To the Editor: Metabolic syndrome (MetS) is a major public health issue, resulting in accelerated development of diabetes mellitus, cardiovascular disease, kidney disease, and even cancer.[1] Resting heart rate (RHR) may be an independent risk factor for MetS. Herein, we reported a cohort study to determine the association of RHR with the risks of MetS in general population in northern China.
Jidong cohort was located in Tangshan. The cohort members completed a standardized questionnaire and underwent physical examinations and laboratory assessments at recruitment from 2013 to 2014. Among them, 7041 participants with complete data of MetS and RHR were available, and 188 participants with the history of heart failure, myocardial infarction, atrial fibrillation or atrial flutter or the medication history of β-receptor blocker were excluded from the study. Finally, a total of 6853 participants were included in the study. RHR was measured for participants sitting in a controlled environment for at least 5 min at a room temperature between 22°C and 25°C in the morning between 8:00 AM and 11:00 AM. Participants had banned smoking and drinking coffee, tea or wine for at least 3 h and had not exercised in the last 30 min before measuring RHR. All medical examinations were conducted by specially trained doctors and nurses. RHR was examined using electrocardiogram and was classified into <60, 60–69, 70–79, 80–89, and ≥90 beats/min. The diagnosis of the MetS was based on the new definition of the International Diabetes Federation for China.[2] A multivariable logistic analysis was used to evaluate the association between RHR and MetS.
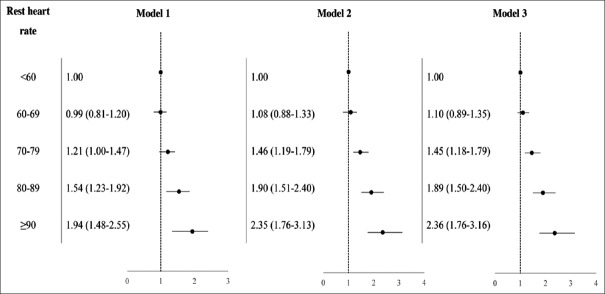
In this study, a total of 2023 (29.5%) participants were diagnosed with the MetS. The mean age of participants was 42.5 years old and 51.6% (3541) were men. With the RHR increasing, the prevalence of MetS also increased. Compared to participants with RHR <60 beats/min, the odds ratios (95% confidence intervals) for participants with the RHR of 70–79, 80–89, and ≥90 beats/min groups were 1.45 (1.18–1.79), 1.89 (1.50–2.40), and 2.36 (1.76–3.16), respectively [Figure 1], after adjusting for age, gender, income, education, physical activity, drinking, and smoking. Subgroup analysis showed that individuals aged younger than 45 years had a higher risk to develop MetS than those older than 45 years [Table 1].
Figure 1.
Odds ratios and 95% confidence interval for developing metabolic syndrome according to categories of resting heart rate. Model 1: Unadjusted; .Model 2: Adjusted for age and gender; Model 3: Adjusted for age, gender, income, education, physical activity, drinking, smoking.
Table 1.
