulgaris – Correct. This is the most likely diagnosis given histopathology findings of suprabasilar acantholysis, which is consistent with pemphigus vulgaris. Findings of epidermal IgG and C3 deposition is also consistent with this diagnosis.
-
D.
Scalp psoriasis – Incorrect. This diagnosis is not supported given histopathology findings and the positive DIF.
-
E.
Bullous pemphigoid – Incorrect. Suprabasilar acantholysis is absent in bullous pemphigoid. However, loss of intercellular connections is expected in a disease such as pemphigus vulgaris.
Question 2: Which of the following is not a mainstay for management of this condition?
-
A.
Rituximab
-
B.
Prednisone
-
C.
Azathioprine
-
D.
Mycophenolate mofetil
-
E.
Etanercept
Anwers:
-
A.
Rituximab – Incorrect. Rituximab is among the most common drugs used in treatment of pemphigus.1
-
B.
Prednisone – Incorrect. Prednisone is among the most common drugs used in treatment of pemphigus.1
-
C.
Azathioprine – Incorrect. Azathioprine is among the most common drugs used in treatment of pemphigus. Many clinicians consider azathioprine the immunosuppressant drug of choice because of its long history of use.2
-
D.
Mycophenolate mofetil – Incorrect. Mycophenolate mofetil is among the most common drugs used in combination with glucocorticoids for patients with pemphigus.3
-
E.
Etanercept – Correct. The use of etanercept has been piloted with a very few patients, and the effect was found to be inconclusive.
Question 3: Findings from which of the following additional laboratory studies, if any, would be the most supportive of the suspected diagnosis?
-
A.
Rheumatoid factor (RF)
-
B.
Enzyme-linked immunosorbent assay (ELISA) testing for Dsg3 and Dsg1 autoantibodies
-
C.
ELISA testing for BP180 and BP230 autoantibodies
-
D.
Erythrocyte sedimentation rate
-
E.
None of the above
Anwers:
-
A.
RF – Incorrect. RF may be useful in the setting of psoriatic arthritis (ie, to work up possible rheumatoid arthritis), but this laboratory study does not have utility in this setting.
-
B.
ELISA testing for desmoglein (DSG) 3 and DSG1 autoantibodies – Correct. This is the test of choice in supporting the diagnosis of pemphigus vulgaris. IgG autoantibodies to DSGs are detected via ELISA in patients with pemphigus, and expression of these autoantibodies often correlates with the disease.4, 5
-
C.
ELISA testing for BP180 and BP230 autoantibodies – Incorrect. ELISA testing for BP180 and BP230 autoantibodies is helpful in the setting of bullous pemphigoid.
-
D.
Erythrocyte sedimentation rate – Incorrect. This is too nonspecific to support a diagnosis and is expected to be elevated in an inflammatory disease.
-
E.
None of the above – Incorrect. Given the suspected diagnosis of pemphigus, ELISA testing for DSG3 and DSG1 autoantibodies can be a supportive laboratory test.
Footnotes
Drs Kao and Wang contributed equally to this article.
Funding sources: Dr Kiuru's involvement in this case report was in part supported by the National Cancer Institute, National Institutes of Health through grant #K12CA138464.
Conflicts of interest: None declared.
References
- 1.Cholera M., Chainani-Wu N. Management of pemphigus vulgaris. Adv Ther. 2016;33:910–958. doi: 10.1007/s12325-016-0343-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chams-Davatchi C., Mortazavizadeh A., Daneshpazhooh M. Randomized double blind trial of prednisolone and azathioprine, vs. prednisolone and placebo, in the treatment of pemphigus vulgaris. Journal of the European Academy of Dermatology and Venereology. JEADV. 2013;27:1285–1292. doi: 10.1111/j.1468-3083.2012.04717.x. [DOI] [PubMed] [Google Scholar]
- 3.Chams-Davatchi C., Esmaili N., Daneshpazhooh M. Randomized controlled open-label trial of four treatment regimens for pemphigus vulgaris. J Am Acad Dermatol. 2007;57:622–628. doi: 10.1016/j.jaad.2007.05.024. [DOI] [PubMed] [Google Scholar]
- 4.Amagai M., Tsunoda K., Zillikens D., Nagai T., Nishikawa T. The clinical phenotype of pemphigus is defined by the anti-desmoglein autoantibody profile. J Am Acad Dermatol. 1999;40:167–170. doi: 10.1016/s0190-9622(99)70183-0. [DOI] [PubMed] [Google Scholar]
- 5.Ding X., Aoki V., Mascaro J.M., Jr., Lopez-Swiderski A., Diaz L.A., Fairley J.A. Mucosal and mucocutaneous (generalized) pemphigus vulgaris show distinct autoantibody profiles. J Invest Dermatol. 1997;109:592–596. doi: 10.1111/1523-1747.ep12337524. [DOI] [PubMed] [Google Scholar]