Abstract
Aims:
The aim of the study was to determine the effect of left ventricular ejection fraction on clinical outcomes of acute ischemic stroke patients.
Study Design:
This study design was a prospective cohort observational study.
Place and Duration of Study:
This study was conducted at Stroke Unit, Neurology Ward, and Cardiology Ward at the Dr. Sardjito Hospital, Yogyakarta, Indonesia, between July and December 2016.
Materials and Methods:
Hospitalized acute ischemic stroke patients were recruited, with sample was taken by consecutive sampling until reaching amount fulfilling inclusion criterion was 62 persons. In this study, clinical outcomes were measured by National Institutes of Health Stroke Scale (NIHSS) scores as well as dependent variables and left ventricular ejection fraction as independent variables. Logistic regression analyses were performed to discover any potential independent variable that can influence the left ventricular ejection fraction role at the clinical outcomes with NIHSS scores.
Results:
Multivariate analyses revealed that several variables were significantly interacted with the influence of left ventricular ejection fraction at the clinical outcomes with NIHSS scores. These variables were the left ventricular ejection fraction <48% (95% confidence interval [CI]: 0.691–0.925; P = 0.001), left ventricular ejection fraction + low high-density lipoprotein (HDL) (95% CI: 0.73–0.949; P = 0,001), left ventricular ejection fraction + diabetes mellitus (DM) (95% CI: 0.799–0.962; P = 0,001), and left ventricular ejection fraction + low HDL + DM (95% CI: 0.841–0.98; P = 0,001).
Conclusion:
The influence of the lower left ventricular ejection fraction to clinical outcome of ischemic stroke patients has a worsening of neurological deficit outcome by considering the combination of several independent variables including the DM and low HDL.
Keywords: Clinical outcomes, ischemic stroke, left ventricular ejection fraction
INTRODUCTION
Stroke has mild-to-severe clinical manifestations and is a major cause of disability and death in developing countries. If neoplasms are not included, then stroke is ranked second as the cause of death in the world after ischemic heart disease.[1] Various scoring scales have been used to measure the neurological deficits of stroke patients. National Institutes of Health Stroke Scale (NIHSS) is a quantitative measure that is often used to measure the degree of stroke disability.[2]
One of the risk factors associated with ischemic stroke is heart failure. Some of the mechanisms underlying this association include the formation of thrombus, endothelial dysfunction, rheological factors, and cerebral autoregulation malfunctions. According to some epidemiological data, 10%–24% of all stroke patients have a history of heart failure. Heart failure not only increases the risk of stroke but also increases mortality and morbidity in stroke patients.[3]
Heart failure is a complex clinical syndrome characterized by impaired function and ventricular structure, so it cannot meet the needs of the body's metabolism. This syndrome can be caused by disruption of the pericardium, myocardium, endocardium, or large blood vessels, but it is mostly caused by left ventricular myocardial dysfunction.[4] Reduced ejection fraction provides objective documentation of left ventricular dysfunction. This is an early form of heart failure that will show changes in the cardial structure on noninvasive examination by echocardiography examination. Ejection fraction is the percentage of the final volume of left ventricular emptying and describes left ventricular systolic function.
Normal values of ejection fraction between 50% and 70% and almost half of the patients with ejection fraction ≤30 indicate clinical syndrome of heart failure.[5] Ejection fraction >50% is still considered normal, 41%–50% as mildly reduced, 31%–40% as moderately reduced, whereas ≤30% as severely reduced. From a study, it was reported that systolic dysfunction occurs if the ejection fraction is <50%.[6]
Research by Byun et al., it was reported that there was a significant relationship between the low ejection fraction and the outcome of cardioembolic stroke.[7] Nevertheless, in Indonesia, there has been no study linking between ejection fraction as an early sign of cardiac dysfunction with clinical outcome of acute ischemic stroke patients.
Based on these considerations, this study aims to determine the effect of left ventricular ejection fraction on clinical outcomes of patients with acute ischemic stroke.
MATERIALS AND METHODS
The study was conducted from July to December 2016, in the Stroke Unit Ward, Neurology Ward, and Cardiology Ward of Dr. Sardjito Hospital, Yogyakarta. Amount of 62 patients were recruited by consecutive sampling.