Logistic analysis of resting heart rate and metabolic syndrome stratified by age, gender, and physical activity
| Characteristics | Resting heart rate | P | ||||
|---|---|---|---|---|---|---|
| <60 bpm | 60–69 bpm | 70–79 bpm | 80–89 bpm | ≥90 bpm | ||
| Gender* | ||||||
| Male | Reference | 1.12 (0.84–1.49) | 1.60 (1.21–2.12) | 1.94 (1.41–2.66) | 2.37 (1.61–3.49) | 0.64 |
| Female | Reference | 1.08 (0.80–1.46) | 1.29 (0.95–1.75) | 1.86 (1.31–2.64) | 2.38 (1.52–3.74) | |
| Age† | ||||||
| <45 years | Reference | 1.30 (0.90–1.87) | 1.74 (1.22–2.49) | 2.70 (1.84–3.95) | 3.34 (2.15–5.18) | 0.02 |
| ≥45 years | Reference | 1.08 (0.83–1.39) | 1.38 (1.06–1.79) | 1.41 (1.02–1.93) | 1.69 (1.11–2.57) | |
| Physical activity‡ | ||||||
| Inactive | Reference | 0.98 (0.69–1.41) | 1.38 (0.96–1.97) | 2.00 (1.35–2.95) | 1.97 (1.23–3.18) | 0.78 |
| Moderately active | Reference | 1.13 (0.51–2.48) | 1.27 (0.58–2.76) | 2.05 (0.86–4.87) | 2.94 (1.10–7.87) | |
| Active | Reference | 1.17 (0.89–1.52) | 1.53 (1.17–2.00) | 1.75 (1.28–2.39) | 2.57 (1.71–3.87) | |
Data were presented by ORs (95% CIs). *Gender subgroup adjusted for age, income, education, drinking, smoking, and physical activity; †Age subgroup adjusted for gender, income, education, drinking, smoking, and physical activity; ‡Physical activity subgroup adjusted for gender, age, income, education, drinking, and smoking. Bpm: Beats/min; CIs: Confidence intervals; ORs: Odds ratios.
Our findings validate previous studies that RHR is correlated to the development of MetS among different populations.[3,4] However, It was also found that the risk of MetS was higher in younger participants (<45 years) than in older participants (≥45 years) as RHR increased, which was not consistent with the similar study.[5] The increasing pressure of working and living young people faced in this study may explain the difference between our study and previous studies. The possible reasons for the association might be the acceleration of RHR which would stimulate the sympathetic dysfunction which in turn could affect some main indicators of insulin resistance and blood pressure that finally result in the occurrence of MetS. The findings of this study might provide a new clue for clinicians to conduct early detection and intervention for MetS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form(s), the patient(s)/patient's guardians has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients/patient's guardians understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by grants from the National Social Science Fund of China (No. 17BGL184) and Central-level Nonprofit Scientific Research Institutes of Basic Scientific Research Projects of China (No. 2017PT63009).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Wu SH, Liu Z, Ho SC. Metabolic syndrome and all-cause mortality: A meta-analysis of prospective cohort studies. Eur J Epidemiol. 2010;25:375–84. doi: 10.1007/s10654-010-9459-z. doi: 10.1007/s10654-010-9459-z. [DOI] [PubMed] [Google Scholar]
- 2.Alberti KG, Zimmet P, Shaw J IDF Epidemiology Task Force Consensus Group. The metabolic syndrome – A new worldwide definition. Lancet. 2005;366:1059–62. doi: 10.1016/S0140-6736(05)67402-8. doi: 10.1016/s0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 3.Licht CM, Vreeburg SA, van Reedt Dortland AK, Giltay EJ, Hoogendijk WJ, DeRijk RH, et al. Increased sympathetic and decreased parasympathetic activity rather than changes in hypothalamic-pituitary-adrenal axis activity is associated with metabolic abnormalities. J Clin Endocrinol Metab. 2010;95:2458–66. doi: 10.1210/jc.2009-2801. doi: 10.1210/jc.2009-2801. [DOI] [PubMed] [Google Scholar]
- 4.Jiang X, Liu X, Wu S, Zhang GQ, Peng M, Wu Y, et al. Metabolic syndrome is associated with and predicted by resting heart rate: A cross-sectional and longitudinal study. Heart. 2015;101:44–9. doi: 10.1136/heartjnl-2014-305685. doi: 10.1136/heartjnl-2014-305685. [DOI] [PubMed] [Google Scholar]
- 5.O'Hartaigh B, Jiang CQ, Bosch JA, Zhang WS, Cheng KK, Lam TH, et al. Influence of heart rate at rest for predicting the metabolic syndrome in older Chinese adults. Acta Diabetol. 2013;50:325–31. doi: 10.1007/s00592-012-0396-z. doi: 10.1007/s00592-012-0396-z. [DOI] [PubMed] [Google Scholar]