This study is a prospective cohort study to see the effect of left ventricular ejection fraction on clinical outcomes of patients with acute ischemic stroke. In this study, clinical outcome was determined by NIHSS score as dependent variable and left ventricular ejection fraction as independent variable.
The inclusion criteria were acute ischemic stroke patients with onset of ≤72 h who were willing to participate in this study by signing an inform consent to participate in the study, whereas the exclusion criteria were patients with heart valve disease, history of atrial fibrillation, systemic infection and/or sepsis, history of previous stroke, history of chronic disease, autoimmune, and malignancy.
Variables dependent on this study were clinical outcomes with NIHSS scores. The NIHSS reliability test between residents in the neurology department had k = 0.86.[8] Differences in NIHSS assessment are considered to be significant when the difference of 2 points or more, if the score is higher in the 2nd calculation, it has a worse predictor.
The main independent variables in this study were left ventricular ejection fraction. Other independent variables studied include age, gender, history of heart disease, smoking history, infarct location, hypertension, hypercholesterolemia, diabetes mellitus (DM), and Glasgow Coma Scale (GCS).
Data analysis in this research is done in three stages is descriptive, bivariate, and multivariate. Descriptive as the first stage is used to determine the characteristics of the subject such as clinical outcome of stroke, left ventricle ejection fraction, age, gender, history of heart disease, smoking history, infarct location, hypertension, hypercholesterolemia, DM, and GCS. Data are presented by calculating the mean and proportion between the two groups. Statistical analysis with categorical comparative bivariate was not paired using one-way ANOVA test and P value. Logistic regression analysis was performed to evaluate the association between several potential independent variables and clinical outcome.
This study has received a recommendation from the Biomedical Research Ethics Committee in humans, Faculty of Medicine, Universitas Gadjah Mada. Every patient and family involved as a research subject is given an explanation and is asked for approval by signing informed consent.
RESULTS
The basic characteristics of research subjects are obtained through descriptive analysis. This study found 62 patients with acute ischemic stroke who meet eligibility criteria in Dr. Sardjito Hospital.
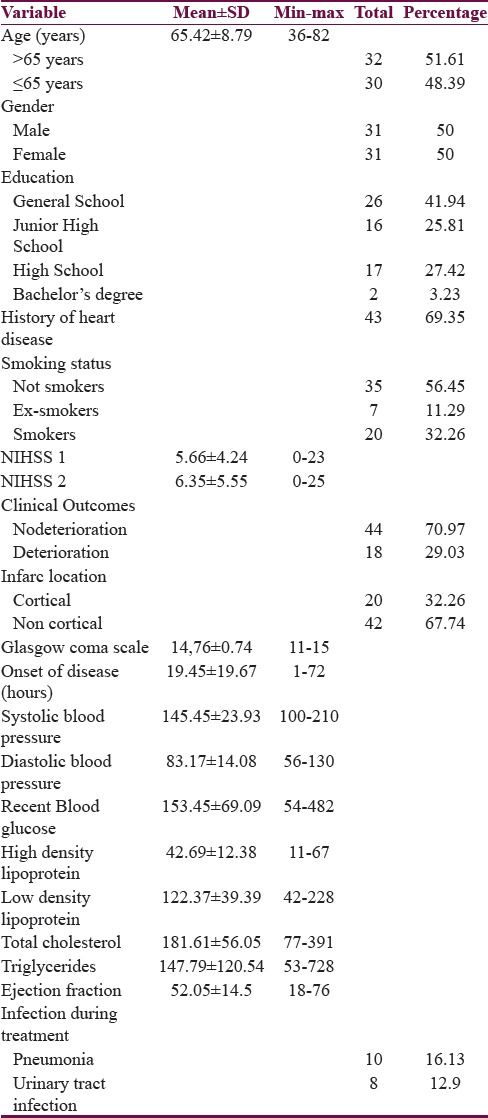
The presence of past history of heart disease in each patient was assessed. Positive past history of heart disease was found in 43 patients (69,35%), whereas 19 patients (30,65%) were free of heart disease history. The number of subjects who smoked regularly was 20 (32,26%), as ex smokers was 7 (11,29%) and without any smoking history was 35 (56,45%). The average score of NIHSS at the beginning of entry was 5.66 ± 4.24 with the lowest score 0 and the highest 23, whereas the mean score of NIHSS evaluation increased to 6.35 ± 5.55 with the lowest value 0 and the highest 25. There were 44 patients (70.97%) without worsening clinical outcomes and 8 patients (29.03%) with worsening clinical outcomes. The area of infarction lesion ≥2 cm was 41.94% with cortical lesion 32.26% and noncortical 67.74%. The average GCS at entry is 14.76 ± 0.74 with the lowest value of 11 and the highest 15. At the time of admission, the mean systolic blood pressure was 145 mmHg with the lowest value of 100 mmHg and the highest was 210 mmHg, whereas the mean diastolic blood pressure was 83 mmHg with the lowest score of 56 mmHg and the highest was 130 mmHg [Table 1].
Table 1.
Basic characteristics of the study
Average total cholesterol was 181 mg/dl with the lowest 77 mg/dl and highest of 391 mg/dl. The mean triglyceride level was 147 mg/dl with the lowest 53 mg/dl and the highest was 728 mg/dl [Table 2].
Table 2.
Variable bivariate analysis on clinical outcome
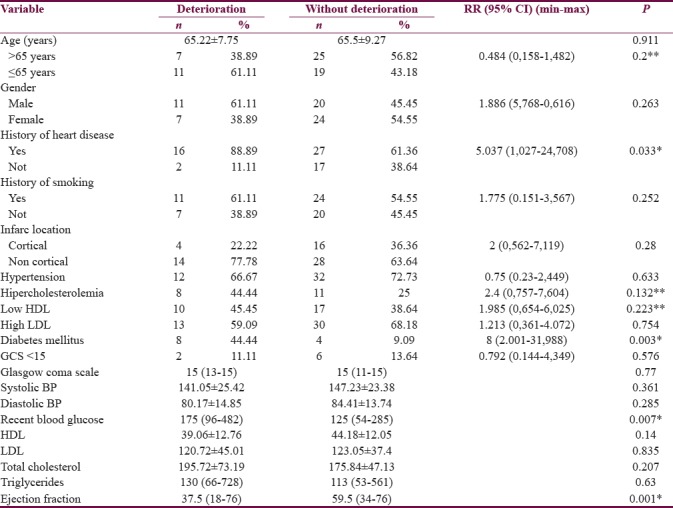
In bivariate analysis, the main variables of left ventricular ejection fraction to clinical outcomes of ischemic stroke patients showed significant differences between the deterioration and without deterioration groups. Left ventricular ejection fraction in patients with deterioration was 37.5 (18%–76%) compared with patients without deterioration was 56.5 (34%–76%) with P = 0.001.
The result of bivariate analysis of age variable on the deterioration of neurological deficit did not found a significant difference between patient age and deterioration of neurological deficit (P = 0.911). In the gender variable, there was no significant difference to the deterioration of the neurological deficit (P = 0.263).
The result of bivariate analysis of the history of heart disease variables on the deterioration of the neurological deficit was found to be a significant difference to the deterioration of the neurological deficit with Relative Risk (RR) = 5.037 (95% confidence interval [CI]: 1.027–24.708; P = 0.033). In the history of hypertension, there was no significant difference to the deterioration of neurological deficit with RR = 0.75 (95% CI: 0.23–2.449; P = 0.633). Systolic and diastolic blood pressure variables showed no difference in mean systolic blood pressure and median diastolic blood pressure (P = 0.361 and P = 0.285).
The result of bivariate analysis for other laboratory parameters such as history of DM variables found a significant difference to the deterioration of neurological deficit with RR = 8 (95% CI: 2.001–31.988; P = 0.003). Random blood sugar variables were found to have a median difference (P = 0.007). In the variable of dyslipidemia, there was no significant difference to the deterioration of neurologic deficit. Variables of high-density lipoprotein (HDL), low-density lipoprotein, total cholesterol, or triglycerides did not show any significant difference to the deterioration of neurological deficit (P = 0.14, P = 0.835, P = 0.207, and P = 0.63).
The result of bivariate analysis of variables on smoking history was no significant difference to the deterioration of neurological deficit with RR = 1.775 (95% CI: 0.151–3.567; P = 0.252). Furthermore, in the variables of the lesion location, there was no significant difference to the deterioration of the neurological deficit with RR = 2 (95% CI: 0.562–7.119; P = 0.28).
In this study, to determine the limitation of left ventricular ejection fraction, the analysis of receiver operating characteristic (ROC) was used. The value of AUC (area under the ROC curve) is obtained from 100% ROC method and P = 0.001; statistically, 100% AUC is powerful. To determine the right value of fraction ejection to be used in obtaining right sensitivity, specificity, and good predictive value, so it was continued with the determination of sensitivity and specificity curve cutting point. Sensitivity and specificity cutting point was obtained in subject number 12 with ejection fraction value was 48%.
From cross-tabulation test of the relationship between left ventricular ejection fraction with clinical outcomes of ischemic stroke patients, it was obtained that patient with left ventricular ejection fraction <48% more had deterioration was 57.14%, compared with the left ventricular ejection fraction >48% as many as 5.88% (P = 0.001; RR = 21.33). In this study, it could be concluded that there was a relationship between left ventricular ejection fraction <48% with deterioration clinical outcomes in ischemic stroke patients. Ischemic stroke patient with ejection fraction <48% had 21 times greater risk to get clinical deterioration.
There were several variable that potent affected clinical outcome of stroke patient called confounding factors. Variables with P < 0.25 were included in multivariate model which would be interacted to know whether those variables also affecting the study result. Those variables were age <65 years, history of heart disease, hypercholesterolemia, low HDL, and DM.
To find out whether these variables affected the clinical outcomes of ischemic stroke patient, then it was tested with logistic regression test [Table 3].
Table 3.
Logistic regression variables which affect clinical outcomes
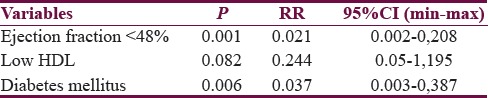
The final results of the logistic regression test yield a P < 0.05; the final variables that affect the clinical outcomes of ischemic stroke patients are the fraction ejection <48%, low HDL, and DM. The final variables that affect the clinical outcomes of ischemic stroke patients are the fraction ejection <48%, low HDL, and DM, with P value 0.001, 0.082, and 0.006 respectively.
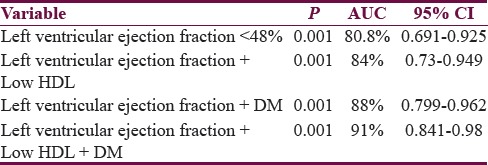
To find out how great the effect of low HDL variable and DM affected clinical outcomes of ischemic stroke besides left ventricular ejection fraction variable <48%, it was tested with under curve area test.
Based on Table 4, the influence of left ventricular ejection fraction, low HDL, and DM, it is obtained that ischemic stroke patient with ejection fraction decline <48% has deterioration clinical outcomes that were 80.8% with P < 0.001. Patient with reduction in left ventricular ejection fraction <48% and low HDL has deterioration clinical outcomes that were 84% with P < 0.001. Patient with reduction in left ventricular ejection fraction <48% and DM has deterioration clinical outcomes that were 88% with P = 0.001. Patient with reduction in left ventricular ejection fraction <48%, low HDL, and DM has deterioration clinical outcomes were 91% with P = 0.001.
Table 4.
Area under curve of the variables that affect clinical outcomes
DISCUSSION
In this study, it was obtained the relationship between the left ventricle ejection fraction with clinical outcomes of ischemic stroke patients with the RR = 21.33 (95% CI: 4.253–107.021; P = 0.001). Left ventricular ejection fraction in patients who experienced deterioration had clinical outcomes lower; it was 37.5 (18%–76%) compared to patients who did not experience a deterioration of clinical outcomes of 56.5 (34%–76%) with P = 0.001. This was similar to study of Milionis et al. with a sample of 2439 subjects which mention that the low left ventricular ejection fraction affected significantly on functional status which was measured using minimal residual disease and the mortality of the 7th day after onset (odds ratio [OR] = 0.46 and OR = 2.89).[9] Study of 135 acute ischemic stroke patients by Rojek et al. mentioned that the left ventricular ejection fraction was higher in patients with better outcomes (54.3 ± 7.9 vs. 49.9 ± 9.8%; P = 0.005), and outcome measurement was conducted with NIHSS in the 10th day. Patients with low left ventricular ejection fraction were associated with decreased autoregulation function of the brain, and brain structure change had occurred. This abnormality condition did not give manifestation before the onset of a stroke.[10] Study of Byun et al.[7] mentioned that the ejection fraction is a strong predictor of acute ischemic stroke patient in 90 days (OR = 0.94). Other study by Cuadrado-Godia et al. with 540 subjects mentioned that heart failure with low ejection fraction as an independent predictor for worse clinical outcomes measured by modified Rankin Scale in the 90th day (OR = 3.01 and P = 0.008).[11] This is mentioned because there are companion's conditions in patients with low ejection fraction such as coronary heart disease, hypertension, and valvular heart disease so that gave impact on the increasing arteriosclerosis and endothelial dysfunction. Left ventricular ejection fraction was found with other factors such as age, incoming NIHSS, brain natriuretic peptide level, coronary heart disease, and atrial fibrillation, and they were statistically significant as predictor stroke outcomes.
Patient with declining ejection fraction had high left ventricular filling pressure that led to decrease in the stroke volume. Reduced ejection fraction has shown to have a role in causing decreased of brain blood vessels reactivity which subsequently leads to cerebral hypoperfusion. Several studies had discussed about heart failure as outcome predictor in ischemic stroke patient. One of the studies proved heart failure as independent predictor toward bad functional prognosis postischemic stroke.[12] Another study stated that stroke risk significantly increased in the initial phase of heart failure diagnosis.[13] In addition, another study mentioned that there was a significant relationship between low ejection fraction with cardioembolic stroke outcomes.[7]
Left ventricular ejection fraction was a determinant factor for clinical outcomes in ischemic stroke patients. Left ventricular ejection fraction in ischemic stroke patient with deterioration was lower than ischemic stroke patient without deterioration. Limits on low or normal ejection fraction of the left ventricle depended on the existing population. However, the clinician gave the left ventricular ejection fraction a low limit <50%.
On the DM history variable, it is obtained significant difference toward a deterioration of neurological deficit with RR = 8 (95% CI: 2.001–31.988; P = 0.003). By random blood sugar variable, it is obtained difference in median value (P = 0.007). This is similar to the study of Weimar et al. which get a significant difference in DM history (P = 0.002) with neurological deterioration which is assessed with NIHSS on 48–72 h after onset.[14] Ryu et al. also get a significant difference of DM history (P = 0.003) and the difference in average glucose level in mmol/L (7.6 ± 2.8 compared to 6.7 ± 2.5; P = 0.008) and a deterioration which is rated from an increase in NIHSS score ≥2 in 3 weeks.
This is contrast with study results from Nacu et al. which do not get DM history difference (P = 0.81) or difference in median glucose levels (P = 0.74) toward a neurological deterioration which is rated from an increase in NIHSS score ≥4 in 9 h since first onset.[15] A study by Lok and Gulach finds that DM history is not significantly take effect into ischemic stroke patients’ mortality (P = 0.132).[16] Tokgoz et al. also found there were no difference in mortality based on history of DM. but obtained that the median glucose levels are significantly higher in ischemic stroke patients who had died (137.5 compared with 113.0; P = 0.001).[17]
Hyperglycemia condition was found on the majority of acute ischemic stroke patients in initial phase and there were much studies support the theory that increased glucose may deteriorate the prognosis. The theory was mentioned that tissue acidosis which was causing anaerobic glycolysis, damaging the blood–brain barrier, resulting in cerebral edema, and increasing hemorrhage transformation.[18] Advanced study using MR spectroscopy showed that hyperglycemia in patients with impaired perfusion-diffusion was related to depletion in the recovery process of the tissue, the larger infarct size, and worse functional outcome.[19]
CONCLUSION
Ischemic stroke patients with low ejection fraction value have a deterioration neurological deficit compared with patients with normal ejection fraction. Thus, left ventricular ejection fraction examination is recommended for ischemic stroke patient because it affects the clinical outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Di Carlo A. Human and economic burden of stroke. Age Ageing. 2009;38:4–5. doi: 10.1093/ageing/afn282. [DOI] [PubMed] [Google Scholar]
- 2.Shah R, Vyas C, Vora J. NIHSS score: A handy tool to predict vascular occlusion in acute ischemic stroke. NHL J Med Sci. 2014;3:18–22. [Google Scholar]
- 3.Haeusler KG, Laufs U, Endres M. Chronic heart failure and ischemic stroke. Stroke. 2011;42:2977–82. doi: 10.1161/STROKEAHA.111.628479. [DOI] [PubMed] [Google Scholar]
- 4.Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: A position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–6. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- 5.Davis S. Endpoints and statistical concerns for acute stroke therapy trials. In: Fisher MMD, editor. Stroke therapy. 2nd ed. Butterworth-Heinemann; 2001. pp. 123–33. [Google Scholar]
- 6.Hays AG, Sacco RL, Rundek T, Sciacca RR, Jin Z, Liu R, et al. Left ventricular systolic dysfunction and the risk of ischemic stroke in a multiethnic population. Stroke. 2006;37:1715–9. doi: 10.1161/01.STR.0000227121.34717.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Byun JI, Jung KH, Kim YD, Kim JM, Roh JK. Cardiac function and outcomes in patients with cardio-embolic stroke. PloS one. 2014;9:9577–85. doi: 10.1371/journal.pone.0095277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasanah M, Paryono Test Reliability NIHSS (National Institutes of Health Stroke Scales) Version of Indonesia to Assess the Degree of Neurological Deficits in Patients of Ischemic Stroke. Research Report, Faculty of Medicine Universitas Gadjah Mada, Yogyakarta. 2013 [Google Scholar]
- 9.Milionis H, Faouzi M, Cordier M, Ambrogio R, Eskandari A, Michel P, et al. Characteristics and early and long-term outcomes in patients with acute ischemic stroke and low ejection fraction. Int J Cardiol. 2012;168:1082–7. doi: 10.1016/j.ijcard.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 10.Rojek A, Gąsecki D, Fijałkowski M, Kowalczyk K, Kwarciany M, Wolf J, et al. Left ventricular ejection fraction and aortic stiffness are independent predictors of neurological outcome in acute ischemic stroke. J Hypertens. 2016;34:2441–8. doi: 10.1097/HJH.0000000000001095. [DOI] [PubMed] [Google Scholar]
- 11.Cuadrado-Godia E, Ois A, Roquer J. Heart failure in acute ischemic stroke. Curr Cardiol Rev. 2010;6:202–13. doi: 10.2174/157340310791658776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burkot J, Kopec G, Pera J, Slowik A, Dziedzic T. Decompensated heart failure is a strong independent predictor of functional outcome after ischemic stroke. J Card Fail. 2015;21:642–6. doi: 10.1016/j.cardfail.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Alberts VP, Bos MJ, Koudstaal P, Hofman A, Witteman JC, Stricker B, et al. Heart failure and the risk of stroke: The Rotterdam Study. Eur J Epidemiol. 2010;25:807–12. doi: 10.1007/s10654-010-9520-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weimar C, Mieck T, Buchthal J, Ehrenfeld CE, Schmid E, Diener HC, et al. Neurologic worsening during the acute phase of ischemic stroke. Arch Neurol. 2005;62:393–7. doi: 10.1001/archneur.62.3.393. [DOI] [PubMed] [Google Scholar]
- 15.Nacu A, Bringeland GH, Khanevski A, Thomassen L, Waje-Andreassen U, Naess H, et al. Early neurological worsening in acute ischaemic stroke patients. Acta Neurol Scand. 2016;133:25–9. doi: 10.1111/ane.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lok U, Gulach U. The predictive effects of the neutrophil to lymphocyte ratio (NLR) on the mortality of acute ischemic stroke and its subtypes: A retrospective cross-sectional study. Eurasian J Emerg Med. 2016;15:69–72. [Google Scholar]
- 17.Tokgoz S, Kayrak M, Akpinar Z, Seyithanoǧlu A, Güney F, Yürüten B, et al. Neutrophil lymphocyte ratio as a predictor of stroke. J Stroke Cerebrovasc Dis. 2013;22:1169–74. doi: 10.1016/j.jstrokecerebrovasdis.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Thanvi B, Treadwell S, Robinson T. Early neurological deterioration in acute ischaemic stroke: Predictors, mechanisms and management. Postgrad Med J. 2008;84:412–7. doi: 10.1136/pgmj.2007.066118. [DOI] [PubMed] [Google Scholar]
- 19.Parsons MW, Barber PA, Desmond PM, Baird TA, Darby DG, Byrnes G, et al. Acute hyperglycemia adversely affects stroke outcome: A magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52:20–8. doi: 10.1002/ana.10241. [DOI] [PubMed] [Google Scholar]


